Outcome of Surgical Management in Lumber Disc Prolapse: A Study in Dhaka Medical College Hospital, Dhaka, Bangladesh
Article Information
Shahidul Islam1*, Muhammad Shahiduzzaman2, Ferdous Ara Banu3, Md Hasan4, Shamiul Alam Siddique5, Fatema Sultana Sumi6, Tahmina Akhter6, Abu Hena Md Atiquzzaman7
1Professor and Head, Department of Orthopedics and Spine Surgery,Addin womens medical college hospital, Dhaka, Bangladesh
2Professor and Head, Department of Orthopedics, Dhaka Medical College Hospital, Dhaka, Bangladesh
3Junior consultant, DGHS, Mohakhali, Deputation in BSMMU, Dhaka, Bangladesh
4Assistant professor, Department of Orthopedics, Holy Family Red Cresent Medical College Hospital, Dhaka, Bangladesh
5Assistant Professor, Department of Neurosurgery, Mymensingh Medical College, Dhaka, Bangladesh
6Medical officer, Department of Orthopedics and Spine Surgery, Addin Medical College Hospital, Dhaka, Bangladesh
7Medical officer, Department of Orthopedics and Spine Surgery, National Institute of Traumatology and Orthopaedic Rehabilitation (NITOR), Dhaka, Bangladesh
*Corresponding Author: Dr. Shahidul Islam, Professor and head, Department of Orthopedics and Spine Surgery, Addin womens medical college hospital, Dhaka, Bangladesh
Received: 27 December 2021; Accepted: 06 January 2022; Published: 14 January 2022
Citation:
Shahidul Islam, Muhammad Shahiduzzaman, Ferdous Ara Banu, Md Hasan, Shamiul Alam Siddique, Fatema Sultana Sumi, Tahmina Akhter, Abu Hena Md Atiquzzaman. Outcome of Surgical Management in Lumber Disc Prolapse: A Study in Dhaka Medical College Hospital, Dhaka, Bangladesh. Journal of Spine Research and Surgery 4 (2022): 018-028.
View / Download Pdf Share at FacebookAbstract
A disc herniation is the term given to any uneven out-pouching or bulging of the posterior region (back region) of the intervertebral disc as seen on MRI. The bigger the lumbar/sacral disc herniation, the more likely it is to cause back and/or leg pain--the latter of which is called sciatica1. The aim of this study was to evaluate the surgical outcome in the treatment of Lumber Disc Prolapse (LDP). The prospective interventional study (Quasi experimental) was done in the Department of Orthopedics and Traumatology, Dhaka Medical College and Hospital during the period of June 2009 to July 2011(2 years). Due to time limitation and financial constraint only 35 cases were selected during study period but out of them 29 cases were feasible to be included in the study, remaining 6 cases were lost during follow up. Patients of both sexes aged between 18-70 years with prolapsed lumber intervertebral disc admitted in the Department of Orthopedics and Traumatology were included as purposive sampling. Data was entered, coded, cleaned, and analyzed by using Statistical Package for Social Science (IBM SPSS), version 20. In our study we found, Clinically 17(58.6%) of patients had weakness in extensor hallucis longus (EHL) and 3(10.3%) of patients had weakness in flexor hallucis longus (FHL). 14(48.3%) of patients had sensory deficit over the distribution of L5 nerve root and 6(20.7%) had S1 nerve root. In X-ray there were 6 transitional vertebra and loss of lumbar lordosis was in 20 patients. MRI shows 20(62.5%) of patients had posterolateral disc bulge and 12(37.5) had posterior disc bulge. In majority of patients (65.5%) of patients had disc prolapse at level L4-L5. 53.7% of patients had left sided disc prolapse. Peroperatively seen that 62.5% of the patients had posterolateral disc prolapse and 37.5% patients had central disc prolapse. There were only 10.3% of patients had complications. Among these 6.9% had per operative dural tear and 3.4% developed discitis. At the final
Keywords
Outcome, Surgical Management, Lumber Disc Prolapse
Outcome articles Outcome Research articles Outcome review articles Outcome PubMed articles Outcome PubMed Central articles Outcome 2023 articles Outcome 2024 articles Outcome Scopus articles Outcome impact factor journals Outcome Scopus journals Outcome PubMed journals Outcome medical journals Outcome free journals Outcome best journals Outcome top journals Outcome free medical journals Outcome famous journals Outcome Google Scholar indexed journals Surgical Management articles Surgical Management Research articles Surgical Management review articles Surgical Management PubMed articles Surgical Management PubMed Central articles Surgical Management 2023 articles Surgical Management 2024 articles Surgical Management Scopus articles Surgical Management impact factor journals Surgical Management Scopus journals Surgical Management PubMed journals Surgical Management medical journals Surgical Management free journals Surgical Management best journals Surgical Management top journals Surgical Management free medical journals Surgical Management famous journals Surgical Management Google Scholar indexed journals Lumber Disc Prolapse articles Lumber Disc Prolapse Research articles Lumber Disc Prolapse review articles Lumber Disc Prolapse PubMed articles Lumber Disc Prolapse PubMed Central articles Lumber Disc Prolapse 2023 articles Lumber Disc Prolapse 2024 articles Lumber Disc Prolapse Scopus articles Lumber Disc Prolapse impact factor journals Lumber Disc Prolapse Scopus journals Lumber Disc Prolapse PubMed journals Lumber Disc Prolapse medical journals Lumber Disc Prolapse free journals Lumber Disc Prolapse best journals Lumber Disc Prolapse top journals Lumber Disc Prolapse free medical journals Lumber Disc Prolapse famous journals Lumber Disc Prolapse Google Scholar indexed journals disc bulge articles disc bulge Research articles disc bulge review articles disc bulge PubMed articles disc bulge PubMed Central articles disc bulge 2023 articles disc bulge 2024 articles disc bulge Scopus articles disc bulge impact factor journals disc bulge Scopus journals disc bulge PubMed journals disc bulge medical journals disc bulge free journals disc bulge best journals disc bulge top journals disc bulge free medical journals disc bulge famous journals disc bulge Google Scholar indexed journals disc prolapse articles disc prolapse Research articles disc prolapse review articles disc prolapse PubMed articles disc prolapse PubMed Central articles disc prolapse 2023 articles disc prolapse 2024 articles disc prolapse Scopus articles disc prolapse impact factor journals disc prolapse Scopus journals disc prolapse PubMed journals disc prolapse medical journals disc prolapse free journals disc prolapse best journals disc prolapse top journals disc prolapse free medical journals disc prolapse famous journals disc prolapse Google Scholar indexed journals L4-L5 articles L4-L5 Research articles L4-L5 review articles L4-L5 PubMed articles L4-L5 PubMed Central articles L4-L5 2023 articles L4-L5 2024 articles L4-L5 Scopus articles L4-L5 impact factor journals L4-L5 Scopus journals L4-L5 PubMed journals L4-L5 medical journals L4-L5 free journals L4-L5 best journals L4-L5 top journals L4-L5 free medical journals L4-L5 famous journals L4-L5 Google Scholar indexed journals disc herniation articles disc herniation Research articles disc herniation review articles disc herniation PubMed articles disc herniation PubMed Central articles disc herniation 2023 articles disc herniation 2024 articles disc herniation Scopus articles disc herniation impact factor journals disc herniation Scopus journals disc herniation PubMed journals disc herniation medical journals disc herniation free journals disc herniation best journals disc herniation top journals disc herniation free medical journals disc herniation famous journals disc herniation Google Scholar indexed journals posterior articles posterior Research articles posterior review articles posterior PubMed articles posterior PubMed Central articles posterior 2023 articles posterior 2024 articles posterior Scopus articles posterior impact factor journals posterior Scopus journals posterior PubMed journals posterior medical journals posterior free journals posterior best journals posterior top journals posterior free medical journals posterior famous journals posterior Google Scholar indexed journals intervertebral disc articles intervertebral disc Research articles intervertebral disc review articles intervertebral disc PubMed articles intervertebral disc PubMed Central articles intervertebral disc 2023 articles intervertebral disc 2024 articles intervertebral disc Scopus articles intervertebral disc impact factor journals intervertebral disc Scopus journals intervertebral disc PubMed journals intervertebral disc medical journals intervertebral disc free journals intervertebral disc best journals intervertebral disc top journals intervertebral disc free medical journals intervertebral disc famous journals intervertebral disc Google Scholar indexed journals Prolapsed lumbar intervert-ebral disc articles Prolapsed lumbar intervert-ebral disc Research articles Prolapsed lumbar intervert-ebral disc review articles Prolapsed lumbar intervert-ebral disc PubMed articles Prolapsed lumbar intervert-ebral disc PubMed Central articles Prolapsed lumbar intervert-ebral disc 2023 articles Prolapsed lumbar intervert-ebral disc 2024 articles Prolapsed lumbar intervert-ebral disc Scopus articles Prolapsed lumbar intervert-ebral disc impact factor journals Prolapsed lumbar intervert-ebral disc Scopus journals Prolapsed lumbar intervert-ebral disc PubMed journals Prolapsed lumbar intervert-ebral disc medical journals Prolapsed lumbar intervert-ebral disc free journals Prolapsed lumbar intervert-ebral disc best journals Prolapsed lumbar intervert-ebral disc top journals Prolapsed lumbar intervert-ebral disc free medical journals Prolapsed lumbar intervert-ebral disc famous journals Prolapsed lumbar intervert-ebral disc Google Scholar indexed journals
Article Details
1. Introduction
A disc herniation is the term given to any uneven out-pouching or bulging of the posterior region (back region) of the intervertebral disc as seen on MRI. The bigger the lumbar/sacral disc herniation, the more likely it is to cause back and/or leg pain--the later of which is called sciatica [1]. Though low back pain and sciatica had affected the human race since time immemorial, until the first quarter of previous century, little knowledge had been acquired about the ways in which the intervertebral disc might cause compression on intra-spinal neural structures. Disc prolapse occurs in the working age adult population as they are the ones most likely to be exposed to trauma due to mechanical stress and strain. The most likely reason for the earlier age of onset of symptoms of low back pain in our studies is the young age at which our people are exposed to manual labour due to their poor socio-economic condition. Gradually, as medicine advanced as a science, the number of speci-fic diagnosis capable of causing back and leg pain increased dramatically. A number of physical manoe-uvres were devised to isolate the true problem in each patient. The most notable of these is the Lasegue sign, or straight leg raising test, described by Forst in 1881 but attributed to Lasegue, his teacher. This test was devised to distinguish between hip disease and sciatica [2]. Prolapsed lumbar intervert-ebral disc (PLID) is an important cause of low back pain and it is one of the frequent cause of disability. Its frequency and annual tool of suffering and disability has been a constant stimulus for investigation in developed countries. Furthermore in Bangladesh a large number of people of working age are suffering from low back pain due to prolapse lumbar inter-vertebral disc. When conservative management fails, surgery is the only way to treat these patients and different surgical procedures are there. Microdisce-ctomy, Endoscopic discetomy, Laser discectomy is the operation of developed countries. The prolapsed intervertebral disc is usually seen in fit adults bet-ween the ages of 20 and 45, but they can also occur below the age of 20 years and elderly. Males suffer more from interverebral disc prolapse than females.
Almost in 80% of cases, the protrusion is traumatic in origin and there is either a history of sudden severe strain due to heavy weight lifting or patients occupation is one in which flexion strain must be resisted, such as packer, fireman, porter, etc [3]. In 20% of cases the condition is degenerative in origin. There is also a history of minor trauma. The precipit-ating factor, therefore, is mainly injury immediately or shortly before the onset of a symptom. Since the mechanism demands the combination of stress and mobility, the disc herniations commonly occur at a site where a relatively rigid segment of the spine join a flexible segment, which are subjected to greater stress and mobility. Hence, in the lumbar region, the L4-L5 and L5-S1 discs are most often affected. The standard procedure for disc removal was total laminectomy followed by a transdural approach to the disc. In 1939, Semmes presented a new procedure to remove the ruptured intervertebral disc that included subtotal laminectomy and retraction of the dural sac to expose and remove the ruptured disc with the patient under local anaesthesia [4]. This proce-dure is now the classic approach for removal of the intervertebral disc. Finally through the anatomic dissections and clinical observations, spinal ageing and the development of pathologic process associated with or complication the process of ageing have evolved as a primary theory in disc disease [5]. To evaluate the surgical outcome in the treatment of Lumber Disc Prolapse (LDP).
2. Materials and Methods
The prospective interventional study (Quasi exper-imental) was done in the Department of Orthopa-edics and Traumatology, Dhaka Medical College and Hospital during the period of June 2009 to July 2011(2 years). Due to time limitation and financial constraint only 35 cases were selected during study period but out of them 29 cases were feasible to be included in the study, remaining 6 cases were lost during follow up. Patients of both sexes aged between 18-70 years with prolapsed lumber intervertebral disc admitted in the Department of Orthopedics and Traumatology were included as purposive sampling.
Moreover, following variables were studied for clinical evaluation Level of involvement, side of involvement, X-ray of lumber spine, MRI of lumbar spine, Relief of rediculopathy, Gait, strai-ght leg raising (SLR), muscle power, sensory deficit, Complications: Root injury, dural tear, discitis, Functional outcome variables: Pain status, relief of presenting symptoms, mobility of spine, return to work, level of activity.Data were collected, complied and tabulated according to key variables. The analysis of different variables was done according to standard statistical analysis by using SPSS. A total of 29 patients with prolapsed lumbar intervertebral disc were operated and followed up routinely. The main objective of the study was to evaluate the prognosis of management of prolapsed lumbar intervertebral disc by lami-notomy and discectomy. The result of laminotomy and discectomy was evaluated by using Modified Macnab outcome criteria (Macnab, 1971).
|
Result |
Criteria |
|
Excellent |
No pain, no restriction of mobility; return to work and level of activity. |
|
Good |
Occasional nonradicular pain; relief of presenting symptoms; able to return to modified work. |
|
Fair |
Some improved functional capacity; still handicapped and unemployed |
|
Poor |
Continued objective symptoms of root involvement: additional operative intervention needed at the index level irrespective of length of postoperative follow up. |
2.1 Inclusion criteria
- Signs of root compression-Sensory, Motor, Reflex.
- Deteriorating signs and symptoms of patie-nts of PLID where leg pain is dominant than
- back pain
- Restricted straight leg raising test with Positive MRI findings refractory to 2-3 weeks of conservative treatment.
2.2 Exclusion criteria
- PLID associated with other spinal pathology e.g. spinal tumor, infection, inflammation etc.
- Repeat lumbar disc surgery due to recurrence of symptoms
- PLID due to direct trauma with fracture-dislocation of vertebra.
- PLID with Cauda-equina Syndrome
3. Results
The mean age of the patients were 38.9 ± 14.0 years ranging from 20-67 years. The mean age of the male patients was 38.5 ± 13.5 years and a female patient was 39.8 ± 16.2 years. Though the mean age of the female patients a little bit higher than the male, but the mean difference was not statistically significant (p>0.05). Data indicated that maximum number of the patients was in age group >40 years (41.4%) followed by 27.6% in the age group 21-30 years, 24.1% in the age group 31-40 years and 6.9% were in the age group <20 years. Clinical examination of the patients indicated that 14(48.3%) had sensory deficit at the level of L5 and 6(20.7%) of patients had sensory deficit at level S1. However, 9(31.0%) patients had intact sensory function. Out of 29 patients, 16(55.2%) had disc prolapse at level L4-L5, 10(35.5%) had at L5-S1, 2(6.9%) had L4-L5 and L5-S1 level and 1(3.4%) patient had disc herniation at L4-L5 and L3-L4.
29 patients had 32 disc prolapse, because 3 patients had two level disc prolapse. It was found that more than half of the disc 17(53.1%) was found on left side, 3(9.4%) on right side and 12(37.5% was found centrally. The mean pain score was 3.0 ± 0.0 preoperatively, 1.79 ± 0.62 during 1st visit, 1.07 ± 0.84 during 2nd visit and 0.24 ± 0.64 during 3rd visit. Repeated measure one way analysis of variance showing that pain significantly decreased from preoperative to 1st visit (p<0.001) and also decreased significantly from 1st visit to 2nd visit and subsequent visit (p<0.005) shown as marginal estimated mean score. It was found that all of patients had preoperative muscle spasm. However, at 1st visit muscle spasm decreased to 20.7% and at 2nd visit it was only 10.3%. However, only 1(3.4%) patient had muscle spasm at 3rd visit. Repeated measure analysis of variance indicated that muscle spasm significantly decreased from 1st to 2nd visit it was only 10.3%. However, no statistically significant difference of muscle spasm was found between 2nd and 3rd visit (P>0.05). Similar to muscle spasm it was found that all of the patients had restricted mobility of the spine. However, following 1st and subsequent visit, it significantly improved from 3.4% to 72.4% (P<0.323). At 3rd visit only 1(3.4%) patients had restricted mobility. All the patients were examined for straight leg raising (SLR) on supine position. Preoperatively, the SLR was 42.6 ± 6.3 degree. However, following operation the SLR significantly improved from baseline 89.3 ± 2.6 at 3rd visit. Subjective assessment of patients indicated that majority (72.4%) had excellent function outcome followed by 17.2% had good functional outcome and (6.9%) had fair outcome. However, (3.4%) of patients had poor functional outcome.
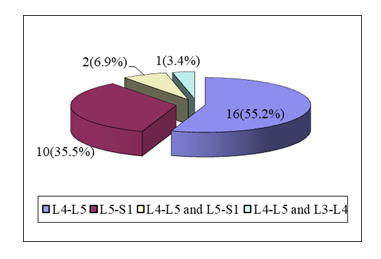
Figure 1: Pie diagram showing the level of disc herniation (n=29).
|
Stage |
Pain score |
Mean ± SD |
P value |
|
Pre-operative |
Absent (0) |
3.00 ± 0.0 |
|
|
1st visit |
Occasional (1) |
1.79 ± 0.62 |
0.001s |
|
2nd visit |
Mild (2) |
1.07 ± 0.84 |
0.001s |
|
3rd visit |
Moderate (3) |
0.24 ± 0.64 |
0.001s |
Table 1: Repeated measure of analysis of variance of pain score in different visits (n=29).
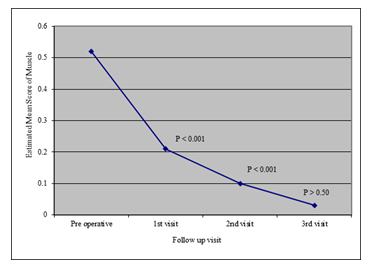
Figure 2: Repeated measure of analysis of variance of Muscle spasm in different visits (n=29).
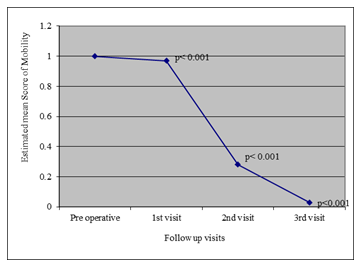
Figure 3: Line diagram showing estimated mean score of mobility in different visit.
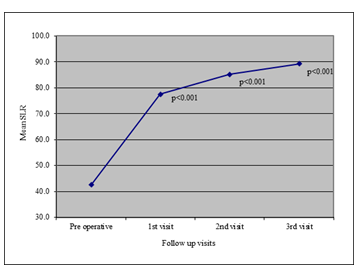
Figure 4: Line diagram showing mean distribution of SLR in different visit.
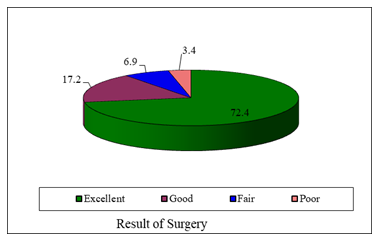
Figure 5: Pie diagram showing the distribution of the patients by subjective assessment of functional outcome (n=29).
4. Discussion
Low back pain commonly afflicts the adult population all over the world. It is of prime importance that the cause of low back pain is diagnosed in its early stage since not all cases are innocent [6]. The syndrome where the diagnosis is not in doubt is when root pain extends below the knee (radiculopathy) [7]. The commonest cause of radicular pain is lumbar disc prolapse. Prior to embarking on surgery for a lumbar disc prolapse it should be recalled that the long-term natural history for such a patient is likely to be good and that many radiologically proven discs may become or remain asymptomatic [8, 9, 10]. Moreover, the outcome of surgical therapy for lumbar disc prolapse was compared to conservative therapy, at six months there was no statistical difference between the two groups [11]. By seven years follow up the surgically treated group had faired better, only in that they had had less episodes of low back pain and had lost less time from work. In a similar study, it was found that at one year the surgical group had faired much better with 92% good results as compared with 60% in the non-surgical group [12]. However, at both four and ten year follow-up there was again no statistical difference between the two groups. It does seem, therefore, that many lumbar disc problems ameliorate by themselves eventually and that the role of surgery may serve only to hasten that final recovery. Although there is no such comparative study in our country, it can be safely assumed that with the improvement of imaging and surgical techniques, the diagnosis and treatment of lumbar disc prolapses around the world has become more uniform. The key to good results in disc surgery is appropriate patient selection. In this study of 45 cases, those patients were selected who fulfilled the criteria for surgical treatment as in other national and international series. Plain X-ray of the lumbar spine is not diagnostic of prolapsed disc. It is done to exclude other pathology like congenital anomaly, spondylolisthesis, tubercul-osis and spinal tumours in some cases. Some studies reported narrow disc space in 49% of patients at L5/S1 level with positive operative findings of prolapsed disc at that level [13]. In 35% of cases there was narrow disc space at L4/5 level in X-ray but prolapse was found in only 14% of cases. Nabi et al (1982) observed narrow disc space 38.57% in their study [14]. In the present series more than one fourth (27.6%) of the cases showed diminished disc space. There was transitional vertebrae in 20.7% cases, loss of lumbar lordosis in 69.0% cases and 10.3% had marginal osteophytes. In MRI of lumbar spine show-ed 61.5% of patients had postero-lateral disc bulge and 37.5% had posterior disc bulge.
In various studies it was reported that 65.2% patients had prolapse at L4/5 level, 22.4% at L5/S1 level and 12.4% at L3/4 level [15]. Khan et al. (1991) observed in their study that 57.25% patients had prolapse at L4/5 level, 34.78% at L4/5 level and 7.97% at L3/4 level [16]. In the present series it was found that among the 29 patients, there were in all 32 incidences of prolapsed disc. In other words, 3 patients had prolapses at two levels. 59.37% of the patients had prolapse at L4/5 level, 37.5% at L5/S1 level and 3.12% at L3/4 level. Lumbar disc prolapse is common at L4/5 level in this current series and in other published series. The 1.5 vertebra articulates with the S1 segment of the fixed sacrum. Therefore, most of the movement of the lumbar spine occurs at L4/5 disc level, which may be the cause of the high incidence of prolapse disc being found at L4/5 level. O’Connell et al. reported that 3.0% patients develop-ed wound infection, haematoma formation 2.0%, pulmonary embolism 1% and operative pain in the back and groin 1.6% [17]. In another study of 954 operations on 905 cases as thrombophlebitis in 5 patients, lung abscess in 1 patient, wound infection in 7 patients, pulmonary embolus (non-fatal) in 2 patients were reported [13]. Brown and Pont reported in their series of 570 cases-2 post-operative deaths, 6 postoperative superficial infection and 5 other complications e.g., one each of pulmonary infection, thrombophlebitis and CSF leak and, two cases of wound disruption [15]. In the present series there was per-operative dural tear in 2 cases and post-operative disc space infection in one case. The infection might be due to sharing of operations in a common opera-tion theatre due to the unavailability of a separate spinal surgery theatre. The two cases of dural tear was repaired by 4-0 vicryl and there were no postoperative CSF leakage. The case of discitis was managed conservatively by absolute bed rest, anti-biotics and analgesics. But the patient is not pain free till now. Various retrospective studies and some prospective studies showed good results range from 46% to 97%. Several points considered in the analysis of the results of lumbar disc surgery [16]. Patient selection appear to be extremely important. Regarding the subjective assessment of current study patients it was observed that most (75.9%) of the patients had excellent functional outcome, 13.8% good, 6.9% fair and 3.4% had poor functional out-come according to modified Macnab criteria.
4.1 Limitations of the study
This was a cross-sectional single centered observa-tory study with a small sample size of sample. So, the findings of this study may not reflect the exact scenario of the whole nation.
5. Conclusion and Recommendations
From this study it reveals that management of prolapsed lumbar intervertebral disc by laminotomy and discectomy is an effective method of treatment and it reduces the complications and increase the chances of successful outcome. This study was done on 29 patients, follow up period was 6-12 months. So, further study with larger sample size, longer follow up period required to delineate the outcome.
Funding
No funding sources.
Conflict of Interest
None declared.
Ethical Approval
The study was approved by the Institutional Ethics Committee.
References
- Ohtori S, Takahashi K, Chiba T, et al. Sensory innervation of the dorsal portion of the lumbar intervertebral discs in rats. Spine 26 (2001): 946-950.
- Fairbank J C T, Couper J, Davies J B. The Oswestry low Back Pain Questionnaire. Physiotherapy 66 (1980): 271-273.
- Farfan HF, Huberdeath RM, Dubow HI. Lumbar intervertebral disc-degeneration. The influence of geometrical features on the pattern of disc degeneration. A post-mortem study. J. Bone Joint Surg 54 (1972): 492.
- Semmes RE. ‘Diagnosis of ruptured inter-vertebral discs without contrast myelo-graphy and comment upon recent experience with modified hemilaminectomy for their removal’. Yale J. Biol. Med 11 (1989): 433.
- Kirkaldy Willis WH, Hill RJ. A more precise diagnosis for low back pain. Spine 4 (1979): 102.
- Raff J. Some observation regarding 905 patients operated upon for protruded lumbar intervertebral disc. Amer. J. Surg 97 (1959): 388.
- Wiltse LL. History of lumbar spine surgery (1956).
- Wiesel SW, Tsourmas N, Fiffer HL, et al. A study of computed assisted tomography: Part I: The incidence of positive CAT scans in an asymptomatic group of patients. Spine 9 (1984): 549.
- Ohtori S. Sensory innervation of the dorsal portion of the lumbar intervertebral disc in rats. Spine 24 (1999): 2295-2299.
- Bowden S, Davis D, Dina T, et al. The incidence of abnormal lumbar spine MRI scans in asymptomatic patients’. J. Neuro-surg 41 (1989): 33.
- Hakelius A. Progress in sciatica: a clinical follow up of surgical and non-surgical treat-ment. Acta Orthop. Secand 129 (1970): 1.
- Weber H. Lumbar disc herniation: a controlled prospective study with ten yeares of observation. Spine 8 (1983): 131.
- Hiselberger W, Witten R. Abnormal myelo-grams in asymptomatic patients. J.Neuro-surg 28 (1967): 204.
- Nabi N Iskander, Chowdhury AB. Lamin-ectomy in prolapsed intervertebral disc (Lumbar). J. Bangladesh Orthop. Society 2 (1982): 6.
- Brown HA, Pont E. Disease of lumbar disc. J.Neurosurg 20 (1963): 410.
- Carragee EJ, Han MY, Yang B. Activity restrictions after posterior lumbar disce-ctomy. A prospective study of outcomes in 152 cases with no postoperative restrictions. Spine 24 (1999): 2346-2351.
- Khan, Rahman AAML, Ali MI, et al. Prolapsed intervertebral disc. Surgical management of 142 cases: Bangladesh. J. Neuroscience 7 (1991): 53.
