Minimally Invasive Surgical Access to Aortic Valve Replacement: Comparison Between Minithoracotomy & Ministernotomy in A Systematic Review
Article Information
Linda Renata Micali, Mohammed Abualsaud, Gianmarco Parise, Cecilia Tetta, Orlando Parise, Francesco Matteucci, Monique de Jong, Massimo Bonacchi, Sandro Gelsomino*
Department of Cardiothoracic Surgery, Cardiovascular Research Institute, Maastricht University, Universiteitssingel 50, 6229 ER Maastricht, The Netherlands
*Corresponding author: Sandro Gelsomino, Department of Cardiothoracic Surgery, Cardiovascular Research Institute, Maastricht University, Universiteitssingel 50, 6229 ER Maastricht, The Netherlands
Received: 11 November 2019; Accepted: 20 November 2019; Published: 23 December 2019
Citation: Linda Renata Micali, Mohammed Abualsaud, Gianmarco Parise, Cecilia Tetta, Orlando Parise, Francesco Matteucci, Monique de Jong, Massimo Bonacchi, Sandro Gelsomino. Minimally Invasive Surgical Access to Aortic Valve Replacement: Comparison Between Minithoracotomy & Ministernotomy in A Systematic Review. Cardiology and Cardiovascular Medicine 3 (2019): 450-463.
View / Download Pdf Share at FacebookAbstract
Background: Minimally invasive aortic valve replacement (MIAVR) procedures are starting to be accepted as the standard procedures for aortic valve diseases. However, only a limited number of studies have directly compared mini-thoracotomy (MT) to mini-sternotomy (MS). Therefore, the aim of this review was to summarize the available literature for comparison between the procedures to have a better understanding of the risks and benefits to guide future procedures.
Methods: A literature search for MT and MS was carried out using two literature databases. Relevant articles were identified and assessed through the inclusion and exclusion criteria.
Results: 15 studies were identified for inclusion in this review. Comparable results were identified between MT and MS in terms of 30-day mortality. In addition, there was no difference in the incidence of stroke, reoperation for bleeding, and wound infection. In contrast, MT showed longer cardiopulmonary bypass (CPB) and cross-clamping durations than MS. Conclusion: Both MT and MS surgical approaches are reliable, efficient, and comparable. These findings have to be confirmed by large randomized trials
Keywords
Minimally invasive; Aortic valve replacement; Minithoracotomy; Ministernotomy
Minimally invasive articles, Aortic valve replacement articles, Minithoracotomy articles, Ministernotomy articles
Article Details
Introduction
Aortic valve (AV) disease affects 2% of the general adult population in industrialized countries [1].
Among surgical option, minimally invasive aortic valve replacement (MIAVR) has been recently introduced into clinical practice [2]. MIAVR involves a small incision in the chest wall as opposed to a conventional full sternotomy (FS) with the aim of reducing the invasiveness of the conventional surgical procedures whilst maintaining efficacy and quality in terms of final outcomes.
Indeed, when compared to FS, MIAVR has shown early and long-term benefits, including reduced postoperative mortality and morbidity, faster recovery, reduced hospitalization time, improved cosmetics results, less rehabilitation resources and therefore reduced costs [1-3].
The most common MIAVR procedures are mini-sternotomy (MS) and mini-thoracotomy (MT), approaching the cardiac structures through the sternum or the intercostal spaces, respectively.
At the best of our knowledge, there are only few available studies directly comparing MS and MT. Therefore, the aim of this review was to compare the risks/benefits of MS and MT procedures in aortic valve replacement by summarizing the existing literature.
Materials and Methods
Literature Search Strategy
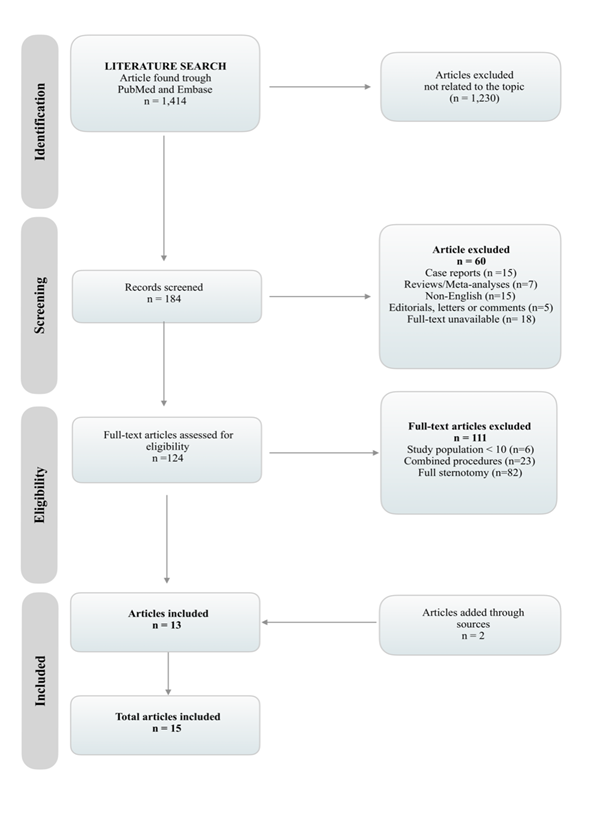
Literature search was in accordance to the principles of the Preferred Reporting Items for Systematic Review and Metanalyses (PRISMA) [4]. The search strategy was decided by two authors (L.M. and M.A.) and approved by another reviewer (M.D.J). Titles and abstracts of papers published between January 2000 and October 2017 were screened. Reference lists of the assessed articles were also reviewed for potentially relevant studies.
The literature search has been performed by one investigator. The search engines used were PubMed and Embase databases. The search strategy included the following search terms: “Mini Aortic Valve Replacement” OR “Mini-Sternotomy” OR “Mini-Thoracotomy”.
Selection criteria
The selection of articles was based on the following inclusion criteria: (1) studies published between 2000 and 2017, (2) studies with cohorts of more than 10 patients, (3) human studies, (4) studies in which patients underwent MIAVR via MS or MT. The following exclusion criteria were applied: (1) non-human studies, (2) case reports, (3) previous reviews and/or meta-analyses, (4) editorials, (5) studies consisting of less than 10 individuals, (6) non-English articles, (7) inaccessible papers.
Endpoints
Outcome measures were classified as either primary or secondary. The primary endpoint was 30-day mortality due to cardiac or non-cardiac reasons. While, secondary endpoints were major/permanent stroke, reoperations for bleeding, wound infections, cardiopulmonary bypass (CPB) duration and aortic cross clamp duration.
Results
Selection Criteria
Figure 1 outlines the study selection process. The initial number of studies found was 1,872. Since, 458 of them were duplicate, 1,414 articles were assessed systematically using the inclusion and exclusion criteria. The final data set consisted of 15 articles. All studies were retrospective [5-19] except for one study, which used prospective analysis [19] (Table 1). A total of 6,278 patients were analyzed: 3,197 patients were treated using MT as a procedural approach and 3,081 patients were treated using MS. Only two studies included less than 100 patients as their sample size [5, 17], and one study was carried out in two separate periods, one of these periods also included less than 100 patients as a sample size [18].
Four studies directly compared the outcomes of MT with MS [9, 12, 15, 16], three of which compared right anterior mini-thoracotomy (RAMT) vs. upper MS (UMS) (12, 15, 16], while one study analyzed anterolateral mini-thoracotomy (ALMT) vs. UMS [9]. On the other hand, 3 articles focused on the early and late clinical outcomes for patients who underwent MS [6, 7, 18], while 8 articles mostly focused on the perioperative clinical outcomes for patients who underwent MT [5, 8, 10, 11, 13, 14, 18, 19]. One study by Totsugawa et al. [5] compared ALMT to RAMT. The majority of patients (65%) included in the studies suffered from aortic stenosis (AS) [5, 7-19]. The follow-up period ranged between 3 months and 94 months, with a median of 30 months [8, 10, 12-15, 17, 19]. CPB duration was mentioned in all studies [5-19]. On the other hand, cross-clamp duration was mentioned in all studies except for one [6] (Table 2). Valve size was mentioned in 7 studies [5, 8, 11, 13-16]. Moreover, [10, 14, 15] 3 studies used sutureless techniques in their procedures [7,9,13] (Table 3).
Postoperative outcomes reported in the studies are summarized in Table 4. 30-day mortality was reported in all studies except for 4, which reported in-hospital mortality [6, 12, 19] and 90-day mortality [9] . Furthermore, stroke was reported in all studies except for two [6, 11], reoperation for bleeding was reported in all studies except for one [6], and wound infection was reported in all studies except for five [6, 9, 10, 12, 17].
|
Author |
Year |
Study Period |
Type of Study |
Sample Size |
MS/MT/Both |
Type of Mini Approach |
Follow-up |
|
Bethencourt et al. [18] |
2017 |
13 years |
R |
202 2003–2009: 65 2010–2015: 137 |
MT |
RA |
- |
|
Bouchard et al. [17] |
2000 |
3 years |
R |
51 |
MS |
Inverted T: 29 Inverted L: 22 |
16±9 months |
|
Fattouch et al. [16] |
2016 |
5 years |
R |
1130 MS: 854 MT: 276 |
Both |
RA MT J-shaped UMS |
- |
|
Gilmanov et al. [15] |
2015 |
12 years |
R/C |
853 MT: 592 MS: 261 |
Both |
RA MT UMS: V-shaped J or inverted T J-shaped |
29.1 months |
|
Glauber et al. [19] |
2011 |
5 years |
P |
192 |
MT |
RA |
24 months (12 – 41) |
|
Glauber et al. [14] |
2015 |
10 years |
R/C |
593 Isolated: 541 |
MT |
RA |
31 months (10-49) |
|
Glower et al. [13] |
2010 |
12 years |
R |
306 |
MT |
RA |
2.8±2.2 years |
|
Miceli et al. [12] |
2014 |
7 years |
R/C |
406 MT: 251 MS: 155 |
Both |
RA V-shaped UMS |
35 months (22 – 52) |
|
Plass et al. [11] |
2009 |
2 years |
R |
172 |
MT |
RA |
- |
|
Reser et al. [10] |
2017 |
7 years |
R |
225 |
MT |
RA |
69.65±24 months |
|
Semsroth et al. [9] |
2015 |
6 years |
R/C |
411 MT: 166 MS: 245 |
Both |
AL MT J-shaped UMS |
- |
|
Stolin?ski et al. [8] |
2016 |
4 years |
R |
194 |
MT |
RA |
3 months |
|
Tabata et al. [7] |
2008 |
10 years |
R |
1005 Isolated: 820 |
MS |
UMS |
- |
|
Totaro et al. [6] |
2009 |
11 years |
R |
1126 Isolated: 695 |
MS |
UMS: Reversed T Inverted L |
- |
|
Totsugawa et al. [5] |
2014 |
6 years |
R |
80 |
MT |
AL RA |
- |
Table 1: Characteristics of the studies
Articles are displayed in alphabetical order. Values are expressed as median [IQR], mean ± standard deviation or number of patients (%).R: Retrospective; P: Prospective; C: Cohort; MT= Mini-Thoracotomy; MS= Mini-Sternotomy; RA= Right Anterior; UMS= Upper Mini-Sternotomy; AL= Anterolateral.
|
Author |
Operation Duration (min) |
Cardiopulmonary Bypass Duration |
Cross Clamp Duration |
|
Bethencourt et al. [18] |
- |
2003-2009: 102.7±36.0 (67–149) 2010-2015: 92.5±33.3 (59–136) |
2003-2009: 84.6±28.1 (57–126) 2010-2015: 78.9 ± 28.2 (48–118) |
|
Bouchard et al. [17] |
- |
100±29 |
70±14 |
|
Fattouch et al. [16] |
- |
MS: 76.8±31.7 MT: 78.7±31.7 |
MS: 62.4±23.7 MT: 62.6±24.8 |
|
Gilmanov et al. [15] |
- |
108 (87-137) |
75 (57-97) |
|
Glauber et al. [19] |
- |
123±45 |
89±32 |
|
Glauber et al. [14] |
- |
107 (86-135) |
74 (55-96) |
|
Glower et al. [13] |
- |
158±35 |
103±26 |
|
Miceli et al. [12] |
- |
MT: 124.9±38.2 MS: 122.2±36.7 |
MT: 89.7±28.3 MS: 84.3±25.3 |
|
Plass et al. [11] |
- |
158±41 |
107±26 |
|
Reser et al. [10] |
4.4±1.2 (h) |
151±42 |
102±29 |
|
Semsroth et al. [9] |
- |
MT: 137 (77–456) MS: 113 (66–339) |
MT: 93 (43–231) MS: 75 (46–209) |
|
Stolin?ski et al. [8] |
199±29.9 |
117±23.1 |
77.6±11.3 |
|
Tabata et al. [7] |
- |
100 |
70 |
|
Totaro et al. [6] |
- |
Cumulative: 100±45 |
- |
|
Totsugawa et al. [5] |
RA: 247±47 AL: 264±31 |
RA: 137±32 AL: 155±23 |
RA: 93±22 AL: 105±15 |
Table 2: Surgical Procedures
Articles are displayed in alphabetical order. Values are expressed as median [IQR] or mean ± standard deviation. MT= Mini-Thoracotomy; MS= Mini-Sternotomy; RA= Right Anterior; UMS= Upper Mini-Sternotomy; AL= Anterolateral.
|
Author |
Valve Size (mm) (%) |
Valve Type (%) |
|
Bethencourt et al. [18] |
- |
- |
|
Bouchard et al. [17] |
- |
Mechanical: 33 Biological: 18 |
|
Fattouch et al. [16] |
MS: Median: 23 mm MT: Median: 23 mm |
Non-sutureless |
|
Gilmanov et al. [15] |
Median: 23 mm |
Biological: 443 (51.9) Sutureless: 368 (43.1) Mechanical: 42 (4.9) |
|
Glauber et al. [19] |
- |
Biological: 160 (83) Mechanical: 32 (17) |
|
Glauber et al. [14] |
Median: 25 mm |
Sutureless 302 (50.9) Mechanical 23 (3.9) Biological 268 (45.2) |
|
Glower et al. [13] |
Median: 23 mm |
Stented prostheses: 306 (100) Biological 240 (78) |
|
Miceli et al. [12] |
- |
- |
|
Plass et al. [11] |
Aortic valve annulus: 25 ± 2 |
Mechanical: 34 Biological: 126 |
|
Reser et al. [10] |
- |
Mechanical: 43 (19.1) Biological: 160 (71.0) Biological sutureless: 20 (8.8) |
|
Semsroth et al. [9] |
- |
- |
|
Stolin?ski et al. [8] |
Median: 23 mm |
Biological 155 (79.9) Mechanical: 39 (20.1) |
|
Tabata et al. [7] |
- |
Stented bioprosthetic/mechanical |
|
Totaro et al. [6] |
- |
- |
|
Totsugawa et al. [5] |
RA: 22.3 ± 1.9 AL: 20.6 ± 1.9 |
Bioprosthesis: RA: 34 (58) AL: 16 (76) |
Table 3: Valves
Articles are displayed in alphabetical order. Values are expressed mean ± standard deviation or number of patients (%). MT= Mini-Thoracotomy; MS= Mini-Sternotomy; RA= Right Anterior; UMS= Upper Mini-Sternotomy; AL= Anterolateral.
|
Author |
All-cause 30-day mortality |
Stroke (%) |
Reoperation for Bleeding |
Wound Infection |
|
Bethencourt et al. [18] |
2003-2009: 1 (1) 2010-2015: 3 (2) |
2003-2009: 4 (6) 2010-2015: 2 (1) |
2003-2009: 4 (6) 2010-2015: 4 (3) |
2003-2009: 0 2010-2015: 0 |
|
Bouchard et al. [17] |
2 (4) |
2 (4) |
2 (4) |
- |
|
Fattouch et al. [16] |
MS: 18 (3.3) MT: 3 (1.1) |
MS: 3 (0.4) MT: 0 |
MS: 30 (3.8) MT: 21 (8.0) |
MS: 18 (3.1) MT: 9 (3.3) |
|
Gilmanov et al. [15] |
16 (1.9) MT: 9 MS: 7 |
15 (1.8) |
37 (4.3) |
29 (3.4) |
|
Glauber et al. [19] |
In-hospital (4-6 days): 3 (1.6) |
1 (0.5) |
12 (6) |
0 |
|
Glauber et al. [14] |
9 (1.5) |
10 (1.7) |
30 (5.1) |
19 (3.2) |
|
Glower et al. [13] |
4 (1) |
5 (1.6) |
2 (1) |
3 (1) |
|
Miceli et al. [12] |
In-hospital (5-8 days): MT 3 (1.2) MS 2 (1.3) |
MT 3 (1.2) MS 2 (1.3) |
MT 12 (4.8) MS 5 (3.2) |
- |
|
Plass et al. [11] |
3 (1.9) |
- |
6 (3.8) |
0 |
|
Reser et al. [10] |
3 (1.3) |
0 |
13 (5.8) |
- |
|
Semsroth et al. [9] |
90 days mortality: MT 6 (3.8) MS 2 (1.3) |
MT: 1 (0.6) MS: 5 (2) |
MT: 20 (12) MS: 20 (8.2) |
- |
|
Stolin?ski et al. [8] |
3 (1.5) |
3 (1.5) |
7 (3.6) |
Superficial chest: 6 (3.1) Groin: 7 (3.6) |
|
Tabata et al. [7] |
17 (2.1) |
15/1005 (1.5) |
25/1005 (2.5) |
5/1005 (0.5) |
|
Totaro et al. [6] |
In-hospital (10±7 days): Isolated: 19 (2.8) |
- |
- |
- |
|
Totsugawa et al. [5] |
RA: 1.2 ± 1.0 AL: 1.8 ± 1.0 |
RA: 1 (1.7) AL: 0 |
RA: 2 (3.4) AL: 0 |
RA: 1 (1.7) AL: 0 |
Table 4: Postoperative Outcomes
Articles are displayed in alphabetical order. Values are expressed as median [IQR], mean ± standard deviation or number of patients (%). MT= Mini-Thoracotomy; MS= Mini-Sternotomy; RA= Right Anterior; UMS= Upper Mini-Sternotomy; AL= Anterolateral.
Primary Endpoint
Studies comparing MT and MS did not show any significant difference in 30-day mortality rates between the two interventions (p= 0.28) [15, 16]. The 30-day mortality rates ranged between 1 and 2% in the studies investigating MT [8, 10, 11, 13, 14, 18]. Moreover, Glauber et al. [19] investigated in-hospital mortality (4-6 days), registering an incidence of 1.6% of deaths. Miceli et al. [12] and Semsroth et al. [9] reported no significant difference in terms of in-hospital (5-8 days) mortality (p= 1) or 90-day mortality (p= 0.16) rates, respectively. According to Totsugawa et al. [5], there was no significant difference in 30-day mortality rates between RAMT and ALMT (1.7% vs. 0%, p=0.58). As regards of MS, Bouchard et al. [17] and Tabata et al. [7] reported 30-day mortality rates of 4% and 2.1%, respectively. In-hospital mortality (10±7 days) was reported to have a rate of 2.8% in the paper of Totaro et al. [6].
Secondary Endpoints
No significant difference was found in the studies comparing MT to MS in terms of stroke [9, 12, 16]. The incidence of stroke in the MT group ranged from 0 to 1.7% [8, 10, 13, 14, 19]. Particularly, no significant difference was found in stroke rates between RAMT and ALMT (p=0.58) [5]. In relation to MS, Bouchard et al. [17] reported an incidence of stroke of 4%.
For re-operations due to bleeding, the study by Fattouch et al. [16] reported a significant difference between MT and MS (8% vs. 3.8%, p=0.006). Conversely, Miceli et al. [12] found no significant differences in terms of reoperations for bleeding in their studies. Additionally, in Semsroth et al. [9], the proportion of patients receiving transfusion was significantly higher in the MT group, compared to the MS group. Across the studies focused on MT, reoperations due to bleeding ranged between 3.6 to 6% [8, 10, 11, 14, 19], with the exception of Glower et al. [13], who registered only 1% reoperations for bleeding. No significant difference was found between RAMT and ALMT (p= 0.97) in Totsugawa et al. [5]. Whereas, in the MS group, the rate of re-operation for bleeding was 4% [17].
Wound infection rates were not significantly different between MT and MS in the study by Fattouch et al. [16] (3.3% vs. 3.1%, p=0.29, respectively). Among the studies focused on MT, three studies reported 0% wound infection rates [4,8,12], while in other three studies wound infection ranged from 1 to 3.6% [8, 13, 14]. In particular, Stolin?ski et al. [8] also reported 3.1% superficial chest wound infections and 3.6% groin wound infections. No significant difference was found for wound infections between RA MT and AL MT (P=0.58) in Totsugawa et al. [5] study. In the MS group, the rate of wound infection was 0.5% [7].
Amongst the 3 studies that compared MT with MS [9, 12, 16], Semsroth et al. [9] indicated that the median CPB and cross-clamping durations were significantly longer in the ALMT group than in the UMS group (137 [77-456] min and 93 [43-231] min vs 113 [66-339] min and 75 [46-209] min, respectively; p<0.0001 and p<0.0001). Differently, the studies by Fattouch et al. [16] and Miceli et al. [12] showed no significant differences between MT and MS in terms of CPB and cross-clamping durations. Across the studies investigating MT, CPB time ranged from 117±23.1 to 158±41, while cross duration ranged from 77.6±11.3 to 107±26 [8, 10, 11, 13]. The study by Bethencourt et al. [18] showed a significant difference between the two study periods, 2003-2009 and 2010-2015, in term of CPB (102.7±36.0 vs. 92.5±33.3 min, p=0.049) duration, but not in terms of cross-clamping (84.6±28.1 vs. 78.9±28.2 min, p=0.2) duration. Moreover, Totsugawa et al. [5] study indicated that ALMT had significantly longer CPB (155±23 vs. 137±32 min, P=0.02) and cross-clamping durations (105±15 vs. 93±22 min, P=0.02) than RAMT.
As regards to the MS group, in Bouchard et al. [17], CPB and cross-clamping durations were 104±38 and 72±16 minutes, respectively. In Totaro et al. [6], CPB time was 100±45 minutes.
Discussion
Mini-sternotomy (MS) procedures are performed through a small 4-5/6-8 cm incision of the sternal notch to the second, third or fourth intercostal space, which allows access to the cardiac structures [1, 2]. Surgical MS can be executed via three accesses: upper (inverted T-shape, V-shape, J-shape), middle, and lower. While the upper and the lower approaches are the most used, the middle approach is rarely employed. Upper MS (UMS) is the most frequently adopted procedure, since it offers the flexibility of a patient- and surgeon-tailored approach, comparable to full sternotomy (FS). The lower MS (LMS) represents valid option because it enables the surgeon to have a satisfactory access to heart and great vessels, as well as providing benefits for the patient’s mobility and post-operative rehabilitation [3]. Mini-thoracotomy (MT) is performed through a small transverse incision of 5-8 cm in the second/third intercostal space, allowing access to cardiac structures [1, 2]. MT is a demanding surgical procedure, since it requires long-lasting and specialized training, but it offers excellent cosmetic results with no costal/sternal injury and with no mobility restrictions. However, because of the limited visualization of the aortic anatomy, a preliminary CT scan is usually required [3].
Current literature reports results comparing MS and MT, although it is controversial whether these the differences between the two techniques are significant. Therefore, in this review we have explored the risks/benefits of MS and mini-thoracotomy MT surgical procedures in aortic valve replacement, primarily investigating 30-day mortality rates. We have also aimed to highlight some of the major postoperative complications such as stroke and wound infections, bleeding as well as CPB and cross-clamping durations. By comparing both procedures, we aimed to increase awareness among surgeons when selecting the appropriate approach.
The major finding of our systematic review was the similarity is all-cause mortality rate in the post-operative 30 days between MS and MT. Our results are consistent with current literature, confirming the ability of both mini-invasive procedures to indiscriminately reduce post-operative mortality when compared to full sternotomy (FS) [2, 20]. Compared to FS, mini-invasive procedures have better outcomes in terms of mortality because both MS and MT equally reduce complications such as stroke and bleeding, representing a valid alternative for elderly patients [21]. Furthermore, mortality in right anterior mini-thoracotomy (RAMT) was not significantly increased when compared to anterolateral mini-thoracotomy (ALMT). Theoretically, RAMT procedures might be related to higher risks since it requires the internal thoracic artery to be sacrificed [5]. However, it has been proven that the usage of the internal thoracic artery is not related to higher in-hospital mortality, and it is actually associated with better medium and long-term survival [22].
As regards of post-operative complications, stroke, re-operation due to bleeding and wound infection occurred in equal proportion in MS and MT as well as in RAMT and ALMT. In comparative studies, stroke incidence resulted to be similar in both groups. This might be partly attributable to the fact that in many studies employing MT, central aortic cannulation was used to minimize the risk of having a stroke, and vascular/groin complications [4,8,10,12]. Furthermore, the incidence of re-operation due to bleeding was comparable in the two groups, with the exception of Fattouch et al. [16], who state the superiority of MS in terms of bleeding, when compared to MT. Fattouch et al. [16] justified such a result by explaining that the initial low familiarity of the surgeons towards the MT procedure might have influenced the results. Indeed, a higher rate of bleeding was observed in the initial phases of the study [16]. The importance of familiarize with the procedure to avoid complications is also described in current literature as determinant for the post-operative outcomes [23]. In relation to wound infection, despite the fact that MS requires the incision of the sternum and the rib bones, thus increasing the chance of developing infection the wound [2], in our review we did not find significant difference between the two techniques in terms of infective risk. In RAMT and ALMT, the occurrence of complications was similar. However, it needed to be acknowledge that RAMT can induce reduction of spirometry parameters postoperatively, thus indicating an impaired pulmonary function, especially in patients with pre-existing COPD [24].
In relation to surgical results, while some studies registered no significant difference between MT and MS in terms of cardiopulmonary bypass (CPB) and cross-clamping duration [12, 16], others reported increased operative times in either MS or MT [9]. From our analysis, it emerged that MS is correlated to shorter CPB time and cross-clamping duration when compared to MT. The reasons for longer MT durations might be due to the limited visualization of the aortic anatomy, the smaller operative field, the higher complexity of the MT approach, and the fact that MT has only been used by more centers over recent times [2, 3, 25]. The use of sutureless valve/fast deployment techniques has shown a significant decrease in operative times, resulting in better outcomes [1]. Glauber et al. [14] reported that the use of sutureless prostheses resulted in significantly shorter CPB (99 vs. 134 min, P<0.0005) and cross-clamping durations (64 vs. 97 min, P<0.0005) than in patients with sutured prostheses. Gilmanov et al. [15] also reported a reduction in CPB and cross-clamping durations due to the usage of sutureless or rapid deployment prostheses. Indeed, current literature reports satisfactory clinical and hemodynamic outcomes after using a sutureless bioprosthesis via MS [26].
Limitations
This review has several limitations that should be noted. Firstly, a meta-analysis was not carried out due to heterogeneity of the included studies such as different outcomes and experience variations of the centers/surgeons. Secondly, most studies were analyzed retrospectively. Finally, some of the studies data were missing, including operation times, 30-day mortality rates, and follow-up periods.
Conclusion
The results suggest that both MT and MS surgical procedures are safe, effective, and comparable. Even though CPB and cross-clamping durations were longer in the MT approach, it is possible to achieve favorable results increasing surgical experience. Moreover, the employment of sutureless valve techniques is able to decrease the operative times, and thus will result in better clinical and hemodynamic outcomes.
Conflict of the interest
The authors declare no conflicts of interest.
References
- Castrovinci S, Emmanuel S, Moscarelli M, Murana G, Caccamo G, Bertolino EC, et al. Minimally invasive aortic valve surgery. Journal of geriatric cardiology: JGC 13 (2016): 499.
- Phan K, Xie A, Tsai Y-C, Black D, Di Eusanio M, Yan TD. Ministernotomy or minithoracotomy for minimally invasive aortic valve replacement: a Bayesian network meta-analysis. Annals of cardiothoracic surgery 4 (2015): 3.
- Kaczmarczyk M, Szaianski P, Zembala M, Filipiak K, Karolak W, Wojarski J, et al. Minimally invasive aortic valve replacement–pros and cons of keyhole aortic surgery. Kardiochirurgia i torakochirurgia polska= Polish journal of cardio-thoracic surgery 12 (2015): 103.
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS medicine 6 (2009): e1000100.
- Totsugawa T, Kuinose M, Hiraoka A, Yoshitaka H, Tamura K, Sakaguchi T. Anterolateral approach for minimally invasive aortic valve replacement. General thoracic and cardiovascular surgery 62 (2014): 290-295.
- Totaro P, Carlini S, Pozzi M, Pagani F, Zattera G, D'Armini AM, et al. Minimally invasive approach for complex cardiac surgery procedures. The Annals of thoracic surgery 88 (2009): 462-467.
- Tabata M, Umakanthan R, Cohn LH, Bolman III RM, Shekar PS, Chen FY, et al. Early and late outcomes of 1000 minimally invasive aortic valve operations. European journal of cardio-thoracic surgery 33 (2008): 537-541.
- Stoli?ski J, Fijorek K, Plicner D, Grudzie? G, Kruszec P, Musia? R, et al. Perioperative outcomes of minimally invasive aortic valve replacement through right anterior minithoracotomy. The Thoracic and cardiovascular surgeon 64 (2016): 392-399.
- Semsroth S, Matteucci-Gothe R, Heinz A, Dal Capello T, Kilo J, Müller L, et al. Comparison of anterolateral minithoracotomy versus partial upper hemisternotomy in aortic valve replacement. The Annals of thoracic surgery 100 (2015): 868-873.
- Reser D, Walser R, van Hemelrijk M, Holubec T, Weber A, Plass A, et al. Long-term outcomes after minimally invasive aortic valve surgery through right anterior minithoracotomy. The Thoracic and cardiovascular surgeon 65 (2017): 191-197.
- Plass A, Scheffel H, Alkadhi H, Kaufmann P, Genoni M, Falk V, et al. Aortic valve replacement through a minimally invasive approach: preoperative planning, surgical technique, and outcome. The Annals of thoracic surgery 88 (2009): 1851-1856.
- Miceli A, Murzi M, Gilmanov D, Fugà R, Ferrarini M, Solinas M, et al. Minimally invasive aortic valve replacement using right minithoracotomy is associated with better outcomes than ministernotomy. The Journal of thoracic and cardiovascular surgery 148 (2014): 133-137.
- Glower DD, Lee T, Desai B. Aortic valve replacement through right minithoracotomy in 306 consecutive patients. Innovations 5 (2010): 326-330.
- Glauber M, Gilmanov D, Farneti PA, Kallushi E, Miceli A, Chiaramonti F, et al. Right anterior minithoracotomy for aortic valve replacement: 10-year experience of a single center. The Journal of thoracic and cardiovascular surgery 150 (2015): 548-556.
- Gilmanov D, Solinas M, Farneti PA, Cerillo AG, Kallushi E, Santarelli F, et al. Minimally invasive aortic valve replacement: 12-year single center experience. Annals of cardiothoracic surgery 4 (2015): 160.
- Fattouch K, Moscarelli M, Del Giglio M, Albertini A, Comoglio C, Coppola R, et al. Non-sutureless minimally invasive aortic valve replacement: mini-sternotomy versus mini-thoracotomy: a series of 1130 patients. Interactive cardiovascular and thoracic surgery 23 (2016): 253-258.
- Bouchard D, Perrault LP, Carrier M, Ménasché P, Bel A, Pelletier LC. Ministernotomy for aortic valve replacement: a study of the preliminary experience. Canadian Journal of Surgery 43 (2000): 39.
- Bethencourt DM, Le J, Rodriguez G, Kalayjian RW, Thomas GS. Minimally invasive aortic valve replacement via right anterior Minithoracotomy and central aortic cannulation: a 13-year experience. Innovations 12 (2017): 87-94.
- Glauber M, Miceli A, Bevilacqua S, Farneti PA. Minimally invasive aortic valve replacement via right anterior minithoracotomy: early outcomes and midterm follow-up. The Journal of thoracic and cardiovascular surgery 142 (2011): 1577.
- Olds A, Saadat S, Azzolini A, Dombrovskiy V, Odroniec K, Lemaire A, et al. Improved operative and recovery times with mini-thoracotomy aortic valve replacement. Journal of cardiothoracic surgery 14 (2019): 91.
- Lamelas J, Sarria A, Santana O, Pineda AM, Lamas GA. Outcomes of minimally invasive valve surgery versus median sternotomy in patients age 75 years or greater. The annals of thoracic surgery 91 (2011): 79-84.
- Karthik S, Srinivasan AK, Grayson AD, Jackson M, Mediratta NK. Left internal mammary artery to the left anterior descending artery: effect on morbidity and mortality and reasons for nonusage. Ann Thorac Surg 78 (2004): 142-148.
- Mikus E, Turci S, Calvi S, Ricci M, Dozza L, Del Giglio M. Aortic valve replacement through right minithoracotomy: is it really biologically minimally invasive? The Annals of thoracic surgery 99 (2015): 826-830.
- Stoli?ski J, Plicner D, Fijorek K, Grudzie? G, Kruszec P, Andres J, et al. Respiratory system function in patients after aortic valve replacement through right anterior minithoracotomy. The Thoracic and cardiovascular surgeon 65 (2017): 182-190.
- Del Giglio M, Mikus E, Nerla R, Micari A, Calvi S, Tripodi A, et al. Right anterior mini-thoracotomy vs. conventional sternotomy for aortic valve replacement: a propensity-matched comparison. Journal of thoracic disease 10 (2018): 1588-1595.
- Fischlein T, Pfeiffer S, Pollari F, Sirch J, Vogt F, Santarpino G. Sutureless valve implantation via mini J-sternotomy: a single center experience with 2 years mean follow-up. The Thoracic and cardiovascular surgeon 63 (2015): 467-471.