Outcome of Infragenicular Prosthetic Grafts with and without Distal Anastomotic Modification - A Retrospective Single Center Study
Article Information
Abhay Setia1*, Omid Yousefi1, Patrick Felix Samp2, Peter Knez3, Farzin Adili1
1Department of Vascular Medicine, Division of Vascular and Endovascular Surgery, Klinikum Darmstadt, Darmstadt, Germany
2Department of Neuroradiology, Goethe-University Medical Center, Frankfurt am Main, Germany
3Department of Vascular Surgery, Klinikum Wetzlar, Wetzlar, Germany
*Corresponding Author: Abhay Setia, Department of Vascular Medicine, Division of Vascular and Endovascular Surgery, Klinikum Darmstadt, Grafenstraße 9, 64283, Darmstadt, Germany
Received: 08 May 2022; Accepted: 16 May 2022; Published: 02 June 2022
Citation: Abhay Setia, Omid Yousefi, Patrick Felix Samp, Peter Knez, Farzin Adili. Outcome of Infragenicular Prosthetic Grafts with and without Distal Anastomotic Modification- A Retrospective Single Center Study. Journal of Surgery and Research 5 (2022): 332-345.
View / Download Pdf Share at FacebookAbstract
Background
Peripheral revascularization with below-knee bypass (REBEL) utilizing prosthetic grafts demonstrate inferior patency and amputation-free survival rates, as compared to venous conduits. Because of improved hemodynamics, adding a venous modification to distal anastomoses in REBEL with prosthetic grafts is assumed to improve both patency and amputation-free survival. The aim of this study was to assess the performance of prosthetic grafts with and without venous modifications of the distal anastomosis (MOD) and compare the results with venous conduits, in terms of patency rates, amputation prevention and survival.
Methods
The present single center retrospective, non-randomized observational study involved 221 REBEL in 201 patients. Data was collected by viewing hospital records and follow-up clinical and duplex ultrasound examinations (up to 48 months). For analysis, the patients were divided in 3 groups; REBEL using prosthetic grafts with MOD (PGY) or without (PGN) anastomotic modification and REBEL using plain venous conduits without anastomotic modifications (VG). Primary patency, assisted primary patency, secondary patency, amputation-free survival and overall survival was analyzed.
Results
The median follow-up was 27 months. The most common site of distal anastomosis in PGY were the crural arteries (77.8%) and 50% of PGY patients had already undergone vein-harvesting for peripheral revascularization. Average duration of surgery for PGY was 284 minutes, >70 minutes more as compared to PGN (p=0,001). In PGY a statistically insignificant tendency to decreased primary and secondary patency rates as compared to PGN was observed at 12 and 36 months. PGY displayed a significant lower amputation-f
Keywords
Peripheral arterial obstructive disease, Below-knee revascularization, Prosthetic grafts, Venous modifications of distal anastomosis, Venous conduits, Amputation-free survival
Peripheral arterial obstructive disease articles; Below-knee revascularization articles; Prosthetic grafts articles; Venous modifications of distal anastomosis articles; Venous conduits articles; Amputation-free survival articles
Peripheral arterial obstructive disease articles Peripheral arterial obstructive disease Research articles Peripheral arterial obstructive disease review articles Peripheral arterial obstructive disease PubMed articles Peripheral arterial obstructive disease PubMed Central articles Peripheral arterial obstructive disease 2023 articles Peripheral arterial obstructive disease 2024 articles Peripheral arterial obstructive disease Scopus articles Peripheral arterial obstructive disease impact factor journals Peripheral arterial obstructive disease Scopus journals Peripheral arterial obstructive disease PubMed journals Peripheral arterial obstructive disease medical journals Peripheral arterial obstructive disease free journals Peripheral arterial obstructive disease best journals Peripheral arterial obstructive disease top journals Peripheral arterial obstructive disease free medical journals Peripheral arterial obstructive disease famous journals Peripheral arterial obstructive disease Google Scholar indexed journals Below-knee revascularization articles Below-knee revascularization Research articles Below-knee revascularization review articles Below-knee revascularization PubMed articles Below-knee revascularization PubMed Central articles Below-knee revascularization 2023 articles Below-knee revascularization 2024 articles Below-knee revascularization Scopus articles Below-knee revascularization impact factor journals Below-knee revascularization Scopus journals Below-knee revascularization PubMed journals Below-knee revascularization medical journals Below-knee revascularization free journals Below-knee revascularization best journals Below-knee revascularization top journals Below-knee revascularization free medical journals Below-knee revascularization famous journals Below-knee revascularization Google Scholar indexed journals Prosthetic grafts articles Prosthetic grafts Research articles Prosthetic grafts review articles Prosthetic grafts PubMed articles Prosthetic grafts PubMed Central articles Prosthetic grafts 2023 articles Prosthetic grafts 2024 articles Prosthetic grafts Scopus articles Prosthetic grafts impact factor journals Prosthetic grafts Scopus journals Prosthetic grafts PubMed journals Prosthetic grafts medical journals Prosthetic grafts free journals Prosthetic grafts best journals Prosthetic grafts top journals Prosthetic grafts free medical journals Prosthetic grafts famous journals Prosthetic grafts Google Scholar indexed journals Venous modifications of distal anastomosis articles Venous modifications of distal anastomosis Research articles Venous modifications of distal anastomosis review articles Venous modifications of distal anastomosis PubMed articles Venous modifications of distal anastomosis PubMed Central articles Venous modifications of distal anastomosis 2023 articles Venous modifications of distal anastomosis 2024 articles Venous modifications of distal anastomosis Scopus articles Venous modifications of distal anastomosis impact factor journals Venous modifications of distal anastomosis Scopus journals Venous modifications of distal anastomosis PubMed journals Venous modifications of distal anastomosis medical journals Venous modifications of distal anastomosis free journals Venous modifications of distal anastomosis best journals Venous modifications of distal anastomosis top journals Venous modifications of distal anastomosis free medical journals Venous modifications of distal anastomosis famous journals Venous modifications of distal anastomosis Google Scholar indexed journals Venous conduits articles Venous conduits Research articles Venous conduits review articles Venous conduits PubMed articles Venous conduits PubMed Central articles Venous conduits 2023 articles Venous conduits 2024 articles Venous conduits Scopus articles Venous conduits impact factor journals Venous conduits Scopus journals Venous conduits PubMed journals Venous conduits medical journals Venous conduits free journals Venous conduits best journals Venous conduits top journals Venous conduits free medical journals Venous conduits famous journals Venous conduits Google Scholar indexed journals Amputation-free survival articles Amputation-free survival Research articles Amputation-free survival review articles Amputation-free survival PubMed articles Amputation-free survival PubMed Central articles Amputation-free survival 2023 articles Amputation-free survival 2024 articles Amputation-free survival Scopus articles Amputation-free survival impact factor journals Amputation-free survival Scopus journals Amputation-free survival PubMed journals Amputation-free survival medical journals Amputation-free survival free journals Amputation-free survival best journals Amputation-free survival top journals Amputation-free survival free medical journals Amputation-free survival famous journals Amputation-free survival Google Scholar indexed journals alloplastic bypass grafts articles alloplastic bypass grafts Research articles alloplastic bypass grafts review articles alloplastic bypass grafts PubMed articles alloplastic bypass grafts PubMed Central articles alloplastic bypass grafts 2023 articles alloplastic bypass grafts 2024 articles alloplastic bypass grafts Scopus articles alloplastic bypass grafts impact factor journals alloplastic bypass grafts Scopus journals alloplastic bypass grafts PubMed journals alloplastic bypass grafts medical journals alloplastic bypass grafts free journals alloplastic bypass grafts best journals alloplastic bypass grafts top journals alloplastic bypass grafts free medical journals alloplastic bypass grafts famous journals alloplastic bypass grafts Google Scholar indexed journals Kaplan-Meier-survival curves articles Kaplan-Meier-survival curves Research articles Kaplan-Meier-survival curves review articles Kaplan-Meier-survival curves PubMed articles Kaplan-Meier-survival curves PubMed Central articles Kaplan-Meier-survival curves 2023 articles Kaplan-Meier-survival curves 2024 articles Kaplan-Meier-survival curves Scopus articles Kaplan-Meier-survival curves impact factor journals Kaplan-Meier-survival curves Scopus journals Kaplan-Meier-survival curves PubMed journals Kaplan-Meier-survival curves medical journals Kaplan-Meier-survival curves free journals Kaplan-Meier-survival curves best journals Kaplan-Meier-survival curves top journals Kaplan-Meier-survival curves free medical journals Kaplan-Meier-survival curves famous journals Kaplan-Meier-survival curves Google Scholar indexed journals
Article Details
1. Introduction
Since the first successful creation of a bypass graft for the treatment of peripheral arterial occlusive disease (PAOD) by Jean Kunlin in 1948, techniques for peripheral revascularization have come a long way [1]. Notwithstanding the recent evolution and implementation of endovascular procedures and strategies calling for the first line use of interventional recanalization, surgical revascularization by means of bypass grafting still bodes its merits, particularly for complex lesions of the superficial femoral (SFA), popliteal and crural arteries [2]. For revascularization of below knee arteries (REBEL), the ipsilateral greater saphenous vein (GSV) remains the conduit of choice [3,4]. However, prosthetic grafts still play an important role in cases where suitable autogenous veins are not available. Yet, diameter and compliance mismatch as well as technical difficulties to surgically connect a relatively rigid graft to a delicate, calcified, low flow crural artery pose a significant obstacle to satisfactory mid- and long-term outcome. Modelling of the distal anastomosis using various cuff-techniques was thought to simplify the surgical procedure and improve patency of alloplastic bypass grafts. Since the outcome of cuff techniques still remains unsettled, the present study was devised to assess the function of prosthetic grafts with and without modification of the distal anastomosis (MOD) as compared to the use of plain venous conduits.
2. Materials and Methods
This single center, retrospective, non-randomized, observational study (approved by the ethics committee of the medical council in Hessen) was carried out in patients undergoing REBEL for the treatment of PAOD or peripheral aneurysms (PA) from April 2009 to April 2013. This retrospective analysis involved 221 REBEL in 201 patients. Patients undergoing REBEL after trauma or embolic episodes without PAOD or PA and patients with distal anastomosis proximal to the P3 Segment of the popliteal artery were excluded from the study. Hospital records were reviewed to collect the data. Follow-up was planned and performed prospectively for up to 48 Months by means of clinical examination and/or by phone and was aided by duplex examination (GE LogiQ7, GE Healthcare, USA). A written consent was obtained from all patients or their legal representatives before enrolment into the study. The following parameters were tabulated (Microsoft Excel, Redmond, WA, USA) and analyzed: Patients’ demographics, comorbidities, Fontaine and Rutherford categorization, ankle brachial index (ABI), duplex ultrasound findings, angiographic findings, intraoperative details (operative time, localization of the proximal and distal anastomosis, bypass material and diameter, location of the anastomosis and MOD if present) were recorded and tabulated (Microsoft Excel, Redmond, WA, USA). REBEL were categorized based on the type of graft and distal anastomosis modifications. The three categories were autogenous venous graft (VG), prosthetic graft without MOD (PGN) and with MOD (PGY). Data analysis: Survival, limb salvage and patency rates were analyzed by Kaplan-Meier-survival curves with log-rank test. IBM SPSS 22.0 (Armonk, NY: IBM Corp.) was used for data analysis
3. Results
The median follow-up was 27 months. In 23 patients the data records were complete for the planned follow-up. Follow-up clinical and duplex ultrasound examinations were performed in 70 patients and 84 bypass grafts. Thirty-two patients were followed up by phone. Sixty-five patients succumbed during the planned follow-up period. Eleven patients were lost to follow-up. The patients’ demographics and comorbidities are illustrated in table 1. The number of males in VG and PGN was statistically higher (Pearson-Chi2-Test; p<0,005). Age distribution was comparable in the three groups (Kruskal-Wallis-Test; p=0,271). There was no significant difference in the presence of individual risk factors in the three groups. Hypertension and hyperlipidemia were the most frequently occurring risk factors. All patients underwent preoperative venous mapping with the help of duplex ultrasound. Out of 48 patients with aneurysm, 23 were asymptomatic and 25 were symptomatic. Most of the patients presented with critical limb ischemia (rest-pain n=44 and tissue loss n=146). Only 8 patients underwent REBEL for lifestyle limiting claudication.
3.1 Intraoperative details
The reasons for opting for a prosthetic graft (n=62) were; small vein caliber <3mm (n=30), vein already harvested for a peripheral (n=23) or coronary bypass (n=7) surgery or varicose veins (n=2). Venous grafts were used in both reversed (n=147/159) and non-reversed (12/159) techniques. MOD in the PGY group are depicted in figure 1. Kruskal-Wallis-Test showed a significant difference (p=0.001) in the distribution of operative time for the three groups. PGN group had significantly higher number of REBEL with operative time <180mins and lower number of REBELs with operative time >300 mins as compared to the PGY group (Pearson-chi2 Test p=0.015). This is in coherence with expectations that revascularization with venous graft and MOD would be more time consuming.
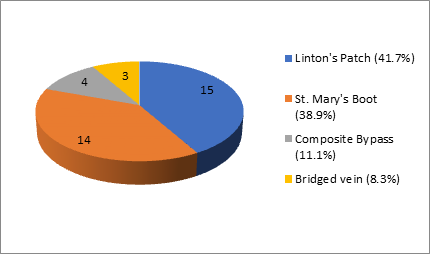
Figure 1: Distribution of type of Venous modifications of distal anastomosis (MOD).
|
PGN |
PGY |
VG |
Total |
|||||
|
Patients |
26 |
33 |
142 |
201 |
||||
|
REBEL |
26 |
36 |
159 |
221 |
||||
|
Average age in years (range) |
73.2 (56-85) |
75.6 (57-92) |
71.9 (39-89) |
72.6 (39-92) |
||||
|
Median age |
72 |
74 |
73 |
73 |
||||
|
Indication for REBEL |
PAOD |
PA |
PAOD |
PA |
PAOD |
PA |
PAOD |
PA |
|
21 |
5 |
33 |
3 |
119 |
40 |
173 |
48 |
|
|
Sex distribution |
Females |
Males |
Females |
Males |
Females |
Males |
Females |
Males |
|
Number (%) |
8 (30.8) |
18 (69.2) |
16 (48.5) |
17 (51.5) |
30 (21.1) |
112 (78.9) |
54 (26.9) |
147 (73.1) |
|
Risk factors (%) |
||||||||
|
DM |
7 |
12 |
64 |
83 (41.3%) |
||||
|
Smoking |
15 |
14 |
68 |
97 (48.2%) |
||||
|
CAD |
14 |
15 |
54 |
83 (41.3%) |
||||
|
Hypertension |
24 |
31 |
123 |
178 (88.5%) |
||||
|
RI |
8 |
10 |
39 |
57 (28.3%) |
||||
|
Hyperlipidaemia |
18 |
24 |
92 |
134 (66.7%) |
||||
REBEL: revascularization of below knee arteries
PGN: prosthetic graft without MOD
PGY: prosthetic graft with modification of the distal anastomosis (MOD)
VG: autogenous venous graft REBEL
PAOD: peripheral arterial occlusive disease
PA: peripheral aneurysms
DM: Diabetes mellitus
CAD: Coronary artery disease
RI: Renal insufficiency
Table 1: Patients’ demographics and comorbidities.
3.2 Postoperative results
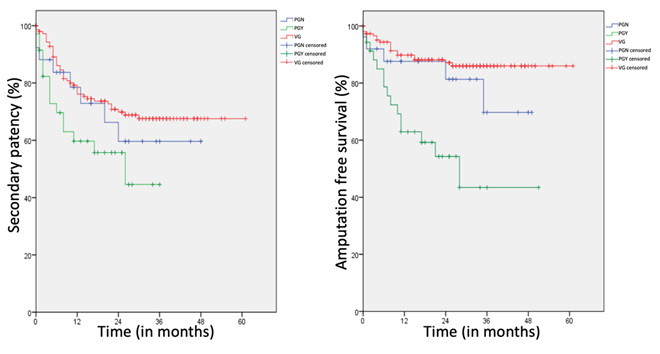
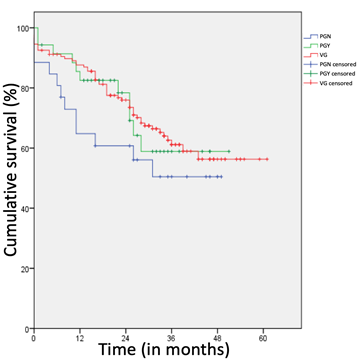
All the patients belonging to the PGN und PGY group were prescribed postoperative antiplatelet drugs (AP). Only 12 patients in the VG didn’t receive any AP but these patients received oral anticoagulants (OAK). 55.6% of patients (n=20/36) in the PGY group received a combination of AP and OAK. This was significantly higher (p=0.05) as compared to the PGN (n=8/26) and the VG (n=53/159) group. Log-rank-test showed no significant difference regarding the primary patency, the assisted patency rates and the cumulative survival between the 3 groups (Figure 2, Table 3, Supplemental Figure 1) at 12 and 36 months. Comparison of the three groups in reference to secondary patency rate at 36 months, revealed a p-value of 0,058. However, paired-log-rank test showed a significant difference in the secondary patency rates (Figure 3) between the VG and PGY (p=0,017) group but this was insignificant (p=0,316) between the PGN and PGY group. There was a significant difference in the amputation free survival between the three groups at 48 months (Log-rank-test p<0.001) (Figure 3). The patients in PGY group showed significantly inferior amputation free survival as compared to VG and PGN at 48 months (p<0,001 and p=0,038).
PGN: prosthetic graft without MOD
PGY: prosthetic graft with modification of the distal anastomosis (MOD)
VG: autogenous venous graft REBEL
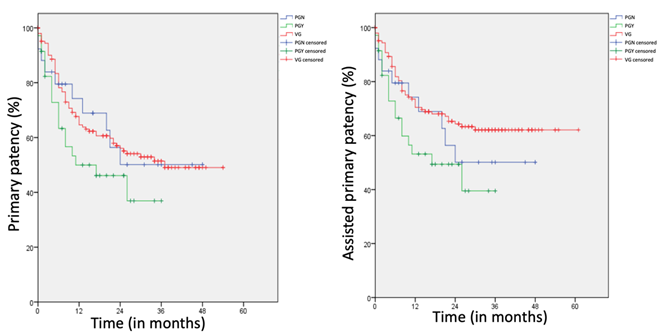
Figure 2: Kaplan-meier plots. No significant difference for primary patency (p=0.226; left) and assisted primary patency (p=0.074; right) between the three groups.
|
Segment for proximal anastomosis |
PGN (n=26) |
PGY (n=36) |
VG (n=159) |
|
External iliac A. (%) |
- |
1 (2.8) |
- |
|
Common femoral A. (%) |
17 (65) |
28 (77.8) |
75 (47.2) |
|
Superficial femoral A. (%) |
4 (15.4) |
2 (5.6) |
25 (15.7) |
|
Deep femoral A. (%) |
1 (3.8) |
3 (8.3) |
6 (3.8) |
|
Popliteal A. (P1) (%) |
4 (15.4) |
1 (2.8) |
37 (23.3) |
|
Popliteal A. (P3) (%) |
- |
- |
14 (8.8) |
|
Crural Arteries (%) |
- |
1 (2.8) |
2 (1.2) |
|
Segment for distal anastomosis |
|||
|
Popliteal A. (P3) (%) |
18 (69.2) |
8 (22.2) |
68 (42.8) |
|
Crural Arteries (%) |
8 (30.8) |
28 (77.8) |
83 (52.2) |
|
Dorsalis pedis A. (%) |
- |
- |
8 (5) |
|
Graft characteristics |
|||
|
Hb-ePTFE (%) |
25 (96.2) |
32 (89) |
- |
|
Omniflow® (%) |
1 (3.8) |
4 (11) |
- |
|
GSV (%) |
- |
- |
146 (91.8) |
|
SSV (%) |
- |
- |
2 (1.3) |
|
> 2Veins |
- |
- |
11 (6.9) |
|
Operative Time |
|||
|
Average time in mins (range) |
212 (117-391) |
284 (178-502) |
285 (131-642) |
|
Median time in mins |
209 |
265 |
262 |
|
<180 mins (n) |
8 |
2 |
17 |
|
180-300 mins (n) |
13 |
18 |
91 |
|
>300 mins (n) |
5 |
16 |
51 |
PGN: prosthetic graft without MOD
PGY: prosthetic graft with modification of the distal anastomosis (MOD)
VG: autogenous venous graft REBEL
REBEL: revascularization of below knee arteries
Hb-ePTFE: Heparin-bonded expanded polytetrafluoroethylene grafts
GSV: Great saphenous vein
SSV: Small saphenous vein
Mins: minutes
Table 2: Intraoperative details
PGN: prosthetic graft without MOD
PGY: prosthetic graft with modification of the distal anastomosis (MOD)
VG: autogenous venous graft REBEL
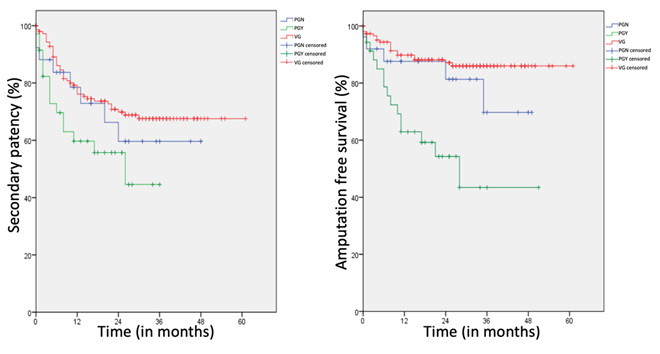
Figure 3: Left: Kaplan-meier plots for secondary patency. Significant difference (p=0.017) between VG and PGY but no significant between PGY and PGN (p=0.316); Right: Kaplan-meier plots for amputation free survival. Significant difference between the three groups (p<0.001).
|
Months |
1 |
12 |
24 |
36 |
48 |
|
Primary patency rates (%) |
|||||
|
PGN |
88.1 |
74.2 |
50.1 |
50.1 |
50.1 |
|
PGY |
91.4 |
50.1 |
46.1 |
36.9 |
- |
|
VG |
95.1 |
64.6 |
56.1 |
51.4 |
49 |
|
Assisted primary patency rates (%) |
|||||
|
PGN |
88.1 |
74.2 |
50.1 |
50.1 |
50.1 |
|
PGY |
91.4 |
53.2 |
49.4 |
39.5 |
- |
|
VG |
95.1 |
70.4 |
64.3 |
62.1 |
62.1 |
|
Secondary patency rates (%) |
|||||
|
PGN |
88.1 |
78.5 |
59.6 |
59.6 |
59.6 |
|
PGY |
91.4 |
59.7 |
55.7 |
44.6 |
- |
|
VG |
97.9 |
76.1 |
69.9 |
67.5 |
67.5 |
|
Amputation free survival (%) |
|||||
|
PGN |
92 |
87.6 |
81.3 |
69.7 |
69.7 |
|
PGY |
95.3 |
62.9 |
54.3 |
43.4 |
43.4 |
|
VG |
97.3 |
89.8 |
87.1 |
86 |
86 |
|
Survival (%) |
|||||
|
PGN |
88.5 |
64.8 |
60.7 |
50.5 |
50.5 |
|
PGY |
94.3 |
82.5 |
78.4 |
58.9 |
58.9 |
|
VG |
92.5 |
87.6 |
76 |
61.1 |
56.3 |
REBEL: revascularization of below knee arteries
PGN: prosthetic graft without MOD
PGY: prosthetic graft with modification of the distal anastomosis (MOD)
VG: autogenous venous graft REBEL
Table 3: Patency rates and survival rates in patients undergoing REBEL (in months)
4. Discussion
Despite advancements in the field of endovascular surgery, bypass surgery is an absolute essential part of vascular surgeons’ armamentarium. Regardless the superiority of venous conduit [3,4], prosthetic grafts are a viable alternative when the vein is disadvantageous [5], for e.g. in cases of small vein caliber, varicose veins or thrombophlebitis or unavailability because of previous harvesting for coronary or peripheral bypass [6]. The initial results of infrapopliteal revascularizations with prosthetic grafts were poor as compared to venous conduits [7-9]. Several strategies have been utilized to improve the performance and patency of prosthetic grafts. Some of these are: venous modifications of the distal anastomosis (MOD) [10,11,12,5], heparin bonding at the luminal surface of PTFE grafts (Hb-ePTFE, Propaten; W.L. Gore & Associates, Inc.) [13,14], distal AV-fistula [15] and grafts reinforced with rings [16]. MOD are advantageous in decreasing the intimal hyperplasia [17], by improving the flow characteristics [18] and reducing compliance-mismatch and shear stress [19] between relatively rigid prosthetic graft and undersized, delicate, calcified crural vessels. Experimental studies show that the intimal hyperplasia is most prominent at the transition between graft and MOD and least at the recipient artery [20]. This spares the artery in an acceptable state for a redo revascularization and may further improve the secondary patency rates [12]. The classical MOD were improved with time [21,22]. A boot shaped modification was described in 2000 and was known as St. Mary’s boot [23]. The distal vein patch technique (DVPT) showed acceptable long-term results in a series published by Neville et al. [11]. We performed the St. Mary’s boot (Supplemental Fig2). and the DVPT in 14 and 15 cases respectively. Holdsworth et al. [24] proposed a composite graft, where a segment of an autologous vein is anastomosed to a prosthetic graft and used for the distal anastomosis. We performed this technique in 4 patients. Bridged Bypass technique to improve the distal run-off and the compliance-mismatch was resorted to in 3 patients [25]. The median follow-up of 27 months was comparable to studies conducted by Daenens et al. and Pulli et al. [26,27]. The three groups (PGN, PGY and VG) in this study were comparable in terms of age (p=0,271) and comorbidities. PGN and VG had significantly higher number of male patients. The most common risk factors were Hyperlipidaemia and Hypertension [28,12]. In 94.5% of patients’ critical limb ischemia was the indication for REBEL. In SCAMICOS [29] pre-existing cardiac illness and previous vascular surgery were the most common risk factors and 94% patients suffered from either rest pain or ulcer or gangrene. In our study out of 48 aneurysm-patients, 25 were asymptomatic. Venous conduit for REBEL was used in 83% (n=40/48) aneurysm-patients. In 50% (n=17/36) of patients in PGY group, the vein had already been harvested for a peripheral reconstruction. This was 20% (n=5/26) in the PGN group. This difference was not significant (p=0,066) but indicates that more patients in PGY had already undergone previous peripheral bypass surgery. The most common site of distal anastomosis in PGN group was the P3 segment of poplitea artery (69%) and in PGY group the crural arteries (77%). This significant difference (p=0.002) suggests that PGY group patients the P3 segment was not adequate for distal anastomosis. This may have been because of previous surgery and/or stenting and/or occlusion due to diseased vessel. In 112 tibial bypass procedures presented by Neville et al (28), the patients with prosthetic graft bypass had a higher rate of prior bypass surgery. The time taken to accomplish REBEL in PGY group was significantly more (p=0,015) as compared to PGN group. Average duration of REBEL in PGY group was 284 minutes, comparable to VG group (average duration 285mins) but 72 minutes more as compared to the average for PGN group (p=0.001). The decision regarding the postoperative antithrombotic therapy was not standardized in our study and was dependent on surgeons’ preference, distal outflow, patients’ comorbidities and type of revascularization performed. More than 50% of patients in the PGY group received a combination of AP and OAK. This was significantly higher (p=0.05) as compared to the both PGN and VG group. Daenens et al. [26] administered 160mg of aspirin per day in the postoperative period. Warfarin anticoagulation was only given to patients who received it preoperatively and in redo venous bypass patients.
The patency rates can be compared with the help of Kaplan-meier plots (Figures 2,3). The primary patency rates for PGY vs PGN were 50% vs 74.2% at 12 months and 36.9% vs 50.1% at 36 months respectively. A similar trend was observed with the assisted primary patency rates. The difference between the PGY and PGN group for both primary patency (p=0,226) and assisted primary patency (p=0.74) was not significant. This may have been because of the relatively lower number of patients. A meta-analysis conducted by Albers et al. [9] revealed pooled 1- and 2-year primary patency rates of 59% and 48%, respectively, for standard ePTFE grafts used in infrapopliteal procedures. Neville et al. [28] performed 62 femoro-crural reconstructions with Hb-ePTFE and distal vein patch and reported a 1-year primary patency of 75.4%, as compared to 86% for venous grafts. The primary, assisted primary and secondary patency rates at 12 and 36 months for PGN group were comparable to VG (Table 3). The secondary patency rates at 12 and 36 months in PGY group were significantly inferior as compared to VG (59.7% vs 76.1% and 44.6% vs 67.5%; p=0.017) but were relatively inferior, even though not significant as compared to PGN group (59.7% vs 78.5% and 44.6% vs 59.6%; p=0.0316). A significantly higher rate of amputation was observed in the PGY group. Amputation-free Survival in PGY group was significantly lower at 12 (62.9% vs 87.6%; p=0.038) and at 48months (43.4% vs 69.75%; p<0.001) as compared to the PGN group. The three groups didn’t show any significant difference (p=0.375) in overall survival (Table 3, Supplemental Figure 1). In SCAMICOS (29) the primary patency at 36 months was 26% with MOD and 43% without MOD in femoro-popliteal reconstructions and 20% and 17% for femoro-crural reconstructions respectively. The amputation-free survival was better for the revascularizations with MOD both for femoro-popliteal and femoro-crural revascularizations, but this was not statistically significant. Similar to our study, the SCAMICOS [29] could not demonstrate any benefit of MOD for below knee revascularizations with PTFE. A meta-analysis [30] published in 2012 involving 885 patients with below-knee popliteal and crural bypasses. This metanalysis showed no significant improvement for primary patency or limb survival at 3 years for femoro-crural bypasses with venous cuff. In our study, we achieved good patency rates at 1 month (Table 3) for all three groups. These were better for the PGY group as compared to PGN, even though this was not statistically significant. This is an evidence of technical success and expertise of our surgeons. These findings are also in coherence with the reanalysis in the SCAMICOS cohort [31].
Keeping the abovementioned results in mind, we would like to indicate towards the fact that the patients undergoing REBEL with MOD suffer from advanced PAD with prior single or multiple revascularizations (surgical or endovascular). The surgery was more time consuming because of the site of distal anastomosis, possible dissection of the fine crural arteries, vein harvesting and MOD. Because of the poor limb salvage rates, patients undergoing REBEL with MOD would require anticoagulation in addition to AP and demand exhaustive perioperative vascular surgical care, monitoring and decision making.
Limitations of the study
In view of aforementioned results, it is difficult to interpret if MOD offer a significant improvement in the patency rates, survival or extremity salvage as compared to revascularizations with prosthetic grafts without MOD, counterwise the patients in PGY group were associated with higher amputation rates. Because of the retrospective and non-randomized design of the study, the three groups were not matched with respect to; the site of distal anastomosis and prior vascular surgeries or interventions. These factors posed a significant difference between PGN and PGY. The question if MOD is advantageous and offers better patency rates and survival can’t be answered until these confounding factors are matched. This study doesn’t document the outflow vessels after bypass surgery, which is an important factor in predicting the patency rates [32]. A prospective, randomized study with more patients should be able to shed light on this question.
Summary
For revascularization of below knee arteries (REBEL), autologous vein is the conduit of choice. In the absence or unsuitability of the vein, prosthetic grafts are recommendable. In the present study, adding a venous modification to the distal anastomosis failed to improve the performance of the prosthetic grafts and offered no advantage in terms of patency or amputation prevention. Surgery in PGY was more time consuming and most common site of distal anastomosis were the crural arteries. Significantly more patients with previous peripheral revascularization surgeries suggests that patients in PGY suffered from advanced PAOD. Nevertheless, in view of the technical difficulties to surgically anastomose a comparatively rigid, large caliber prosthetic graft to a delicate crural artery and flow-improving advantages of MOD [15,33], lower extremity revascularization in crural region with prosthetic grafts should be performed with MOD.
Author contributions
Conceiving and designing the study: AF, PS, PK
Collecting the data: AF, PS, PK
Analyzing and interpretation the data: AS, OY, AF, PS, PK
Writing the manuscript: AS, OY, AF
Statistical Analysis: AF, PS, AS, PK
Critical Revisions of the article: AS, OY, AF, PS, PK
Final approval of the article: AS, OY, AF, PS, PK
Overall responsibility: AS, OY, AF, PS, PK.
References
- Menzoian JO, Koshar AL, Rodrigues N. Alexis Carrel, Rene Leriche, Jean Kunlin, and the history of bypass surgery. J Vasc Surg. 54 (2011): 571-574.
- Balletshofer B, Ito W, Lawall H. et al. Positionspapier zur Diagnostik und Therapie der peripheren arteriellen Verschlusskrankheit (pAVK) bei Menschen mit Diabetes mellitus. Diabetologe 16 (2020): 65-73.
- Ambler GK, Twine CP. Graft type for femoro-popliteal bypass surgery. Cochrane Database of Systematic Reviews 2 (2018) : CD001487.
- Pereira CE, Albers M, Romiti M et al. Meta-analysis of femoropopliteal bypass grafts for lower extremity arterial insufficiency, Journal of Vascular Surgery 44 (2006): 510-517.
- Aracil-Sanus E. Infragenicular bypass graft for limb salvage using polytetrafluoroethylene and distal vein cuff as the first alternative in patients without ipsilateral greater saphenous vein. Ann Vasc Surg 19 (2005): 1-7.
- Chew DK, Owens CD, Belkin M et al. Bypass in the absence of ipsilateral greater saphenous vein: safety and superiority of the contralateral greater saphenous vein. J Vasc Surg 35 (2002): 1085-1092.
- Whittemore AD, Kent KC, Donaldson MC et al. What is the proper role of polytetrafluoroethylene grafts in infrainguinal reconstruction? J Vasc Surg 10 (1989): 299-305.
- Londrey GL, Ramsey DE, Hodgson KJ et al. Infrapopliteal bypass for severe ischemia: comparison of autogenous vein, composite, and prosthetic grafts. J Vasc Surg 13 (1991): 631-636.
- Albers M, Battistella VM, Romiti M et al. Meta-analysis of polytetrafluoroethylene bypass grafts to infrapopliteal arteries. J Vasc Surg. 37 (2003): 1263-1269.
- Neville RF, Sidaway AN. Myointimal hyperplasia: basic science and clinical considerations. Semin Vasc Surg 28 (1998): 143-148.
- Neville RF, Lidsky M, Capone A et al. An expanded series of distal bypass using the distal vein patch technique to improve prosthetic graft performance in critical limb ischemia. Eur J Vasc Endovasc Surg 44 (2012): 177-182.
- Raptis S, Miller JH. Influence of a vein cuff on polytetrafluoroethylene grafts for primary femoropopliteal bypass. Br J Surg 82 (1995): 487-491.
- Lindholt JS, Gottschalksen B, Johannesen N et al. The Scandinavian Propaten(®) trial - 1-year patency of PTFE vascular prostheses with heparin-bonded luminal surfaces compared to ordinary pure PTFE vascular prostheses - a randomized clinical controlled multi-centre trial. Eur J Vasc Endovasc Surg 41 (2011): 668-673.
- Dorigo W, et al. Results from an Italian multicentric registry comparing heparin bonded ePTFE graft and autologous saphenous vein in below-knee femoro-popliteal bypasses. J Cardiovasc Surg (Torino). 53 (2012): 187-194.
- Kreienberg PB, Darling RC III, Chang BB et al. Adjunctive techniques to improve patency of distal prosthetic bypass grafts: polytetrafluoroethylene with remote arteriovenous fistulae versus vein cuffs. J Vasc Surg 31 (2000): 696-701.
- Debus ES, Diener H, Larena-Avellaneda A. Postoperative Komplikationen in der Gefäßchirurgie. Chirurg 80 (2009): 814-826.
- Kissin M, Kansal N, Pappas PJ et al. Vein interposition cuffs decrease the intimal hyperplasia response of polytetrafluoroethylene bypass grafts. J Vasc Surg 31 (2000): 69-83.
- Beard JD, Benveniste GL, Miller JH et al. Hemodynamics of the interposition vein cuff. Br J Surg 73 (1986): 823-825.
- How TV, Rowe CS, Gilling-Smith GL et al. Interposition vein cuff anastomosis alters wall shear stress distribution in the recipient artery. J Vasc Surg 31 (2000): 1008-1017.
- Trubel W, Schima H, Czerny M et al. Experimental comparison of four methods of end-to-side anastomosis with expanded polytetrafluoroethylene. Br J Surg 91 (2004): 159-167.
- Miller JH, Foreman RK, Ferguson L et al. Interposition vein cuff for anastomosis of prosthesis to small artery. Aust N Z J Surg 54 (1984): 283-285.
- Taylor RS, Loh A, McFarland RJ et al. Improved technique for polytetrafluoroethylene bypass grafting: long-term results using anastomotic vein patches. Br J Surg. 79 (1992): 348-354.
- Smout JD, Wolfe JH. Venous boot construction for a distal prosthetic bypass. Semin Vasc Surg 13 (2000): 53-57.
- Holdsworth PJ, Riddell PS, Leveson SH. Distal femoropopliteal bypass using a composite graft of PTFE and non-reversed saphenous vein. Ann R Coll Surg Engl 71 (1989): 4-6.
- Deutsch M, Meinhart J, Howanietz N et al. The bridge graft: a new concept for infrapopliteal surgery. Eur J Vasc Endovasc Surg 21 (2001): 508-512.
- Daenens K, Schepers S, Fourneau I et al. Heparin- bonded ePTFE grafts compared with vein grafts in femoropopliteal and femorocrural bypasses: 1- and 2-year results. J Vasc Surg. 49 (2009): 1210-1216.
- Pulli R, Dorigo W, Castelli P et al. Midterm results from a multicenter registry on the treatment of infrainguinal critical limb ischemia using a heparin-bonded ePTFE graft. J Vasc Surg. 51 (2010): 1167-1177.
- Neville RF, Capone A, Amdur R et al. A comparison of tibial artery bypass performed with heparin-bonded expanded polytetrafluoroethylene and great saphenous vein to treat critical limb ischemia. J Vasc Surg 56 (2012): 1008-1014.
- Lundgren F. Scandinavian Miller Collar Study (SCAMICOS). PTFE Bypass to Below-knee Arteries: Distal Vein Collar or Not? A Prospective Randomized Multicenter Study. Eur J Vasc Endovasc Surg 39 (2010): 747-754.
- Twine CP, Williams IM, Fligelstone LJ. Systematic review and meta- analysis of vein cuffs for below-knee synthetic bypass. British Journal of Surgery. 99 (2012): 1195-1202.
- Lundgren F. The vein collar: an anastomotic servant or a patency promoter? Re-analysis of a randomized trial. Int Angiol 31 (2012): 234-238.
- Conte MS, Belkin M, Upchurch GR et al. Impact of increasing comorbidity on infrainguinal reconstruction: a 20-year perspective. Ann Surg. 233 (2001): 445-452.
- Moawad J, Gagne P. Adjuncts to Improve Patency of Infrainguinal Prosthetic Bypass Grafts. Vasc Endovasc Surg. 37 (2003): 381-386.
Supplemental Figure 1:
Supplemental Figure 1:Kaplan-meier plots for cumulative survival. No significant difference between the three groups (p<0.375).
PGN: prosthetic graft without MOD
PGY: prosthetic graft with modification of the distal anastomosis (MOD)
VG: autogenous venous graft REBEL
Supplemental Figure 2:
Supplemental Figure 2:
CT-Angiogram with coronal (right) and longitudinal (left) section depiction distal anastomosis between tibialis posterior artery (ATP) and prosthetic graft (PG) with St. mary’s boot anastomotic modification. The patient was followed up after 36 months.
