Motor Injury by Compression of Spinal Cord at Cervical Level During Surgery
Article Information
Inaki Arrotegui*
Department of Neurosurgery, University General Hospital of Valencia, Valencia, Spain
*Corresponding Author: Inaki Arrotegui, Department of Neurosurgery, University General Hospital of Valencia, Avda Tres Cruces S/n. 46014-Valencia, Spain
Received: 23 April 2019; Accepted: 06 May 2019; Published: 10 May 2019
Citation:
Inaki Arrotegui. Motor Injury by Compression of Spinal Cord at Cervical Level During Surgery. Journal of Spine Research and Surgery 1 (2019): 023-028.
View / Download Pdf Share at FacebookKeywords
Nonspecific neck pain, Anxiety, Depression, Kinesiophobia, Catastrophism, Quality of life
Nonspecific neck pain articles Nonspecific neck pain Research articles Nonspecific neck pain review articles Nonspecific neck pain PubMed articles Nonspecific neck pain PubMed Central articles Nonspecific neck pain 2023 articles Nonspecific neck pain 2024 articles Nonspecific neck pain Scopus articles Nonspecific neck pain impact factor journals Nonspecific neck pain Scopus journals Nonspecific neck pain PubMed journals Nonspecific neck pain medical journals Nonspecific neck pain free journals Nonspecific neck pain best journals Nonspecific neck pain top journals Nonspecific neck pain free medical journals Nonspecific neck pain famous journals Nonspecific neck pain Google Scholar indexed journals Anxiety articles Anxiety Research articles Anxiety review articles Anxiety PubMed articles Anxiety PubMed Central articles Anxiety 2023 articles Anxiety 2024 articles Anxiety Scopus articles Anxiety impact factor journals Anxiety Scopus journals Anxiety PubMed journals Anxiety medical journals Anxiety free journals Anxiety best journals Anxiety top journals Anxiety free medical journals Anxiety famous journals Anxiety Google Scholar indexed journals Depression articles Depression Research articles Depression review articles Depression PubMed articles Depression PubMed Central articles Depression 2023 articles Depression 2024 articles Depression Scopus articles Depression impact factor journals Depression Scopus journals Depression PubMed journals Depression medical journals Depression free journals Depression best journals Depression top journals Depression free medical journals Depression famous journals Depression Google Scholar indexed journals Kinesiophobia articles Kinesiophobia Research articles Kinesiophobia review articles Kinesiophobia PubMed articles Kinesiophobia PubMed Central articles Kinesiophobia 2023 articles Kinesiophobia 2024 articles Kinesiophobia Scopus articles Kinesiophobia impact factor journals Kinesiophobia Scopus journals Kinesiophobia PubMed journals Kinesiophobia medical journals Kinesiophobia free journals Kinesiophobia best journals Kinesiophobia top journals Kinesiophobia free medical journals Kinesiophobia famous journals Kinesiophobia Google Scholar indexed journals Catastrophism articles Catastrophism Research articles Catastrophism review articles Catastrophism PubMed articles Catastrophism PubMed Central articles Catastrophism 2023 articles Catastrophism 2024 articles Catastrophism Scopus articles Catastrophism impact factor journals Catastrophism Scopus journals Catastrophism PubMed journals Catastrophism medical journals Catastrophism free journals Catastrophism best journals Catastrophism top journals Catastrophism free medical journals Catastrophism famous journals Catastrophism Google Scholar indexed journals Quality of life articles Quality of life Research articles Quality of life review articles Quality of life PubMed articles Quality of life PubMed Central articles Quality of life 2023 articles Quality of life 2024 articles Quality of life Scopus articles Quality of life impact factor journals Quality of life Scopus journals Quality of life PubMed journals Quality of life medical journals Quality of life free journals Quality of life best journals Quality of life top journals Quality of life free medical journals Quality of life famous journals Quality of life Google Scholar indexed journals anesthesia articles anesthesia Research articles anesthesia review articles anesthesia PubMed articles anesthesia PubMed Central articles anesthesia 2023 articles anesthesia 2024 articles anesthesia Scopus articles anesthesia impact factor journals anesthesia Scopus journals anesthesia PubMed journals anesthesia medical journals anesthesia free journals anesthesia best journals anesthesia top journals anesthesia free medical journals anesthesia famous journals anesthesia Google Scholar indexed journals cervical herniated disc surgery articles cervical herniated disc surgery Research articles cervical herniated disc surgery review articles cervical herniated disc surgery PubMed articles cervical herniated disc surgery PubMed Central articles cervical herniated disc surgery 2023 articles cervical herniated disc surgery 2024 articles cervical herniated disc surgery Scopus articles cervical herniated disc surgery impact factor journals cervical herniated disc surgery Scopus journals cervical herniated disc surgery PubMed journals cervical herniated disc surgery medical journals cervical herniated disc surgery free journals cervical herniated disc surgery best journals cervical herniated disc surgery top journals cervical herniated disc surgery free medical journals cervical herniated disc surgery famous journals cervical herniated disc surgery Google Scholar indexed journals Neurosurgery articles Neurosurgery Research articles Neurosurgery review articles Neurosurgery PubMed articles Neurosurgery PubMed Central articles Neurosurgery 2023 articles Neurosurgery 2024 articles Neurosurgery Scopus articles Neurosurgery impact factor journals Neurosurgery Scopus journals Neurosurgery PubMed journals Neurosurgery medical journals Neurosurgery free journals Neurosurgery best journals Neurosurgery top journals Neurosurgery free medical journals Neurosurgery famous journals Neurosurgery Google Scholar indexed journals
Article Details
1. Introduction
It is impossible to predict in each patient, what will happen. There is always, even in the most banal surgical intervention, an even vital risk, even if in a proportion or percentage of possibilities almost infinitely small. The factors that influence are very varied and range from the conditions of the patient (general condition, anatomical characteristics), to those dependent on the medication required (allergies, gastrointestinal disorders) or inherent to the surgical act itself (anesthesia, technique surgical performed). For this reason, each surgical intervention is selected for each determined patient when theoretically the possibilities of healing or improvement with the intervention are superior to those offered by nature itself in the normal course of the disease. The Spanish Society of Neurosurgery has tried to offer a global view of the possible complications that may appear in this type of cervical herniated disc surgery. It distinguishes the complications common to other surgical acts on the spine and the specific ones of the interventions on the cervical spine by anterior route, already explained.
The list that follows is not intended to alarm, but to show the wide range of possibilities that a complication may arise. Although in daily practice, in patients with a good general condition, the real chances of a complication arising and can leave serious sequelae less than 1%:
1.1 General complications
1.1.1 Gastrointestinal complications:
- Stress ulcer
- By medications.
1.1.2 Venous thrombosis. aerial embolism (frequent in spinal trauma):
- Deep vein thrombosis (4.3%)
- Pulmonary thromboembolism (0.5%).
1.1.3 Acute respiratory failure:
Hospital infection, pneumonia; More in patients with low level of consciousness and in immunosuppressed.
1.1.4 Urinary infection:
- In sick patients
- Immunosuppressed
- In proximity with other patients with bladder catheter.
1.2 Infections
1.2.1 Clean contaminated surgery (surgery lasting more than 2 hours):
- Surface infection (1.6%)
- Deep infection (5.1%).
1.2.2 Clean surgery with a foreign body (Implants [vertebral fixation material, acrylics, dural plasties]):
- Surface infection (1.7%)
- Deep infection (4.34%).
1.2.3 Clean surgery
- Surface infection (1.9%)
- Deep infection (0.7%).
1.3 Cervical column surgery previous route
- Mortality (0-3%)
- New spinal cord injury (worsening) (0.2-4%)
- Preexisting spinal cord injury (05-3.3%)
- Transient radicular deficit (1.2-19%)
- Persistent radicular deficit (0.4%)
- Vascular injury
1.3.1 Carotid and vertebral artery, casual complication:
- Recurrent nerve injury (0.2-4%)
- Pneumothorax (Exceptional Complication)
- Esophageal perforation (Exceptional complication)
- Graft
- Extrusion
- Break
- Infection
- Resorption
1.3.2 Subluxation infection:
- Superficial (wound)
- Discitis (0.2-1.9%)
- Meningitis (exceptional complication)
- Abscess (exceptional complication
- Laryngeal edema
- Dysphagia (difficulty swallowing)
1.4 Information to the patient
Increasingly, the medical act and, above all, the surgical act, is a commitment between the parties (surgeon/hospital-patient/family and social environment) to walk together towards the best possible solution within the limits that nature imposes, counting on the means and adequate medical experience, as well as with the effective collaboration of the patient and his environment. All patients prior to their surgical intervention receive a C.I, which is usually validated by the different health departments or scientific societies of each medical specialty.
2. Clinical Case
The patient was seen in outpatient clinics since 2014. A complete and detailed clinical history was made and any type of clinical pathway was followed regarding the Conservative and Symptomatic treatment. The mandatory complementary tests (EMG, MRI) were performed until a correct diagnosis of the pathology suffered by the patient. The patient was diagnosed with a Cervical disc herniation with compression of the C6 root and paresthesia of the left upper limb (Figure 1).

Figure 1: MRI prior to surgery, the arrow indicates the presence of a cervical disc at level C6.
During the surgical act, there was an affectation of the dura mater and exit of cerebrospinal fluid, treated by means of a biological sealant. At the moment of placing the intersomatic box (Figure 2), the neurophysiologist warns of the fall of potentials. The surgery ends and the patient is transferred to the ITU. When carrying out the clinical assessment, a clear paraparesis of the Upper and Lower Left Member 2/5 was observed.

Figure 2: Rx intraoperative control with the placement of the cage and plate.
Urgently, a control MRI was performed (Figure 3), where the presence of blood in the surgical bed with mass effect on the spinal cord was verified. The operating room was reopened, the previous incision was opened, the plate and intersomatic cage were removed, the hematoma and the biological sealant that was in contact with the medulla was evacuated. The patient was referred back to the ITU, where a new neurological scan detected a slight improvement in his clinical picture.
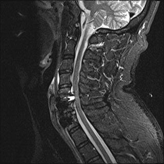
Figure 3: Postoperative MRI; the compression of the marrow is observed by a collection of blood and / or biological sealant.
3. Discussion
The failure of conservative treatment, the progression of the motor lesion or the spinal cord involvement are the indications for the surgical treatment of cervical disc hernias. This occurs, depending on the series in 10-20% of patients. The objective of surgery in cervical spine disc is the decompression of the nervous structures.
3.1 Characteristics of complications
They were classified into three groups, the first included complications related to the approach and surgical procedure, such as laryngeal complications (dysphonia, aphonia), tracheal, esophageal (rupture, laceration, swallowing discomfort) and pharyngeal, injury to the laryngeal nerves, rupture of large vessels, alteration of the sympathetic-cervical chain, the increase of the neurological deficit (radicular, medullar) as a direct consequence of the intervention, the dural laceration or the cerebrospinal fluid fistula, the soft tissue hematomas and the respiratory problems derived from these, the infection superficial or deep (discitis, meningitis, abscess). The second group included the complications derived from the arthrodesis material, both graft (extrusion, collapse, fracture), and instrumentation (plaque fracture, rupture, extrusion of the screws, extrusion of the Inter somatic box). Systemic complications constituted the third group.
3.2 Duration of the complication
We established as a transitory complication that which did not last after three months, and as a permanent complication, that which remained past this time. Cerebrospinal fluid leakage (CSF) is a potential complication of cranial and spinal surgery. Postoperative CSF leak can induce delayed healing, wound infection and meningitis. . DuraSeal® (Covidien, Waltham, MA, USA) It is a synthetic material. Product that has been increasingly used to facilitate tightness. Repair of dural defects after cranial and spinal surgery. DuraSeal® has been shown to be safe and effective in clinical studies and approved in 2005. By the Food and Drug Administration (FDA) [1]. CSF leak can cause delayed healing of surrounding tissues, such as skin, muscles and bones, due to its caustic effect [2]. Other potential complications include meningitis and severe headaches from CSF depletion. The goal, therefore, once a CSF leak is identified, is to stop the leak. DuraSeal® is a self-curing agent that quickly forms a firm, watertight hydrogel layer several seconds after application on the dural surface. Compared to fibrin glue, there is a “higher resistance of tissue adhesion and resistance to breakage”. The firm layer is robust enough to withstand irrigation and gentle suction maneuvers without risk of eviction. These properties are advantageous to affect a hermetic barrier to minimize the risk of leakage of CSF [2].
After review of the literature [3-5] we have found a case similar to the one we are dealing with: A case of compression of the cervical cord has also been reported in a patient who underwent anterior cervical decompression C5-C6 and fusion that suffered a CSF leak when removing the posterior longitudinal ligament. Using DuraSeal® as primary sealant [3]. Three hours after the operation, the patient developed progressive motor weakness of the upper and lower extremities. During the emerging exploration and decompression, the surgeons determined that the expanded hydrogel was the cause of the compression [3]. Differences between the two cases: In our case the lesion appears during the intervention, therefore it seems unlikely that it is the mass effect of the duraseal that has not had time to consolidate, the one responsible for the motor injury. Rather, it would be a repeated microtrauma during the release of the common ligament. Posterior or a contact during the disc excrescence causes the injury. In the other cases examined, the time necessary for the appearance of neurological locality was much higher, 9 days in Lumbar pathology; In experimental studies, it took between 3 days and 2 weeks to obtain a neurological lesion [4, 5]. A review in the literature reveals an extensive list of complications in anterior cervical spine surgery. Although, many of them are extremely rare [6]. The percentage of complications in anterior cervical surgery ranges from 5% to 30% of cases [7], and 9.8% if we consider only complications that remain permanently as morbidity. In some studies they speak of the epidural hematoma as a complication of anterior cervical surgery. It occurs in 1% of surgeries [7].
The appearance of a new neurological deficit is a rare complication. If the neurological deficit becomes evident immediately after the intervention, the most probable cause of the deficit is due to surgical trauma or problems related to the position or manipulation of the neck during intubation [8]. Between 1.3% to 11% there is a new radicular deficit, and from 0.7 to 3.1% worsening of the spinal deficit [8]. The rupture of the dura mater and cerebrospinal fluid fistula occur between 3.1% to 14% [9]. Surgery carries a risk with percentages of probabilities of improvement, but also of complications and are likely not assurances of improvement if not probability of improvement and also probability or possibility of complications.
References
- Akeson WH, Massie JB, Huang B, et al. Topical high-molecular-weight hyaluronan and roofing barrier sheet equally inhibit postlaminectomy fibrosis. The Spine Journal 5 (2005): 180-1
- Boogaarts JD, Grotenhuis JA, Bartels RH, et al. Use of a novel absorbable hydrogel for augmentation of dural repair: resultsof apreliminary clinical study. Neurosurgery 57 (2005): 146-151.
- Thavarajah D, De Lacy PD, Hussain R, et al. Postoperative cervical cord compression induced by hydrogel (duraseal): a possible complication. Spine (PhilaPa 1976) 35 (2010): 25-26.
- Blackburn SL, Smyth MD. Hydrogel-induced cervico medullary compression after posterior fossa decompression for chiari malformation.case report. J Neurosurg 106 (2007): 302-304.
- Neuman BJ, Radcliff K, Rihn J. Cauda equina syndrome after a TLIF resulting from postoperative expansion of a hydrogel dural sealant. Clin Orthop Relat Res 470 (2012): 1640-1645.
- Kim KD, Wright NM. The Spinal Sealant Study Group: polyethyleneglycol (PEG) hydrogel spinal sealant (duraSeal™ spinal sealant) as an adjunct to sutured dural repair in the spine: resultsof a prospective, multicenter, randomized controlled study. Spine (Phila Pa 1976) 36 (2011): 1906-1912.
- Lee G, Lee CK, Bynevelt M. Duraseal-hematoma: concealed hematoma causing spinal cord compression. Spine (Phila Pa 1976) 35 (2010): 1522-1524.
- Martín R, Carda JR, Pinto JI, et al. Discectomia cervical y artrodesisIntersomática mediante la técnica de Cloward: Análisis retrospectivo de las complicaciones y de los resultados radiológicos en 167 casos. Neurocirugía 13 (2002): 265-284.
- Hanbali F, Gokaslan Z, Cooper Ventral and Ventrolateral subaxial descompression. En: Spine Surgery: Techniques, complications, avoidance and management. Philadelphia, Elsevier (2005): 341-350.
