Minimally-Invasive Treatment of Multiple Trauma Concomitant with Idiopathic Portal Hypertension (IPH)
Article Information
Tae-Hyok RI*, Hak-Su Kim, Chang-Hwan O, In-Song RI
Pyongyang Medical College, KIM IL SUNG University, Pyongyang, Democratic People’s Republic of Korea
*Corresponding Author: Tae-Hyok RI, Pyongyang Medical College, KIM IL SUNG University, Pyongyang, Democratic People’s Republic of Korea
Received: 01 December 2019; Accepted: 10 December 2019; Published: 30 December 2019
Citation: Tae-Hyok RI, Hak-Su Kim, Chang-Hwan O, In-Song RI. Minimally-Invasive Treatment of Multiple Trauma Concomitant with Idiopathic Portal Hypertension (IPH). Journal of Orthopaedics and Sports Medicine 1 (2019): 114-119
View / Download Pdf Share at FacebookAbstract
Context: Multiple trauma concomitant with idiopathic portal hypertension (IPH) encountered in orthopaedics department is very rare.
Methods and Material: A 23-year old male presented with right femoral subtrochanteric fracture and ipsilateral open tibial and fibular fracture. He had been suffered IPH from childhood and his laboratory test results was too poor to undergo invasive surgery. Minimally invasive treatment fashions were selected, including skeletal traction, external fixation and autograft skin coverage.
Results: At follow-up of 8 months, he regained full weight bearing function and was satisfied with the result.
Conclusions: Selection of minimally invasive treatment options in case of multiple trauma concomitant with severe systemic lesion like IPH is mandatory to avoid massive and critical invasion, and to recover limb’s function properly.
Keywords
Minimally invasive; Multiple trauma; Idiopathic portal hypertension (IPH)
Idiopathic Portal Hypertension articles Idiopathic Portal Hypertension Research articles Idiopathic Portal Hypertension review articles Idiopathic Portal Hypertension PubMed articles Idiopathic Portal Hypertension PubMed Central articles Idiopathic Portal Hypertension 2023 articles Idiopathic Portal Hypertension 2024 articles Idiopathic Portal Hypertension Scopus articles Idiopathic Portal Hypertension impact factor journals Idiopathic Portal Hypertension Scopus journals Idiopathic Portal Hypertension PubMed journals Idiopathic Portal Hypertension medical journals Idiopathic Portal Hypertension free journals Idiopathic Portal Hypertension best journals Idiopathic Portal Hypertension top journals Idiopathic Portal Hypertension free medical journals Idiopathic Portal Hypertension famous journals Idiopathic Portal Hypertension Google Scholar indexed journals Liver cirrhosis articles Liver cirrhosis Research articles Liver cirrhosis review articles Liver cirrhosis PubMed articles Liver cirrhosis PubMed Central articles Liver cirrhosis 2023 articles Liver cirrhosis 2024 articles Liver cirrhosis Scopus articles Liver cirrhosis impact factor journals Liver cirrhosis Scopus journals Liver cirrhosis PubMed journals Liver cirrhosis medical journals Liver cirrhosis free journals Liver cirrhosis best journals Liver cirrhosis top journals Liver cirrhosis free medical journals Liver cirrhosis famous journals Liver cirrhosis Google Scholar indexed journals Variceal articles Variceal Research articles Variceal review articles Variceal PubMed articles Variceal PubMed Central articles Variceal 2023 articles Variceal 2024 articles Variceal Scopus articles Variceal impact factor journals Variceal Scopus journals Variceal PubMed journals Variceal medical journals Variceal free journals Variceal best journals Variceal top journals Variceal free medical journals Variceal famous journals Variceal Google Scholar indexed journals Invasive surgery articles Invasive surgery Research articles Invasive surgery review articles Invasive surgery PubMed articles Invasive surgery PubMed Central articles Invasive surgery 2023 articles Invasive surgery 2024 articles Invasive surgery Scopus articles Invasive surgery impact factor journals Invasive surgery Scopus journals Invasive surgery PubMed journals Invasive surgery medical journals Invasive surgery free journals Invasive surgery best journals Invasive surgery top journals Invasive surgery free medical journals Invasive surgery famous journals Invasive surgery Google Scholar indexed journals Subtrochanteric fracture articles Subtrochanteric fracture Research articles Subtrochanteric fracture review articles Subtrochanteric fracture PubMed articles Subtrochanteric fracture PubMed Central articles Subtrochanteric fracture 2023 articles Subtrochanteric fracture 2024 articles Subtrochanteric fracture Scopus articles Subtrochanteric fracture impact factor journals Subtrochanteric fracture Scopus journals Subtrochanteric fracture PubMed journals Subtrochanteric fracture medical journals Subtrochanteric fracture free journals Subtrochanteric fracture best journals Subtrochanteric fracture top journals Subtrochanteric fracture free medical journals Subtrochanteric fracture famous journals Subtrochanteric fracture Google Scholar indexed journals Fibular fracture articles Fibular fracture Research articles Fibular fracture review articles Fibular fracture PubMed articles Fibular fracture PubMed Central articles Fibular fracture 2023 articles Fibular fracture 2024 articles Fibular fracture Scopus articles Fibular fracture impact factor journals Fibular fracture Scopus journals Fibular fracture PubMed journals Fibular fracture medical journals Fibular fracture free journals Fibular fracture best journals Fibular fracture top journals Fibular fracture free medical journals Fibular fracture famous journals Fibular fracture Google Scholar indexed journals Skeletal traction articles Skeletal traction Research articles Skeletal traction review articles Skeletal traction PubMed articles Skeletal traction PubMed Central articles Skeletal traction 2023 articles Skeletal traction 2024 articles Skeletal traction Scopus articles Skeletal traction impact factor journals Skeletal traction Scopus journals Skeletal traction PubMed journals Skeletal traction medical journals Skeletal traction free journals Skeletal traction best journals Skeletal traction top journals Skeletal traction free medical journals Skeletal traction famous journals Skeletal traction Google Scholar indexed journals Orthopaedic articles Orthopaedic Research articles Orthopaedic review articles Orthopaedic PubMed articles Orthopaedic PubMed Central articles Orthopaedic 2023 articles Orthopaedic 2024 articles Orthopaedic Scopus articles Orthopaedic impact factor journals Orthopaedic Scopus journals Orthopaedic PubMed journals Orthopaedic medical journals Orthopaedic free journals Orthopaedic best journals Orthopaedic top journals Orthopaedic free medical journals Orthopaedic famous journals Orthopaedic Google Scholar indexed journals Soft tissue necrosis articles Soft tissue necrosis Research articles Soft tissue necrosis review articles Soft tissue necrosis PubMed articles Soft tissue necrosis PubMed Central articles Soft tissue necrosis 2023 articles Soft tissue necrosis 2024 articles Soft tissue necrosis Scopus articles Soft tissue necrosis impact factor journals Soft tissue necrosis Scopus journals Soft tissue necrosis PubMed journals Soft tissue necrosis medical journals Soft tissue necrosis free journals Soft tissue necrosis best journals Soft tissue necrosis top journals Soft tissue necrosis free medical journals Soft tissue necrosis famous journals Soft tissue necrosis Google Scholar indexed journals Liver function articles Liver function Research articles Liver function review articles Liver function PubMed articles Liver function PubMed Central articles Liver function 2023 articles Liver function 2024 articles Liver function Scopus articles Liver function impact factor journals Liver function Scopus journals Liver function PubMed journals Liver function medical journals Liver function free journals Liver function best journals Liver function top journals Liver function free medical journals Liver function famous journals Liver function Google Scholar indexed journals
Article Details
1. Introduction
The management for multiple trauma patient is not simple and requires application of various modes and steps according to area, property, severity and type of existing injury. Furthermore, if there is trauma which requires invasive operation, but it accompanies a pre-existing systemic lesion, it makes the management very difficult [1-3].
Idiopathic portal hypertension (IPH) is the lesion that is characterized by the presence of portal hypertension in the absence of liver cirrhosis [4-9]. The key issues in the management of patients with IPH are related mainly to management and prevention of variceal hemorrhage. If severe trauma accompanies this lesion, invasive surgery is contraindicative [4, 6, 9]. The patient in the case had been suffered IPH from childhood and had several times of intervention to treat it. Unfortunately he injured in traffic accident and suffered right femoral subtrochanteric fracture and ipsilateral open tibial and fibular fracture. Both injuries needed invasive operations, but his liver condition didn’t allow it, thus we sought minimally-invasive alternative to recover injured limb’s function and treated him for 47 days. At 6-month follow-up after discharge the patient regained ambulatory function for full weight bearing and was satisfied with the result. We experienced that correct selection of minimally-invasive fashion in multiple trauma patient concomitant with systemic lesion which is contraindication for major open surgery could recover function of injured limb and yield comparatively fair result.
2. Case Report
A 23 year-old male was injured by wheel of truck December 12th 2016 and received emergent debridement for his open tibial fracture and skeletal traction for ipsilateral femoral fracture; then transferred to our hospital December 26th. He was diagnosed IPH in August 2012 and received intervention therapy to embolize splenic artery, but didn’t find any effect. Orthopaedic diagnosis was right femoral subtrochanteric fracture (AO 32-B1.1), ipsilateral open tibial and fibular complex fracture (AO 42-B3.3, Gustilo type III B2), soft tissue necrosis and acute osteomyelitis (Figure 1). Laboratory test results were RBC 2.7T/L, ESR 31mm/h, Hb 10.0g/dL, ALB 3.0g/dL, CHE* 756U/L, ALT 128U/L, AST 116U/L, ZTT 15.0U, S-P 5.3%. (*: Acetylthiocholine method, normal range 1579-2535). Ultrasound findings: normal size, high echo, irregular vessels of the liver, splenomegaly grade III, low-echo around upper pole of spleen, small amount of ascites.
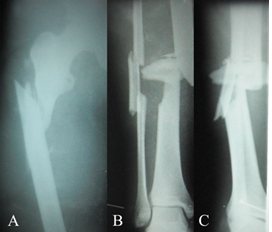
Figure 1: Radiographs at admission. A. Right femoral subtrochanteric fracture (AO 32-B1.1); B and C. Ipsilateral open tibial and fibular complex fracture (AO 42-B3.3, Gustilo Type III B2), B. AP; C. Lateral view.
On endoscopy finding of his stomach there was esophageal varix grade III, erosive gastritis.In consultation with internal medicine department he was diagnosed idiopathic portal hypertension (IPH). The patient was concomitant with IPH and poor liver function, in addition there was esophageal varix on endoscopy, otherwise ORIF for right femoral subtrochanteric fracture, and secondary debridement, pedicle flap transplantation and external fixation for open tibial fracture were appropriate. Unfortunately he was not suitable for indication for invasive ORIF, and large operative invasion might threaten his life critically. We selected skeletal traction for right femoral subtrochanteric fracture; external fixation and epithelial skin grafting for open tibial fracture and soft tissue necrosis. The skeletal traction weight for right femoral subtrochanteric fracture was set to 9kg that was about 15% of patient’s body weight at the outset, and was reduced to 6Kg 7 weeks later.
Immediately after secondary debridement of the wound of open tibial fracture, external fixation was applied. There was partial necrosis of the wound 17 days following trauma, and after resection of it, proximal and distal ends and some part of fragment were exposed. A few days later partial decortication of exposed bone, drilling of free fragment and epithelial skin grafting were done. (Figure 2). There was angulation deformity of tibial fracture on postoperative 5-day X-ray finding, which needed correction.Laboratory tests 6 days after operation were RBC 3.08T/L, ESR 37mm/h, ALT 119/L, AST 94U/L.There was no systemic or local abnormal hemorrhage. Because union of subtrochanteric fracture was identified 8 weeks after trauma, skeletal traction was removed; we encouraged knee motion. The area of tibial wound was reduced to about 1cm×1cm and he discharged (Figure 3). 8 months after trauma his wound was nearly healed and the patient visited our department on his foot; at this time there was radiographic finding of union at the open tibial fracture and full weight bearing; we removed external fixation, and he was satisfied with the result (Figures 4 and 5).

Figure 2: Wound of open tibial fracture site at 22 post-operative day.
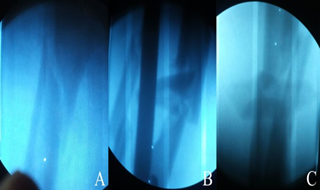
Figure 3: X-ray findings 7 weeks after trauma. A. Union of right femoral subtrochanteric fracture was identified; B. Open tibial fracture, AP; C. Lateral view.

Figure 4: X-ray findings 8 months after trauma. A. Full union of right femoral subtrochanteric fracture was identified; B. Union of open tibial and fibular fracture was identified, AP; C. Lateral view.

Figure 5: Wound of open tibial fracture site was nearly healed.
3. Discussion
Because of preserved liver function, the prognosis of patients with IPH is better than that of patients with cirrhosis who have a similar degree of portal hypertension. However, a subgroup of IPH patients progresses to develop advanced hepatic insufficiency, eventually requiring liver transplantation [4-6]. The key issues in the management of patients with IPH are related mainly to management and prevention of variceal hemorrhage [4, 8]. Multiple trauma concomitant with IPH is rare, and if invasive surgery is expected it could result in critical outcome without considering condition of liver and effect to the system [4, 7, 9]. The patient in the case had been suffered IPH from childhood and had several interventions for it. Unfortunately he injured in traffic accident and suffered right femoral subtrochanteric fracture and ipsilateral open tibial and fibular fracture. Both injuries needed invasive operations, but his liver condition didn’t allow it, thus we sought minimally-invasive alternative to recover limb’s function. Eventually we applied minimally-invasive fashions like skeletal traction for femoral subtrochanteric fracture, external fixation and epithelial skin grafting for open tibial fracture; thus found relatively fair result. Though skeletal traction and external fixation for fracture treatment are relatively conventional and conservative fashions [1-3, 10], we experienced that proper combination of these methods are minimally-invasive and effective when patient’s condition is bad or concomitant with a lesion not allowing major surgery invasion. In addition, we confirmed again that relatively large butterfly fragment which is partially exposed should not be removed and managed carefully; then it could play a positive role in fracture union.
4. Conclusion
We consider that proper application of minimally-invasive methods such as skeletal traction or external fixation in multiple trauma patient concomitant with IPH like this case can result in fair result.
References
- Marvin Tile. Fractures of the Tibia In: Joseph Schatzker (editor) The Rationale of Operative Fracture Care. 3rd ed. Springer, Berlin (2005): 515-517.
- Matthew I, Rudloff. Fractures of the Lower Extremity. In Campbell’s Operative Orthopaedics. 12th ed. S. Terry Canale and James H. Beaty (eds.). Mosby, Philadelphia (2013): 2657-2662.
- Saleh M, Yang L, Nayagam S. External fixation of complex tibial fractures. Injury, Int. J. Care Injured 29 (1998): 155.
- Vispo E, Morello J, Rodriguez-Novoa S, et al. Noncirrhotic portal hypertension in HIV infection. Curr. Opin. Infect. Dis 24 (2011): 12.
- Yamaguchi E, Yamanoi A, Ono T, et al. Experimental investigation of the role of endothelin-1 in idiopathic portal hypertension. J. Gastroenterol. Hepatol 22 (2007): 1134.
- Okudaira M, Ohbu M, Okuda K. Idiopathic portal hypertension and its pathology. Semin. Liver. Dis 22 (2002): 59.
- de Franchis R, Baveno V. Revising consensus in portal hypertension: report of the Baveno V consensus workshop on methodology of diagnosis and therapy in portal hypertension. J. Hepatol 53 (2010): 762.
- Sarin SK, Gupta N, Jha SK. Equal efficacy of endoscopic variceal ligation and propranolol in preventing variceal bleeding in patients with noncirrhotic portal hypertension. Gastroenterology 139 (2010): 1238.
- Schouten JN, Nevens F, Hansen B. Idiopathic noncirrhotic portal hypertension is associated with poor survival: results of a long-term cohort study. Aliment. Pharmacol. Ther 35 (2012): 1424.
- Canovas F, Bonnel F, Faure F. Extensive bone loss in an open tibial shaft fracture (immediate bone boiling reimplantation) Injury Int. J. Care Injured 30 (1999): 709-710.
