Multiple Alloantibodies Induced Autoimmune Hemolytic Anemia in Beta Thalassemia Woman with Megaloblastic Anemia during Pregnancy: A Case Report and Literature Review
Article Information
Shiguang Ye#, Mengmeng Pan#, Lili Zhou, Ping Li, Xiuqin Wang*, Aibin Liang*
Department of Hematology, Tongji Hospital, Tongji University School of Medicine, Shanghai, P.R. China
# Contributed equally
*Corresponding Author: Aibin Liang, Department of Hematology, Tongji Hospital, Tongji University School of Medicine, 389 Xincun Road, Shanghai 200065, P.R. China
Xiuqin Wang, Department of Hematology, Tongji Hospital, Tongji University School of Medicine, 389 Xincun Road, Shanghai 200065, P.R. China
Received:20 June 2019; Accepted: 09 July 2019; Published: 23 September 2019
Citation: Shiguang Ye, Mengmeng Pan, Lili Zhou, Ping Li, Xiuqin Wang, Aibin Liang. Multiple Alloantibodies Induced Autoimmune Hemolytic Anemia in Beta Thalassemia Woman with Megaloblastic Anemia during Pregnancy: A Case Report and Literature Review. Archives of Clinical and Medical Case Reports 3 (2019): 278-284.
View / Download Pdf Share at FacebookAbstract
Thalassemia is prevalent in Southern China and pregnancy with thalassemia becomes not rare in this area. Due to the unique pathophysiologic mechanism, pregnant complications in beta thalassemia are more complicated than normal pregnancy, such as hypercoagulation state, infant intrauterine growth restriction, impaired heart function and anemia. Despite of these, the clinical outcome of beta thalassemia pregnancy has been reported better currently. In this article, we report one interesting and distinct case of beta thalassemia pregnancy with complicated anemia. A pregnant woman, with beta thalassemia intermedia and underlying megaloblastic anemia, suffers the complex autoimmune hemolytic anemia after delivery. Screening for antibodies identifies two alloantibodies, anti-E IgG and anti-Lea IgM antibodies, which both contribute to the autoimmune hemolytic anemia. Glucocorticoid combined with immunoglobin has a good response and warm blood transfusion is also important in the treatment.
Keywords
Beta thalassemia, Autoimmune hemolytic anemia, Pregnancy
Beta thalassemia articles Beta thalassemia Research articles Beta thalassemia review articles Beta thalassemia PubMed articles Beta thalassemia PubMed Central articles Beta thalassemia 2023 articles Beta thalassemia 2024 articles Beta thalassemia Scopus articles Beta thalassemia impact factor journals Beta thalassemia Scopus journals Beta thalassemia PubMed journals Beta thalassemia medical journals Beta thalassemia free journals Beta thalassemia best journals Beta thalassemia top journals Beta thalassemia free medical journals Beta thalassemia famous journals Beta thalassemia Google Scholar indexed journals Autoimmune hemolytic anemia articles Autoimmune hemolytic anemia Research articles Autoimmune hemolytic anemia review articles Autoimmune hemolytic anemia PubMed articles Autoimmune hemolytic anemia PubMed Central articles Autoimmune hemolytic anemia 2023 articles Autoimmune hemolytic anemia 2024 articles Autoimmune hemolytic anemia Scopus articles Autoimmune hemolytic anemia impact factor journals Autoimmune hemolytic anemia Scopus journals Autoimmune hemolytic anemia PubMed journals Autoimmune hemolytic anemia medical journals Autoimmune hemolytic anemia free journals Autoimmune hemolytic anemia best journals Autoimmune hemolytic anemia top journals Autoimmune hemolytic anemia free medical journals Autoimmune hemolytic anemia famous journals Autoimmune hemolytic anemia Google Scholar indexed journals Pregnancy articles Pregnancy Research articles Pregnancy review articles Pregnancy PubMed articles Pregnancy PubMed Central articles Pregnancy 2023 articles Pregnancy 2024 articles Pregnancy Scopus articles Pregnancy impact factor journals Pregnancy Scopus journals Pregnancy PubMed journals Pregnancy medical journals Pregnancy free journals Pregnancy best journals Pregnancy top journals Pregnancy free medical journals Pregnancy famous journals Pregnancy Google Scholar indexed journals health articles health Research articles health review articles health PubMed articles health PubMed Central articles health 2023 articles health 2024 articles health Scopus articles health impact factor journals health Scopus journals health PubMed journals health medical journals health free journals health best journals health top journals health free medical journals health famous journals health Google Scholar indexed journals Alloantibodies articles Alloantibodies Research articles Alloantibodies review articles Alloantibodies PubMed articles Alloantibodies PubMed Central articles Alloantibodies 2023 articles Alloantibodies 2024 articles Alloantibodies Scopus articles Alloantibodies impact factor journals Alloantibodies Scopus journals Alloantibodies PubMed journals Alloantibodies medical journals Alloantibodies free journals Alloantibodies best journals Alloantibodies top journals Alloantibodies free medical journals Alloantibodies famous journals Alloantibodies Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals Megaloblastic Anemia articles Megaloblastic Anemia Research articles Megaloblastic Anemia review articles Megaloblastic Anemia PubMed articles Megaloblastic Anemia PubMed Central articles Megaloblastic Anemia 2023 articles Megaloblastic Anemia 2024 articles Megaloblastic Anemia Scopus articles Megaloblastic Anemia impact factor journals Megaloblastic Anemia Scopus journals Megaloblastic Anemia PubMed journals Megaloblastic Anemia medical journals Megaloblastic Anemia free journals Megaloblastic Anemia best journals Megaloblastic Anemia top journals Megaloblastic Anemia free medical journals Megaloblastic Anemia famous journals Megaloblastic Anemia Google Scholar indexed journals patient articles patient Research articles patient review articles patient PubMed articles patient PubMed Central articles patient 2023 articles patient 2024 articles patient Scopus articles patient impact factor journals patient Scopus journals patient PubMed journals patient medical journals patient free journals patient best journals patient top journals patient free medical journals patient famous journals patient Google Scholar indexed journals Thalassemia articles Thalassemia Research articles Thalassemia review articles Thalassemia PubMed articles Thalassemia PubMed Central articles Thalassemia 2023 articles Thalassemia 2024 articles Thalassemia Scopus articles Thalassemia impact factor journals Thalassemia Scopus journals Thalassemia PubMed journals Thalassemia medical journals Thalassemia free journals Thalassemia best journals Thalassemia top journals Thalassemia free medical journals Thalassemia famous journals Thalassemia Google Scholar indexed journals immunoglobin articles immunoglobin Research articles immunoglobin review articles immunoglobin PubMed articles immunoglobin PubMed Central articles immunoglobin 2023 articles immunoglobin 2024 articles immunoglobin Scopus articles immunoglobin impact factor journals immunoglobin Scopus journals immunoglobin PubMed journals immunoglobin medical journals immunoglobin free journals immunoglobin best journals immunoglobin top journals immunoglobin free medical journals immunoglobin famous journals immunoglobin Google Scholar indexed journals
Article Details
1. Introduction
Thalassemia is one of the most common hereditary hemoglobinopathies, which nearly affects 5 percent of the world’s population. In Southern China, the carrier rate of beta thalassemia is about 1.9% [1]. Over 20 β-thalassemia mutations have been identified in Chinese population. Four mutations, [CD41-42 (-4 bp), IVS-2-654C→T, CD17A→T, and -28A→G], account for approximately 90% of the disease [2]. Three subtypes of beta thalassemia have been classified with clinical phenotype and genotype: transfusion-dependent (major), non-transfusion-dependent (intermedia) and minor. High rate of successful pregnancy in individuals with thalassemia minor and intermedia has been observed, moreover good pregnancy outcomes have been seen in beta thalassemia major cases [3-5]. Autoimmune hemolytic anemia (AIHA) is due to the presence of antibodies that react with protein antigens on the red blood cell (RBC) surface. The causes of AIHA are associated with many factors, but prior allogeneic blood transfusion is one of the most important factors in thalassemia pregnant patients [6]. Approximately 1.5 to 2.5 percent of pregnancies with alloantibodies are non-Rh(D) red blood cell (RBC) antibodies, which rarely cross the placenta, causing hemolytic disease of the fetus and newborn (HDFN) [7]. In this article we reported a case that a pregnant woman, who had beta thalassemia intermedia and megaloblastic anemia, suffered AIHA after delivery due to multiple alloantibodies and had a good response to the treatment of glucocorticoid and immunoglobulin.
2. Case Report
A 27-year-old Chinese gravida 3 para 0 woman from Fujian province, who had family history of anemia and no history of transfusion, first had been diagnosed anemia at 22 weeks of pregnancy with hemoglobin (Hb) 78 g/L. During her 36 weeks’ pregnancy, her Hb level had once dropped to 50 g/L and she had been transfused with 2 units (U) of leukocyte-reduced red blood cells. At 38+1 weeks of pregnancy, she came to the hospital with the complaint of abdominal pain. Her vital sign was stable and physical examination showed pallor skin, splenomegaly, no hepatomegaly, no jaundice, and others were unremarkable. Complete blood count showed severe anemia (Hb 51 g/L) with decreased mean corpuscular volume (76.7 fl), mean corpuscular hemoglobin (22.5 pg) and mean corpuscular hemoglobin concentration (293 g/L). Peripheral blood smear indicated uneven size of erythrocytes, with teardrop-shaped, irregular and immature erythrocytes. Nutrition tests showed low serum VitB12 (cobalamin), low folate and normal ferritin. Total and unconjugated bilirubin levels were slightly increased (25 μmol/L and 23.1 μmol/L, respectively). Direct and indirect coomb’s test (DCT, ICT) were negative. Coagulation tests were within normal limits. The blood group of the patient was O Rh(D+). She received 6U red blood suspension (RBS) transfusion, and gave birth to a healthy baby girl by caesarean section on the next day.
Considering the family history that the patient’s sister had undergone splenectomy for splenomegaly, we suspected the woman had hereditary hemoglobinopathy and analyzed her hemoglobin by high performance liquid chromatography (HPLC). The result was positive, showing a significant increase in HBF (49% HBF, 50.5% HBA and 0.5% HBA2). Other hemolysis test was negative: glucose?6?phosphate dehydrogenase (G6PD) activities, pyruvate kinase (PK) activities and Heinz-body forming test. Bone marrow aspiration showed that Gaucher’s cells were found in her bone marrow smear. Then, the specific test was performed by reverse dot-blot hybridization to detect thalassemia-associated mutations. The result showed the woman carried a heterozygous mutation of the beta-thalassemia gene CD41-42(-4 bp). Moreover, the patient’s level of VitB12 and folate was low. Above all, we gave the diagnosis as beta thalassemia intermedia with megaloblastic anemia. Oral folic acid and parenteral VitB12 were given.
On the fifth day after the operation, the woman developed a fever with a maximum body temperature of 39.0°C (102°F) and accompanied by dark urine. Her Hb decreased to 31 g/L and reticulocytes increased (5%). Total and unconjugated bilirubin increased significantly (58.9 μmol/L and 51.9 μmol/L, respectively). LDH is higher than upper limit. DCT was positive (C3 positive and IgG negative). ICT was negative. She was received 3U washed red blood cells (WRBC) and 8U specially cross-matched red blood cells (RBC) transfusion, but it did not improve and her Hb was still around 30 g/L. Antibody screen and identification showed that there were anti-E IgG antibody and cold agglutinin antibodies (anti-Lea IgM antibody) in the serum. Her RBC haplotype was finally confirmed to be O Rh (CCD ee) Leb. The diagnosis of mixed autoimmune hemolytic anemia was certain. Due to the complex antibodies caused autoimmune hemolytic anemia, the patient was given the treatment with methylprednisolone (1 mg/kg) for 15 days and subsequent dosing slowly. She was also received immunoglobulin at dose of 0.4 mg/kg daily for 5 days followed by 0.2 mg/kg daily for 5 days. In transfusion, she received specially cross-matched RBC, which had been warmed appropriately prior to and during transfusion. The patient’s Hb increased and stabilized above 60 g/L. Then she was discharged and followed up. One year later, her Hb increased and remained around 90 g/L.
|
Chinese Pregnant woman, 27 years old, G3P0, 38+1 weeks |
|||||||
|
Days after admission |
Laboratory test |
Treatment |
|||||
|
Hb g/L |
Ret % |
IB mmol/L |
TB mmol/L |
LDH u/L |
Others |
||
|
D1 |
51 |
- |
23.1 |
24.1 |
1001 |
VitB12↓, faltate↓, Coomb (-), ANA (-) |
Transfuse RBC and plasma |
|
D2 |
Caesarean section, delivery of a healthy baby girl |
||||||
|
D4-5 |
57 |
4.9 |
46.9 |
49.4 |
696 |
49% HBF, 50.5% HBA, 0.5% HBA2 G6PD, PK activity normal heterozygous mutation of beta: CD41-42 (-4 bp) |
Oral folic acid and parenteral VitB12 |
|
D7 |
31 |
- |
51.9 |
58.9 |
>2150 |
DCT (+): C3 positiv and IgG negative ICT (-); dark urine |
Transfuse WRBC 3U; MP 1 mg/kg daily |
|
D8 |
26 |
5.2 |
52.3 |
64.1 |
>2150 |
Multiple alloantibodies positive |
Transfuse specially cross-matched RBC; IVIg 0.4 mg/kg daily |
|
D10 |
33 |
10.6 |
37.7 |
49.7 |
>2150 |
Antibody Screening: anti-E IgG, anti-Lea IgM antibody |
Transfuse warm specially cross-matched RBC |
|
D24 |
62 |
- |
37 |
44.6 |
976 |
- |
|
MP-methylprednisolone; IVIg-intravenous immunogloblin; Hb-hemoglobin; Tb-total bilirubin; Ib-indirect bilirubin; G6PD-glucose6phosphate; PK-pyruvate kinase; DCT-direct coomb’s test; ICT-indirect coomb’s test; RBC-red blood cell; WRBC-washed red blood cell.
Table 1: Laboratory test and treatment schedule.
Treatment: MP(1mg/kg) for 15 days, IVIg for 10 days; MP-methylprednisolone; IVIg-intravenous immunogloblin; Hb-hemoglobin; Tb-total bilirubin; Ib-indirect bilirubin.
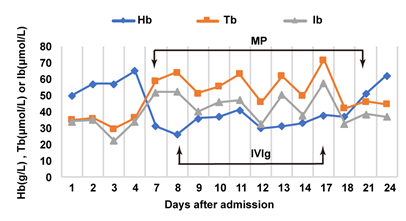
Figure 1: Illustration of therapeutic effect.
3. Discussion
Since thalassemia pregnancy (mainly thalassemia intermedia) was first observed in the mid-1960s, in the past few decades many reports have focused on the outcomes of thalassemia pregnant women in different regions [3-5, 8, 9]. In Lebanon and Italy, a total of 48 pregnant women with thalassemia have a live birth rate of 93% and a spontaneous abortion rate of 7% [9]. In the United Kingdom and North America, over 70% of pregnancies resulted in live births and 73/83 (88%) of live births occurred at full term [4]. Pregnancy in women with thalassemia appears to have no adverse effects on the progression of the disease, but are associated with high rate of thrombotic events, including placental thrombosis and deep vein thrombosis, as well as high rate of intrauterine growth restriction (IUGR) [5, 9, 10].
This case explores a complicated anemia in a thalassemia pregnant woman. Firstly, the patient has beta thalassemia intermedia, confirmed by the gene test result and there is no transfusion history before pregnancy. Due to the increasing demand nutrition and metabolism during pregnancy, her anemia is exacerbating and megaloblastic anemia occurs with the low VitB12 and folic acid level. After delivery, she has met a more challenging problem: AIHA. There are two alloantibodies in her serum, both are non-RH(D) RBC antibody: anti-E IgG antibody and cold agglutinin antibodies (anti-Lea IgM antibody), which would cause mixed AIHA (both warm and cold). Anti-E IgG antibody is one of the antibodies against Rh complex on the normal red cell membrane and can easily deposite to initiate complement activation causing AIHA [11]. The anti Leb IgM antibody is one of the Lewis antibodies, which are usually IgM and appear in pregnancy and postpartum [12]. In cold temperature, the antibody is easily agglutinated and cause hemolytic events. So prior to transfusion, the blood (and any co-administered solutions) should be warmed appropriately (typically, using a blood warmer to raise it to body temperature), but not exceed 40°C (104°F) causing thermal hemolysis [13].
Our treatment strategy is the combination of corticosteroids and immunoglobulins. Glucocorticoids are the most common medication used in the treatment of AIHA, by which nearly 80% patients could achieve an initial clinical response. Intravenous immune globulin (IVIG) is only occasionally effective in the treatment of AIHA refractory to conventional therapy with prednisone and splenectomy; it can also be used as part of the initial regimen to establish control of patients in very severe status. If the patient is refractory, rituximab is also an alternative option of treatments. High efficiency of rituximab has been seen in resistant or refractory AIHA, with response rates similar to splenectomy (∼70%). Rituximab combined with steroids is also an optional treatment [14]. In patient with thalassemia intermedia (TI), blood transfusion therapy is currently not a routine treatment. TI during pregnancy is confused with physiological anemia. Pregnancy is usually characterized by hemodynamic and cardiovascular changes, which are caused by increased total circulation volume and subsequent blood dilution. Transfusion therapy in anemic pregnant cases does reduce the risk of IUGR and other complications. Data from non-thalassemia populations indicate that hemoglobin above 10 g/dl during pregnancy is the best recommendation for fetal growth and prevention of preterm birth [15].
Patients with TI have a higher risk of thrombosis than the general population. One study shows that 30% of patients with TI had venous thromboembolism after 10 years of follow-up, suggesting a chronic hypercoagulable state [16]. Impaired cardiovascular system is also common seen in thalassemia. Pregnancy is expected to further increase these risks; fortunately, such complications do not occur in our patient. With the development of new therapies, the effectiveness and successful rates of pregnancy are now increasing. Allogeneic hematopoietic cell transplantation (HCT) and gene therapy are now potential methods of treatment for thalassemia. Thousands of patients with thalassemia have undergone allogeneic HCT and outcomes were illustrated that about 81% patients have free recurrence of thalassemia [17].
4. Conclusion
Thalassemia during pregnancy may bring out unique management challenges that requires close maternal and fetal monitoring. The case we report is a thalassemia pregnant woman accompanied by megaloblastic anemia and AIHA and shows a good clinical outcome. This case alerts us that patients with thalassemia need to be assessed in detail to rule out other complex causes of anemia, especially when the frequency of transfusion increases or Hb level decreases progressively. The patients, who have received repeated transfusions or been in immune stimulating state like pregnancy, should be scheduled to screen and identify of alloantibodies and irregular autoantibodies. The effective treatment includes glucocorticoid, gamma-immunoglobulin or rituximab.
Acknowledgement
The present study was supported by a grant from the Shanghai Shen-Kang Hospital Development Center Emerging Frontier Technology Project (SHDC12015108).
References
- He J, Zeng H, Zhu L, et al. Prevalence and spectrum of thalassaemia in Changsha, Hunan province, China: discussion of an innovative screening strategy. J Genet 96 (2017): 327-332.
- He X, Sheng M, Xu M, et al. Rapid identification of common beta-thalassemia mutations in the Chinese population using duplex or triplex amplicon genotyping by high-resolution melting analysis. Genet Test Mol Biomarkers 14 (2010): 851-856.
- Jensen CE, Tuck SM, Wonke B. Fertility in beta thalassaemia major: a report of 16 pregnancies, preconceptual evaluation and a review of the literature. Br J Obstet Gynaecol 102 (1995): 625-629.
- Thompson AA, Kim HY, Singer ST, et al. Pregnancy outcomes in women with thalassemia in North America and the United Kingdom. Am J Hematol 88 (2013): 771-773.
- Nassar AH, Usta IM, Rechdan JB, et al. Pregnancy in patients with beta-thalassemia intermedia: outcome of mothers and newborns. Am J Hematol 81 (2006): 499-502.
- Young PP, Uzieblo A, Trulock E, et al. Autoantibody formation after alloimmunization: are blood transfusions a risk factor for autoimmune hemolytic anemia? Transfusion 44 (2004): 67-72.
- ACOG Practice Bulletin No. 192: Management of Alloimmunization During Pregnancy. Obstet Gynecol 131 (2018): 82-90.
- Nassar AH, Naja M, Cesaretti C, et al. Pregnancy outcome in patients with beta-thalassemia intermedia at two tertiary care centers, in Beirut and Milan. Haematologica 93 (2008): 1586-1587.
- Roumi JE, Moukhadder HM, Graziadei G, et al. Pregnancy in beta-thalassemia intermedia at two tertiary care centers in Lebanon and Italy: A follow-up report on fetal and maternal outcomes. Am J Hematol 92 (2017): 96-99.
- Petrakos G, Andriopoulos P, Tsironi M. Pregnancy in women with thalassemia: challenges and solutions. Int J Womens Health 8 (2016): 441-451.
- Avent ND and Reid ME. The Rh blood group system: a review. Blood 95 (2000): 375-387.
- Ilver D, Arnqvist A, Ogren J, et al. Helicobacter pylori adhesin binding fucosylated histo-blood group antigens revealed by retagging. Science 279 (1998): 373-377.
- Berentsen S. How I manage patients with cold agglutinin disease. Br J Haematol 181 (2018): 320-330.
- Dierickx D, Kentos A, and Delannoy. The role of rituximab in adults with warm antibody autoimmune hemolytic anemia. Blood 125 (2015): 3223-3229.
- ACOG Practice Bulletin No. 78: hemoglobinopathies in pregnancy. Obstet Gynecol 109 (2007): 229-237.
- Eldor A and Rachmilewitz EA. The hypercoagulable state in thalassemia. Blood 99 (2002): 36-43.
- Caocci G, Orofino MG, Vacca A, et al. Long-term survival of beta thalassemia major patients treated with hematopoietic stem cell transplantation compared with survival with conventional treatment. Am J Hematol 92 (2017): 1303-1310.
