Patent Ductus Arteriosus and Hypotension in a Preterm Infant: Fluids or Furosemide?
Article Information
Shabih Manzar
Department of Pediatrics, College of Medicine, Louisiana State University of Health Sciences, 1501 Kings Highway, Shreveport, LA, 71130, USA
*Corresponding Author: Shabih Manzar, Associate Professor, Department of Pediatrics, College of Medicine
Louisiana State University of Health Sciences, 1501 Kings Highway, Shreveport, LA, 71130, USA
Received: 22 June 2020; Accepted: 06 July 2020; Published: 08 July 2020
Citation: Shabih Manzar. Patent Ductus Arteriosus and Hypotension in a Preterm Infant: Fluids or Furosemide?. Fortune Journal of Health Sciences 3 (2020): 103-109.
View / Download Pdf Share at FacebookAbstract
Abstract
Hypotension is common in preterm infants. A gestational age-based BP range has been published but the definition of “normal” blood pressure (BP) in preterm infant has not been established. The use of gestational age as surrogate of mean arterial BP is discouraged. Preterm infants are at risk of low blood flow and low BP due to many factors. Patent ductus arteriosus (PDA) is one of the factor that leads to diastolic hypotension because of the diastolic run off of blood flow into the pulmonary vascular system from left-to-right shunt. Hypotension with is often difficult to treat. The dilemma is restricting versus liberalizing fluids. At one end we have fluid overload on left atrium while at the other end we have pulmonary edema. We present a case in brief, followed by the discussion on how one should approach such a situation.
Keywords
Infant; Hypotension
Hypotension articles, blood pressure articles blood pressure Research articles blood pressure review articles blood pressure PubMed articles blood pressure PubMed Central articles blood pressure 2023 articles blood pressure 2024 articles blood pressure Scopus articles blood pressure impact factor journals blood pressure Scopus journals blood pressure PubMed journals blood pressure medical journals blood pressure free journals blood pressure best journals blood pressure top journals blood pressure free medical journals blood pressure famous journals blood pressure Google Scholar indexed journals Hypotension articles Hypotension Research articles Hypotension review articles Hypotension PubMed articles Hypotension PubMed Central articles Hypotension 2023 articles Hypotension 2024 articles Hypotension Scopus articles Hypotension impact factor journals Hypotension Scopus journals Hypotension PubMed journals Hypotension medical journals Hypotension free journals Hypotension best journals Hypotension top journals Hypotension free medical journals Hypotension famous journals Hypotension Google Scholar indexed journals Gestational Age articles Gestational Age Research articles Gestational Age review articles Gestational Age PubMed articles Gestational Age PubMed Central articles Gestational Age 2023 articles Gestational Age 2024 articles Gestational Age Scopus articles Gestational Age impact factor journals Gestational Age Scopus journals Gestational Age PubMed journals Gestational Age medical journals Gestational Age free journals Gestational Age best journals Gestational Age top journals Gestational Age free medical journals Gestational Age famous journals Gestational Age Google Scholar indexed journals ventricular articles ventricular Research articles ventricular review articles ventricular PubMed articles ventricular PubMed Central articles ventricular 2023 articles ventricular 2024 articles ventricular Scopus articles ventricular impact factor journals ventricular Scopus journals ventricular PubMed journals ventricular medical journals ventricular free journals ventricular best journals ventricular top journals ventricular free medical journals ventricular famous journals ventricular Google Scholar indexed journals ejection fraction articles ejection fraction Research articles ejection fraction review articles ejection fraction PubMed articles ejection fraction PubMed Central articles ejection fraction 2023 articles ejection fraction 2024 articles ejection fraction Scopus articles ejection fraction impact factor journals ejection fraction Scopus journals ejection fraction PubMed journals ejection fraction medical journals ejection fraction free journals ejection fraction best journals ejection fraction top journals ejection fraction free medical journals ejection fraction famous journals ejection fraction Google Scholar indexed journals Triglycerides articles Triglycerides Research articles Triglycerides review articles Triglycerides PubMed articles Triglycerides PubMed Central articles Triglycerides 2023 articles Triglycerides 2024 articles Triglycerides Scopus articles Triglycerides impact factor journals Triglycerides Scopus journals Triglycerides PubMed journals Triglycerides medical journals Triglycerides free journals Triglycerides best journals Triglycerides top journals Triglycerides free medical journals Triglycerides famous journals Triglycerides Google Scholar indexed journals atrial septal defect articles atrial septal defect Research articles atrial septal defect review articles atrial septal defect PubMed articles atrial septal defect PubMed Central articles atrial septal defect 2023 articles atrial septal defect 2024 articles atrial septal defect Scopus articles atrial septal defect impact factor journals atrial septal defect Scopus journals atrial septal defect PubMed journals atrial septal defect medical journals atrial septal defect free journals atrial septal defect best journals atrial septal defect top journals atrial septal defect free medical journals atrial septal defect famous journals atrial septal defect Google Scholar indexed journals epinephrine articles epinephrine Research articles epinephrine review articles epinephrine PubMed articles epinephrine PubMed Central articles epinephrine 2023 articles epinephrine 2024 articles epinephrine Scopus articles epinephrine impact factor journals epinephrine Scopus journals epinephrine PubMed journals epinephrine medical journals epinephrine free journals epinephrine best journals epinephrine top journals epinephrine free medical journals epinephrine famous journals epinephrine Google Scholar indexed journals mean arterial pressure articles mean arterial pressure Research articles mean arterial pressure review articles mean arterial pressure PubMed articles mean arterial pressure PubMed Central articles mean arterial pressure 2023 articles mean arterial pressure 2024 articles mean arterial pressure Scopus articles mean arterial pressure impact factor journals mean arterial pressure Scopus journals mean arterial pressure PubMed journals mean arterial pressure medical journals mean arterial pressure free journals mean arterial pressure best journals mean arterial pressure top journals mean arterial pressure free medical journals mean arterial pressure famous journals mean arterial pressure Google Scholar indexed journals
Article Details
Introduction
The definition of “normal” blood pressure (BP) in preterm infant is not established. Observational study with limited data has been published providing a gestational age-based BP range (Table) [1]. In preterm infants the most common cause of diastolic hypotension is a patent ductus arteriosus (PDA). This occurs because of diastolic run off into the pulmonary vascular system from left-to-right shunt [2]. Due to the shunting and increase flow in the pulmonary vasculature, fluid overload occurs in the lungs leading to edema. Further venous congestion increases the preload on the left atrium. Therefore, decision regarding giving fluids or furosemide is not easy. Many factors play a role in the management of hypotension with PDA. Here we present a case of preterm infant who had hypotension and PDA. The case presentations is followed by literature review on the approach to treatment of hypotension with PDA.
Table: Normal blood pressure ranges at different gestational ages
|
Gestational Age (Weeks) |
Systolic BP (mmHg) |
Diastolic BP (mmHg) |
Mean BP (mmHg) |
|
24 |
32 |
15 |
26 |
|
25 |
34 |
16 |
26 |
|
26 |
36 |
17 |
27 |
|
27 |
38 |
17 |
27 |
|
28 |
40 |
18 |
28 |
|
29 |
42 |
19 |
28 |
|
30 |
43 |
20 |
29 |
|
31 |
45 |
20 |
30 |
|
32 |
46 |
21 |
30 |
|
33 |
47 |
22 |
30 |
|
34 |
48 |
23 |
31 |
|
35 |
49 |
24 |
32 |
Adapted from: Arch Dis Child Fetal Neonatal Ed.1999; 80: F38-F42 (Reference 1)
Case
This male infant is born at 265/7 weeks of gestation to a 29-year-old G2P0010 mother. The pregnancy was complicated by class B diabetes, omphalocele and two- vessel cord. Antenatal screen were negative for any chromosomal abnormalities (FISH and Microarray negative). Mother received cerclage for short cervix. She presented to the labor unit complaining of leaking fluid. She received antibiotics, steroids, and magnesium sulphate. Next day, on examination, the fetal heel was found to be protruding from the cervix and mother was taken for C-section due to fetal malpresentation and omphalocele.
At delivery, infant was immediately intubated and omphalocele was covered with the sterile gauze. He was dried, stimulated, & bulb suctioned. Apgar scores were 2 and 5 at one and five minutes, respectively. In NICU he was placed on the oscillator ventilator. On day 4 of life, he developed a loud murmur and was noted to have low blood pressures. Echo showed mildly decreased left ventricular (LV) systolic function with ejection fraction (EF) of 50-55%, small to moderate patent ductus arteriosus (PDA) with left to right shunt (peak gradient across shunt <10 mmHg) and patent forman ovale (PFO) vs small secundum atrial septal defect (ASD) with left to right shunt. The management of hypotension was started.
Discussion
While treatment of neonatal PDA remains controversial, symptomatic management of concomitant hypotension is a clinical challenge. The question posed in this paper is about using fluid versus furosemide in dealing with hypotension in a preterm infant that happened to have a significant PDA. The usual supportive argument in favor of using furosemide is to treat the pulmonary edema secondary to left to right shunt overflowing the pulmonary vasculature. However, the potential cardiac effect of using furosemide is relaxing the PDA by activating renal prostaglandin E2 [3-5]. Also, by decreasing the preload, the cardiac output is compromised, which could accentuate hypotension further. The argument against fluid bolus is overloading the heart with extra fluid accentuating pulmonary edema. So, the question is how can we balance the treatment of hypotension in preterm infant with PDA?.
The answer lies in the complete clinical assessment of the infant. What is the respiratory status (e.g. requiring persistent mechanical support)?, are there any signs of heart failure?, or large left-to-right ductus shunt with evidence of hemodynamic compromise (echocardiogram findings)?, any signs of ductal steal phenomenon whereby descending aorta blood flow is compromised?, any oliguria or rising serum creatinine concentration? [6].
As noted in figure 1, there were no definite signs of severe pulmonary overload. The chest x-ray showed right upper lobe atelectasis and pulmonary interstitial emphysema without significant haziness. However, Figure 2a demonstrated significant PDA with left to right shunt and Figure 2b showed dilated left atrium suggesting pulmonary overflow. In the same picture (Figure 2c), however, showed a low left ventricular diastolic volume. In summary, with the mix echocardiographic findings, one cannot make a concrete decision on fluid versus furosemide.

Figure 1: Chest x-ray showing right upper lobe atelectasis (bold arrow), pulmonary interstitial emphysema (open arrow)
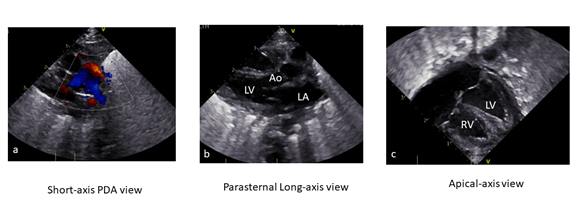
Figure 2: Echocardiogram (LA-Left Atrium, LV-Left Ventricle, Ao-Aorta, RV-Right Ventricle); a. Image obtained in Short-axis PDA view, showing PDA with left to right shunt; b. Image obtained in Long-axis PDA view, showing dilated left atrium (increase LA:Ao ratio); c. Image obtained in Apical-axis view, showing slightly low diastolic volume (Ejection Fraction 52%, confirmed by M-mode measurement).
Next assessment should be to look for systemic signs of hypoperfusion. The infants had extremities edema and capillary refill was < 2 seconds. The blood gas showed a pH of 7.28, pCO2 of 53, pO2 of 60 with HCO3 of 22 and -0.9 base access. Serum creatinine was 0.7 mg/dL with normal electrolytes. The fluid assessment showed an appropriate input and output (Figure 3). For persistent low BP, the infant received blood (hemoglobin of 12 g/dL) followed by dopamine infusion (Figure 4). Fluid bolus should not be given without complete clinical assessment. Ewer et al [7] have concluded in their study that unless there is clear evidence of hypovolemia, clinicians should exercise caution when prescribing volume expansion. They showed that aggressive fluid bolus administration of or greater than 30 mL/kg to be associated with increased mortality in neonates of 27-28 weeks' gestation.
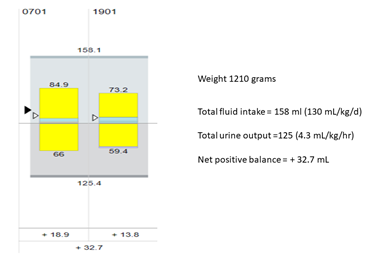
Figure 3: Showing 24-hour shift fluid intake output chart
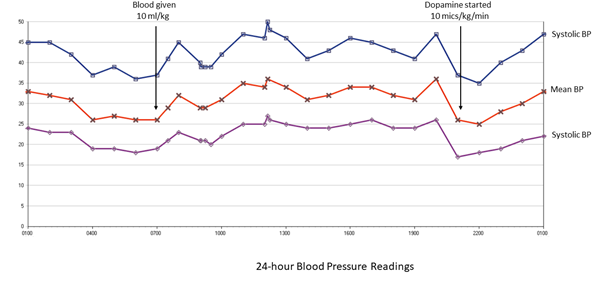
Figure 4: 24-hour Blood Pressure Readings obtained from indwelling radial artery catheter (arrows pointing at the time of use of blood and dopamine).
The other argument is the definition of hypotension in preterm infants and using a gestational age-based mean arterial pressure (MAP). Batton et al [8] have argued against the use of MAP less than or equal to the infant’s GA. Similarly, despite ongoing clinical use, literature is sparse on the comparative studies on the use dobutamine, epinephrine, norepinephrine, vasopressin or milrinone in neonatal hypotension [9]. Also, among the different vasopressors, there is no agreement on the superiority of one over other, however, dobutamine use has been down from the second to fourth vasopressor in neonatal hypotension (Figure 5) [10].
In conclusion, when encountered with hypotension in preterm infant with concomitant PDA, one must look at many factors to decide on the fluid chase or giving diuretics. Figure 6 summarizes these steps. A comprehensive assessment of the respiratory status, perfusion and urine output should be coupled with an echocardiogram and looking at blood gases, serum creatinine and electrolytes.
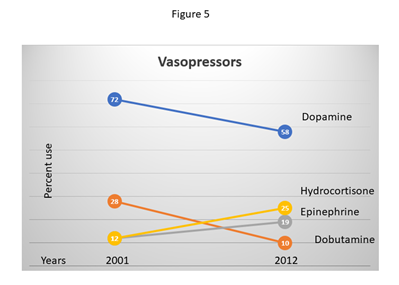
Figure 5: Pharmacotherapy of Neonatal Hypotension 2001-2012; Chart adapted from: Rios DR, et al. Pediatrics 165 (2014): 697-701
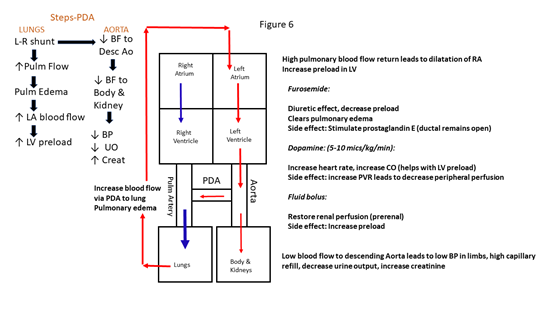
Figure 6: Summary of PDA-hypotension cycle (role of furosemide & fluid)
References:
- Northern Neonatal Nursing Initiative. Systolic blood pressure in babies of less than 32 weeks gestation in the first year of life. Archives of Disease in Childhood-Fetal and Neonatal Edition 80 (1999): F38-F42.
- Evans N, Moorcraft J. Effect of patency of the ductus arteriosus on blood pressure in very preterm infants. Archives of Disease in Childhood 67 (1992): 1169-1173.
- Laughon MM, Chantala K, Aliaga S, et al. Diuretic exposure in premature infants from 1997 to 2011. American Journal of Perinatology 32 (2015): 49-56.
- Cotton R, Suarez S, Reese J. Unexpected extra-renal effects of loop diuretics in the preterm neonate. Acta Paediatrica 101 (2012): 835-845.
- Green TP, Thompson TR, Johnson DE, et al. Furosemide promotes patent ductus arteriosus in premature infants with the respiratory-distress syndrome. New England Journal of Medicine 308 (1983): 743-748.
- Gillam-Krakauer M, Reese J. Diagnosis and management of patent ductus arteriosus. Neoreviews 19 (2018): e394-e402.
- Ewer AK, Tyler W, Francis A, et al. Excessive volume expansion and neonatal death in preterm infants born at 27–28 weeks gestation. Paediatric and Perinatal Epidemiology 17 (2003): 180-186.
- Batton B, Li L, Newman NS, et al. Use of antihypotensive therapies in extremely preterm infants. Pediatrics 131 (2013): e1865-e1873.
- Joynt C, Cheung PY. Treating hypotension in preterm neonates with vasoactive medications. Frontiers in Pediatrics 6 (2018): 86.
- Rios DR, Moffett BS, Kaiser JR. Trends in pharmacotherapy for neonatal hypotension. The Journal of Pediatrics 165 (2014): 697-701.
