Pandemic or Endemic? The Hamletic dilemma about the uncertain evolution of the Covid-19 Pandemic: the Role of Income Inequalities
Article Information
Matteo Maria Cati
Adjunct Professor, Department of Economics, University of Bologna, Italy
*Corresponding author: Matteo Maria Cati, University of Bologna, 2 Scaravilli Square, 40126 Bologna, Italy.
Received: 05 November 2022; Accepted: 11 November 2022; Published: 16 November 2022
Citation: Matteo Maria Cati. Pandemic or Endemic? The Hamletic dilemma about the uncertain evolution of the Covid-19 Pandemic: the Role of Income Inequalities. Archives of Microbiology and Immunology 6 (2022): 256-262.
View / Download Pdf Share at FacebookAbstract
The evolution of the COVID-19 pandemic, originating from severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is under the close scrutiny of the World Health Organization (W.H.O.). Many governments, such as the Italian government, are relaxing or even completely canceling the various emergency measures (as an example, readmitting no vax health personnel to work in the hospitals), and everyone is wondering when the COVID-19 pandemic will be downgraded to an endemic. Is it too soon to do so? Even if the news on the pandemic is comforting, there are still reasons for uncertainty and concern. This article raises two important questions: a) is Omicron, the SARS-CoV-2 Variant of Concern (V.O.C)s currently circulating, the last one? and b) what factors can favor or disfavor the onset of new Variant of Concern (VOCs)? The given answers to those questions have the potential to identify new lines of research.
Keywords
COVID-19, Variants of Concern (VOCs), Vaccine inequity, Income and Health Inequalities, Public Health Policy
COVID-19 articles, Variants of Concern (VOCs) articles, Vaccine inequity articles, Income and Health Inequalities articles, Public Health Policy articles
Article Details
1. Introduction
The evolution of the COVID-19 pandemic, originating from severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is under the close scrutiny of the World Health Organization (W.H.O.), whose Director General has recently stated [1] that:
- although the pandemic cannot be said to be over yet, we are presumably in its final phase;
- the only strategy that needs to be pursued is to continue the vaccination campaign to secure all the population and, in particular, health care workers and older individuals.
Many governments, such as the Italian government, are relaxing or even completely canceling the various emergency measures, and everyone is wondering when the COVID-10 pandemic will be downgraded to an endemic [2]. Is it too soon to do it? Even if the news on the pandemic is comforting, there are still reasons for uncertainty and concern.
This article raises two important questions:
- is Omicron, the SARS-CoV-2 Variant of Concern (VOCs) [3] currently circulating, the last one?
- What factors can favor or vice versa disfavor the onset of new Variant of Concern (VOCs) and change the course of the events?
Tracking the evolution of the pandemic virus is of fundamental importance, given its recent devastating impact in terms of the number of infected individuals and victims, as shown in Table 1 worldwide and in Italy (as of November 1, 2022, the total population in Italy was 59,037,000 people, and the total population in the world was 7,922,312,800 people – U.S. Census World Population clock https://worldpopulationreview.com/). Table 1 also shows the data on the vaccination campaign (number of people vaccinated with at least one dose and number of completed vaccinations):
Table 1: Number of infected individuals, number of deaths, number of doses of the vaccine as of November 1, 2022 in Italy (source: Istituto Superiore di Sanità – links: https://www.epicentro.iss.it/en/coronavirus/sars-cov-2-dashboard and (vaccines) Italian Government website https://www.governo.it/it/cscovid19/report-vaccini/) and worldwide (source: World Health Organization – link: https://covid19.who.int/)
|
|
Number of infected individuals |
Number of deaths |
People vaccinated (with at least one dose) |
Completed vaccinations
|
|
Italy |
23,442,860 |
175,318 |
50,846,155 |
47,970,350 |
|
World |
622,389,418 |
6,548,492 |
5,392,424,039 |
4,951,178,365 |
At first glance, it can be noticed that (as of November 1, 2022):
In Italy, whose overall population is 59,037,000 individuals:
- the number of infected individuals (23,325,837) corresponds to more than 39.5% of the overall population;
- the number of deaths (175,318 individuals) accounts for approximately 3% of the overall population and 0.7% of the infected individuals;
- the number of people vaccinated (with at least one dose) (50,846,155) corresponds to 84% of the population, while the number of completed vaccinations (47,970,350) corresponds to 79%.
In the world, whose overall population is 7,922,312,800 individuals:
- the number of infected individuals (622,389,418) corresponds to more than 7.85% of the global population;
- the number of deaths (6,548,492 individuals) accounts for approximately 083% of the overall population and 0.10% of the infected individuals;
- the number of people vaccinated corresponds to 68.1% of the population, while the number of completed vaccinations to 62.5%.
More in depth:
- in Italy, 8,190,845 individuals, mainly belonging to the so-called ‘no vax’ population, corresponding to approximately 16% of the total Italian population, have yet to get vaccinated. The impact of the so-called no-vax people (whose decision of not getting vaccinated is often due to low levels of educational attainment, to a low income level, to government mistrust, and to other aspects such as political attitudes) [4] on the evolution of the pandemic may be significant. On this issue, the World Health Organization (W.H.O.) has in fact indicated vaccine hesitancy [5] as one of the ten major threats to global health [6].
- however,9% (2,527,217,783 individuals) of the worldwide population, including Italy, is completely unvaccinated, showing that vaccines are unfortunately still unequally distributed to the detriment of low-income countries. In particular, in 22 African countries [7], fewer than 40 out of 100 people in the population have received a dose of the vaccine.
Can these data give us some hints on how to answer the previous questions?
2. The SARS-CoV-2 virus and its Current Trend
The answer to the first question is rather obvious and intuitive: there is no certainty that Omicron is going to be [8, 9] the last Variant of Concern (VOCs). The answer to the second question is not simple at all. The retrospective study of the recent evolution of the virus shows that the emergence of new variants has had a certain regularity (every few months), and how a new variant becomes a Variant of Concern remains an open and unsolved question [10, 11]. Is there anything that governments and health authorities can do to minimize the risk of the onset of new variants and facilitate the transition of COVID-19 from pandemic status to epidemic status?
This is quite an important issue since Omicron, the most recent Variant of Concern (VOCs), accounted [12, 13] after February 2022 for over 98% of viral sequences shared on GISAID [14]. It has proven to be highly transmissible and to have weakened the capacity of vaccines to prevent the infection so much so that various pharmaceutical multinationals (such as Pfizer, BioNtech and others [15]) have recently decided to update their vaccines to target the Omicron variant and its mutations. For this reason, one strategy might be to determine what conditions favored the rise of Omicron (also known as Pango Lineage B.1.1.529). There are different theories about where Omicron came from [16] and why no one has been able to identify its origin, such as how researchers in sequencing hundreds of millions of genomes could have missed a set of mutations that led to the rise of Omicron; that Omicron evolved during chronic long term Covid-19 infections within single individuals or that Omicron emerged in different animal hosts with respect to the ones usually considered and others. Unfortunately, thus far, there is no evidence in favor of any of the theories. However, even if there is not a clear answer, the proposed theories have a common denominator, that is, they all refer to the possibility of an unobserved evolution (for example, in a geographical area with no sequencing capacity) of the virus, considering that the collected data of the GISAID database represents less than 1% of the sequenced genomes of SARS-CoV-2 among the overall reported cases of COVID-19 in Africa, Asia and the United States. In other words, the data collected to date represent an infinitesimal part of the mass of information available, and much work needs to be done.
Table 2: Variant of Concern (VOCs) – (source: World Health Organization – Tracking SARS-CoV-2 variants. Available at the link: https://www.who.int/activities/tracking-SARS-CoV-2-variants
|
Previously circulating Variant of Concern (VOCs) |
|||
|
Country |
Scientific name (Pango lineage) |
WHO name |
Year |
|
UK |
B 1.1.7 |
Alfa |
Sept. 2020 |
|
South Africa |
B.1.351 |
Beta |
May 2020 |
|
Brazil |
P.1 |
Gamma |
Nov. 2020 |
|
India |
B.1.617.2 |
Delta |
Oct. 2020 |
|
Current circulating Variant of Concern (V.O.C.) |
|||
|
South Africa Botswana |
B.1.1.529 |
Omicron |
Nov. 2021 |
A different and perhaps more rewarding strategy [17] could be to identify where the previous and the current Variant of Concerns were first detected - see Table 2 - and thereafter to study if there are environmental and/or human factors that have facilitated their onset. SARS-CoV-2 is an extremely pathogenic and highly transmissible coronavirus that has materialized through zoonotic spillover events, such as those occurring in the Huanan Seafood Wholesale Market in Wuhan [18], China, believed to be the early epicenter of the COVID-19 pandemic in 2019. A similar spill-over event from animals to humans of the so-called SARS-CoV-1 coronavirus (giving rise to a much less lethal disease) occurred in China [19] in November 2002 in Guangdong Province, showing that there was an animal reservoir (with an increasing number of species involved in the contagion) for SARS coronavirus.
Historically and similarly with respect to the ongoing COVID-19 pandemic, most of the known pandemics, such as influenza, and of the recent epidemics, such as Ebola and Zika, are zoonoses [20, 21] i.e., they have been caused by the ‘spill over’ [22, 23] of microbes of animal origin, or to other animals that can serve as intermediate hosts, to humans due to interactions among wildlife, livestock and people. Furthermore, being an RNA virus, SARS-CoV-2, similar to other viruses of this type, tends to adapt to its new human hosts with the development of mutations over time, resulting in the appearance of multiple variants that may have different characteristics than its original strains. As we saw, some of these variants, namely, the so-called Variant of Concern (VOCs), can present concerning characteristics in terms of perniciousness, vaccine resistance, contagiousness and virulence, so much so that they represent an increasing risk for public global health. It is therefore of fundamental importance to trace and monitor the emergence of new variants and sub variants. As a recent study states, there are factors that seem to favor the onset of new variants [24]:
”emergence of new variants has been due to multiple predisposing factors, including molecular characteristics of the virus, geographic and environmental conditions, and the impact of social determinants of health that favor the genetic diversification of SARS-CoV-2 in the world”.
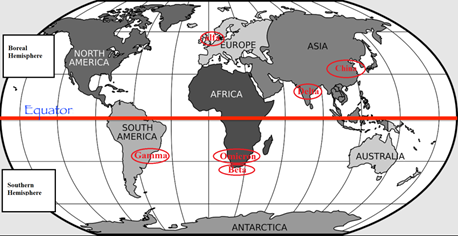
If we now notice that most of the Variants of Concerns (V.O.C)s - Table 2 - thus far have been detected in developing countries (see Figure 1 - for example, in 2020 the Delta variant (PANGO lineage: B.1.617.2) [25-27] was first detected in India and the variant Gamma (PANGO lineage P.1) was first detected in Manaus, the capital of the Amazonas state, and in a few months it spread to other Brazilian states, particularly in the southeastern region [28-30]. In 2021, the Omicron variant (also known as PANGO lineage B.1.1.529) [31-33] was first detected in South Africa and Botswana), it is intuitive to think that the complex system consisting of territoriality, environmental and economic conditions, human habits and, in particular, promiscuity with fauna, hygienic habits and eating habits, absence or inefficiency of the health system, unfortunately may become synonymous with diseases and the emergence of pandemics.
3. Ecosystem, COVID-19 and Income and Health Inequalities
There is a word that well represents and simplifies the complexity inherent in the study of pandemics, such as COVID-19, and epidemic diseases that have a zoonotic origin (i.e., caused by the ‘spill over’ of microbes of animal origin to humans), which is the word ‘interconnection’. Intuitively, any human activity that affects those interactions between the animal and the human world, such as increasing wildlife trafficking (see, for example, what has happened in the Chinese Wuhan Market), loss of biodiversity [34] (caused, for example, by tropical deforestation as in the Amazon rainforest) [35], environmental and climate changes, may become a source of danger.
Furthermore, as the literature on the transmission of SARS-CoV-2 suggests, the ‘spill over’ of microbes is bidirectional, not only from animal to human (zoonotic) but also from human to animal (zooanthroponotic). Spillback of the SARS-CoV-2 virus from humans to domestic and wild animals is well known in the literature on the topic [36-40]. Therefore, it is plausible to think that, in the complexity of the various ecosystems, there might be a triple ‘spill over’ effect of the mutated virus from animal species to humans, from humans to animal species and then back from animal species to humans, increasing the probability of the onset of new variants.
As a result, it is plausible to think that there is a strict relationship between human activities that disrupt the ecosystem and the likelihood of the development of pandemics and other infectious diseases of zoonotic and/or zooanthroponotic origin, particularly in geographic areas, such as Brazil, African nations and China, where there are human habits that encourage promiscuity with fauna, such as hygienic habits and eating habits that facilitate close contacts between humans and many animal species. Equivalently, the global ecosystem that by its nature should be a riskless asset becomes a risky ecosystem because of most human activities (pollution, resource depletion and so on). However, what can we do to handle a risky asset such as an already disrupted ecosystem? First, it is necessary to change worldwide governance toward more ecofriendly behavior. However, this change requires a strong global and intergenerational commitment that has years, if not decades, to go.
In another recent statement [41], the Director General of the World Health Organization (W.H.O.) once again stated that the only strategy to address the spread of the pandemic and the onset of new variants is vaccination of the global population. Unfortunately, as a consequence of within and across countries’ income and health inequalities and in particular poverty, vaccines [42-46] are unevenly distributed across countries. While the complete vaccination rate of the population of high-income countries (North America, Western Europe, Japan and China) is more than 70%, thus far (as of December 31st, 2021), less than 50% of the population of low-income countries has received the vaccine (in particular, the complete vaccination rate is below 10% in more than fifteen countries in Africa). The urgent need to find a remedy for vaccine inequality [47, 48] has become an even more relevant topic in the still ongoing ‘pandemic era’, since such a situation may slow the economic recovery and threaten the development and diffusion of new variants within the unvaccinated fraction of the world population and, as a consequence, spread over the already vaccinated population [49].
In other words, income inequalities, exacerbated by the COVID-19 pandemic [50], as well as inequalities in the quality of health systems (if any) within and across countries, not only in EMDE (Emerging Markets and Developing Economies) countries [51] but also in Europe [52], can make a difference in terms of the number of individuals vaccinated. People in low-income countries do not get vaccinated not because they do not want to but because in their countries or regions, vaccines are not yet available, there are no health systems or, if there are any, they are very weak. In other words, people who live in EMDE countries have a lower probability of getting vaccinated and, as a result, a higher probability of dying of COVID-19. Furthermore, as an intuitive result [53-55], there is a positive correlation between low vaccination rates and GDP growth rates: low vaccination rates imply low GDP growth rates.
4. Conclusions
Territorial economic conditions are an important key element in explaining the uncertain evolution of the COVID-19 pandemic and the difficulty of solving the ‘to be or not to be’ (pandemic or endemic) Hamletic dilemma. If we consider simultaneously the likely zoonotic and zooanthroponotic origin of the mutations of the virus together with the problem of vaccine inequity, due to economic and health inequalities, the disruption of the global ecosystem as a consequence of human activities, and the ease of spread due to the globalization of international movements of people, we can easily identify fertile soil for the onset of new variants.
The fact that the least vaccinated part of the world is made up for the most part by low-income countries (and in particular subtropical and tropical areas such as Africa, Asia and Latin America (in particular Brazil)) leads to some relevant consequences and obstacles to the transition of COVID-19 from a pandemic to an endemic disease, which is also due to the characteristics of the SARS-CoV-2 virus from which it originates.
References
- World Health Organization Director-General's opening remarks at the media briefing– 14 September 2022: “We have never been in a better position to end the pandemic. We are not there yet, but the end is in sight”. (2022).
- Biancolella, M., Colona, V.L., Mehrian-Shai, R.et al.COVID-19 2022 update: transition of the pandemic to the endemic phase.Hum Genomics16 (2022): 19.
- On the basis of the World Health Organization (W.H.O.) definitio “A SARS-CoV-2VOI(Variant of Interest) is a SARS-CoV-2 variant: a) with genetic changes that are predicted or known to affect virus characteristics such as transmissibility, disease severity, immune escape, diagnostic or therapeutic escape; AND b) that has been identified as causing significant community transmission or multiple COVID-19 clusters, in multiple countries with increasing relative prevalence alongside increasing number of cases over time, or other apparent epidemiological impacts to suggest an emerging risk to global public health.
- A SARS-CoV-2VOC(Variant of Concern) is a SARS-CoV-2 variant that meets the definition of a VOI (see above) and, through a comparative assessment, has been demonstrated to be associated with one or more of the following changes at a degree of global public health significance: a) increase in transmissibility or detrimental change in COVID-19 epidemiology; OR b) increase in virulence or change in clinical disease presentation; OR c) decrease in effectiveness of public health and social measures or available diagnostics, vaccines, therapeutics. See W.H.O. website at: https://www.who.int/news/item/26-11-2021-classification-of-omicron-(b.1.1.529)-sars-cov-2-variant-of-concern
- Lazarus, J.V., Wyka, K., White, T.M.et al.Revisiting COVID-19 vaccine hesitancy around the world using data from 23 countries in 2021Nat Commun13 (2022): 3801.
- Vaccine Hesitancy is defined by the WHO SAGE (i.e. the World Health Organization Strategic Advisory Group for Emergencies - Working Group on Vaccine Hesitancy) as the “delay in acceptance or refusal of vaccination despite availability of vaccination services”. See MacDonald, N. E., SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: definition, scope and determinants. Vaccine 33 (2015): 4161–4164.
- World Health Organization. Ten threats to global health in 2019.
- See the World Health Organization dashboard, available at the link https://covid19.who.int/
- Mahase E Covid-19: What we know about the BA.4 and BA.5 omicron variants 2022.
- Islam S, Islam T, Islam MR. New Coronavirus Variants are Creating More Challenges to Global Healthcare System: A Brief Report on the Current Knowledge. Clin Pathol (2022).
- Ledford H. The next variant: three key questions about what's after Omicron. Nature 603 (2022): 212-213.
- Ghafari M, Liu Q, Dhillon A, Katzourakis A and Weissman DB (2022) Investigating the evolutionary origins of the first three SARS-CoV-2 variants of concern. Front. Virol 2 (2022): 942555.
- Kannan, P. Shaik Syed Ali, A. Sheeza Omicron (B.1.1.529) – variant of concern – molecular profile and epidemiology: a mini review Eur Rev Med Pharmacol Sci 25 (2021): 8019-8022.
- Gowrisankar A, Priyanka TMC, Banerjee S. Omicron: a mysterious variant of concern. Eur Phys J Plus 137 (2022): 100.
- [14] GISAID - Global Initiative on Sharing Avian Influenza Data – “The GISAID Initiative promotes the rapid sharing of data from all influenza viruses and the coronavirus causing COVID-19. This includes genetic sequence and related clinical and epidemiological data associated with human viruses, and geographical as well as species-specific data associated with avian and other animal viruses, to help researchers understand how viruses evolve and spread during epidemics and pandemics.”
- Pfizer and BioNTech Announce Omicron-Adapted COVID-19 Vaccine Candidates Demonstrate High Immune Response against Omicron - Pfizer press release.
- Mallapaty, Smriti. Where did Omicron come from? Three key theories. Nature 602 (2022): 26-28.
- Aleem A, Akbar Samad AB, Slenker AK. Emerging Variants of SARS-CoV-2 and Novel Therapeutics against Coronavirus (COVID-19). 2022 Oct 10. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing (2022).
- Worobey M. et al. The Huanan Seafood Wholesale Market in Wuhan was the early epicenter of the COVID-19 pandemic 377 (2022): 951-959.
- Shi Z, Hu Z. A review of studies on animal reservoirs of the SARS coronavirus. Virus Res 133 (2008): 74-87.
- Pekar JE. et al. The molecular epidemiology of multiple zoonotic origins of SARS-CoV-2 Science 377: 960-966.
- Holmes EC. COVID-19-lessons for zoonotic disease. Science 375 (2022): 1114-1115.
- Sánchez CA, Li H, Phelps KLet al.A strategy to assess spillover risk of bat SARS-related coronaviruses in Southeast Asia.Nat Commun13 (2022): 4380.
- Grange ZL. et al. Ranking the risk of animal-to-human spillover for newly discovered viruses 2021 Proceedings of the National Academy of Sciences 118: e2002324118.
- Parra-Lucares, A.; Segura, P.; Rojas, V.; Pumarino, C.; Saint-Pierre, G.; Toro, L. Emergence of SARS-CoV-2 Variants in the World: How Could This Happen? Life 12 (2022): 194.
- Yang W, Shaman J. COVID-19 pandemic dynamics in India, the SARS-CoV-2 Delta variant and implications for vaccination 2022 Journal of The Royal Society Interface 19 (2022) 20210900.
- Shiehzadegan S, Alaghemand N, Fox M, Venketaraman V. Clinics and Practice 11 (2021): 2039-7283.
- Bian L, Gao Q, Gao F, Wang Q, He Q, Wu X, et al. Impact of the Delta variant on vaccine efficacy and response strategies, Expert Review of Vaccines 20 (2021): 1201-1209.
- Banho CA, Sacchetto L, Campos, GRF,et al.Impact of SARS-CoV-2 Gamma lineage introduction and COVID-19 vaccination on the epidemiological landscape of a Brazilian city.Commun Med2 (2022):
- Duong D. Alpha, Beta, Delta, Gamma: What's important to know about SARS-CoV-2 variants of concern? CMAJ 193 (2021): E1059-E1060.
- Naveca FG. et al. COVID-19 in Amazonas, Brazil, was driven by the persistence of endemic lineages and P.1 emergence. Med(2021).
- Fan Y, Li X, Zhang L.et al.SARS-CoV-2 Omicron variant: recent progress and future perspectives.Sig Transduct Target Ther7 (2022): 141.
- Ledford H. How severe are Omicron infections?Nature600 (2021): 577–578.
- Burki TK. Omicron variant and booster COVID-19 vaccines.Lancet Respir. Med10 (2022): e17.
- Tajudeen YA, Oladunjoye IO, Bajinka O, Oladipo HJ. Zoonotic Spillover in an Era of Rapid Deforestation of Tropical Areas and Unprecedented Wildlife Trafficking: Into the Wild. Challenges 13 (2022): 41.
- Cardinale B, Duffy J, Gonzalez A.et al.Biodiversity loss and its impact on humanity.Nature486 (2012): 59–67.
- Clayton E. et al. Structural Bases of Zoonotic and Zooanthroponotic Transmission of SARS-CoV-2.Viruses14 (2022): 418.
- Bashor L. et al. SARS-CoV-2 evolution in animals suggests mechanisms for rapid variant selection (2021).
- Balasubramaniam KN, Aiempichitkijkarn N, Kaburu SSK.et al.Impact of joint interactions with humans and social interactions with conspecifics on the risk of zooanthroponotic outbreaks among wildlife populations.Sci Rep12 (2022): 11600.
- Delahay RJ, de la Fuente J, Smith GC.et al.Assessing the risks of SARS-CoV-2 in wildlife.One Health Outlook3 (2021): 7.
- Ellwanger, Joel HenriqueandChies, José Artur BogoZoonotic spillover: Understanding basic aspects for better prevention. Genetics and Molecular Biology 44 (2021): e20200355.
- WHO Director-General's opening remarks at the UNGA UNSG-hosted event: “Ending the pandemic through equitable access to COVID-19 vaccines, tests and treatments” – 23 September 2022:” We have never been in a better position to end COVID-19 as a global health emergency, as Prime Minister De Croo of Belgium said. The number of weekly reported deaths is near the lowest since the pandemic began; And two-thirds of the world’s population is vaccinated, including 75% of health workers and older people. But these encouraging global numbers mask disparities that put us all at risk. Only 19% of the populations of low-income countries are vaccinated, compared with 75% in high-income countries. A new report published yesterday by the ACT Accelerator Council highlights falling testing rates globally, virtually non-existent access to new antivirals in most low- and middle-income countries, and outlines what needs to be done to close these gaps. These inequities are not just a risk for those they affect directly; they are a risk for all of us.So closing them is essential if we are to truly end the pandemic”.
- Kavanagh MM, Gostin LO, Sunder M. Sharing Technology and Vaccine Doses to Address Global Vaccine Inequity and End the COVID-19 Pandemic. JAMA 326 (2021): 219-220.
- Priti K, Hassan F, Share vaccine know-how (2021): 374-379.
- World Bank Blog: Uribe JP Supporting vaccine rollout in developing countries December 15 (2021).
- Burki TK. Challenges in the rollout of COVID-19 vaccines worldwide. Lancet Respir Med 9 (2021): e42-e43.
- Efficient remedies to tackle vaccine inequality are represented, as an example, by: a) global solidarity (sharing vaccines among the nations of the world); b) the provision of effective vaccines at very low cost by pharmaceutical multinationals for the less fortunate countries, offsetting the losses with the high profits deriving from rich countries; c) free licening of vaccines.
- Bayati M, Noroozi R, Ghanbari-Jahromi M.et al.Inequality in the distribution of Covid-19 vaccine: a systematic review.Int J Equity Health21 (2022): 122.
- Oehler RL, Vega VR Worldwide vaccine inequality threatens to unleash the next COVID-19 variant, International Journal of Infectious Diseases 123 (2022): 133-135.
- Duffy S. Why are RNA virus mutation rates so damn high? PLoS Biol 16 (2018): e3000003.
- Adarov A. Global income inequality and the COVID-19 pandemic in three charts 2022 (Feb. 07) World Bank Blogs, Published on Let’s Talk Development (2022).
- Bandyopadhyay S,Vadlamannati K. (Editors) Special Issue: Long run effects of Covid-19 on developing countries, Journal of International Development 34 (2022).
- González Rodríguez, I Pascual Sáez, M Cantarero Prieto, D. Have Health Inequalities Increased during the COVID-19 Pandemic? Evidence from Recent Years for Older European Union Citizens. Int. J. Environ. Res. Public Health 19 (2022): 7812.
- Suárez-Álvarez A, López-Menéndez AJ. Is COVID-19 vaccine inequality undermining the recovery from the COVID-19 pandemic? J Glob Health 12 (2022): 05020
- Impact of vaccine inequity on economic recovery – Global Dashboard for Vaccine Equity Archive – Data Futures Platform UNPD Feb (2022).
- Abir T, Al Mamun A, Zainol NR, Khanam M, Haque MR, Milton AH, Agho KE. A Global Study on the Correlates of Gross Domestic Product (GDP) and COVID-19 Vaccine Distribution. Vaccines 10 (2022): 266.