Outcomes Following Capsular Distention for Stage II Adhesive Capsulitis
Article Information
Alyssa Pelak1, Amier Hassan1, Arnav Barve2, Antonio Madrazo-Ibarra3, Jonathan Kirschner3, Vijay B. Vad3*
1Weill Cornell Medical College, New York, NY, USA
2University College Dublin School of Medicine, Belfield, Dublin, Ireland
3Hospital for Special Surgery, New York, NY, USA
*Corresponding Author: Vijay B. Vad, Hospital for Special Surgery, 535 E 70th St New York, NY, USA
Received: 23 February 2023; Accepted: 28 February 2023; Published: 08 March 2023
Citation:
Alyssa Pelak, Amier Hassan, Arnav Barve, Antonio Madrazo-Ibarra, Jonathan Kirschner, Vijay Vad. Outcomes Following Capsular Distention for Stage II Adhesive Capsulitis. Journal of Orthopedics and Sports Medicine. 5 (2023): 106-111.
View / Download Pdf Share at FacebookAbstract
Background: There has been many different treatments for adhesive capsulitis explored including physical therapy, manipulation under anesthesia, arthroscopic capsular release, corticosteroid injections, and capsular distention without consensus regarding the most effective treatment. Capsular distention has not been explored in a mid-term study. Therefore, this study aims to investigate the mid-term outcomes of the procedure and analyze the need for a second procedure following initial distention.
Methods: This study included 27 patients with average age of 58 diagnosed with stage II adhesive capsulitis. The primary outcome was the rate of second procedures in patients following initial capsular distention, utilizing both electronic medical record and direct patient questions. The secondary outcomes included patient satisfaction rating, range of motion (ROM) limitations, limitations on Activities of Daily Living (ADLs) and time to follow up.
Results: At an average follow up of 49 months, 78% of patients did not require a second procedure following capsular distention. The group that required second procedure had a significantly higher percentage of hypothyroid patients and a shorter time to follow up visits. Additionally, 81% of the total cohort reported their outcomes as “good,” 74% had no ROM limitations and 89% had no limitations on ADLs.
Conclusion: Capsular distention shows promising results for mid-term follow up with patient reported outcomes and over three quarters of patients not requiring a second procedure. Further research on the use of this treatment is warranted including randomized controlled trials and longer term follow up.
Keywords
Adhesive Capsulitis; Capsular distention
Adhesive capsulitis articles Adhesive capsulitis Research articles Adhesive capsulitis review articles Adhesive capsulitis PubMed articles Adhesive capsulitis PubMed Central articles Adhesive capsulitis 2023 articles Adhesive capsulitis 2024 articles Adhesive capsulitis Scopus articles Adhesive capsulitis impact factor journals Adhesive capsulitis Scopus journals Adhesive capsulitis PubMed journals Adhesive capsulitis medical journals Adhesive capsulitis free journals Adhesive capsulitis best journals Adhesive capsulitis top journals Adhesive capsulitis free medical journals Adhesive capsulitis famous journals Adhesive capsulitis Google Scholar indexed journals Frozen shoulder articles Frozen shoulder Research articles Frozen shoulder review articles Frozen shoulder PubMed articles Frozen shoulder PubMed Central articles Frozen shoulder 2023 articles Frozen shoulder 2024 articles Frozen shoulder Scopus articles Frozen shoulder impact factor journals Frozen shoulder Scopus journals Frozen shoulder PubMed journals Frozen shoulder medical journals Frozen shoulder free journals Frozen shoulder best journals Frozen shoulder top journals Frozen shoulder free medical journals Frozen shoulder famous journals Frozen shoulder Google Scholar indexed journals Glenohumeral capsule articles Glenohumeral capsule Research articles Glenohumeral capsule review articles Glenohumeral capsule PubMed articles Glenohumeral capsule PubMed Central articles Glenohumeral capsule 2023 articles Glenohumeral capsule 2024 articles Glenohumeral capsule Scopus articles Glenohumeral capsule impact factor journals Glenohumeral capsule Scopus journals Glenohumeral capsule PubMed journals Glenohumeral capsule medical journals Glenohumeral capsule free journals Glenohumeral capsule best journals Glenohumeral capsule top journals Glenohumeral capsule free medical journals Glenohumeral capsule famous journals Glenohumeral capsule Google Scholar indexed journals Coracohumeral ligament articles Coracohumeral ligament Research articles Coracohumeral ligament review articles Coracohumeral ligament PubMed articles Coracohumeral ligament PubMed Central articles Coracohumeral ligament 2023 articles Coracohumeral ligament 2024 articles Coracohumeral ligament Scopus articles Coracohumeral ligament impact factor journals Coracohumeral ligament Scopus journals Coracohumeral ligament PubMed journals Coracohumeral ligament medical journals Coracohumeral ligament free journals Coracohumeral ligament best journals Coracohumeral ligament top journals Coracohumeral ligament free medical journals Coracohumeral ligament famous journals Coracohumeral ligament Google Scholar indexed journals Hypothyroidism articles Hypothyroidism Research articles Hypothyroidism review articles Hypothyroidism PubMed articles Hypothyroidism PubMed Central articles Hypothyroidism 2023 articles Hypothyroidism 2024 articles Hypothyroidism Scopus articles Hypothyroidism impact factor journals Hypothyroidism Scopus journals Hypothyroidism PubMed journals Hypothyroidism medical journals Hypothyroidism free journals Hypothyroidism best journals Hypothyroidism top journals Hypothyroidism free medical journals Hypothyroidism famous journals Hypothyroidism Google Scholar indexed journals Breast cancer articles Breast cancer Research articles Breast cancer review articles Breast cancer PubMed articles Breast cancer PubMed Central articles Breast cancer 2023 articles Breast cancer 2024 articles Breast cancer Scopus articles Breast cancer impact factor journals Breast cancer Scopus journals Breast cancer PubMed journals Breast cancer medical journals Breast cancer free journals Breast cancer best journals Breast cancer top journals Breast cancer free medical journals Breast cancer famous journals Breast cancer Google Scholar indexed journals Minimal pain articles Minimal pain Research articles Minimal pain review articles Minimal pain PubMed articles Minimal pain PubMed Central articles Minimal pain 2023 articles Minimal pain 2024 articles Minimal pain Scopus articles Minimal pain impact factor journals Minimal pain Scopus journals Minimal pain PubMed journals Minimal pain medical journals Minimal pain free journals Minimal pain best journals Minimal pain top journals Minimal pain free medical journals Minimal pain famous journals Minimal pain Google Scholar indexed journals Non-steroidal anti-inflammatories articles Non-steroidal anti-inflammatories Research articles Non-steroidal anti-inflammatories review articles Non-steroidal anti-inflammatories PubMed articles Non-steroidal anti-inflammatories PubMed Central articles Non-steroidal anti-inflammatories 2023 articles Non-steroidal anti-inflammatories 2024 articles Non-steroidal anti-inflammatories Scopus articles Non-steroidal anti-inflammatories impact factor journals Non-steroidal anti-inflammatories Scopus journals Non-steroidal anti-inflammatories PubMed journals Non-steroidal anti-inflammatories medical journals Non-steroidal anti-inflammatories free journals Non-steroidal anti-inflammatories best journals Non-steroidal anti-inflammatories top journals Non-steroidal anti-inflammatories free medical journals Non-steroidal anti-inflammatories famous journals Non-steroidal anti-inflammatories Google Scholar indexed journals Physiotherapy articles Physiotherapy Research articles Physiotherapy review articles Physiotherapy PubMed articles Physiotherapy PubMed Central articles Physiotherapy 2023 articles Physiotherapy 2024 articles Physiotherapy Scopus articles Physiotherapy impact factor journals Physiotherapy Scopus journals Physiotherapy PubMed journals Physiotherapy medical journals Physiotherapy free journals Physiotherapy best journals Physiotherapy top journals Physiotherapy free medical journals Physiotherapy famous journals Physiotherapy Google Scholar indexed journals Hyaluronic acid articles Hyaluronic acid Research articles Hyaluronic acid review articles Hyaluronic acid PubMed articles Hyaluronic acid PubMed Central articles Hyaluronic acid 2023 articles Hyaluronic acid 2024 articles Hyaluronic acid Scopus articles Hyaluronic acid impact factor journals Hyaluronic acid Scopus journals Hyaluronic acid PubMed journals Hyaluronic acid medical journals Hyaluronic acid free journals Hyaluronic acid best journals Hyaluronic acid top journals Hyaluronic acid free medical journals Hyaluronic acid famous journals Hyaluronic acid Google Scholar indexed journals Menstrual bleeding articles Menstrual bleeding Research articles Menstrual bleeding review articles Menstrual bleeding PubMed articles Menstrual bleeding PubMed Central articles Menstrual bleeding 2023 articles Menstrual bleeding 2024 articles Menstrual bleeding Scopus articles Menstrual bleeding impact factor journals Menstrual bleeding Scopus journals Menstrual bleeding PubMed journals Menstrual bleeding medical journals Menstrual bleeding free journals Menstrual bleeding best journals Menstrual bleeding top journals Menstrual bleeding free medical journals Menstrual bleeding famous journals Menstrual bleeding Google Scholar indexed journals Humerus articles Humerus Research articles Humerus review articles Humerus PubMed articles Humerus PubMed Central articles Humerus 2023 articles Humerus 2024 articles Humerus Scopus articles Humerus impact factor journals Humerus Scopus journals Humerus PubMed journals Humerus medical journals Humerus free journals Humerus best journals Humerus top journals Humerus free medical journals Humerus famous journals Humerus Google Scholar indexed journals Neurological injury articles Neurological injury Research articles Neurological injury review articles Neurological injury PubMed articles Neurological injury PubMed Central articles Neurological injury 2023 articles Neurological injury 2024 articles Neurological injury Scopus articles Neurological injury impact factor journals Neurological injury Scopus journals Neurological injury PubMed journals Neurological injury medical journals Neurological injury free journals Neurological injury best journals Neurological injury top journals Neurological injury free medical journals Neurological injury famous journals Neurological injury Google Scholar indexed journals Fluoroscopy articles Fluoroscopy Research articles Fluoroscopy review articles Fluoroscopy PubMed articles Fluoroscopy PubMed Central articles Fluoroscopy 2023 articles Fluoroscopy 2024 articles Fluoroscopy Scopus articles Fluoroscopy impact factor journals Fluoroscopy Scopus journals Fluoroscopy PubMed journals Fluoroscopy medical journals Fluoroscopy free journals Fluoroscopy best journals Fluoroscopy top journals Fluoroscopy free medical journals Fluoroscopy famous journals Fluoroscopy Google Scholar indexed journals Muscle atrophy articles Muscle atrophy Research articles Muscle atrophy review articles Muscle atrophy PubMed articles Muscle atrophy PubMed Central articles Muscle atrophy 2023 articles Muscle atrophy 2024 articles Muscle atrophy Scopus articles Muscle atrophy impact factor journals Muscle atrophy Scopus journals Muscle atrophy PubMed journals Muscle atrophy medical journals Muscle atrophy free journals Muscle atrophy best journals Muscle atrophy top journals Muscle atrophy free medical journals Muscle atrophy famous journals Muscle atrophy Google Scholar indexed journals
Article Details
1. Introduction
Adhesive Capsulitis (AC), commonly known as “frozen shoulder,” was first described in 1872 as a contracture of the glenohumeral capsule, loss of the synovial layer, thickening of the coracohumeral ligament, and fibrosis [1]. This condition impacts 2-5% of the population, predominantly middle-aged women and individuals with diabetes, hypothyroidism, or a history of treatment for breast cancer [1-4]. Patients commonly present with pain and limited active and passive range of motion (ROM) [3]. AC is a progressive condition and can be broadly categorized into 4 stages. Stage 1 (Pre-freezing stage – pain usually at night, ROM limited), Stage 2 (Freezing stage – movement of shoulder causes pain, restricted ROM, lasts from 3 to 9 months), Stage 3 (Frozen stage – pain is reduced but stiffness remains, lasts from 9 to 15 months) and Stage 4 (Thawing stage – minimal pain, ROM improves until complete restoration.) [2,3,5,6]. This decrease in ROM along with the pain, greatly impacts the quality of life of patients, by affecting daily activities such as combing hair, dressing, and reaching into pockets [2]. This creates the need for effective treatment options which can provide long-lasting pain relief.
As of today, there is no common consensus in the treatment for AC. However, due to the self-limiting nature of this condition, conservative treatment is preferred as a first line treatment [3,4,6]. Non-steroidal anti-inflammatories (NSAIDs) and physiotherapy have demonstrated success in treatment [7]. However, the administration of NSAIDs alone has shown to cause additional side effects along with no significant improvement in joint mobility [8]. Moreover, physical therapy by itself has shown little to no effect on patient outcomes [7]. Hence, NSAIDs and physiotherapy are usually administered together but are not recommended after stage 1 due to their inability to provide long-term pain relief [3,9]. Image guided injections, including steroids or hyaluronic acid, are also commonly utilized in early stages of the disease and have shown positive results [2,5,10]. However, corticosteroid injections have not proved to be a suitable treatment option. This is due to the ineffectiveness of the injections 6 months after their administration, and the onset of additional side effects in female patients, such as facial flushing and menstrual bleeding [11,12].
If patients continue to experience persisting symptoms after conservative treatments, surgical intervention is recommended [13]. Historically, manipulation under anesthesia is done to rupture the capsule from humerus [14]. However, use of this procedure is reducing due to the risk of humeral fracture, neurological injury, and vascular injury [3,14]. Arthroscopic capsular releases are more commonly utilized. This procedure is effective at improving pain and ROM longer term and allows for concurrent evaluation of other structures [3,5]. However, differing surgical outcomes and improvements, along with the possibility of injury to the axillary nerve, has led to variation in the surgical approach and protocol, preventing the establishment of a common consensus [15,16].
Capsular distention consists on injecting saline into the glenohumeral joint until the joint capsule bursts [3,17]. It is a simple technique that can be performed in the office [18-20]. Complications such as afterpains, numbness and nausea may rarely occur, but they have been reported as mild and self-resolving [21,23]. This procedure has showed to improve pain, function, and range of motion in the short term (around 3 months), in patients with stage 2 AC [9,14]. But, the mid-term outcomes of this procedure have not yet been reported [9,14]. Therefore we have decided to conduct a retrospective study evaluating the outcomes after 1 year of capsular distention in patients with stage 2 AC.
2. Methods
2.1 Study design
This retrospective cohort study was performed at a single private practice affiliated with the Hospital for Special Surgery (New York, NY). We reviewed all electronic medical records of patients diagnosed with stage 2 AC that received a capsular distention procedure between January 2016 and July 2021. Patients were identified using electronic patient tracking systems. The inclusion criteria for this study were: 18 years of age and a diagnosis of stage 2 adhesive capsulitis. Moreover, upon receiving the capsular distension procedure, capsular rupture was confirmed in all cases using dye pre and post-distention rupture under fluoroscopy (Figure 1). No complications such as muscle atrophy or discoloration were seen. Patients were excluded if they had bilateral capsular distention or glenohumeral osteoarthritis. Data extracted included age, sex, height, weight, BMI, date of procedure, affected shoulder, any noted medical conditions, and any other surgeries or procedures done to the shoulder. The Electronic Medical Record (EMR) was also evaluated for evidence and notes indicating glenohumeral osteoarthritis to determine eligibility.
Physician notes were reviewed for the most recent follow-up post-capsular distention at least 1 year after the procedure. The physician routinely noted whether the patients had ever been diagnosed with diabetes, hypothyroidism, or any other chronic medical conditions prior to the procedure. They were also asked whether they were pre-menopausal, post-menopausal, or unsure at the time of their procedure.
2.2 Outcomes
The primary outcome was the incidence of future procedures, which was directly evaluated through the EMR and physician notes. The secondary outcome was patients´ satisfaction as reported by the physician, based upon a questionnaire filled by the patient after 1 year of the procedure. The satisfaction questionnaire is included in the supplementary files.
2.3 Statistical analysis
Statistical analysis was performed to identify correlation of demographics with incidence of future procedures using a Pearson’s chi-squared test and a paired t-test where appropriate. A p-value below 0.05 was considered significant. The statistical analysis was carried out using SAS version 9.4.
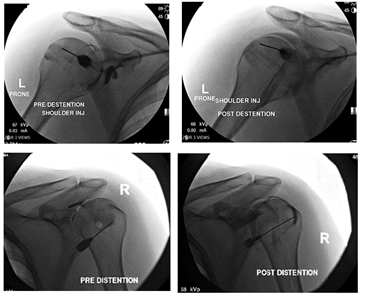
Figure 1: Photos pre- distention and post-distention under fluoroscopy.
3. Results
Twenty-seven patients were included in the final analysis (Table 1). A large majority of the patients identified as female, with more of the women being post-menopausal. Additionally, almost one quarter of the patients had hypothyroidism. There were not enough diabetic patients (n=1) to analyze. The mean time to follow up of the population was over 4 years.
|
Characteristic |
Study Population (n=27) |
|
Age (years) |
57.7 ± 9.20 |
|
BMI |
23.6 ± 5.53 |
|
Sex (F) |
22 (81.5%) |
|
Time to Follow up (months) |
49.1 ± 19.2 |
|
Hypothyroid (%) |
22.2 |
|
Pre-Menopause (%) |
40.9 |
|
Post-Menopause (%) |
59.1 |
Table 1: Demographic characteristics of population.
22.2 % of the cohort received another procedure and 77.8 % did not (p = 0.0039) (Figure 2). The procedures done were second capsular distentions (n=2), injections including lidocaine and corticosteroids (n=3), and large joint arthrocentesis (n=1). The demographic characteristics of the patients in both groups did not differ significantly except for in the number with hypothyroidism and the length of time between the initial capsular distention and follow up. 66.7% of the second procedure group and 9.5% of the no second procedure group identified as having a diagnosis of hypothyroidism. Hypothyroid patients were more likely to get another surgery (p < 0.05). Moreover, the time between the initial capsular distention and the follow up visit was longer in the no second procedure group (53.2 months) than the second procedure group (34.3) (p<0.05) (Table 2). The risk of needing a second procedure increases over time (Figure 3). After around 34.3 months, the survival does not decline.
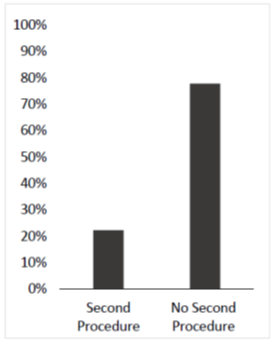
Figure 2: There was a statistically significant difference in the number of patients that received another procedure following their capsular distention (22.2%) as compared to those who did not (77.8%) (p < 0.05).
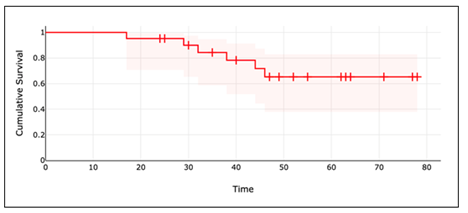
Figure 3: The risk of needing a second procedure increases over time.
|
Second Procedure |
No Second Procedure |
P-value |
|
|
Participants (%) |
6 (22.2%) |
21 (77.8%) |
0.0039 |
|
Age (years) |
58.5 ± 10.4 |
57.5 ± 9.11 |
0.41 |
|
BMI (kg/m2) |
25.3 ± 4.33 |
23.2 ± 5.84 |
0.23 |
|
Sex (F) |
5 (83.3%) |
17 (81.0%) |
0.64 |
|
Time to Data Collection (Months) |
34.3 ±10.8 |
53.2 ± 19.6 |
0.017 |
|
Hypothyroidism |
4 (66.7%) |
3 (9.5%) |
0.0098 |
|
Pre-menopausal |
3 (60.0%) |
6 (35.3%) |
0.32 |
|
Post-menopausal |
2 (40.0%) |
10 (64.7%) |
0.46 |
Table 2: Comparative Demographics.
Patient reported outcomes at follow up showed 81% reporting their outcomes as good, 15% fair, and 4% poor (p < 0.001) (Figure 4). Additionally, 74.07% reported no range of motion limitations at the time of follow up and 88.9% reported no limitations on performing activities of daily living. There was no significant difference between the second procedure group and the no second procedure group with regards to the patient reported outcomes (p>0.05).
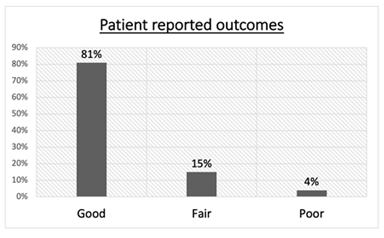
Figure 4: There was a statistically significant difference in the number of patients that reported their outcome as “good” as compared to “fair” and “poor.”
4. Conclusion
To our knowledge, this is one of the only studies examining long term patient outcomes post-capsular distention procedure for stage 2 adhesive capsulitis. Amongst the patients included in this study, the majority were post-menopausal females. It was seen that most patients (77.8%) required no second procedures after the first capsular distention. Moreover, patients that did receive a second procedure averaged a time to follow up of under 3 years while those who did not get a second procedure averaged 4.5 years. This was likely related to the need for follow up for those still experiencing pain and range of motion deficits. Additionally, the Kaplan-Meier survival analysis indicated that after 45 months, there was not a change in survival defined as the probability of needing a second procedure. This indicated that most patients who will receive another procedure may need it prior to 4 years after initial capsular distention.
The long-term effectiveness of this treatment is further supported by patient-reported outcomes, since most patients reported “good” outcomes, no deficits in the range of motion, and no difficulties with activities of daily living. An interesting finding of this study was that a higher proportion of patients that required a second procedure following their capsular distention were reported as hypothyroid. This warrants investigations into clinical outcomes of adhesive capsulitis in patients with comorbidities such as hypothyroidism.
Similar studies focusing on the effectiveness of capsular distention for AC have observed a significant improvement in the ROM and pain relief in patients. However, the greatest improvement in ROM and pain relief was seen in patients that received a steroid injection in addition to the capsular distension [23-26]. Hence, further research is required to investigate the effect of intra-articular steroid injections on adhesive capsulitis.
Although other treatment options such as physical therapy, acupuncture and surgical interventions do exist, capsular distention has shown the most promising results for patient outcomes including pain, satisfaction, and range of motion at an extended time point. A prior study analyzing outcomes of physical therapy, the current first-line treatment for adhesive capsulitis, showed that 7% of patients underwent manipulation and/or arthroscopic capsular release and 90% of the patients indicated a satisfactory outcome after almost 2 years [27]. The study did not focus on rates of second procedures such as injections and capsular distention to directly compare with the findings of this study. Another study demonstrated that 50% of patients, also managed with physical therapy, reported either pain or stiffness and 60% had a deficit in shoulder range of motion at an average follow up of seven years [28]. Moreover, acupuncture treatments, which are used for other musculoskeletal conditions, have shown little promise in treating AC. The use of this treatment remains largely speculative [18]. This shows that capsular distention may have better outcomes than physical therapy and acupuncture, but further studies need to be conducted to directly compare interventions.
Currently, surgical interventions such as Manipulation Under Anesthesia (MUA) and arthroscopic capsular releases are recommended if conservative treatments are ineffective. An open surgical release is another treatment option, but its prevalence has decreased in recent years owing to the possible risks and the availability of other safer procedures [15,29]. MUA involves mobilization of the joint under anesthesia. Although this procedure has yielded satisfactory results, its effectiveness in comparison to capsular distension remains uncertain [16]. Moreover, the possibility of requiring recurrent procedures, and the risk of iatrogenic complications, reduces the benefit of this procedure [30,31]. Arthroscopic capsular releases are also utilized in patients if MUA proves to be ineffective. Despite showing promising results, the variation in the surgical approaches and probability of nerve injury associated with the procedure, has prevented the formation of a standardized surgical protocol [15,32].
One of the main limitations of our study was that a validated questionnaire was not utilized for the collection of the data. Although the questions used in our study were standardized, future studies should seek to utilize validated measurements such as the Disabilities of the Arm, Shoulder, And Hand (DASH) and goniometry for specific range of motion reporting. Moreover, the addition of a comparison group would enable us to directly analyze improvements as a result of this procedure. Additionally, the inclusion of a larger randomized pool of patients from different clinics would reduce any bias and may also enable the discovery of other significant differences between the two focus groups.
Overall, capsular distension is a long-lasting and minimally invasive procedure which has shown to alleviate the symptoms of adhesive capsulitis. Given the clinical outcome metrics and subjective reports of patients in this study, the long-term therapeutic efficacy of this procedure is promising. Furthermore, the application of this procedure in combination with other forms of treatment warrants further exploration.
References
- Patel R, Urits I, Wolf J, et al. A Comprehensive Update of Adhesive Capsulitis and Minimally Invasive Treatment Options. Psychopharmacol Bull 50 (2020): 91-107.
- Neviaser AS, Neviaser RJ. Adhesive Capsulitis of the Shoulder. JAAOS - Journal of the American Academy of Orthopaedic Surgeons 19 (2011): 536-542.
- Fields BKK, Skalski MR, Patel DB, et al. Adhesive capsulitis: review of imaging findings, pathophysiology, clinical presentation, and treatment options. Skeletal Radiol 48 (2019): 1171-1184.
- Kingston K, Curry EJ, Galvin JW, et al. Shoulder adhesive capsulitis: epidemiology and predictors of surgery. J Shoulder Elbow Surg 27 (2018): 1437-1443.
- Redler LH, Dennis ER. Treatment of Adhesive Capsulitis of the Shoulder. J Am Acad Orthop Surg 27 (2019): e544-e554.
- Nakandala P, Nanayakkara I, Wadugodapitiya S, et al. The efficacy of physiotherapy interventions in the treatment of adhesive capsulitis: A systematic review. J Back Musculoskelet Rehabil 34 (2021): 195-205.
- Le HV, Lee SJ, Nazarian A, et al. Adhesive capsulitis of the shoulder: Review of pathophysiology and current clinical treatments. Shoulder and Elbow 9 (2016): 75-84.
- Rhind V, Downie WW, Bird HA, et al. Naproxen and indomethacin in periarthritis of the shoulder. Rheumatology 21 (1982): 51-53.
- Ramirez J. Adhesive Capsulitis: Diagnosis and Management. American Family Physician 99 (2019): 4.
- Park KD, Nam HS, Lee JK, et al. Treatment Effects of Ultrasound-Guided Capsular Distension with Hyaluronic Acid in Adhesive Capsulitis of the Shoulder. Archives of Physical Medicine and Rehabilitation 94 (2013): 264-270.
- Bulgen DY, Binder AI, Hazleman BL, et al. Frozen Shoulder: Prospective clinical study with an evaluation of three treatment regimens. Annals of the Rheumatic Diseases 43 (1984): 353-60.
- van der Windt DA, Koes BW, Deville W, et al. Effectiveness of corticosteroid injections versus physiotherapy for treatment of painful stiff shoulder in primary care: Randomised trial. BMJ 317 (1998): 1292-1296.
- Sharma S, Jacobs L. Management of frozen shoulder – conservative vs. surgical? The Annals of The Royal College of Surgeons of England 93 (2011): 343.
- Sandor R. Adhesive capsulitis: optimal treatment of “frozen shoulder”. Phys Sportsmed 28 (2000): 23-29.
- Cho C-H, Bae K-C, Kim D-H. Treatment strategy for Frozen Shoulder. Clinics in Orthopedic Surgery 11 (2019): 249.
- Uppal HS. Frozen Shoulder: A systematic review of Therapeutic Options. World Journal of Orthopedics 6 (2015): 263.
- Vad VB, Sakalkale D, Warren RF. The role of capsular distention in adhesive capsulitis. Arch Phys Med Rehabil 84 (2003): 1290-1292.
- Lewis J. Frozen shoulder contracture syndrome - Aetiology, diagnosis and management. Man Ther 20 (2015): 2-9.
- Lin M-T, Hsiao M-Y, Tu Y-K, et al. Comparative efficacy of intra-articular steroid injection and distension in patients with frozen shoulder: A systematic review and network meta-analysis. Archives of Physical Medicine and Rehabilitation 99 (2018).
- Zhang J, Zhong S, Tan T, et al. Comparative efficacy and patient-specific moderating factors of nonsurgical treatment strategies for frozen shoulder: An updated systematic review and network meta-analysis. The American Journal of Sports Medicine 49 (2020): 1669-1679.
- Catapano M, Mittal N, Adamich J, et al. Hydrodilatation with corticosteroid for the treatment of Adhesive capsulitis: A systematic review. PM and R 10 (2017): 623-635.
- Buchbinder R, Green S, Youd JM, et al. Arthrographic distension for adhesive capsulitis (frozen shoulder). Cochrane Database of Systematic Reviews (2008).
- Buchbinder R, Lawler G, Hall S, et al. Arthrographic Joint Distension with saline and steroid improves function and reduces pain in patients with painful stiff shoulder: Results of a randomised, double blind, placebo controlled trial. Annals of the Rheumatic Diseases 63 (2004): 302-309.
- Jacobs LG, Barton MA, Wallace WA, et al. Intra-articular distension and steroids in the management of capsulitis of the shoulder. BMJ 302 (1991): 1498-1501.
- Rizk TE, Gavant ML, Pinals RS. Treatment of adhesive capsulitis (frozen shoulder) with Arthrographic Capsular distension and rupture. Archives of Physical Medicine and Rehabilitation 75 (1994): 803-807.
- Gam A, Schydlowsky P, Rossel I, et al. Treatment of 'frozen shoulder' with distension and glucorticoid compared with glucorticoid alone: A randomised controlled trial. Scandinavian Journal of Rheumatology 27 (1998): 425-430.
- Griggs SM, Ahn A, Green A. Idiopathic Adhesive Capsulitis: A Prospective Functional Outcome Study of Nonoperative Treatment. JBJS 82 (2000): 1398.
- Shaffer B, Tibone JE, Kerlan RK. Frozen shoulder. A long-term follow-up. J Bone Joint Surg Am 74 (1992): 738-746.
- Robinson CM, Seah KT, Chee YH, et al. Frozen Shoulder. The Journal of Bone and Joint Surgery British volume 94-B (2012): 1-9.
- Theodorides AA, Owen JM, Sayers AE, et al. Factors affecting short- and long-term outcomes of manipulation under anaesthesia in patients with adhesive capsulitis of the shoulder. Shoulder and Elbow 6 (2014): 245-256.
- Loew M, Heichel TO, Lehner B. Intraarticular lesions in primary frozen shoulder after manipulation under general anesthesia. Journal of Shoulder and Elbow Surgery 14 (2005): 16-21.
- Chen J, Chen S, Li Y, et al. Is the extended release of the inferior glenohumeral ligament necessary for frozen shoulder? Arthroscopy: The Journal of Arthroscopic and Related Surgery 26 (2010): 529-535.
