Misunderstandings in Interpersonal and Inter-Professional Communication and their Impact On Health Outcomes and Patient Safety
Article Information
Nabi Fatahi*
Department of Learning and Leadership for Health Care Professionals, Institute of Health and Care Sciences, The Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden
*Corresponding Author: Dr. Nabi Fatahi, Department of Learning and Leadership for Health Care Professionals, Institute of Health and Care Sciences, The Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden
Received: 17 August 2019; Accepted: 07 September 2019; Published: 26 November 2019
Citation: Nabi Fatahi. Misunderstandings in Interpersonal and Inter-Professional Communication and their Impact On Health Outcomes and Patient Safety. Archives of Clinical and Medical Case Reports 3 (2019): 585-590.
View / Download Pdf Share at FacebookAbstract
Since clinical health communication is the basic stage in the process of diagnosis and treatment, adequate clinical interaction is essential between patients and healthcare providers, as well as between the clinicians involved. The healthcare communication modes that are the focus of this study are interpersonal and inter-professional encounters, which in both cases involve both oral and written communication. This paper will review the literature on factors influencing clinical encounters and their impact on health outcomes and patient safety. Inadequate oral and written communication leads to misunderstanding in clinical encounters, which causes patient insecurity. In addition to language and culture, as the main factors that influence communication outcome, professionalism, caring attitudes, time, respect and openness are additional factors that are frequently mentioned in this context. Oral communication between healthcare providers may be performed directly or through a third person (interpreter) who facilitates encounters in cases of a language barrier between patient and the caregiver. Mutual understanding in both interpersonal and inter-professional communication is very important for quality health care and patient satisfaction. Written misunderstandings are more visible in inter-professional encounters, whereas in interpersonal communication oral misunderstandings are more frequent. Cultural misunderstandings in clinical encounters may be rooted in individual, organizational or ethnic and cultural backgrounds. The last will be in focus in this study. Due to the importance of communication as the fundamental stage in diagnosis and treatment procedures, it is vital to prevent misunderstandings in communication between patients and caregivers during clinical encounters as well as between the clinicians involved.
Keywords
Clinical health communication; Inter-professional clinical encounters; Health outcome
Clinical health communication articles, Inter-professional clinical encounters articles, Health outcome articles
Clinical health communication articles Clinical health communication Research articles Clinical health communication review articles Clinical health communication PubMed articles Clinical health communication PubMed Central articles Clinical health communication 2023 articles Clinical health communication 2024 articles Clinical health communication Scopus articles Clinical health communication impact factor journals Clinical health communication Scopus journals Clinical health communication PubMed journals Clinical health communication medical journals Clinical health communication free journals Clinical health communication best journals Clinical health communication top journals Clinical health communication free medical journals Clinical health communication famous journals Clinical health communication Google Scholar indexed journals health articles health Research articles health review articles health PubMed articles health PubMed Central articles health 2023 articles health 2024 articles health Scopus articles health impact factor journals health Scopus journals health PubMed journals health medical journals health free journals health best journals health top journals health free medical journals health famous journals health Google Scholar indexed journals Inter-professional clinical encounters articles Inter-professional clinical encounters Research articles Inter-professional clinical encounters review articles Inter-professional clinical encounters PubMed articles Inter-professional clinical encounters PubMed Central articles Inter-professional clinical encounters 2023 articles Inter-professional clinical encounters 2024 articles Inter-professional clinical encounters Scopus articles Inter-professional clinical encounters impact factor journals Inter-professional clinical encounters Scopus journals Inter-professional clinical encounters PubMed journals Inter-professional clinical encounters medical journals Inter-professional clinical encounters free journals Inter-professional clinical encounters best journals Inter-professional clinical encounters top journals Inter-professional clinical encounters free medical journals Inter-professional clinical encounters famous journals Inter-professional clinical encounters Google Scholar indexed journals Health outcome articles Health outcome Research articles Health outcome review articles Health outcome PubMed articles Health outcome PubMed Central articles Health outcome 2023 articles Health outcome 2024 articles Health outcome Scopus articles Health outcome impact factor journals Health outcome Scopus journals Health outcome PubMed journals Health outcome medical journals Health outcome free journals Health outcome best journals Health outcome top journals Health outcome free medical journals Health outcome famous journals Health outcome Google Scholar indexed journals Gamer’s articles Gamer’s Research articles Gamer’s review articles Gamer’s PubMed articles Gamer’s PubMed Central articles Gamer’s 2023 articles Gamer’s 2024 articles Gamer’s Scopus articles Gamer’s impact factor journals Gamer’s Scopus journals Gamer’s PubMed journals Gamer’s medical journals Gamer’s free journals Gamer’s best journals Gamer’s top journals Gamer’s free medical journals Gamer’s famous journals Gamer’s Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals cuirasse articles cuirasse Research articles cuirasse review articles cuirasse PubMed articles cuirasse PubMed Central articles cuirasse 2023 articles cuirasse 2024 articles cuirasse Scopus articles cuirasse impact factor journals cuirasse Scopus journals cuirasse PubMed journals cuirasse medical journals cuirasse free journals cuirasse best journals cuirasse top journals cuirasse free medical journals cuirasse famous journals cuirasse Google Scholar indexed journals caregivers articles caregivers Research articles caregivers review articles caregivers PubMed articles caregivers PubMed Central articles caregivers 2023 articles caregivers 2024 articles caregivers Scopus articles caregivers impact factor journals caregivers Scopus journals caregivers PubMed journals caregivers medical journals caregivers free journals caregivers best journals caregivers top journals caregivers free medical journals caregivers famous journals caregivers Google Scholar indexed journals infusion articles infusion Research articles infusion review articles infusion PubMed articles infusion PubMed Central articles infusion 2023 articles infusion 2024 articles infusion Scopus articles infusion impact factor journals infusion Scopus journals infusion PubMed journals infusion medical journals infusion free journals infusion best journals infusion top journals infusion free medical journals infusion famous journals infusion Google Scholar indexed journals patient articles patient Research articles patient review articles patient PubMed articles patient PubMed Central articles patient 2023 articles patient 2024 articles patient Scopus articles patient impact factor journals patient Scopus journals patient PubMed journals patient medical journals patient free journals patient best journals patient top journals patient free medical journals patient famous journals patient Google Scholar indexed journals
Article Details
1. Background
1.1 Clinical health communication
Despite differences in the definition of health communication because of its multidisciplinary nature, its role concerning health outcomes in both individual and public health seems to be common to most definitions [1]. Health communication offers a unique opportunity to healthcare professionals to provide an expressive contribution to improving and saving human lives [2]. Healthcare communication usually occurs at two levels, interpersonal and inter-professional, which both involve oral as well as written communications. Due to inequality in power and situations, clinical health communication is quite different from other types of human communication. Healthcare providers have the opportunity to decide about communication, where test results (diagnosis) are an obvious issue in this inequality of power in clinical health communication. Thus, efforts to minimize the factors that have an negative effect on clinical communication may have an important impact on the communication outcome [1]. Since the health communication theory moved away from the Shannon- Weaver linear model of communication and focused on Gamer’s “Circularity of the process of understanding” a meaningful concept has been provided, particularly regarding clinical health communication [4, 5].
1.2 Inter-professional clinical encounters
Poor communication in inter-professional interaction in healthcare has a significant impact on patient outcomes. In order to achieve satisfactory health outcomes, improving inter-professional communication skills is crucial [6]. According to a study in Canada, inter-professional communication and collaboration are considered as the key building blocks to improve patient safety and meet the requirements for increasingly satisfactory care. [7]. Mutual understanding in inter-professional communication is of great importance for quality in health care [8]. Communication quality in inter-professional contacts has a significant effect in management of patient cases, and treatment procedures, which is essential for patient safety [9]. Insufficient communication between healthcare professionals has been identified as one of the main causes of medical mistakes that adversely affect the health of the patient [10, 11]. Working in an inter-professional context requires greater sensitivity to social issues within the team and willingness to share roles in developing cooperation and working methods. Inter-professional cooperation improves through strategies to improve and enhance joint activities, such as seminars and workshops for professionals who have frequent contact in relation to their duties [12, 13]. At the same time, over the last few decades the introduction of electronic communication [12, 13], has brought a new challenge for staff familiar with traditional inter-professional communication [14]. This is particularly evident in radiology, where the delivery of radiological images and radiologist reports are electronically based on digital images and filing systems. Due to the fact that radiologists receive enormous numbers of requests from clinicians every day for producing radiologist reports as a response to clinicians, written inter-professional communication is the most important and obvious issue in this context [13].
1.3 Interpersonal communication
Interpersonal communication means people’s communication with each other in a face-to-face context, that provides a structure for a complete introduction to the how and why of this kind of communication [1]. A previous study indicated that effective strategies in interpersonal communication in both inter-professional and personal settings has a significant impact on nurses’ well-being and reducing stress and improving the quality of their lives [16]. Due to the importance of interpersonal communication in the process of the transfer of knowledge in both individuals and organizations, its improvement influences the quality of the communication outcome [17, 18]. The most common interpersonal, clinical health communication occurs between patients and caregivers, and it may performed directly or through interpreters, it may be cross-cultural or non-cross-cultural, as shown in Figure 1 [19].
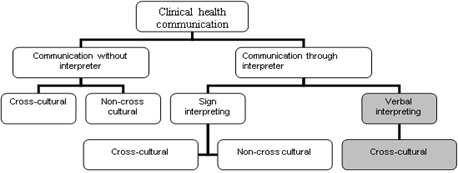
Figure 1: Clinical health communication modes.
Although misunderstandings in interpersonal health communication occur in both cross-cultural and non-cross-cultural situations, they are more frequently in cross-cultural encounters [19]. Despite similarities in the biological nature of disease, there are obvious differences concerning the understanding of health and illness between different societies [20]. Cross-cultural communication will be more complicated when a language barrier is also involved. Interpersonal communication is a social interaction that is influenced by socio-cultural and emotional aspects [21]. Language and culture are considered to be the basic elements of all communication, which means that understanding both language and culture is considered as prerequisite for good cross-cultural communication [22]. In interaction with patients, who have a different linguistic and cultural background, one should be aware that communication is affected by culture in both verbal and non-verbal issues [23]. Apart from the language barrier, there are other factors that influence health communication through interpreters, as shown in Figure 2 [24].
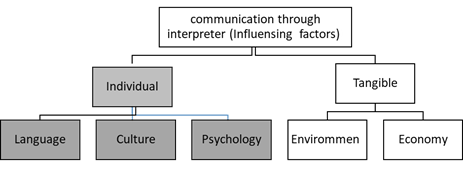
Figure 2: Factors influencing communication.
2. Discussion
Satisfactory inter-professional clinical consultation has a significant impact on health outcome and influences patient safety. Due to the role of the radiologist in the diagnosis of diseases, consultation between clinicians and radiologists in both written and oral forms, adequate clinical communication and mutual understanding are crucial. According to a previous study [31] although difficulties were more frequently in written communication, a number of problems were highlighted in both oral and written consultation by radiologists. Problems with request forms were reported by radiologists concerning deficient patient history, as well as inappropriate choices of examination mode, unclear clinical questions, lack of specific terms and unclear abbreviations on the request form. Difficulties in oral communication reported by clinicians were inadequate attention being paid by participating clinicians during radiology conferences and problems reaching the referring clinicians by telephone when it was necessary [13]. A previous study showed that cooperation and satisfactory inter-personal communication are needed to provide adequate care to patients [25].
The most common interpersonal clinical encounter occurs between patients and healthcare providers. Oral communication is the first stage in interaction between healthcare professionals and patients. Encounters between patients and healthcare professionals are either performed directly or through an interpreter. Although there is a risk of misunderstandings in both the above-mentioned clinical encounters, they are more frequent when there is a language barrier and when a third person (interpreter) is involved in the clinical encounter [26].In oral communication, there is a risk of both linguistic and cultural misunderstandings in cases of communication through interpreters. In order to prevent misunderstandings, we should use professional interpreters rather than the patient’s friend or her/his relatives as a language bridge to the patient [27]. The prerequisites for satisfactory clinical encounters through interpreters are the interpreter’s competence and neutrality in language, relationship and gender (triangle neutrality). Patients’ relatives or friends often do not have sufficient language competence and there is no guarantee that they are acting neutrally during the interpretation.
Assigning interpreters according to the patients’ mother tongue has a significant impact on the communication outcome. If the interpreter and the patient share the same language, just two languages will be involved in the interpretation process (bilingual interpretation process). If interpreters are assigned according to the patients’ citizenship sometimes the patient and the interpreter do not share the same language, so that three languages are involved in the interpretation process (trilingual), in this context the risk of misunderstanding is considerably greater than in a bilingual process [28].
3. Conclusion
In order to minimize misunderstandings in inter-professional and interpersonal, clinical encounters, satisfactory communication, both in written and oral form is crucial. Overall, oral communication between clinicians and radiologists functions well. Limitations in writing communications have been identified, in information about the patients’ data, disease history and examinations. Due to the language barrier and cultural diversity in interpersonal communication, there is a risk of misunderstandings. Joint meetings between radiologists and referring clinicians are necessary for both of them to understand the needs of the other party and to improve communication quality. Avoiding unqualified interpreters and assigning them according to the patient’s mother tongue rather than the patient’s citizenship has a significant impact on communication outcome and patient safety.
References
- Schiavo R. Health communication - from theory to practice. Jossey-Bass Publishing, San Fransisco (2007): 3-7.
- Rajiv N Rimal, Maria K Lapinski. Why health communication is important in public health.Bulletin of the World Health Organization 87 (2009): 247-247.
- Fatahi N. Cross-Cultural encounters through interpreter - Experiences of patients, interpreters and healthcare professionals. Avhandling. Göteborgs universtitet (2010).
- Shannon CE, Weaver W. The mathematical theory of communication.University of Illinois Press, Chicago (1949): 6-10.
- Debesay J, Nåden D, Slettebø Å. How do we close the hermeneutic circle? A Gadamerian approach to justification in interpretation in qualitative studies.Nursing Inquiryn15 (2008): 57-66.
- Foronda C, MacWilliams B, McArthur E. Inter-professional communication in healthcare: An integrative review. Nurse Educ Pract 19 (2016): 004-005.
- Katheen R et al. An intervention to improve inter-professional collaboration and communications: A comparative qualitative study. Journal of Inter-professional Care. July 24 (2010): 350-361.
- Schiavo R. Health communication - from theory to practice. Jossey-Bass Publishing, San Fransisco (2007): 3-7.
- Vasiliki M, etal. Physician and nursing perceptions concerning inter-professional communication and collaboration. J Interprof Car 28 (2014): 526-533.
- Kundel HL, Seshadri SB, Langlotz CP, et al. Prospective study of a PACS: information flow and clinical action in a medical intensive care unit. Radiology 199 (1996): 143-149.
- Smith T, Jones P. Remote x-ray operator radiography: A case study in inter-professional rural clinical practice. Journal of Inter-professional Care (2007): 289-302.
- Katheen R. An intervention to improve inter-professional collaboration and communications: A comparative qualitative study. Journal of Inter-professional Care 4 (2010): 350-361.
- Fatahi N, Krupic F, Hellström M. Quality of radiologists' communication with other clinicians--As experienced by radiologists. Patient Educ Couns. 98 (2015): 722-727.
- Watkins J. A hospital-wide picture archiving and communication system (PACS): the views of users and providers of the radiology service at Hammersmith Hospital. Eur J Radiol 32 (1999): 106-112.
- Hartley P. Interpersonal Communication Second edition Taylor & Francis e: New York (2001).
- Vertino KA. Effective Interpersonal Communication: A Practical Guide to Improve Your Life. Online J Issues Nurs 19 (2014): 1.
- Gainforth HL, Latimer-Cheung AE, Athanasopoulos P, et al. The role of interpersonal communication in the process of knowledge mobilization within a community-based organization: a network analysis. Implement Sc 59 (2014): 9-59.
- Siburian TA. The Effect of Interpersonal Communication, Organizational Culture, Job Satisfaction, and Achievement Motivation to Organizational Commitment of State High School Teacher in the District Humbang Hasundutan, North Sumatera, Indonesia International Journal of Humanities and Social Science 12 (2013): 247-263.
- Fatahi N. Cross-cultural encounters through interpreter - experiences of patients, interpreters and healthcare professionals. Gothenburg: University of Gothenburg (2010).
- Bishop GD. Health and illness: Mental representations in different cultures. In: International Encyclopaedia of the Social and Behavioural Sciences. Singapore: National University of Singapore (2002).
- Courteille O. Computer simulations of the clinical counter-perception and educational aspects [dissertation]. Stockholm: Karolinska institutet (2008).
- Blomsterberg M. Att förstå och bli förstådd. Om etnisk och kulturell mångfald i primärvårdsarbete. Göteborg: Göteborgs universitet (2004): 3-24.
- Backlund B. Inte bara ord – en bok om talad kommunikation. Lund: Studentlitteratur; 1991. p. 19-34. Smith M1, Greene BR, Haas M, Allareddy V. Intra-professional and inter-professional referral patterns of chiropractors. Chiropr Osteopat 6 (2006): 14-12.
- Fatahi N. Cross-cultural health communication through interpreter. Gothenburg: University of Gothenburg department of primary healthcare (2006).
- Smith M, Greene BR, Haas M, et al. Intra-professional and inter-professional referral patterns of chiropractors. Chiropr Osteopat 6 (2006): 14:12.
- Fatahi N, Hellström M, Skott C, et al. General practitioners' views on consultations with interpreters: a triad situation with complex issues. Scand J Prim Health Care 26 (2008): 40-45.
- Rew KT, Clarke SL, Gossa W, et al. Immigrant and refugee health: cross-cultural communication. FP Essent 23 (2014): 30-39.
- Fatahi N. Trilingual Clinical Encounters and Its Impact on Communication Outcome- Case Reports in Healthcare Settings. J Family Med Community Health 2 (2015): 1038.
