Overcoming the Challenges of Complementary Feeding and the Potential Role of Fortified Infant Cereals: A Position Paper from India and Nepal
Article Information
Complementary Feeding Consortium, Ganesh Kulkarni1*, Madhumita Dobe2, M D Ravi3, Rahul Verma4, Shantanu Dutt5, Soumitra Dutta6, Sunil Sehgal7
1Sanjeevani Children’s Hospital, Aurangabad, Maharashtra, India
2Department of Health Promotion and Education, AIIH and PH, Kolkata, West Bengal, India
3JSS Medical College, Mysuru, Karnataka, India
4Sir HN Reliance Foundation Hospital, Mumbai, Maharashtra, India
5Dutt Children Hospital, Moradabad, Uttar Pradesh, India
6Bhagirathi Neotia Woman and Child Care Centre, Kolkata, West Bengal, India
7Dr. Sehgal's Clinic, New Delhi, India
*Corresponding Author: Ganesh Kulkarni, Sanjeevani Children’s Hospital. Flat no. 14/15, Kushal Nagar, Jalna Road, Aurangabad, Maharashtra, India.
Received: 14 June 2023; Accepted: 25 July 2023; Published: 14 August 2023
Citation:
Complementary Feeding Consortium, Ganesh Kulkarni, Madhumita Dobe, M D Ravi, Rahul Verma, Shantanu Dutt, Soumitra Dutta, Sunil Sehgal. Overcoming the Challenges of Complementary Feeding, and the Potential Role of Fortified Infant Cereals: A Position Paper from India and Nepal. Journal of Pediatrics, Perinatology and Child Health. 7 (2023): 142-158.
View / Download Pdf Share at FacebookAbstract
The last National Family Health Survey, 2019–2021, suggests suboptimal infant feeding practices and an increasing burden of micronutrient deficiencies across the country’s states. The research has well established an association of child nutrition with eating habits and health outcomes in later life. The latest National Family Health Survey-5 data state that only about 4 of every 10 infants are introduced solid foods timely i.e., introduced to complementary feeding as per the recommended age. It is equally worrisome to note that only 11.1% of all children in India in the age-group of 6–23 months were fed the minimum acceptable diet with a direct correlation of around 67.1% of children under the age of 5 years suffering from anemia. These findings highlight that incorrect timing of initiation of complementary foods, early or delayed, and inadequate nutrition are a few critical factors behind the prevalence of nutrient deficiencies. In this regard, a group of experts from the field of pediatric nutrition from different parts of India and Nepal gathered and acknowledged that in addition to lack of knowledge on ageappropriate nutrition to infants, cultural beliefs, traditions, myths, and lack of awareness about nutrient enhancers and inhibitors are some of the common challenges in meeting age-appropriate nutrition. The expert group also recognized that supplementation and fortification co-exist in the clinical practice where supplementation is offered on a case-to-case basis to address the therapeutic needs of micronutrient deficiencies. In contrast, fortification should be advised as part of a balanced diet to reduce the risk of micronutrient deficiencies. However, it was unanimously agreed that scientific research and clinical practice have established that fortification or the use of Fortified Infant Cereals (FIC) to have better compliance and suggests this as a strategy to be used as a preventive, long-term sustainable mass approach to partner with homemade feeds for meeting the nutritional needs during the critical period of 6–23 months of age.
The present position paper captures the opinion and suggestions of a group of clinicians regarding the pervasive concerns and challenges of complementary feeding in a diverse country like India with varied cultural and eating preferences. Further, the role of FIC is also discussed as a strategy to consider supporting age-appropriate nutrition in the country irrespective of its diversity.
Keywords
Complementary feeding; 6-23 months; Undernutrition; Micronutrient deficiency; Iron deficiency anemia; Position paper; India; Nepal; Fortified infant cereals; Dietary diversity; Meal frequency; Ageappropriate nutrition; Feed texture
Children’s articles Children’s Research articles Children’s review articles Children’s PubMed articles Children’s PubMed Central articles Children’s 2023 articles Children’s 2024 articles Children’s Scopus articles Children’s impact factor journals Children’s Scopus journals Children’s PubMed journals Children’s medical journals Children’s free journals Children’s best journals Children’s top journals Children’s free medical journals Children’s famous journals Children’s Google Scholar indexed journals Breast-Feeding articles Breast-Feeding Research articles Breast-Feeding review articles Breast-Feeding PubMed articles Breast-Feeding PubMed Central articles Breast-Feeding 2023 articles Breast-Feeding 2024 articles Breast-Feeding Scopus articles Breast-Feeding impact factor journals Breast-Feeding Scopus journals Breast-Feeding PubMed journals Breast-Feeding medical journals Breast-Feeding free journals Breast-Feeding best journals Breast-Feeding top journals Breast-Feeding free medical journals Breast-Feeding famous journals Breast-Feeding Google Scholar indexed journals Toddler articles Toddler Research articles Toddler review articles Toddler PubMed articles Toddler PubMed Central articles Toddler 2023 articles Toddler 2024 articles Toddler Scopus articles Toddler impact factor journals Toddler Scopus journals Toddler PubMed journals Toddler medical journals Toddler free journals Toddler best journals Toddler top journals Toddler free medical journals Toddler famous journals Toddler Google Scholar indexed journals Multi-micronutrient deficiencies articles Multi-micronutrient deficiencies Research articles Multi-micronutrient deficiencies review articles Multi-micronutrient deficiencies PubMed articles Multi-micronutrient deficiencies PubMed Central articles Multi-micronutrient deficiencies 2023 articles Multi-micronutrient deficiencies 2024 articles Multi-micronutrient deficiencies Scopus articles Multi-micronutrient deficiencies impact factor journals Multi-micronutrient deficiencies Scopus journals Multi-micronutrient deficiencies PubMed journals Multi-micronutrient deficiencies medical journals Multi-micronutrient deficiencies free journals Multi-micronutrient deficiencies best journals Multi-micronutrient deficiencies top journals Multi-micronutrient deficiencies free medical journals Multi-micronutrient deficiencies famous journals Multi-micronutrient deficiencies Google Scholar indexed journals Breast milk articles Breast milk Research articles Breast milk review articles Breast milk PubMed articles Breast milk PubMed Central articles Breast milk 2023 articles Breast milk 2024 articles Breast milk Scopus articles Breast milk impact factor journals Breast milk Scopus journals Breast milk PubMed journals Breast milk medical journals Breast milk free journals Breast milk best journals Breast milk top journals Breast milk free medical journals Breast milk famous journals Breast milk Google Scholar indexed journals Food fortification articles Food fortification Research articles Food fortification review articles Food fortification PubMed articles Food fortification PubMed Central articles Food fortification 2023 articles Food fortification 2024 articles Food fortification Scopus articles Food fortification impact factor journals Food fortification Scopus journals Food fortification PubMed journals Food fortification medical journals Food fortification free journals Food fortification best journals Food fortification top journals Food fortification free medical journals Food fortification famous journals Food fortification Google Scholar indexed journals Child nutrition articles Child nutrition Research articles Child nutrition review articles Child nutrition PubMed articles Child nutrition PubMed Central articles Child nutrition 2023 articles Child nutrition 2024 articles Child nutrition Scopus articles Child nutrition impact factor journals Child nutrition Scopus journals Child nutrition PubMed journals Child nutrition medical journals Child nutrition free journals Child nutrition best journals Child nutrition top journals Child nutrition free medical journals Child nutrition famous journals Child nutrition Google Scholar indexed journals Obese children articles Obese children Research articles Obese children review articles Obese children PubMed articles Obese children PubMed Central articles Obese children 2023 articles Obese children 2024 articles Obese children Scopus articles Obese children impact factor journals Obese children Scopus journals Obese children PubMed journals Obese children medical journals Obese children free journals Obese children best journals Obese children top journals Obese children free medical journals Obese children famous journals Obese children Google Scholar indexed journals Preschool-aged children articles Preschool-aged children Research articles Preschool-aged children review articles Preschool-aged children PubMed articles Preschool-aged children PubMed Central articles Preschool-aged children 2023 articles Preschool-aged children 2024 articles Preschool-aged children Scopus articles Preschool-aged children impact factor journals Preschool-aged children Scopus journals Preschool-aged children PubMed journals Preschool-aged children medical journals Preschool-aged children free journals Preschool-aged children best journals Preschool-aged children top journals Preschool-aged children free medical journals Preschool-aged children famous journals Preschool-aged children Google Scholar indexed journals Overweight articles Overweight Research articles Overweight review articles Overweight PubMed articles Overweight PubMed Central articles Overweight 2023 articles Overweight 2024 articles Overweight Scopus articles Overweight impact factor journals Overweight Scopus journals Overweight PubMed journals Overweight medical journals Overweight free journals Overweight best journals Overweight top journals Overweight free medical journals Overweight famous journals Overweight Google Scholar indexed journals Iron deficiency anemia articles Iron deficiency anemia Research articles Iron deficiency anemia review articles Iron deficiency anemia PubMed articles Iron deficiency anemia PubMed Central articles Iron deficiency anemia 2023 articles Iron deficiency anemia 2024 articles Iron deficiency anemia Scopus articles Iron deficiency anemia impact factor journals Iron deficiency anemia Scopus journals Iron deficiency anemia PubMed journals Iron deficiency anemia medical journals Iron deficiency anemia free journals Iron deficiency anemia best journals Iron deficiency anemia top journals Iron deficiency anemia free medical journals Iron deficiency anemia famous journals Iron deficiency anemia Google Scholar indexed journals Breastfed infants articles Breastfed infants Research articles Breastfed infants review articles Breastfed infants PubMed articles Breastfed infants PubMed Central articles Breastfed infants 2023 articles Breastfed infants 2024 articles Breastfed infants Scopus articles Breastfed infants impact factor journals Breastfed infants Scopus journals Breastfed infants PubMed journals Breastfed infants medical journals Breastfed infants free journals Breastfed infants best journals Breastfed infants top journals Breastfed infants free medical journals Breastfed infants famous journals Breastfed infants Google Scholar indexed journals Minimum meal frequenc articles Minimum meal frequenc Research articles Minimum meal frequenc review articles Minimum meal frequenc PubMed articles Minimum meal frequenc PubMed Central articles Minimum meal frequenc 2023 articles Minimum meal frequenc 2024 articles Minimum meal frequenc Scopus articles Minimum meal frequenc impact factor journals Minimum meal frequenc Scopus journals Minimum meal frequenc PubMed journals Minimum meal frequenc medical journals Minimum meal frequenc free journals Minimum meal frequenc best journals Minimum meal frequenc top journals Minimum meal frequenc free medical journals Minimum meal frequenc famous journals Minimum meal frequenc Google Scholar indexed journals Healthcare articles Healthcare Research articles Healthcare review articles Healthcare PubMed articles Healthcare PubMed Central articles Healthcare 2023 articles Healthcare 2024 articles Healthcare Scopus articles Healthcare impact factor journals Healthcare Scopus journals Healthcare PubMed journals Healthcare medical journals Healthcare free journals Healthcare best journals Healthcare top journals Healthcare free medical journals Healthcare famous journals Healthcare Google Scholar indexed journals Child care articles Child care Research articles Child care review articles Child care PubMed articles Child care PubMed Central articles Child care 2023 articles Child care 2024 articles Child care Scopus articles Child care impact factor journals Child care Scopus journals Child care PubMed journals Child care medical journals Child care free journals Child care best journals Child care top journals Child care free medical journals Child care famous journals Child care Google Scholar indexed journals
Article Details
Abbreviations:
CF: Complementary Feeding; EBF: Exclusive Breast-Feeding; FIC: Fortified Infant Cereal; FITS: Feeding Infant and Toddler Study; HCP: Health Care Practitioner; IDHS-17: The Indonesia Demographic and Health Survey 2017; IFLS: Indonesia Family Life Survey (IFLS); IFPS II: Infant Feeding Practices Study II; IYCF: Infant and Young Child Feeding; LMICS: Low- and Middle-Income Countries; MAD: Minimum Acceptable Diet; MDD: Minimum Dietary Diversity; MICS: Multiple Indicator Cluster Survey; MMF: Minimum Meal Frequency; MNDS: Micronutrient Deficiencies; NDHS: Nepal Demographic and Health Survey; NFHS: National Family Health Survey; RCTS: Randomized Controlled Trials; UNICEF: United Nations International Children's Emergency Fund
1. Introduction
The rapid growth of the infant during the first two years of life increases the demand for iron and other micronutrients much more than that required at any other developmental stage [1-4]. Breast milk alone cannot fulfill this increased demand after 6 months of age. Therefore, timely age-appropriate Complementary Feeding (CF) plays a vital role in fulfilling this increased micronutrient demand [1,3,4]. The World Health Organization (WHO) defines CF as “the process starting when breast milk alone is no longer sufficient to meet the nutritional requirements of infants” so that “other foods and liquids are needed, along with breast milk” [2]. The WHO and the United Nations International Children's Emergency Fund (UNICEF) recommend Exclusive Breast-Feeding (EBF) for the first 6 months, followed by the introduction of CF along with continued breast-feeding up to the age of 2 years and beyond [4].
The role of CF is to provide vital nutrients, the in-utero stores of which get depleted by 4 to 6 months of life [4]. Given the importance of CF, globally the WHO, and nationally the Indian and Nepal ‘Infant and Young Child Feeding’ (IYCF) practices provide guidelines and recommendations for frequency, consistency, composition and quantity of CF [5-7]. Government of India in its nationwide program- ‘Mother’s Absolute Affection’ of Ministry of Health and Family Welfare, also provides information and conduct various activities for capacity building in communities regarding the importance of introduction of complementary foods after 6 months of age in addition to breastfeeding.
In addition to practicing ideal complementary feeding, the WHO also recommends fortified CF and micronutrient powders as a strategy to risk reduction of MNDs and undernutrition in 6–23-month-olds [8]. However, CF practices are often inadequate and age inappropriate especially in developing countries like India and Nepal [7,9-13].
Inadequate and age-inappropriate CF practices is one of the known causes of Micronutrient Deficiencies (MNDs) in 6–23-month-olds [2,9,14-16]. Deficiencies of iron, zinc, iodine, folate, vitamin A, vitamin B12 and vitamin D are prevalent due to inadequate or inappropriate diet being fed to 6-23 month olds [17].
MNDs in infants cause both short-term and long-term impacts on growth, cognitive, metabolic, and social development, and are associated with frequent illness and lack of energy as well [11,12]. The deficiency of one micronutrient is a proxy for multi-micronutrient deficiencies. Understanding the micronutrients’ deficit in the diet during the complementary feeding period is vital for addressing undernutrition-related growth impairments. Many of these impacts cannot be reversed even after providing nutritionally adequate CF [12,15]. But are largely preventable. The early identification of complementary feeding gaps is vital for an intervention to ensure adherence to the guidelines, recommendations, policies and programs intended to improve child health and nutrition [18,19].
The government of India and Nepal have launched many programs to combat malnutrition such as food fortification, micronutrient supplementation, promoting dietary diversification, nutritional education, and environmental sanitation and hygiene due to the high prevalence of MNDs in 6-23 month olds in these countries which has worsened from NFHS-4 to NFHS-5 [7,15].
India and Nepal’s education, income and social environment are rapidly changing. There is a trend towards increased family income, nuclear families, working mothers, increased access to information due to internet etc. Hence, there was a need to understand the current challenges around attaining adequate CF and the potential role of Fortified Infant Cereal (FIC) in addition to homemade food in providing a nutritionally adequate and age-appropriate CF.
2. Methodology
Four expert group meetings were conducted region-wise (East, West, North, and South) in India from October 2022 to December 2022. Each meeting was attended by 12-15 expert pediatricians from that region. Eight pediatricians from Nepal also participated in the North zone meeting.
Under five child nutrition and CF data (6–23-month-olds) from WHO, UNICEF, National Family Health Survey (NFHS-5) pan-India and regional data, and Nepal Demographic and Health Survey (NDHS) 2022 was presented at the regional meetings along with the available scientific evidence from clinical trials, guidelines, systematic reviews and meta-analysis, IYCF practices, reviews, and other literary sources.
The participants discussed the scientific evidence and added their clinical experience to suggest solutions for some vital and practical questions around barriers and challenges to appropriate CF in their regions and the potential role of FIC in partnering along (i.e., in addition to) with homemade food in providing a nutritionally adequate and age-appropriate CF. The suggestions on which majority of the experts agreed upon were taken as the recommendations from this expert group, which could act as a reference for the clinical practice dealing with similar challenges regarding CF practices.
Overview of the problem statements and the expert recommendations
An overview of the problem statements discussed during the four meets and a solution to mitigate these problems. However, the experts concur that though these scientific shreds of evidences and recommendations can act as guiding principles for CF and the role of FIC, every infant for whom these recommendations are applicable should also receive individualized care and nutritional counselling.
Problem Statement 1: Anemia and Micronutrient Deficiencies are Prevalent in 6-23 Month-Olds in India and Nepal
MNDs are globally prevalent in children under 5 years. MNDs have a direct association with stunted, wasted, and obese children [14]. The WHO statistics show that 45% of deaths in children aged <5 years are linked to undernutrition [20]. This means that almost half the children under five who die could have survived if they were properly nourished.
Population-based surveys show that over half (56%) of preschool-aged children worldwide have MNDs, and three-fourth of these children with MNDs live in South Asia [21]. One in two children under five years in South Asia is either wasted, overweight, and/or stunted [7]. A survey of 490 pediatricians in India found that 94% saw MNDs in 2-6 year olds visiting their outpatient clinics [14].
The NFHS-5 (2019-2021) data showed that 67.1 percent of children (of age group 6-59 months) had anemia, an increase from 58.5% which was seen in NFHS-4 (2015-2016) (Figure 1) [22].
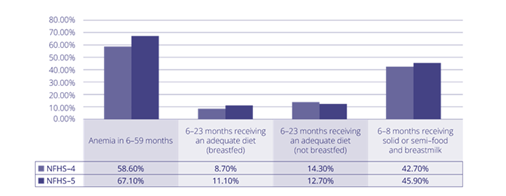
Figure 1: Nutrition status of infants in India
NFHS-5: National Family Health Survey-5 [22].
The most common MNDs seen in this age group are the deficiencies of iron, iodine, folate, zinc, vitamin A, vitamin B12 and vitamin D [17,23]. Globally, iodine, iron and vitamin A are considered vital micronutrients in Low-and-Middle Income Countries (LMIC) for the health of under five years as their deficiency affects 42% of children <5 years [20].
Recommendation 1: Starting the complementary feeding at the right time is critical and crucial to meet the increased nutrient and energy demand beyond 6 months of age
The 6-23 months window is a time of accelerated growth, with the need for age-appropriate nutrients and energy exceeding what can be provided by breast milk alone. This period carries the highest risk of growth faltering in children from Low- and Middle-Income Countries (LMICs) [23]. The occurrence of stunting in 6-month olds is correlated with inappropriate CF practices [15].
An Italian Expert Consensus on CF noted that Iron Deficiency Anemia (IDA) is common from one year of age or earlier and is an indicator of the inadequacy of CF [1]. A systematic review of nine studies (which also included Randomized Controlled Trials [RCTs]) found strong evidence suggesting that iron and zinc containing CF (e.g., meat, fortified infant cereals) initiated in breastfed infants helped in maintaining adequate iron and zinc status and thus preventing their deficiency during the first year of life [24].
The experts opined that it is a known and proven fact that breastfeeding beyond six months alone is insufficient to meet the growing infants’ nutrient and energy requirements. Undoubtedly, CF is critical to meet these nutrient and energy demands. Fortified infant cereals have a decisive role when partnered with home-made preparations, which can support in bridging the nutrient gap, ensuring an age-appropriate nutrition in the critical growth period of 6-23 months.
Problem Statement 2: Complementary Feeding is Not Initiated on Time, is Age-Inappropriate and Nutritionally Inadequate in 6-23 Month-Olds
The WHO and UNICEF have four indicators for the adequacy of CF: timely introduction (INTRO), Minimum Meal Frequency (MMF), Minimum Dietary Diversity (MDD), and Minimum Acceptable Diet (MAD) (Figure 2) [25,26]. Further, the feed should be of adequate consistency, texture and hygienically prepared and served [26].
The NFHS-5 data (Figure 1) showed inadequate and age-inappropriate CF trends persisting in <5 year olds [22]. Only 45.9% of infants aged 6-8 months received solid or semi-solid food along with breast milk; only 11.1% of 6-23 month olds received adequate diet (MAD) [22].
Evidence from South Asia (including India and Nepal) shows that in addition to CF not being starting at the recommended time of around 6 months, it does not meet the MDD and MMF or MAD standards leading to an increased risk of wasting and stunting in 6–23-months-old [7,9]. This occurs due to inadequate awareness regarding appropriate CF practices, incorrect perceptions and beliefs and due to sub-optimal counselling by healthcare professionals (HCPs) [11].
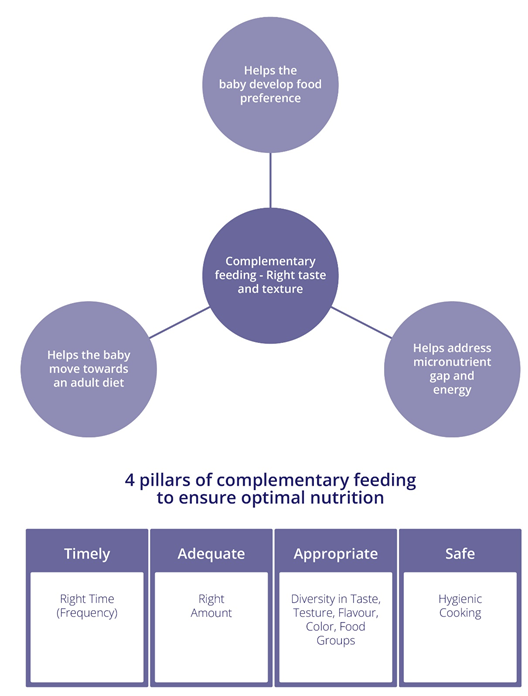
Figure 2: Four pillars of complementary feeding [26].
A community-based cross-sectional study from Nepal showed that 19% of infants were given CF feed at the WHO-UNICEF recommended time (around 6 months); 46% received CF at 4-5 months; and 35% received CF much before the recommended age [10]. The energy intake by the infants was as per the WHO recommended standard; 84% of the infants received processed food as a part of CF to achieve the energy requirements [10]. The Nepal Multiple Indicator Cluster Survey (MICS) showed that 69% of children aged 6-23 months receive the recommended MMF; 40 % received MDD and 30% received MAD [27].
A survey of pediatricians from India showed that 97% of the pediatricians believed that MNDs were caused by “not eating a balanced diet” [14].
Recommendation 2: Complementary feeding should be on the concept of ‘starting right’, which is, it should be started around 6 months of age, and continued until 2 years; breastfeeding should continue during this period
After the first 6 months of life, a child’s nutritional requirements and limited gastric capacity, accentuate the importance of providing nutrient-dense feeds. A systematic review of 33 studies concluded that it is difficult to pinpoint the exact and ideal time for starting CF as some infants benefit from the introduction of CF at 6 months while others may require earlier initiation of CF to meet the nutritional requirements [28]. Early introduction of CF, before the infant is developmentally ready for it, can result in issues such as allergy, choking hazard, diarrhea from food contamination, etc. [3,28]. On the other hand, delaying CF, beyond 6 months, can miss the developmentally ready window of opportunity and add a risk of MNDs and thereby growth faltering [3,28].
An assessment of the national IYCF recommendations on the timing of CF from 34 member states of the WHO European region found that 74% of countries recommended that 6 months is the ideal age to start CF while 18% recommended beginning at 4 months and 9% at 5 months [4]. Notably, the WHO and Indian Academy of Paediatrics (IAP) Infant and Young Child Feeding Guidelines call out that the initiation of CF should be around 6 months of age [5]. Analysis of the Infant Feeding Practices Study II (IFPS-II) showed that the infants were at greater risk of poor health if introduced to CF before 4 to 6 months [29].

Figure 3: Feeding cues that show that the infant is developmentally ready for complementary feeding [26,70].
The experts concurred with the recommendation by IAP and WHO. They opined that the initiation of CF should occur around 6 months of age. If the mother is healthy, is producing adequate milk, is available for breastfeeding on demand, and has a full-term baby doing well, then exclusive breastfeeding should be continued until 6 months of age. However, if the baby is lagging on its growth curve and is developmentally ready (exhibits feeding cues (Figure 3)) or if the mother’s milk is not adequate to meet the nutrition and growth requirements of the baby, beginning CF earlier could be assessed and weighed from the risk-benefit aspect.
Recommendation 3: Dietary diversity is a critical, essential, crucial and sustainable approach towards nutritionally adequate complementary feeding
According to WHO-UNICEF, an infant has MDD, if the infant consumes at least four of the seven food groups daily (Figure 4) [9,30]. MDD ensures micronutrient density in an infant’s diet [9]. However, lack of dietary diversity appears to be a significant challenge during the CF period in South Asia [7,31].
A systematic review and meta-analysis of eight RCTs showed that animal-source foods were the most suitable CF to improve growth in 6 to 23-month-old children in LMICs [32]. On the other hand, another systematic review of studies exploring a vegetarian/vegan CF concluded that only vegetarian/vegan diet carries high risk of critical micronutrient deficiencies and risk of growth retardation [33].
The IYCF practices encourage offering foods of all tastes, including bitter taste, as part of the CF [5-7]. This is to leverage the window of flavor bridging between 6-12 months of age. The varied flavors introduced during this age (6-9 months) have shown to have better acceptability in later childhood. Exposure to various flavor and textures ensures development of taste for food items, which most children reject, also help in achieving MDD.
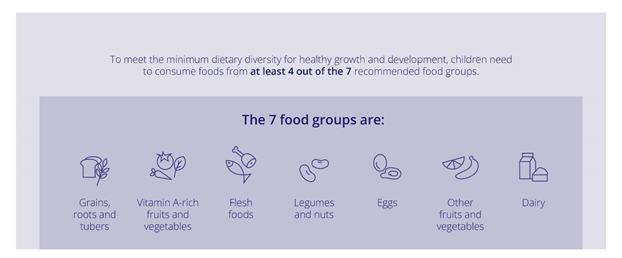
Figure 4: Dietary diversity 6-23 month olds: including 4 out of 7 food groups [65].
National surveys and scientific papers have shown that dietary diversity has been linked to adequate nutrition and reduced risk of stunting, wasting and underweight [9,34,35]. However, national and regional food group data from India shows that infants not achieving MDD are less likely to consume iron and vitamin A-rich vegetables and fruits and flesh foods [9]. There are many clusters in India where infants do not get dietary diversity from grains, roots, and tubers, dairy, nuts and legumes, and vegetables and fruits including those rich in iron and vitamin A [9]. These children are more likely to be at higher risk of micronutrient deficiencies which may manifest as stunting, wasting and being underweight [35].
A longitudinal cohort study from Nepal found that CF composed of animal-source food, vegetables and fruits, thereby meeting MDD requirements, was associated with a significant reduction in neurodevelopmental deficits and growth faltering [36].
Expert opinion
Most food items given to Indian and Nepalese infants are from grains, roots, or tubers such as dalia, ragi, kheer, and rice, which are rich in carbohydrates. Some of the wrong food choices find their way into an infants’ diet earlier than expected e.g. biscuits or biscuits dissolved in water or milk and made as feed. The expert group acknowledged that mostly the feed offered to infants might be energy sufficient but are nutrient-poor. Also, feed containing varied food groups are often given less. When diversity does not exist across the food items, it fails to meet the required nutritional demand. A diet deficient in variety can surge the risk of micronutrient deficiencies, which may have a detrimental outcome on children’s physical and cognitive development. The feed which are nutrient dense and energy dense should thus be provided during CF period. Studies have yielded that little or no consumption of nutrient-dense foods, such as foods from animal-source, eggs, dairy products, fruits, and vegetables, between 6 months and 23 months of age is associated with stunting. The prevalence of stunting increases rapidly between 12-23 months of age, when the focus on complementary feeding is reduced and an infant is offered food from the family bowl, made for an adult but given in lesser quantity. Often mothers and caregivers lack an understanding of preparing age-appropriate feed for infants. The clinician and pediatrician fraternity should advocate active counselling, conversations and generating awareness of the preparation of such feed. In cases with high predisposition of risk of MNDs or where the feeds are prepared from only staples, fortified infant cereals could be considered a strategy to partner along with home-made preparation. This could ensure bridging any gap due to a lack of understanding of recommended CF practices.
Recommendation 4: Complementary feeds should have age-appropriate frequency, consistency, portion size, texture, palatability, energy and nutrient density to ensure nutritional adequacy
A systematic review concluded that infants become accustomed to different food groups through four processes: familiarization; observational learning; associative learning; and categorization of food [37]. Infants should be made familiar with one type of food through repeated exposure to its taste, texture or appearance [37]. Infants should be offered one flavor at a time to familiarize themselves. Infants should be offered a food for 8-10 times before concluding their dislike towards it. The introduction of potentially allergenic foods (e.g., eggs, fish, peanuts, seeds etc.) is influenced by the quantity of allergen and the degree of cooking with the probability of an allergic reaction. The introduction of these allergens to a low-risk infant should be initiated with a small quantity of the food and then gradually increase the quantity. The introduction of these allergens to high-risk allergic reaction should be clinically assessed.
The infant adapts to different food flavors through associative learning and learns to eat what others eat through observational learning. An infant’s willingness to consume food depends on the ability to recognize and categorize the items on the plate [37].
The IYCF practices provide details for age-appropriate frequency, consistency, quantity and composition of CF (Table 1) [5-7]. Achieving MDD is a proxy for nutrient density, which confirms foods of different color, palatability and texture are included in the diet [5,7-9].
|
6-9 months |
9-12 months |
12 to 23 months |
|
|
Food |
Thick porridge; fruit and dark green vegetables, rich in vitamin A and iron; and animal source foods (meat, fish, eggs, and curd or other dairy products) |
Fruit and dark green vegetables, rich in vitamin A and iron; and animal source foods |
Greater variety of fruit and dark green vegetables, rich in vitamin A and iron; and animal source foods |
|
Quantity, how much at each meal |
Start with 2-3 spoons increase to 1/2 Katori of food |
1/2 katori |
3/4 katori |
|
Frequency, how often meals provided |
2 to 3 meals each day |
3 or 4 meals each day |
3 or 4 meals each day |
|
Snacks (ready to eat foods: banana, and other fruits; other items like panjeeri, laddoo, halwa, upma, idli, poha etc. |
1 or 2 snacks |
1 or 2 snacks |
1 or 2 snacks |
|
Consistency, how it is prepared for a child to eat |
A mashed texture, thick consistency that stays on the spoon |
Mashed or finely chopped; some chewable items that the child can hold |
Mashed or chopped; some things the child can hold |
Table 1: Fulfilling nutritional needs as the infant grows.
Experience with food texture is linked to the development of a child’s oro-motor skills which continues to develop with age during the CF period. Age-appropriate exposure to textured food items facilitates the acceptance of more complex textures and easy acceptance of family foods, later [38,39]. A longitudinal study accessed 6 to 18 month olds’ acceptance (ability to process and swallow a food) and feeding behaviors (sucking and chewing) for each food texture [39]. Pureed textures were highly accepted at 6 months while soft cooked pieces were highly accepted at 8 months. More complex and coarser textures were increasingly accepted as age increased and the chewing behavior improved, such that most food textures were accepted at 12 months. Further, raw vegetable pieces and foods were increasingly accepted up to 18 months of age [39].
A large survey-based study (n=2999 mothers) reported that an infant’s ability to eat foods without difficulty increased with age [38]. The global food texture score was positively associated with exposure to soft small pieces for 6 months while hard/large pieces, and multiple textures in 6-29 month olds, and negative association with exposure to purees in 9-36-months-old [38].
Expert opinion
It has been underlined that the gaps during the complementary feeding period are mostly recognized as poor dietary quality, poor feeding practices, or both. Food consistency (Figure 5) and portion size (Figure 6) are essential as young infants have limited gastric capabilities and are not equipped to handle a large volume of foods [26]. There is a need to provide energy-dense foods that are easily digestible and readily metabolized. However, often complementary foods have nutrient imbalance, inadequate dietary diversity, thin consistency, insufficient micronutrient content and may lack age-appropriate feed textures.
Recommendation 5: Fortified infant cereals (FIC) in partnership along with homemade preparations can be a routine and sustainable strategy for combating micronutrient deficiencies
There is abundant scientific evidence proving the role of multi-nutrient fortification and FIC in improving the nutritional status, physical and neurocognitive development of 6-23 month olds [23,40-47]. Though iron is an important micronutrient for cognitive, motor, social-emotional and neurophysiological development, multinutrient fortification is more effective strategy to combat the risk of iron deficiency under-five year olds as it counters the risk of multiple deficiencies through a single strategy or intervention [40,44,47]. Further the Indian government is focused on improving undernutrition by fortifying foods with essential micronutrients such as iodine, iron, folic acid, vitamin B12, vitamin A and vitamin D [15].
A systematic review of 15 studies from India confirms that infants receiving only locally available foods fulfill the protein requirement of 6-23 month olds, however, the overall nutrition remined deficient in iron, calcium, vitamin B12 and zinc [40]. Locally available foods were often associated with deficiency of specific nutrients like vitamin A, vitamin C, thiamine, riboflavin, niacin, folate and energy. When these diets were modelled using mathematical models, it was found that modifying them could meet most of the nutritional requirements of 6-23 month olds [40]. However, the systematic review concluded that cost-effective modification of locally available foods is required to overcome iron and zinc deficiencies [40].
Another systematic review and meta-analysis of 18 trials (n=5468 children; mean hemoglobin values: 9.0 to 12.6 g/dL) showed that fortification of milk and cereals with iron plus other micronutrients was a more effective strategy for improving hematologic outcomes than fortification with only iron [44]. The authors concluded that in developing countries multi-micronutrient fortified milk and infant cereal products could be an effective option to reduce anemia in children ≤3 years [44].
Another systematic review and meta-analysis found moderate-certainty evidence from six trials (n=1209) that FIC consumption in 6–23-months-old reduced the risk of anemia with higher hemoglobin concentrations and serum ferritin versus those who did not receive FIC [42].
The Feeding Infant and Toddler Study (FITS) study showed that infant cereal was one of the richest dietary iron sources for infants aged 6-12 months. The FITS study also showed that the dependence on infant cereals decreased as the age progressed: infant cereal was consumed by 74.6% of infants aged 6-8.9 months, 51.5% of those aged between 9-11.9 months and 14.8% among 12-17.9-months-old [43]. Similarly, two double-blinded, cluster-randomized, controlled trials (Cameroon Study and Ghana study) showed that daily intake of micronutrient-FIC for 6 months significantly improved hemoglobin and iron status in children and significantly decreased the prevalence of anemia, iron deficiency, and IDA as compared to infants who did not receive micronutrient-FIC [41,45].

Figure 5: Food consistency 6 months to 2 years [26].
Analysis of the data from the Indonesia Family Life Survey (IFLS) and the Indonesia Demographic and Health Survey 2017 (IDHS-17) showed that the iron deficiency and IDA was significantly lower in 6–23-month-olds who consumed FIC versus those who did not [46]. The multicenter study in Indian infants found that consuming micronutrient-FIC for 6 months improved the iron status (hemoglobin and serum ferritin), superior neurodevelopmental scores and lower risk of iron deficiency and IDA [47]. The authors of all the above studies concluded that fortified infant cereals should be considered as part of a sustainable strategy to partner daily balanced diet in infants (Figure 7).
Usually FIC consumption is associated with high concerns regarding excessive weight gain and obesity [49]. The evidence established in studies from Ghana and India showed that the FIC and non-FIC groups showed no significant difference in weight gain over the six months [45,47]. A systematic review of 49 articles also found no evidence of unfavorable influence of FIC on size, body composition, and weight and no association with overweight/obesity [48].

Figure 6: Food adequacy/portion size 6-23 months [26].

Figure 7: Iron bioavailability [18,66-69].
Expert opinion on how to encourage fortification and explain the role of fortified infant cereal
- The experts suggest that the approach of “vocal about the local” should be the way and should emphasize locally available and seasonal foods as they are cheaper and nutrient dense. Every interaction with mothers and caregivers should be seen as an opportunity to generate awareness on providing nutrient dense, diverse and energy dense feeds to infants during CF. FIC can be added as one or two meals during the diet to compensate for the nutritionally inadequate complementary feeds arising from the lack of knowledge on ideal CF practices.
- Advice on food processing techniques and food cooking methods should be provided to caregivers as processes like fermentation, soaking, germination, and sprouting increases the nutrient density of the feeds.
- For infants who are lagging behind their growth curve on homemade CF made up of ONLY from staples, or are provided only vegetarian feeds due to regional or cultural preference, or for working mothers, multinutrient-FIC in partnership with homemade food can be an effective and sustainable strategy as multinutrient-FIC are scientifically formulated to meet age-appropriate daily nutrient requirements (especially iron, vitamin A, vitamin B12, zinc, and calcium) and are a source of high bioavailable nutrients in the right combinations.
- Requirements of critical nutrients like iron and zinc are multifold during CF period and any insufficiency of these nutrients will have short- and long-term impact which could be irreversible. It is essential to highlight that only vegetarian diet and lack of nonheme food sources can increase the IDA burden, therefore, all the strategies should be drafted to ensure the sufficiency of the critical nutrients. Iron supplementation is a routine practice to ensure iron store sufficiency. Supplementation as a blanket ‘one-size-fits all’ approach does not work well. Supplementation should be reserved for cases where therapeutic approach to iron deficiency or anemia is to be taken. The challenges of palatability, constipation, adherence to prescription, and compliance with consumption associated with supplementation, make the success of this approach questionable for all. As a mass approach, fortification or FIC should be considered as it is not associated with the challenges mentioned earlier. It is a sustainable strategy that does not involve a change in the daily behavioral pattern. The choice of FIC or fortified foods also depends on the economic consideration of the family, in cases where affordability may be a problem.
- Wrong food choices like biscuits and chips find their way into the diet of infants much early than what is usually thought by the healthcare fraternity. The clinician should spend time educating and explaining the incorrect perception or comparison of FIC being packaged just like biscuits and chips, as FIC is age-appropriate and is nutritionally superior to these inappropriate choices, which are nutritionally inadequate.
- The perception of FIC being only a convenience food should be adequately addressed by providing the scientific proof of concept on the benefits of fortification, bridging the nutritional gap and thereby decreasing the risk of malnutrition’s short-term and long-term impact.
Expert opinion on incorporating FIC along with homemade food between age of 12–23 months
The experts felt that though FIC was incorporated in the diet of <1 year old, they were used less, beyond 12 months of age, despite the high prevalence of MNDs and growth faltering in 12- to 23-month-olds. These are the critical periods of neurodevelopment and scientific papers have shown a strong association between delayed neurocognitive/physical growth and development with the prevalence of MNDs.
- There exists an opportunity to explain and establish the vital role of FIC, which extends beyond 12 months. The benefits should be highlighted by the clinicians in simplified language in their communication with the mother and other family members.
- Every infant visit can be used as a leverage, to communicate this message, especially reinforcing when parents raise concerns about developmental milestones, height, immunity, IQ etc.
- Visual growth faltering seen via anthropometric measures plotted on a growth chart along with developmental milestones can act as a medium to drive home the message to include FIC.
- Meal frequency decreases at 12 months as parents think the child should start eating just like adults. This adjustment of infants’ meal frequency like that of an adult meal could be considered around 2-3 years after the child has completely transitioned to family foods, have dietary diversity (minimum of 4 out of 7 food groups), and have nutrient and energy dense diets.
- Meeting all these aspects of the feeding of <2 years of an infant is challenging to fulfill, hence messaging to caregivers, at every doctor visit is essential to continue higher meal frequency, and diversity, which could be attained with FIC in partnership with homemade food.
Problem Statement 3: Inadequate Complementary Feeding in 6–23-Month-Olds is influenced by Traditional Beliefs, Myths, Cultural Preferences and Lack of Awareness
Problem Statement 4: Clinicians Often Have a Scarcity of Time in their Clinic for Nutritional Counselling or to Educate the Caregivers Regarding Appropriate CF Practices during Infant Visits to their Clinics
Maternal and caregiver’s knowledge, perceptions and awareness about CF and the cultural practices and myths around CF are major barriers to adequate CF in 6-23 month olds, even in food secure areas [27,49-52]. Certain myths and false beliefs result in the infants’ diet lacking in nutrient and energy density. For e.g. cereals or pulses are usually not offered initially in the CF period as they are perceived to be difficult to digest [52]. The infants may also not be offered almonds, animal-origin foods, eggs, mangoes, etc. as they are considered “hot” foods or curd, banana during winters and cold season as they are considered as “cold” food [52]. Maternal feeding practices and perceptions regarding the introduction of solid foods directly or indirectly affect her child’s acceptance of the food [38].
A study from Nepal showed that while 73.4% of mothers had adequate knowledge about CF, only 51.9% followed the correct practices. Only 39% of mothers received knowledge about CF from their Paediatricians [50]. Another study from Nepal showed that while 87% of mothers know when to start CF, 28.3% gave “lito” (porridge made from rice, maize or millet) alone as CF; 53.3% were giving marketed weaning foods; about 50% fed CF of appropriate consistency and 66% fed appropriate amount. However, only 15.8% of mothers fed their infants with CF that had all aspects: age appropriate frequency, amount and quality of feed [51].
Another study from Nepal showed that although the local physician regularly saw infants, the opportunity to counsel mother or caregiver about CF wasn’t utilized in 85% of the visits [53]. A survey of pediatricians from India showed that only 40% suggested interventions for MNDs to 25-50% of children who have been seldom followed up for the practice of the provided advice [14].
Recommendation 6: Problem focused nutritional counselling around CF should be part of routine infant care at all touch points or opportunities of conversation with caregivers such as immunization and/or illness visits. The nutritional counselling should continue until 2 years of age to ensure age-appropriate nutrition is given to infants in critical period of 6-23 months
Maternal or caregiver education or counselling regarding age-appropriate CF practices in line with the IYCF feeding guidance is an effective strategy for improving nutrient intake and reducing the risk of growth faltering [23]. A cluster RCT showed that participatory community-based nutrition education for LMIC caregivers improved a child’s dietary diversity versus providing only food [54]. A significant association exists between ideal CF practices with maternal education and IYCF-related advice given during immunization sessions [12].
A systematic review and meta-analysis found that education or counseling regarding nutrition had a small yet significant impact on linear and ponderal growth in 6-23 month olds from LMIC [23]. Another systematic review of 16 studies from LMIC showed that CF education alone significantly improved linear and ponderal growth and significantly reduced stunting rates [55].
Expert opinion
The experts felt that most clinicians might lack nutrition information. This is because nutrition is not taught at the undergraduate level. Their practices are more focused on treating illness and immunization. Hence, regular continued medical education programs, courses or scientific seminars focused on CF should be designed for nutrition during the first two years of life. Also, initiatives like paramedical or nursing staff training on imparting the same CF-related information will reduce the sole burden of nutrition counseling on the pediatrician/family doctor seeing the infant in a busy practice and bring in the hands-on approach with the whole clinical staff conversing with the caregivers. IYCF practices should be reinforced at each infant visit for immunization or illness. This messaging should cover the entire infant clinic ecosystem and should be identical across the spectrum of HCPs from nurses to general practitioners to pediatricians. This will reinforce the same information in the mother’s mind at multiple steps, from when she enters the clinic with the infant to when she meets the pediatrician or family doctor. A particular focus on evolving food texture with age, age-appropriate consistency, meal frequency and dietary diversity should be implemented to ensure optimal infant nutrition.
- HCP (Health Care Practitioner) and entire pediatric clinic messaging:
- Include information regarding the choice of food groups, cooking methods, and nutrient interaction to increase nutrient bioavailability.
- HCPs should be conversant with local and simplified words for different types of food and food groups, and their properties.
- Examples should be regionally and culturally appropriate (e.g., In Nepal red pumpkin is readily available, culturally acceptable and affordable with high nutrient properties).
- Active conversation on daily diets emphasizing the benefits of partnering FIC along with fresh home cooked meals should be made.
- Regular anthropometric measures: at each infant visit and conversations around it with the mother along with the visual impact of growth faltering on the growth chart can help drive message around appropriate CF practices: For a child whose growth graphs are going down, spend extra time counselling on nutrition and keep replotting on each subsequent visit. A mother is more likely to listen to the HCP regarding nutritional interventions and follow them if her baby is not growing well. The correct CF practices will result in the baby’s risk reduction of nutritional deficiencies and faltered growth; the mother will believe the HCP and follow all other nutrition advice including those around FIC, which will also help break the myths around CF as well.
- Regular nutrition or feeding pattern history of the infant at each infant visit should be taken by a trained nurse or any other HCP staff at the clinic; this will help identify if MMF, MDD, and MAD are met and if there is correct understanding of texture evolution with age. Emphasis on the age-appropriate nutrition, texture, uplifting the nutrient and energy density of the feed by adding FIC should also be identified and explained to caregivers. This will further address the risk of the infant being a fussy eater later in childhood and will enable the child early on to transition to family food easily.
- Regular sensitization: Just as a pregnant mother is sensitized about exclusive breastfeeding, all mothers should be sensitized about the correct time and method of introduction of solid food, and its correct practices post-delivery and at all visits (immunization/sickness) before her child attains 6 months of age; this sensitization should be age-appropriate and should continue until 2 years of age to reduce the risk of growth faltering esp. between 1-2 years of age.
- Scheduled CF visit: After the third vaccination visit, mothers can be called around 6 months for a specific session on CF; usually, this is also the time for first flu vaccine and both visits can be combined to explain correct timing of introducing CF and evolution of feed as per the age of the infant.
- Communication techniques:
- Pediatricians/HCPs should be informed about CF in short key messages that can be communicated to caregivers.
- Know ways to reassure the mother that the oro-motor reflexes are adequately developed to take solid food, visual cue cards that could tell the indications of changing the feed texture, quantity and consistency.
- Doctors can be updated on the extent of the prevalence of MNDs and its consequences by sharing NHFS-5 data on MNDs and insufficient CF practices through easy-to-understand visual charts, which could be communicated to the caregivers.
- Positive reinforcement: Praise the mothers, grandparents and caregivers of the infants for their efforts and then give them practical knowledge on how to improve on what they are doing.
- Include family members who influence the mother and infant’s diet into conversations around CF.
- Do not overburden the parents with extra information which is difficult to follow and retain: The information around CF and FIC should be simple, easy to understand, full of local terms, and be presented in take home leaflets that are not text heavy and are visually appealing (e.g., food plate method).
- QR codes for small CF age-appropriate modules or videos can be provided on these leaflets or at clinics with detailed information for parents wanting to know more.
- Overcoming barriers to age-appropriate CF: Knowledge about local beliefs and myths and methods to address key barriers to introducing a new diet should be provided. Some of the key obstacles to introducing age-appropriate CF encountered by the experts and the suggested methods to overcome them include:
- Over-dependence on milk: Inform that animal milk should not be introduced before 12 months of age. It is a poor source of iron and has imbalanced nutrient content. The nutrients in animal milk are for the nutritional requirements of its progeny but are not age-adapted for the human infants. Any early introduction of animal milk would further exaggerate the risk of micronutrient deficiencies. Thus, the quality of complementary feeds becomes necessary right from the time of its introduction. Most parents understand anemia, and know anemia is rampant in India. Examples such as this could be used to explain to the caregivers regarding the importance of avoiding animal milk till 1 year of age and the importance of appropriate CF practices till 2 years of age.
- Give easy-to-understand scientific information about CF and tell that quantity and quality both matters. “Dal pani/water” or “rice water” alone is not helpful as it lacks in nutrient density, energy density, consistency, texture and diversity which are critical aspects of CF practices.
- Explain that local grains inherently have micronutrient inhibitors like tannins, phytates, oxalates etc. which inhibit the absorption of crucial nutrients like iron, zinc etc. [56,57]. Take the example of anemia as it is well understood and propose adding fortified infant cereals to daily diet to support the hemoglobin status, serum ferritin levels, and risk reduction of anemia in that period which can have detrimental lifelong impacts [58].
Expert view: Fortification versus supplementation; which is a better method to reduce the risk of micronutrient deficiency in 6–23-month-old?
There is enough clinical evidence to show the benefits of FIC and the concept of fortification, but supplementation is preferred by many HCPs because of the ease of prescription and administration.
Fortification and supplementation should never be compared head-to-head as both co-exist. The experts emphasize that scientifically as well as clinically, supplementation is often associated with lack of compliance, chances of toxicity by accidental overdose and other issues like palatability, bloating, constipation etc. But accidental overdose toxicity seen with supplementation are not seen with fortification. Further, supplementing nutrients like iron in iron replete infants or infants whose iron status is not known can negatively impact growth and weight gain [59-61].
However, many pediatricians and HCPs believe that fortification is industry-driven and often is negatively perceived. The clinician fraternity needs to be sensitized that WHO and many National and International pediatric societies including the IAP endorse fortification and use of iron-fortified, vitamin A enriched foods that should be encouraged during the CF period.
Supplementation should be evaluated for a case-to-case basis where the hemoglobin levels have severely declined, warranting a therapeutic intervention. Fortification should be considered as a mass approach and FIC can be regarded as a preventive approach to risk reduction of anemia.
Though supplementation is often required to combat acute micronutrient deficiencies, the advantage of fortification spans over a longer period on the neurocognitive development and building a healthy eating habit for later life. The experts agreed that iron is critical during the first 1000 days of a child’s life owing to its role in brain development. Iron deficiency has far-reaching implications, the most important of which is impaired cognitive development during this period. It was strongly felt that infants with IDA are at risk for compromised cognitive, motor, social-emotional and neurophysiological development in the short and long term. The expert group opined that identifying the infants’ profile to understand the risk potential of iron deficiency is essential for any timely intervention. However, in cases where the child has high predisposition of risk of iron or other MNDs due to incorrectly followed CF practices, the preventive approach of FIC along with home-made preparations should be considered and advocated.
In cases where the infant has become symptomatically iron deficient and demands a therapeutic approach towards iron deficiency, it might not be apt to only depend on the hemoglobin concentrations for such critical identification and hence, serum ferritin as a marker of iron deficiency should also be considered.
Expert view: Role of government and other bodies in improving undernutrition in 6–23-months-old
The experts felt that since inadequate complementary feeding and MNDs persist in 6-23-months-old, the whole healthcare and industry ecosystem messaging through all media channels, advocacy and government policies should be actively energized to address these challenges. These could include:
- Strengthening existing strategies [50]
- Capacity building and education of healthcare workers to improve infant feeding practices [50]
- Supplemental feeding program leaflets [62]
- Nutrition-sensitive agricultural interventions such as home garden promotion [62,63]
- Targeted food assistance programs [62]
- Appropriate dissemination of benefits of fortification and FIC, which is age-appropriate [64]
- Availability of fortified finger foods or snacks for 12-23 months
- Consumption of biofortified grains and crops
- Point-of-use fortification with micronutrient powders or sprinklers
- Responsive feeding to ensure adequate intake of nutrient rich food and avoiding the development of fussy eaters
Acknowledgements:
We would like to thank BioQuest Solutions Pvt Ltd for their editorial assistance. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work, and have given final approval for the version to be published.
Complementary Feeding Consortium, Ali Raza8, Ananth Pai P9, Anil Thapa10, Anita Lamichhane11, Anya Sharma12, Arijit Das13, Chakra Pani C14, Gaurav Sethi15, Gnanapandithan GM16, Gopinath Muthuselvan17, Hemchandra Bhat18, Hem Sagar Rimal19, Himanshu Kelkar20, Jasjit Singh Bhasin21, Joshi Anand Kerketta22, Kaushik Chakraborty23, Lokesh Pandey24, Madhumita Bhattacharyya25, Manoj Prasad Kushwaha26, Manzur Quader27, Sadiq Hussain MD28, Nayan Kalawadia29, Nicola Flynn30, Om Prakash Mahansaria31, Pavitra Chakraborty32, Pawana Kayastha Shakya33, Prashant Moralwar34, Rachana Shetty35, Rajendra Prasad Gupta36, Rakesh Patel37, Ranjit Joshi38, Ritu Gupta39, Shailendra Bir Karmacharya40, Sameera P41, Samundra Bajimaya42, Sandip Mehta43, Sanjay Pakmode44, Sanjiv Mehta45, Sartaj Ali46, Shakil Akhtar47, Shekhar Biswas48, Sivagurunathan P49, Sourabh Duwarah50, Srinivasa Prasad BR51, Subramania Krishnamoorthy S52, Subhasis Bhattacharya53, Suhas Kulkarni54, Supraja Chandrasekar55, Suresh Kumar Surapaneni56, Sumana Chakrabarty57, Sunil Agarwala58, Umesh Kumar59, Vishnu Kumar Tondon60 and Yasir Wani61
Affiliations:
8Sehat Children Hospital, 9Dr Pai’s Paediatric Centre, Mangalore, 10Advance Multi Speciality Hospitality, Damak, 11Lumbini Medical College, Palpa, 12Medicity Hospital, Kathmandu, 13Department of Paediatrics, College of Medicine and JNM Hospital (The West Bengal University of Health Sciences), Nadia, West Bengal, 14Gayathri Children Nursing Home, Sangareddy, 15In Good Hands Clinic, New Delhi, 16Sundaram Medical Foundation, Chennai, 17Kaveri children hospital, Krishnagiri, 18Max Hospital, Patparganj, New Delhi, 19Nobel Medical College Teaching Hospital/Birat Nursing Home, Biratnagar, 20Sushrusha Clinic, Indore, 21Centre for Child Health, BLK-Max Super Speciality Hospital, Delhi, 22The Mission Hospital, Durgapur, 23Consultant Pediatrics, West Bengal, 24Bhagirathi Neotia Woman and Child Care Centre, RSV Hospital, Kolkata, 25RKSM, Matribhavan, Kolkata, 26Lumbini Zonal/Lumbini Nursing Home, Butwal, 27Bhagirathi Neotia Woman and Child Care Centre, Dilkhusha Nursing Home and Royd Nursing Home, Kolkata, 28Little Champ Child Care Clinic, Bangalore, 29Amruta Hospitals and Astha Children Hospital, Rajkot, 30Medica Hospital, Kolkata, 31Paedriatric Intensivist and Neonatologist Ranchi Trust Hospital, Ranchi, 32Bhagirathi Neotia Woman and Child Care Centre, Kolkata, 33Kathmandu Medical College, Kathmandu, 34Motherhood Hospital Kharghar, 35Poornima Hospital and Sahil Children Clinic, RT Nagar, Bangalore, 36Sanjeevni Mother and Child Hospital, Varanasi, 37Amruta Hospital, Rajkot, 38Apollo Hospitals, Bhubaneswar, 39Priti Nursing Home, Allahabad, 40Neonatology Department, Thapathaly Maternity Hospital/Valley Maternity Hospital, Kathmandu, 41Manipal Hospital, Jayanagar, Bangalore, 42International Friendship Children's Hospital, Kathmandu, 43SRCC Bhatia and Saifee Hospitals, Mumbai, 44Sayali Children Hospital, Nagpur, 45 Deepak Kailash Hospital, New Delhi, 46Ahmad Hospital, Srinagar, 47Department of Pediatrics and Nephrology, Institute of Child Health, Kolkata, 48Kindergarten Clinic, New Delhi, 49Siva Child Clinic, Trichy, 50Akanksha Hospital, Guwahati, 51 Pediatrics, Tumkur, Karnataka, 52GG Hospital, Trivandrum, 53Department of Paediatrics, Chittaranjan Seva Sadan and Sishu Sadan Hospital, Kolkata,54Chiranjeevi Hospital, Thane, 55DHEE Hospitals, Kanakapura Road, Bangalore, 56Pragna Hospitals, Hyderabad, Telangana, 57 Pediatrics, Dibrugarh, Assam, 58Sardar Vallabhbhai Patel Post Graduate Institute of Paediatrics, Cuttack, 59Sumitra Hospital, Noida, 60Sanjeevni Hospital and Rama Hospital, Kanpur, 61Medvalley Healthcare, Srinagar
Conflict of Interest:
None
Funding:
None
Author contributions:
Sunil Sehgal, Shantanu Dutt, Ganesh Kulkarni, Rahul Verma, Ravi MD, Soumitra Dutta, Madhumita Dobe have contributed equally to the conception, design drafting the manuscript, review and finalization of manuscript. Rest of the author have read, reviewed and approved the final manuscript. Consortium has contributed to the recommendations and opinion on relevant concerns.
References
- Miniello VL, Verga MC, Miniello A, et al. Complementary Feeding and Iron Status: “The Unbearable Lightness of Being” Infants. Nutrients 13 (2021): 4201.
- Fewtrell M, Bronsky J, Campoy C, et al. Complementary Feeding: A Position Paper by the European Society for Paediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) Committee on Nutrition. J Pediatr Gastroenterol Nutr 64 (2017): 119-132.
- Abeshu MA, Lelisa A, Geleta B. Complementary Feeding: Review of Recommendations, Feeding Practices, and Adequacy of Homemade Complementary Food Preparations in Developing Countries – Lessons from Ethiopia. Frontiers in Nutrition. (2016): 3.
- Koletzko B, Hirsch NL, Jewell JM, et al. National Recommendations for Infant and Young Child Feeding in the World Health Organization European Region. Journal of Pediatric Gastroenterology and Nutrition 71 (2020): 672.
- Infant and young child feeding: Fact sheet [Internet]. World Health Organization. 2021 [cited 2023 Apr 19]. Available from: https://www.who.int/news-room/fact-sheets/detail/infant-and-young-child-feeding
- Ministry of Health and Family Welfare. Infant and Child Feeding [Internet]. Ministry of Health and Family Welfare, Government of India; [cited 2023 Apr 19]. Available from: https://www.nhm.gov.in/MAA/One_Day_Sensitization_Module/One_Day_
tgSensitization_Module_English_lowres.pdf - Torlesse H, Murira Z, Hoogendoorn A. Complementary feeding in South Asia: a multi-system analysis of the enabling environment and programme context. J Public Health (Berl) 1 (2022): 935-947.
- Food fortification: recommendations [Internet]. World Health Organization. [cited 2023 Apr 19]. Available from: https://www.who.int/health-topics/food-fortification#tab=tab_2
- Jain A, Wang W, James KS, et al. Small Area Variations in Dietary Diversity among Children in India: A Multilevel Analysis of 6–23-Month-Old Children. Frontiers in Nutrition 8 (2022): 8.
- Ulak N, Dhan K, Tiwari K. Complementary Feeding Practices and its Associated Factors Among Mothers in Selected Urban Area of Nepal. Asploro Journal of Biomedical and Clinical Case Reports 3 (2020): 6-14.
- Paintal K, Aguayo VM. Feeding practices for infants and young children during and after common illness. Evidence from South Asia. Matern Child Nutr 12 (2016): 39-71.
- Kumar A, Kumar DL, Kumar T, et al. Study on factors affecting complementary feeding practices in infants and young children in a rural area of Bihar. Public Health Review: International Journal of Public Health Research 7 (2020): 01-6.
- Mehlawat U, Rekhi TK, Puri S, et al. Status of complementary feeding practices of infants and young children (0-23 months) in India. Journal of the Pediatrics Association of India 7 (2018): 40.
- Gungam P, Kadhe G, Shaikh IA. Clinical assessment of micronutrient deficiencies in 2-6 years old children: a survey with pediatricians. International Journal of Contemporary Pediatrics 8 (2021): 255-262.
- Venkatesh U, Sharma A, Ananthan VA, et al. Micronutrient’s deficiency in India: a systematic review and meta-analysis. J Nutr Sci 10 (2021): e110.
- Ministry of Health and Population, Nepal, New ERA, UNICEF, EU, USAID, CDC. Nepal National Micronutrient Status Survey 2016 [Internet]. Kathmandu, Nepal: Ministry of Health and Population, Government of Nepal; 2018 [cited 2023 Apr 14]. Available from: https://www.unicef.org/nepal/sites/unicef.org.nepal/files/2018-08/NNMSS%20Report%202016.pdf
- Bailey RL, West KP, Black RE. The epidemiology of global micronutrient deficiencies. Ann Nutr Metab 66 (2015): 22-33.
- Hallberg L, Hulthén L. Prediction of dietary iron absorption: an algorithm for calculating absorption and bioavailability of dietary iron. Am J Clin Nutr 15 (2000): 1147-1160.
- Abeshu MA, Lelisa A, Geleta B. Complementary Feeding: Review of Recommendations, Feeding Practices, and Adequacy of Homemade Complementary Food Preparations in Developing Countries - Lessons from Ethiopia. Front Nutr 3 (2016): 41.
- Malnutrition: Key facts [Internet]. World Health Organization. 2021 [cited 2023 Apr 19]. Available from: https://www.who.int/news-room/fact-sheets/detail/malnutrition.
- Stevens GA, Beal T, Mbuya MNN, et al. Micronutrient deficiencies among preschool-aged children and women of reproductive age worldwide: a pooled analysis of individual-level data from population-representative surveys. The Lancet Global Health 10 (2022): e1590-e1599.
- Ministry of Health and Family Welfare, Government of India. National Family Health Survey - 5 (2019-21): Indian Fact Sheet [Internet]. Delhi: International Institute for Population Sciences and Ministry of Health and Family Welfare, Government of India; 2021 [cited 2023 Apr 22]. Available from: http://rchiips.org/nfhs/NFHS-5_FCTS/India.pdf.
- Panjwani A, Heidkamp R. Complementary Feeding Interventions Have a Small but Significant Impact on Linear and Ponderal Growth of Children in Low- and Middle-Income Countries: A Systematic Review and Meta-Analysis. The Journal of Nutrition 147 (2017): 2169S-2178S.
- Obbagy JE, English LK, Psota TL, et al. Complementary feeding and micronutrient status: a systematic review. Am J Clin Nutr 109 (2019): 852S-871S.
- Na M, Aguayo VM, Arimond M, et al. Trends and predictors of appropriate complementary feeding practices in Nepal: An analysis of national household survey data collected between 2001 and 2014. Maternal and Child Nutrition 14 (2018): e12564.
- Rashtriya Bal Swasthya Karyakram. Journey of The First 1000 Days: Foundation for a Brighter Future [Internet]. Ministry of Health & Family Welfare, Government of India; 2018 [cited 2023 Apr 22]. Available from: https://nhm.gov.in/images/pdf/programmes/RBSK/Resource_Documents
/Journey_of_The_First_1000_Days.pdf - The Nepal Multiple Indicator Cluster Survey, (MICS). Infant and Young Child Feeding [Internet]. Central Bureau of Statistics (CBS); 2019. Available from: https://www.unicef.org/nepal/media/16246/file/Nepal%20MICS%20Statistical%20Snapshot%20-%20%20Infant%20and%20Young%20Child%20Feeding.pdf.
- Lanigan JA, Bishop J, Kimber AC, et al. Systematic review concerning the age of introduction of complementary foods to the healthy full-term infant. Eur J Clin Nutr 55 (2001): 309-320.
- Rippey PLF, Aravena F, Nyonator JP. Health Impacts of Early Complementary Food Introduction Between Formula-fed and Breastfed Infants. J Pediatr Gastroenterol Nutr 70 (2020): 375-380.
- Nutrition Landscape Information System (NLiS): Infant and young child feeding [Internet]. World Health Organization. [cited 2023 Apr 19]. Available from: https://www.who.int/data/nutrition/nlis/info/infant-and-young-child-feeding
- Chaudhary V, Saraswathy KN, Sarwal R. Dietary diversity as a sustainable approach towards micronutrient deficiencies in India. Indian Journal of Medical Research 156 (2022): 31.
- Asare H, Rosi A, Faber M, et al. Animal-source foods as a suitable complementary food for improved physical growth in 6 to 24-month-old children in low- and middle-income countries: a systematic review and meta-analysis of randomised controlled trials. British Journal of Nutrition 128 (2022): 2453-2463.
- Simeone G, Bergamini M, Verga MC, et al. Do Vegetarian Diets Provide Adequate Nutrient Intake during Complementary Feeding? A Systematic Review. Nutrients 14 (2022): 3591.
- Khamis AG, Mwanri AW, Ntwenya JE, et al. The influence of dietary diversity on the nutritional status of children between 6 and 23 months of age in Tanzania. BMC Pediatrics 19 (2019): 518.
- Saha J, Chouhan P, Malik NI, et al. Effects of Dietary Diversity on Growth Outcomes of Children Aged 6 to 23 Months in India: Evidence from National Family and Health Survey. Nutrients 15 (2023): 159.
- Thorne-Lyman AL, Shrestha M, Fawzi WW, et al. Dietary Diversity and Child Development in the Far West of Nepal: A Cohort Study. Nutrients 11 (2019): 1799.
- Mura Paroche M, Caton SJ, Vereijken CMJL, et al. How Infants and Young Children Learn About Food: A Systematic Review. Front Psychol 8 (2017): 1046.
- Tournier C, Demonteil L, Ksiazek E, et al. Factors Associated with Food Texture Acceptance in 4- to 36-Month-Old French Children: Findings From a Survey Study. Front Nutr 7 (2020): 616484.
- Demonteil L, Tournier C, Marduel A, et al. Longitudinal study on acceptance of food textures between 6 and 18-months. Food Quality and Preference 71 (2019): 54-65.
- Osendarp SJM, Broersen B, van Liere MJ, et al. Complementary Feeding Diets Made of Local Foods Can Be Optimized, but Additional Interventions Will Be Needed to Meet Iron and Zinc Requirements in 6- to 23-Month-Old Children in Low- and Middle-Income Countries. Food Nutr Bull 37 (2016): 544-570.
- Ekoe T, Bianpambe OI, Nguefack F, et al. Efficacy of an iron-fortified infant cereal to reduce the risk of iron deficiency anemia in young children in East Cameroon. Food Sci Nutr 8 (2020): 3566-3577.
- Csölle I, Fels? R, Szabó É, et al. Health outcomes associated with micronutrient-fortified complementary foods in infants and young children aged 6–23 months: a systematic review and meta-analysis. The Lancet Child & Adolescent Health 6 (2022): 533-544.
- Finn K, Callen C, Bhatia J, et al. Importance of Dietary Sources of Iron in Infants and Toddlers: Lessons from the FITS Study. Nutrients 9 (2017): 733.
- Eichler K, Wieser S, Rüthemann I, et al. Effects of micronutrient fortified milk and cereal food for infants and children: a systematic review. BMC Public Health 12 (2012): 506.
- Harrison OA, Hays NP, Ansong RS, et al. Effect of iron-fortified infant cereal on nutritional status of infants in Ghana. Food Sci Nutr 10 (2022): 286-294.
- Prieto-Patron A, Detzel P, Ramayulis R, et al. Impact of Fortified Infant Cereals on the Burden of Iron Deficiency Anemia in 6- to 23-Month-Old Indonesian Infants and Young Children: A Health Economic Simulation Model. International Journal of Environmental Research and Public Health 19 (2022): 5416.
- Awasthi S, Reddy NU, Mitra M, et al. Micronutrient-fortified infant cereal improves Hb status and reduces iron-deficiency anaemia in Indian infants: an effectiveness study. Br J Nutr 123 (2020): 780-791.
- English LK, Obbagy JE, Wong YP, et al. Types and amounts of complementary foods and beverages consumed and growth, size, and body composition: a systematic review. The American Journal of Clinical Nutrition 109 (2019): 956S-977S.
- Paudel RK, Basaula YN, Tiwari S. Knowledge and practice of Mothers of under Two Years Children on Complementary Feeding at Bharatpur Hospital, Chitwan, Nepal. Journal of Advanced Academic Research 4 (2017): 111-116.
- Bhujel S, Khadka R, Baskota S, et al. Knowledge and Practice of Complementary Feeding among the Mothers of the Child Aged Group 6-24 Months, Tanahu Distirct, Nepal. J Nepal Health Res Counc 19 (2021): 127-134.
- Chapagain RH. Complementary feeding practices of Nepali mothers for 6 months to 24 months children. JNMA J Nepal Med Assoc 191 (2013): 443-448.
- Chellaiyan VG, Liaquathali F, Marudupandiyan J. Healthy nutrition for a healthy child: A review on infant feeding in India. J Family Community Med 27 (2020): 1-7.
- Bisoi SK, Mohanty MD, Dash DK, et al. Complementary Feeding Practices And Its Economic And Social Impact: A Cross Sectional Hospital Based Study. Journal of Nepal Paediatric Society 39 (2019): 22-28.
- Kuchenbecker J, Reinbott A, Mtimuni B, et al. Nutrition education improves dietary diversity of children 6-23 months at community-level: Results from a cluster randomized controlled trial in Malawi. PLOS ONE 12 (2017): e0175216.
- Lassi ZS, Das JK, Zahid G, et al. Impact of education and provision of complementary feeding on growth and morbidity in children less than 2 years of age in developing countries: a systematic review. BMC Public Health 13 (2013): S13.
- Venkidasamy B, Selvaraj D, Nile AS, et al. Indian pulses: A review on nutritional, functional and biochemical properties with future perspectives. Trends in Food Science and Technology 88 (2019): 228-242.
- Amalraj A, Pius A. Influence of Oxalate, Phytate, Tannin, Dietary Fiber, and Cooking on Calcium Bioavailability of Commonly Consumed Cereals and Millets in India. Cereal Chemistry 92 (2015): 389-394.
- Louis A. Kazal J. Prevention of Iron Deficiency in Infants and Toddlers. AFP 66 (2002): 1217-1225.
- Majumdar I, Paul P, Talib VH, et al. The Effect of Iron Therapy on the Growth of Iron-replete and Iron-deplete Children. Journal of Tropical Pediatrics 49 (2003): 84-88.
- Idjradinata P, Watkins WE, Pollitt E. Adverse effect of iron supplementation on weight gain of iron-replete young children. The Lancet 343 (1994): 1252-1254.
- Iannotti LL, Tielsch JM, Black MM, et al. Iron supplementation in early childhood: health benefits and risks. Am J Clin Nutr 84 (2006): 1261-1276.
- Shively G, Evans A. Dietary Diversity in Nepal: A Latent Class Approach. Food Nutr Bull 42 (2021): 259-273.
- Margolies A, Kemp CG, Choo EM, et al. Nutrition-sensitive agriculture programs increase dietary diversity in children under 5 years: A review and meta-analysis. J Glob Health 12 (2022): 08001.
- Theurich MA, Fewtrell M, Baumgartner J, et al. Moving Complementary Feeding Forward: Report on a Workshop of the Federation of International Societies for Pediatric Gastroenterology, Hepatology and Nutrition (FISPGHAN) and the World Health Organization Regional Office for Europe. Journal of Pediatric Gastroenterology and Nutrition 4 (2022): 411.
- Hassfurter K. Child Food Poverty: A Nutrition Crisis in Early Childhood [Internet]. UNICEF DATA. 2022 [cited 2023 Apr 24]. Available from: https://data.unicef.org/resources/child-food-poverty/
- Lynch SR, Beard JL, Dassenko SA, et al. Iron absorption from legumes in humans. The American Journal of Clinical Nutrition. 40 (1984): 42-47.
- Gillooly M, Bothwell TH, Torrance JD, et al. The effects of organic acids, phytates and polyphenols on the absorption of iron from vegetables. British Journal of Nutrition 3 (1983): 331-342.
- Hurrell R, Egli I. Iron bioavailability and dietary reference values. Am J Clin Nutr 5 (2010): 1461S-1467S.
- Hallberg L. Bioavailability of Dietary Iron in Man. Annual Review of Nutrition 1 (1981): 123-147.
- Infant and Toddler Forum. Developmental stages in infant and toddler feeding. Available at: https://infantandtoddlerforum.org/media/upload/pdf-downloads/3.5_Developmental_Stages_in_Infant_and_Toddler_Feeding_NEW.pdf. Accessed on: 8 August 2023.
