Myocardial Injury Leading to Left Ventricular Failure: A COVID-19 Complication
Article Information
Muhammad Humayoun Rashid1*, Muhammad Usman Piracha2, Azka Aisha3, Aqsa Komel3, Mehjabeen Ahmad3, Meher Fatima4, Usama Bin Saif1, Umar Farooque5
1Department of Cardiology, Chaudhry Pervaiz Elahi Institute of Cardiology, Multan, Pakistan
2Department of Biochemistry, Bakhtawar Amin Medical and Dental College, Multan, Pakistan
3Department of Internal Medicine, Nishtar Medical University, Multan, Pakistan
4Department of Pathology, Chaudhry Pervaiz Elahi Institute of Cardiology, Multan, Pakistan
5Department of Neurology, Dow University of Health Sciences, Karachi, Pakistan
*Corresponding Authors: Muhammad Humayoun Rashid, Department of Cardiology, Chaudhry Pervaiz Elahi Institute of Cardiology, Multan, Pakistan
Received: 08 September 2020; Accepted: 16 Septeber 2020; Published: 22 September 2020
Citation: Muhammad Humayoun Rashid, Muhammad Usman Piracha, Azka Aisha, Aqsa Komel, Mehjabeen Ahmad, Meher Fatima, Usama Bin Saif, Umar Farooque. Myocardial Injury Leading to Left Ventricular Failure: A COVID-19 Complication. Cardiology and Cardiovascular Medicine 4 (2020): 563-568.
View / Download Pdf Share at FacebookAbstract
SARS-CoV-2 has been associated with a lot of complications one of which is myocardial injury which is still a subject under study. Here we present a case of a 63 years old diabetic man with signs of left ventricular failure and clear evidence of myocardial injury, later diagnosed as COVID-19. In the setting of cardiac emergency medical professionals need to have a high index of suspicion early on during the management.
Keywords
COVID-19; Myocardial injury; Left ventricular failure; SARS-CoV-2
Article Details
1. Background
Three strains of corona virus are identified in previous two decades. These are the severe acute respiratory syndrome coronavirus (SARS-CoV) in 2002 with case fatality rate of 11%, Middle East respiratory syndrome coronavirus (MERS-CoV) in 2012 with case fatality rate of 34.4%, and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in 2019 with case fatality rate of 3.27%. Among the wide spectrum of complications that SARS-CoV-2 can cause, myocardial injury is one of them. Here we discuss a tricky case scenario of a known ischemic heart disease patient suffering from left ventricular failure with superimposed COVID-19. The symptomatology is similar enough and both the conditions are difficult to distinguish clinically. High clinical suspicion along with the radiological evidence is needed to reach the diagnosis.
2. Case Presentation
On 13th April 2020, a 63 years old man presented in the emergency department with fever, cough, shortness of breath, and generalized body aches for 3 days. Fever was mild and continuous. Cough was intermittent and productive. Initially, he had shortness of breath only at night during sleep for which he had to sit up to feel comfortable, but his shortness of breath has worsened since then. On asking further, he said that he has not traveled outside Pakistan recently and has not met any known person who had a positive travel history.
On examination, he was a sick looking man, fully oriented in time, place, and person, sitting up and breathing heavily. Body temperature was 100.7 degrees Fahrenheit. His blood pressure was 80/50 mmHg, pulse was 110/min and feeble, respiratory rate 36/min, and oxygen saturation (SpO2) was 82% on room air. High flow supplemental oxygen therapy was started to maintain saturation. On auscultation of precordium, S1 and S2 were audible with no added sound. On chest auscultation breath sounds were decreased on the bases of lungs and bilateral basal inspiratory crepitations were present. He had a previous history of diabetes mellitus for 10 years and myocardial infarction 2 years ago and was on prophylactic medications including aspirin and statins in addition to other oral anti-diabetics. Differential diagnoses included left ventricular failure (LVF), community acquitted pneumonia, and atypical pneumonia. We had suspicion for COVID-19 at the back of our minds due to all the risk factors that he possessed and the ongoing situation throughout the world.
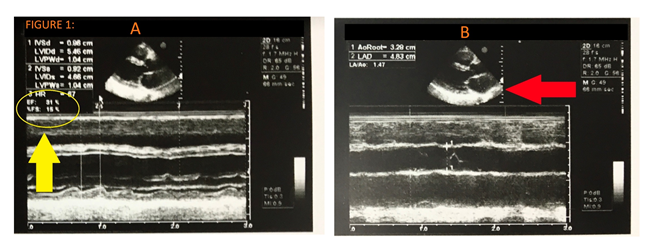
Cardiac enzymes (CPK and CK-MB) and troponin I were elevated showing evidence of myocardial injury. Echocardiography showed an ejection fraction of 31%, nondilated left ventricle with hypokinetic and calcified walls, and akinetic septum (Figure 1).
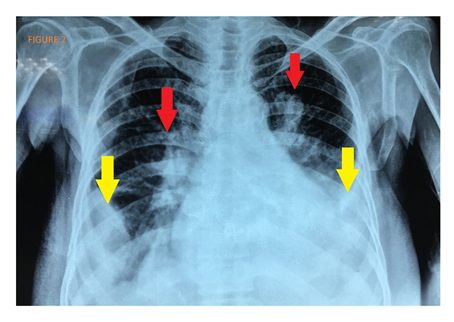
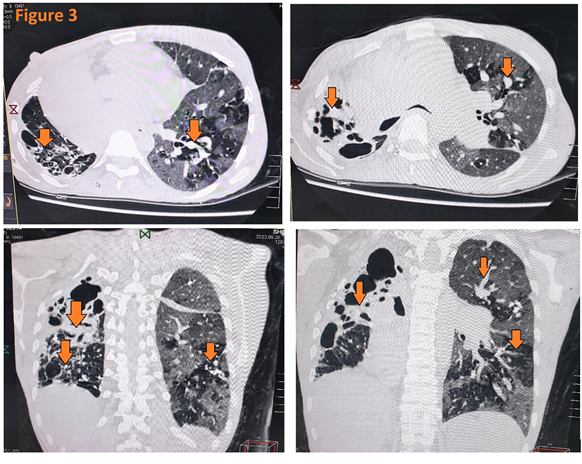
Chest X-ray showed bilateral opacities with mild bilateral pleural effusion, peri-bronchial cuffing, and perihilar haze (Figure 2). Blood and sputum cultures for bacterial pathogens and nasopharyngeal swab to do RT-PCR for SARS-C0V-2 were sent. Meanwhile HRCT was done which showed bilateral reticulonodular opacities (Figure 3). The patient was started on injectable inotropes, heparin infusion, and furosemide to increase heart pumping, prevent ischemia (if any), and reduce preload. Moxifloxacin and ceftriaxone were given as a cover for superimposed infections till the blood tests return. Laboratory results showed lymphopenia, leukocytosis, and elevated CRP.
Figure 1: Transthoracic Echocardiography. (A) Yellow arrow shows ejection fraction of 30%. Ejection fraction is reduced due impaired left ventricle; (B) Red arrow shows left ventricle. It is non dilated and has calcified well due to myocardial injury. Movement of anterior wall of left ventricle and septum is reduced which causes reduced ejection fraction.
The patient went into respiratory fatigue and was intubated and mechanically ventilated. He was shifted to ICU and was placed on airborne, droplet, and contact isolation because of the high suspicion of corona-virus infection. All the health care workers were duly informed about the COVID-19 suspicion and preventive measures were endorsed. Blood and sputum cultures came out to be negative. Nasopharyngeal swab specimen tested positive for SARS-CoV-2 leading to diagnosis of COVID-19. Two further samples were taken for consecutive two days, which were positive as well. After three days of ICU management the patient started to maintain his saturation and was extubated and shifted to the isolation ward. He was kept under conservative management. Serial x-rays were taken and the opacities gradually improved and his symptoms started vanishing. His management was done with inotropes (dobutamine infusion), diuretics (furosemide 40 mg IV twice daily), heparin, supplemental oxygenation as needed, prophylactic antibiotics (moxifloxacin 400 mg IV daily) and hydroxychloroquine (800 mg on day 1 then 400mg daily). He was also started on tocilizumab (6 mg/kg body weight), an antiinterleukin-6 receptor monoclonal antibody, to reduce the cytokine storm.
His condition improved gradually till he became asymptomatic. He was discharged to home isolation for two weeks on day 14 after double negative SARS-CoV-2 testing. His symptoms resolved completely with progressive increases in plasma SARS-CoV-2-binding IgM and IgG antibodies from day 7 until day 20. The patient recovered completely on follow up after two weeks.
3. Discussion
COVID-19, a short form of 2019 novel coronavirus disease, is a disease caused by a newly discovered virus known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Early diagnosis, self-isolation, and quarantine remain the key to flatten the curve of this contagious disease as there is a real risk of the healthcare system being overwhelmed. It is now clear that SARS-CoV-2 attaches to the angiotensin-converting enzyme2 receptor in the respiratory epithelium to attach to and infect cells [1]. The incubation period varies from one to fourteen days with a median of three to seven days. Cytokine storm due to excessive elaboration of tumor necrosis factor-alpha (TNF-α) and interleukins (IL)-2, IL-6, IL-7, and IL-10 have been seen [2]. CT scan of thorax commonly reveals bilateral multi-lobar ground-glass opacities with peripheral or posterior distribution, with consolidation seen more in the elderly. Likewise, the patient we discussed above had these opacities. Our patient had no contact or travel history, so he might have extracted the disease from an asymptomatic carrier. Respiratory droplets and contaminated hands of the person carrying SARS-CoV-2, may be symptomatic or asymptomatic, can transmit the disease to another person.
For people who have no comorbidities and their immune system is working fine can go pass through this asymptomatic or with just mild flu-like illness. But those having comorbidities can have a severe form of the disease. Comorbidities may include diabetes, ischemic heart disease, chronic liver disease, chronic kidney disease, restrictive lung diseases, chronic obstructive lung disease, cancers, leukemias, thalassemia, people taking immunosuppressants, and other immunosuppressing diseases [3]. Similarly, the patient discussed above had diabetes mellitus and ischemic heart disease due to which the COVID-19 expressed its severe form. The diagnostic criteria is given in Table 1.
Real-time reverse-transcriptase polymerase-chain-reaction (RT-PCR) is the diagnostic test of choice for COVID-19, hence we used this test to diagnose our case. He had fever, cough, shortness of breath as supportive symptoms and lymphopenia, elevated CRP, and bilateral basal lung involvement as supportive investigations. Raised cardiac enzymes and troponin I gave the evidence of recent myocardial injury, which lead to left ventricular failure (LVF). Reduced ejection fraction of 30% on transthoracic echocardiography helped us to diagnose LVF. Pulmonary edema, decreased blood pressure, feeble pulse and decreased oxygen saturation were the signs due to left ventricular failure. This case shows that SARS-CoV-2 has some mechanism of causing myocardial injury which is currently not clearly understood and needs more attention. A similar sort of evidence of myocardial injury has been presented forward by Nianguo Dong in his case series [4]. Two cohort studies have been done in China linking myocardial injury with COVID-19 [5, 6]. A group of Chinese researchers concluded that COVID-19 can significantly affect the heart function and lead to myocardial injury [7]. Healthcare workers are on the frontline for taking care of patients who have possible or confirmed COVID-19. Hospitals and state governments need to ensure the presence of personal protective equipment to each health care professional and ensure their safety first because they are our heroes and the frontline defense in this war against COVID-19.
4. Conclusion
In the setting of cardiac emergency medical professionals need to be more vigilant regarding COVID-19. Myocardial injury is one of the complications of COVID-19 and should be distinguished from the symptoms of left ventricular failure alone. This needs a high index of suspicion and proper investigations early on during the management.
References
- Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. The Lancet 395 (2020): 507-513.
- Guo YR, Cao QD, Hong ZS, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak–an update on the status. Military Medical Research 7 (2020): 1.
- Cheng Y, Luo R, Wang K, et al. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney international 97 (2020): 829-838.
- Chen X, Zhang Y, Zhu B, et al. Associations of clinical characteristics and antiviral drugs with viral RNA clearance in patients with COVID-19 in Guangzhou, China: a retrospective cohort study. medRxiv (2020).
- Guo T, Fan Y, Chen M, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA cardiology 5 (2020): 811-818.
- Shi S, Qin M, Shen B, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA cardiology 5 (2020): 802-810.
- Chen C, Yan JT, Zhou N, et al. Analysis of myocardial injury in patients with COVID-19 and association between concomitant cardiovascular diseases and severity of COVID-19. Zhonghua xin xue guan bing za zhi 48 (2020): 567-571.