Novel Surgical Management of an Extensive Recurrent Hickman Line Thrombosis involving the SVC and Right Atrium
Article Information
Anna Zingale1, Danai M Karamanou1, Pietro G Malvindi1, Suvitesh Luthra1, Sunil K Ohri1
Wessex Cardiothoracic Centre, University Hospital Southampton, Southampton, United Kingdom
*Corresponding Author: Anna Zingale, Wessex Cardiothoracic Centre, University Hospital Southampton, Southampton, United Kingdom
Received: 24 July 2023; Accepted: 02 August 2023; Published: 25 August 2023
Citation: Anna Zingale, Danai M Karamanou, Pietro G Malvindi, Suvitesh Luthra, Sunil K Ohri. Novel surgical management of an extensive recurrent Hickman line thrombosis involving the SVC and right atrium. Journal of Surgery and Research. 6 (2023): 292-294.
View / Download Pdf Share at FacebookAbstract
Intravenous central line catheters are often at risk of line-related thrombosis. We report on how the cardiopulmonary bypass strategy was tailored to the particular anatomical challenges with the use of an unconventional venous cannulation site to optimise intraoperative venous drainage, improve surgical exposure and avoid circulatory arrest in a case with a complex intracardiac thrombosis. This report also highlights the importance of assiduously monitoring the efficacy of anticoagulation therapy, especially in the context of small bowel syndrome.
Keywords
Thrombosis, Catheters, Anticoagulation therapy
Thrombosis articles Thrombosis Research articles Thrombosis review articles Thrombosis PubMed articles Thrombosis PubMed Central articles Thrombosis 2023 articles Thrombosis 2024 articles Thrombosis Scopus articles Thrombosis impact factor journals Thrombosis Scopus journals Thrombosis PubMed journals Thrombosis medical journals Thrombosis free journals Thrombosis best journals Thrombosis top journals Thrombosis free medical journals Thrombosis famous journals Thrombosis Google Scholar indexed journals Catheters articles Catheters Research articles Catheters review articles Catheters PubMed articles Catheters PubMed Central articles Catheters 2023 articles Catheters 2024 articles Catheters Scopus articles Catheters impact factor journals Catheters Scopus journals Catheters PubMed journals Catheters medical journals Catheters free journals Catheters best journals Catheters top journals Catheters free medical journals Catheters famous journals Catheters Google Scholar indexed journals Anticoagulation therapy articles Anticoagulation therapy Research articles Anticoagulation therapy review articles Anticoagulation therapy PubMed articles Anticoagulation therapy PubMed Central articles Anticoagulation therapy 2023 articles Anticoagulation therapy 2024 articles Anticoagulation therapy Scopus articles Anticoagulation therapy impact factor journals Anticoagulation therapy Scopus journals Anticoagulation therapy PubMed journals Anticoagulation therapy medical journals Anticoagulation therapy free journals Anticoagulation therapy best journals Anticoagulation therapy top journals Anticoagulation therapy free medical journals Anticoagulation therapy famous journals Anticoagulation therapy Google Scholar indexed journals foramen ovale articles foramen ovale Research articles foramen ovale review articles foramen ovale PubMed articles foramen ovale PubMed Central articles foramen ovale 2023 articles foramen ovale 2024 articles foramen ovale Scopus articles foramen ovale impact factor journals foramen ovale Scopus journals foramen ovale PubMed journals foramen ovale medical journals foramen ovale free journals foramen ovale best journals foramen ovale top journals foramen ovale free medical journals foramen ovale famous journals foramen ovale Google Scholar indexed journals embolic stroke articles embolic stroke Research articles embolic stroke review articles embolic stroke PubMed articles embolic stroke PubMed Central articles embolic stroke 2023 articles embolic stroke 2024 articles embolic stroke Scopus articles embolic stroke impact factor journals embolic stroke Scopus journals embolic stroke PubMed journals embolic stroke medical journals embolic stroke free journals embolic stroke best journals embolic stroke top journals embolic stroke free medical journals embolic stroke famous journals embolic stroke Google Scholar indexed journals Residual venous drainage articles Residual venous drainage Research articles Residual venous drainage review articles Residual venous drainage PubMed articles Residual venous drainage PubMed Central articles Residual venous drainage 2023 articles Residual venous drainage 2024 articles Residual venous drainage Scopus articles Residual venous drainage impact factor journals Residual venous drainage Scopus journals Residual venous drainage PubMed journals Residual venous drainage medical journals Residual venous drainage free journals Residual venous drainage best journals Residual venous drainage top journals Residual venous drainage free medical journals Residual venous drainage famous journals Residual venous drainage Google Scholar indexed journals Postoperative recovery articles Postoperative recovery Research articles Postoperative recovery review articles Postoperative recovery PubMed articles Postoperative recovery PubMed Central articles Postoperative recovery 2023 articles Postoperative recovery 2024 articles Postoperative recovery Scopus articles Postoperative recovery impact factor journals Postoperative recovery Scopus journals Postoperative recovery PubMed journals Postoperative recovery medical journals Postoperative recovery free journals Postoperative recovery best journals Postoperative recovery top journals Postoperative recovery free medical journals Postoperative recovery famous journals Postoperative recovery Google Scholar indexed journals tricuspid valve articles tricuspid valve Research articles tricuspid valve review articles tricuspid valve PubMed articles tricuspid valve PubMed Central articles tricuspid valve 2023 articles tricuspid valve 2024 articles tricuspid valve Scopus articles tricuspid valve impact factor journals tricuspid valve Scopus journals tricuspid valve PubMed journals tricuspid valve medical journals tricuspid valve free journals tricuspid valve best journals tricuspid valve top journals tricuspid valve free medical journals tricuspid valve famous journals tricuspid valve Google Scholar indexed journals atrial thrombus articles atrial thrombus Research articles atrial thrombus review articles atrial thrombus PubMed articles atrial thrombus PubMed Central articles atrial thrombus 2023 articles atrial thrombus 2024 articles atrial thrombus Scopus articles atrial thrombus impact factor journals atrial thrombus Scopus journals atrial thrombus PubMed journals atrial thrombus medical journals atrial thrombus free journals atrial thrombus best journals atrial thrombus top journals atrial thrombus free medical journals atrial thrombus famous journals atrial thrombus Google Scholar indexed journals
Article Details
Introduction
In vivo incidence of catheter-related right atrial thrombosis ranges between 5.4-12.5%. However in post-mortem examinations of patients with intravenous central line catheters this liability has been reported to be twice as high. Given that these patients are often asymptomatic this complication is commonly underdiagnosed. Depending on the size of the thrombus, rescue therapy may include surgical thrombectomy [1]. We present an intriguing case requiring a unique surgical approach and challenging postoperative anticoagulative management.
Case Report
A 46-year-old lady underwent previous extensive small bowel excision for volvulitic ischaemia thereafter required long-term total parenteral nutrition therapy via a Hickman line. Her care was complicated by SVC thrombosis. Initial medical intervention included SVC stenting and anticoagulation with warfarin which was administered orally. Of note is the variable warfarin absorption in patients with short bowel syndrome [2-5]. In this case INR regulation was poor, leading to subcutaneous administration of therapeutic doses of enoxaparin sodium injections instead. 20 months after initial treatment, the patient re-presented with a further thrombus evident on transthoracic echocardiogram (figure 1C). The finding was confirmed with a venogram and cardiac MRI (figures 1A-1B). The thrombus extended from the distal aspect of the SVC stent into the right atrium, involving the entire chamber whilst abutting the tricuspid valve. An incidental finding of a patent foramen ovale was established, which increases the risk of embolic stroke.
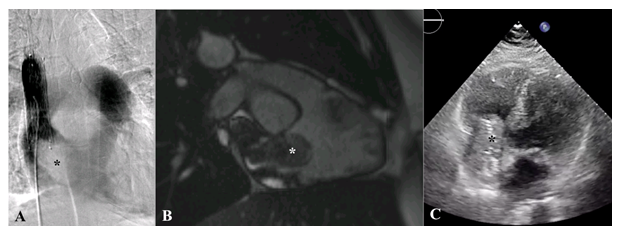
Figure 1: (A) Venogram with filling defect (*) at the distal aspect of the SVC stent. (B) Cardiac MRI demonstrates SVC occluded with thrombus (*) that dangles into the atrium. (C) Transthoracic echocardiogram shows the right atrial mass (*) falling into the tricuspid valve orifice.
The management of this case required a novel surgical approach. Following median sternotomy and systemic heparinization, the patient was placed on total cardiopulmonary bypass with insertion of an arterial cannula in the ascending aorta and primary venous cannulation of the IVC. A second venous cannula, placed in the brachiocephalic vein, offered an alternative to a classic SVC cannulation [6]. This approach has been implemented in congenital and minimally invasive cardiac surgery. We opted for this approach to optimise upper-body drainage while maintaining myocardial and organ preservation, thereby avoiding the need for circulatory arrest. The patient was cooled down to 24°C. After opening of the right atrium a vascular clamp was placed between the junction of the brachiocephalic vein and the SVC to reduce venous backflow. Residual venous drainage from the Azygous was dealt with by pump suction.
The complex thrombus extending from the SVC stent encompassing the Hickman line and extending into the right atrium, was excised. The PFO was identified and closed with a continuous suture. Thereafter the SVC stent was decorticated from the SVC wall. The Hickman line was trimmed, so that only 2-3 cm remained within the atrium and a pericardial patch was used to reconstruct the SVC before closure of the right atrium. The patient was readily weaned from cardiopulmonary bypass and closed routinely. Postoperative recovery was uncomplicated. Anticoagulation was resumed with an enoxaparin dose of 1.5mg/kg once daily. We referred the patient to the haematology service for further investigations.
Unfortunately one year following surgery the patient presented with a 4-month history of dyspnoea and fatigue. A chest CT and confirmatory transoesophageal echocardiogram revealed a large right atrial thrombus once more abutting the tricuspid valve (Figures 2-3).
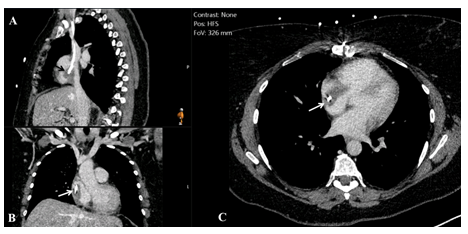
Figure 2: Chest computed tomography (A) sagittal, (B) coronal and (C) axial plane. The arrow indicates the catheter surrounded by the thrombus.
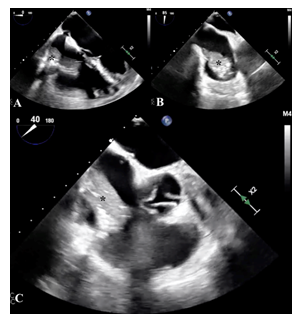
Figure 3: Transoesophageal echocardiogram (A) four chambers, (B) bicaval and (C) aortic valve short-axis view of the atrial thrombus (*).
Haematological investigations were undertaken demonstrating antithrombin III activity within normal limits and no presence of heparin antibodies. She was commenced on intravenous unfractionated heparin infusion (maintaining APTR levels between 1.8 and 3) and proceeded to urgent redo surgery. A redo-sternotomy was performed. Sharp dissection was required around the atrium, which was firmly adherent to the pericardium. Cardiopulmonary bypass was established via distal ascending aortic and bicaval cannulation, with direct SVC cannulation, superior to the previous patch repair. A right atriotomy was performed after snaring of the cavae. Where the Hickman line tip abutted the lateral wall of the atrium it appeared abraded, with an adherent thrombus on its surface. The chronic nature of the thrombus was reflective in the signs of encapsulation. Nonetheless a successful excision was achieved. Once more the Hickman line was therefore shortened. The operation was concluded in a routine fashion. Anticoagulation was resumed with an increased subcutaneous enoxaparin dose of 100 mg twice daily (over 1mg/kg twice daily) comparative to the preoperative dose of 120 mg once daily. The anti-factor Xa levels were monitored weekly for 1 month post-operatively to ensure adequate anticoagulation. Dose adjustments were implemented after checking anti-Xa levels. In addition the specialist intestinal failure team reviewed the case as part of an umbrella plan to trial oral nutrition with a long-term goal of removing the Hickman line. Unfortunately the patient was unable to tolerate oral nutrition and remains on total parenteral feeding. Follow-up at 12 months has found no evidence of recurrent atrial thrombus.
Discussion
This case highlights the paramount necessity to closely monitor the efficacy of anticoagulation therapy, as current guidelines of standard doses of factor X-inhibitors may not prevent catheter-related thrombosis [7,8]. We also suggest tailoring the cardiopulmonary bypass strategy to the particular anatomical challenges, with the use of an alternative venous cannulation to optimise venous drainage and improve surgical exposure during removal of an intracardiac thrombus.
Conflict of interests
The authors have no conflicts of interest to declare.
Ethics statement
Institutional IRB approval was waived for our case study and we have verbal consent of the patient for publication. No patient identifiers have been included in the manuscript.
References
- Tran M, Wilcox T, Tran PN. Catheter-related right atrial thrombosis. The journal of vascular access 21 (2019): 300-307.
- Brophy DF, Ford SL, Crouch MA. Warfarin resistance in a patient with short bowel syndrome. Pharmacotherapy 18 (1998): 646-649.
- Sobieraj DM, Wang F, Kirton OC. Warfarin resistance after total gastrectomy and Roux-en-Y esophagojejunostomy. Pharmacotherapy 28 (2008): 1537-1541.
- Owens JP, Mirtallo JM, Murphy CC. Oral anticoagulation in patients with short-bowel syndrome. DICP 24 (1990): 585-589.
- Strong AT, Sharma G, Nor Hanipah Z, et al. Adjustments to warfarin dosing after gastric bypass and sleeve gastrectomy. Surg Obes Relat Dis 14 (2018): 700-706.
- Aazami MH, Gholoobi A, Amini S, et al. Left Brachiocephalic Vein Cannulation in Bicaval Venous Drainage Is Safe, Effective, and Technically Advantageous. Tex Heart Inst J 43 (2016): 144-147.
- Fallouh N, McGuirk HM, Flanders SA, et al. Peripherally inserted central catheter – associated deep vein thrombosis: a narrative review. Am J Med 128 (2015): 722-738.
- Bishop L, Dougherty L, Bodenham A, et al. Guidelines on the insertion and management of central venous access devices in adults. Int J Lab Hematol 29 (2007): 261-278.
