Metachronous Malingnancy, 27 Years After Teflon Cordal Injection
Article Information
Marco Bottazzoli MD1, Alessandra Marcantoni MD1, Lorena Picori MD2, Cesare Grandi MD1, Franca Chierichetti MD2, Davide Donner MD2
1Department of Otorhinolaryngology, S. Chiara Hospital, Trento (TN), Italy
2Department of Nuclear Medicine, S. Chiara Hospital, Trento (TN), Italy
*Corresponding Author: Dr. Marco Bottazzoli, Department of Otorhinolaryngology, S. Chiara Hospital, Largo Medaglie d’Oro, 38122, Trento, Italy
Received: 23 July 2019; Accepted: 13 August 2019; Published: 14 November 2019
Citation: Bottazzoli M, Marcantoni A, Picori L, Grandi C, Chierichetti F, Donner D. Metacronous Malingnancy, 27 Years After Teflon Cordal Injection Archives of Clinical and Medical Case Reports 3 (2019): 442-450.
View / Download Pdf Share at FacebookAbstract
We report a rare case of a patient known for a long-time history of iatrogenic VC paralysis, with unusual PET-CT findings. Due to a bilateral paragangliomas (PGLs), 27 years before the patient underwent a left jugulo-petrosectomy. After admission for contralateral sudden hearing loss, MRI and PET-CT scans were acquired. We tried to critically analyze the clinical relevance of multimodal imaging in an unusual condition of comorbities. Moreover, we suggested a physiopathological interpretation of collecting imagings and clinical otorhinolaryngological aspects. We could determine that high SUV in paralyzed left VC was related to a foreign-body reaction after laryngeal injection by polytetrafluoroethylene fluoropolymer resin (Teflon) performed 27 years before. Moreover, an asymptomatic pT1c mixed lung adenocarcinoma was serendipitously detected in the left lung. The SUVs of these two lesions were both compatible with neoplasms. A further possible lesion in the right lung highlighted by MRI was not confirmed by PET-CT imaging (MRI artifact). Although Teflon is no longer in use for laryngeal injection, clinicians should be aware of the potential misinterpretation laryngeal findings in patients with such a clinical history, even long time after the procedure.
Keywords
Teflon; Teflonoma; Laryngeal injection; PET-CT, False-positive; Oncology; Tumor
Teflon articles, Teflonoma articles, Laryngeal injection articles, PET-CT articles, False-positive articles, Oncology articles, Tumor articles
Teflon articles Teflon Research articles Teflon review articles Teflon PubMed articles Teflon PubMed Central articles Teflon 2023 articles Teflon 2024 articles Teflon Scopus articles Teflon impact factor journals Teflon Scopus journals Teflon PubMed journals Teflon medical journals Teflon free journals Teflon best journals Teflon top journals Teflon free medical journals Teflon famous journals Teflon Google Scholar indexed journals Teflon articles Teflon Research articles Teflon review articles Teflon PubMed articles Teflon PubMed Central articles Teflon 2023 articles Teflon 2024 articles Teflon Scopus articles Teflon impact factor journals Teflon Scopus journals Teflon PubMed journals Teflon medical journals Teflon free journals Teflon best journals Teflon top journals Teflon free medical journals Teflon famous journals Teflon Google Scholar indexed journals Laryngeal injection articles Laryngeal injection Research articles Laryngeal injection review articles Laryngeal injection PubMed articles Laryngeal injection PubMed Central articles Laryngeal injection 2023 articles Laryngeal injection 2024 articles Laryngeal injection Scopus articles Laryngeal injection impact factor journals Laryngeal injection Scopus journals Laryngeal injection PubMed journals Laryngeal injection medical journals Laryngeal injection free journals Laryngeal injection best journals Laryngeal injection top journals Laryngeal injection free medical journals Laryngeal injection famous journals Laryngeal injection Google Scholar indexed journals injection articles injection Research articles injection review articles injection PubMed articles injection PubMed Central articles injection 2023 articles injection 2024 articles injection Scopus articles injection impact factor journals injection Scopus journals injection PubMed journals injection medical journals injection free journals injection best journals injection top journals injection free medical journals injection famous journals injection Google Scholar indexed journals PET-CT articles PET-CT Research articles PET-CT review articles PET-CT PubMed articles PET-CT PubMed Central articles PET-CT 2023 articles PET-CT 2024 articles PET-CT Scopus articles PET-CT impact factor journals PET-CT Scopus journals PET-CT PubMed journals PET-CT medical journals PET-CT free journals PET-CT best journals PET-CT top journals PET-CT free medical journals PET-CT famous journals PET-CT Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals False-positive articles False-positive Research articles False-positive review articles False-positive PubMed articles False-positive PubMed Central articles False-positive 2023 articles False-positive 2024 articles False-positive Scopus articles False-positive impact factor journals False-positive Scopus journals False-positive PubMed journals False-positive medical journals False-positive free journals False-positive best journals False-positive top journals False-positive free medical journals False-positive famous journals False-positive Google Scholar indexed journals Congenital thrombophilia articles Congenital thrombophilia Research articles Congenital thrombophilia review articles Congenital thrombophilia PubMed articles Congenital thrombophilia PubMed Central articles Congenital thrombophilia 2023 articles Congenital thrombophilia 2024 articles Congenital thrombophilia Scopus articles Congenital thrombophilia impact factor journals Congenital thrombophilia Scopus journals Congenital thrombophilia PubMed journals Congenital thrombophilia medical journals Congenital thrombophilia free journals Congenital thrombophilia best journals Congenital thrombophilia top journals Congenital thrombophilia free medical journals Congenital thrombophilia famous journals Congenital thrombophilia Google Scholar indexed journals Oncology articles Oncology Research articles Oncology review articles Oncology PubMed articles Oncology PubMed Central articles Oncology 2023 articles Oncology 2024 articles Oncology Scopus articles Oncology impact factor journals Oncology Scopus journals Oncology PubMed journals Oncology medical journals Oncology free journals Oncology best journals Oncology top journals Oncology free medical journals Oncology famous journals Oncology Google Scholar indexed journals Tumor articles Tumor Research articles Tumor review articles Tumor PubMed articles Tumor PubMed Central articles Tumor 2023 articles Tumor 2024 articles Tumor Scopus articles Tumor impact factor journals Tumor Scopus journals Tumor PubMed journals Tumor medical journals Tumor free journals Tumor best journals Tumor top journals Tumor free medical journals Tumor famous journals Tumor Google Scholar indexed journals
Article Details
1. Introduction
Positron Emission Tomography (PET) has been increasingly used in the diagnostic investigation of patient with neoplasms, with more accuracy by fusing images with CT scan. On the other hand, a plaetora of benign and inflammatory lesions are more and more detected due to their increased 18-fluorodeoxyglucose (FDG) uptake and can be misinterpreted as malignancies. We present a case where PET showed an increased FDG uptake in an iatrogenic paralyzed vocal cord (VC), because of a left jugulo-petrosectomy performed decades before for a tympano-jugular paraganglioma (PGL): during the investigation, two serendipitously found pulmonary and laryngeal lesions suggested two sincronous malignant lesions. By subsequent analysis, we were able to determine that the high glycolityc activity was related to a foreign-body reaction after a laryngeal injection by polytetrafluoroethylene fluoropolymer resin (Teflon; Du Pont, Wilmington, Delaware, USA) performed 26 years before.
2. Matherials and Methods
A 70-year-old male, heavy smoker (50 pack/year) and former alcoholic, in September 2016 referred to our Department for a sudden right-sided hearing loss. The patient’s history was also relevant for being affected by familiar paraganglioma (PGL)-1-syndrome, a rare genetic disease that causes multiple PGLs. This syndrome is extremely common in a nearby area (Val dei Mocheni, Trento, Italy): in his family, also his mother as well as the patient’s 2 daughters carried the PGL-1-syndrome.
Due to multiple bilateral PGLs, the patient underwent in 1980 a left-sided radical jugulo-petrosectomy at another Institution, that caused a subsequent deficit of the left mixed nerves (8th to 12th), also consisting in complete left-sided hearing loss and left vocal cord (VC) palsy. Although a second, right-sided procedure was already scheduled for right PGL resection, it was called off in order to prevent a bilateral VC palsy. However, the patient voluntarily dropped off from follow-up for over 20 years, also because a major depressive syndrome as well as alcoholism.
To treat his recent sudden hearing loss, he underwent an effective steroid therapy that restored the hearing on the right side. As changings though time in size or extension of the right PGL could have caused the right sudden hearing loss, a head and neck MRI scan was also scheduled. No changing was detected, but an irregular swelling in left VC and a serendipitous, sincronous lesion of the right pulmonary apex, both suspicious for malignancies, were highlighted.
Therefore, the patient underwent a staging 18-fluorodeoxyglucose (18F-FDG) PET-CT which confirmed a suspicious lesion in the left VC, but also retrived a further one in the superior lobe of the left lung. Their standardized uptake values (SUVs) were 9.52 and 11.76, respectively (Fig 1). On the other hand, the lesion in the right superior lobe detected by MRI was no longer confirmed at the PET-CT. No pathologic nodes nor distant metastases were found.
A subsequent office-based flexible direct laryngoscopy confirmed the palsy of the left VC, with a typical loose appearance. Moreover, a swelling of the subglottic region on the left side was noted, with a small leucoplakia at its center (Figure 2). On narrow band imaging (Figure 2), vascular pattern of the mucosa above the swelling was normal, while the leucoplakia showed no vascular pattern at all, resembling a highly-keratinized lesion.
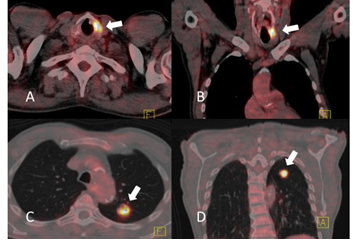
Figure 1: Axial (Figure 1A and 1C) and coronal (Figure 1B and 1D) PET-CT scans of the neck (Figure 1A and 1B) and the chest (Figure 1C and 1D) demonstrating (white arrows) two areas of pathologic FDG uptake respectively on neck and chest. The former (Figure 1A and 1B) has an SUV of 9.52 and is clearly localized within the left vocal cord. Note the absence of unilateral ossification of the left laryngeal cartilage. Similarly, the lesion in the left superior lobe (Figure 1C and D) has an SUV of 11.76. These PET-CT images are compatible either with two sincronous primitive tumors, a laryngeal metastasis from a lung tumor, or a lung metastasis from a laryngeal tumor.
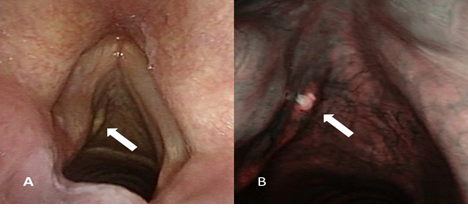
Figure 2: White light direct laryngoscopy (left photo) demonstrating the paralyzed left true VC with a normal mucosa, while a small submucosal mass (white arrow) is present within the left conus elasticus. Note the loose endocopic appearance of the paretic left VC. A slightly enlarged image using NBI (right photo) shows the normal mucosa overlying the swalling, with a consistently normal vascular pattern. On the other hand, the leucoplakia at the center of the swalling showes no vascular pattern at all, resembling a highly-keratinized lesion (white arrow).
CV: vocal cord, NBI: narrow band imaging.
The remaining head and neck examination was uneventfull. All these examinations were all initially consistent whit a possible submucosal VC malignancy.
3. Results
A direct laryngoscopy with biopsy under general anesthesia was scheduled, in order to confirm the diagnosis of malignancy. Final histopathologic report showed no evidence of neoplasm, but a marked inflammation with granulomatous reaction, including foreign-body giant cells and reactive fibrosis. The granulomatous reaction was induced by fragments of exogenous translucent material, so a diagnosis of foreign-body-induced Teflon granuloma (teflonoma) was made. Upon further interviews, the patient reportered that, few months after the jugulo-petrosectomy in 1980, he underwent a Teflon injection into the left paralyzed VC, to improve his voice quality. Initially, he experienced a good vocal result, followed by a gradual worsening of the dysphonia. Despite the deterioration, he did not express any concern on the quality of the voice, refusing any additional treatment. Furthermore, he referred of having forgotten about this procedure, due to its minimal morbidity.
In the following months, the patient also underwent an athipical resection of the superior lobe of the left lung, leading to a radical excision of the pulmonary neoplasm, subsequently defined as a pT1c pN0 cM0 mixed adenocarcinoma (papillary, micropapillary, acinic, and lepidic types). At the time of submission of the present paper, the patient was alive without evidence of disease for 35 months, while the remaining right PGL did not show any progression in the last 27 years.
4. Discussion
By identifying areas of augmented glucose uptake, PET can localize malignancies, metastatic lesions, and unknown primary tumors [1]. While PET-CT has a negative predictive value up to 100% [2] there is a multuplicity of conditions that physiologically increase SUV. Infectious, autoimmune, or granulomatous diseases as well as other benign lesions may have an increased FDG uptake. These areas of high uptake can be misinterpreted as a malignancy, due to the high glucose usage by activated granulocytes, lymphocytes, and macrophages.
An asymmetrical FDG uptake in VCs is a well-known feature in patients with unilateral VC paralysis: an increased[2] or even superphysiologic [3, 4] SUV is usually found in unparalyzed VC, theoretically caused by the overactivity of healthy laryngeal muscles that compensate the paralyzed VC. Physiological asymmetrical increased FDG uptake in VCs can be also caused by muscular activation during speech, entailing that the patient should refrain from talking during FDG administration and PET scanning [4].
An effective surgical procedure to correct a unilateral paralyzed VC is the medialization by injection of the paralyzed one, to improve vocal quality. This procedure was once performed by external puncture, while nowadays is done by endoscopy. To the best of our knowledge, the first report of cord medialization dates back to 1911, by Brunings, who used paraffin to successfully treat patients with VC paralisys [5]. However, paraffin was prone to dislocate itself and cause inflammation of the surrounding tissues, with a specific, foreign-body reaction defined as paraffinoma [5].
In the last century, a variety of materials were tested in the search of the ideal one to inject: it should be stable through time, atoxic, and without risk of extrusion or dislocation. Medializations were performed by: cartilage graft, bovine bone paste, tantalum powder, silicone, hydroxyapatite, Teflon, and autologous fat [6]. Only the latter proved not to cause a local inflammation, but its clinical effectiveness on vocal improvement may be unstable through time due to physiological reabsorption.
Use of Teflon was first described in 1962 by Arnold [7] and become mostly popular throughout the 1980s for laryngeal medialization after unilateral paralysis. Its use is also reported in microvascular decompression for hemifacial spasm [8], velopharyngeal augmentation [9], and even for urologic purposes, such as periurethral bulking for male incontinence [10-12]. Teflon was considered an ideal material because it was thought to be biologically stable and not be able to migrate, or cause significant postoperative modifications in tissue thickness. When the proper quantity of Teflon was injected in the correct site, the procedure proved to be effective in relieving dysphonya due to unilateral recurrent laryngeal nerve paralysis. In the short term after its use, few major clinical complications were described [13], although even significant cases of acute airway obstruction have be reported [13].
An inflammatory response to Teflon always occurs. Differently from what believed in the past [14], the phagocytosis of Teflon immediately evokes inflammation, that leads to a local giant-cells foreign-body reaction. Within 3 to 6 months, a collagenous capsule around Teflon can be demonstrated [6]. The granulomatous inflammatory response is known to persist through time, but its duration is still undetermined [15]; in a minority of cases, it can evolve in the socalled teflonoma. Duband et al believed that teflonomas could occour only in badly performed injections, due to overspill or wrong site and depth of injection [6]. However, badly performed injections should theoretically became symptomatic almost immediately, while teflonomas are usually developed after a variable time spawn characterized by an improved vocal quality, that suggests an evolution through the years. Moreover, they are tipically serendipitously detected. Initially, these granulomas are not always recognized both because of their slow progression and that their onset may be delayed for many years. Therefore, it is reasonable to hypothesize that granulomas should relate to Teflon progressive dislocation or to inflammatory overreaction, rather than badly performed injections.
Teflonomas usually occour at site of treatment, mostly in the subglottic region when considering laryngeal injections [16]. However, some papers report Teflon granulomas at distant sites: cervical lymphnodes after laryngeal injection in animals [17] as well as distant localizations (lung, brain, kiney, and spleen) after periurethral injections for urinary incontinence in animals [12] and in a single human case report [11]. Teflon granulomas are a known complication of a VC medialisation, eventually occurring in approximately 2-3% of patients [18]. When a teflonoma becames clinically significant, it usually cause a deterioration in the quality of the voice [19]. The tendency to induce granulomas, even long after a technically correct injection, was actually one of the major problem that led to abandon the use of Teflon, fostering the development of other, safer types of injectable materials, such as autologous fat.
A possible, not well known non-neoplastic cause of increased FDG uptake is a granulomatous reaction to previous cordal injections, included those performed with Teflon. According to the literature, Teflon-related PET-CT findings were reported after a period of time from the laryngeal injection that ranged from months [20] to almost 20 years [21]. Moreover, a single article demonstrated pathological SUVs in 2 cases of nasopharyngeal Teflon injection after 25 and 27 years respectively [9] clearly confutating the belief that inflammation is temporary [14]. The duration of Teflon-related FDG avidity is unknow [15]; therefore, it can be foreseen that the inflammatory response to Teflon injection can last indefinitely. 18F-FDG high uptake is also described after use of silicone elastomers [22, 23], with chronic foreign-body granulomatous reactions analogous to those caused by Teflon injections. However, silicone elastomers are believed to be related to less side effects [22]. Accordingly, only 2 cases of silicone-related foreign-body reactions were reported in the scientific literature, to the best of our knowledge.
Differently from Teflon and silicone elastomers, injection of calcium hydroxyapatite and/or methylcellulose proved that injected and non-injected cords had no statistical difference in SUVs [20]. Grant et al also demonstrated the absence of significant relation between SUV and time from injection as well as the extreme variability of SUVs in VCs, either treated or untreated [20]. However, beside the very short time spawn between injection and the PET-CT scan (range 0.1-8.0 months, median 3.2 months) [20], this paper seems to be hardly comparable to the case we report mainly because of the different injected materials.
Appearance at CT or MR imaging of laryngeal teflonomas is advocaded by some authors to be diriment [9, 15, 24]. In particular, it is expected to have a low-to-intermediate intensity on T2-weighted MRI scans [9, 24] while on CT imaging it should appear as not well defined, high-density, amorphpous material with high density [15, 24]. However, CT and MRI may be misleading, as sometimes long-lasting granulomas may no longer have a regular shape, but may resemble a malignancy by presenting as spiculated, possibly due to the fibroblastic reaction that leads to retracting scars. Moreover, SUVs of teflonomas can be extremely high (up to 15.0) [15] further mimicking a tumour.
Beside the rarity of the coexistance of unusual clinical conditions (PGL-1-syndrome, bilateral PGLs, sudden hearing loss, and serendipitous finding of pulmonary neoplasm), in the case we report, correct diagnosis was jeopardized by the fact that Teflon injection was not initially reported by the patient, as he considered it as a procedure of minor relevance. At the same time, gadolinium-enhanced MRI was not diriment, while such an intense SUV (9.52) was unexpected after 27 years without previous symptoms, including pain, dysphonia, dysphagia, or any other sign related to to the inflammatory process of the VC.
5. Conclusions
PET shows areas with increased glycolytic activity, with a variety of benign lesions that may produce high FDG uptake that may be misinterpreted as malignancies. It is therefore mandatory to critically interpretate SUVs: they quantify a metabolic process. VC medializations performed with laryngeal injection of eterologous substances produce an FDG-avid lesion which may show a high SUV. Among them, Teflon injection may have significant foreign-body granulomatous reaction, with long-lasting inflammation and fibrosis. Teflon granulomas should be considered in differential dignosis of patients with history of VC paralysis treated with injection laryngoplasty. Inflammatory reaction to Teflon can persist indefinitely and its clinical relevance may therefore be underestimate. Although Teflon is no longer in use for laryngeal injection, nuclear medicine physicians, radiologists, and head and neck surgeons should be aware of the potential misinterpretation laryngeal findings in patients with such a clinical history, even decades after the procedure.
Beyond literature evidences, our case highlights the arduous clinical assessment in a patient with uncommon sincronous pathologies (PGL-1-syndrome, bilateral PGLs, sudden hearing loss, and serendipitous finding of pulmonary tumor). Moreover, to the best of our knowledge, no other laryngeal teflonoma was ever reported after such a long spawn of time.
Acknowledgments
None of the authors have any potential conflicts of interest to disclose. No source of support and no founds were received for this paper.
References
- Prowse SJ, Shaw R, Ganeshan D, et al. The added value of 18F-fluorodeoxyglucose positron emission tomography computed tomography in patients with neck lymph node metastases from an unknown primary malignancy. J Laryngol Otol 127 (2013): 780-787.
- Thomassen A, Nielsen AL, Lauridsen JK, et al. FDG-PET/CT can rule out malignancy in patients with vocal cord palsy. Am J Nucl Med Mol Imaging 4 (2014): 193-201.
- Paquette CM, Manos DC, Psooy BJ. Unilateral vocal cord paralysis: a review of CT findings, mediastinal causes, and the course of the recurrent laryngeal nerves. Radiographics 32 (2012): 721-740.
- Lee M, Ramaswamy MR, Lilien DL, et al. Unilateral vocal cord paralysis causes contralateral false-positive positron emission tomography scans of the larynx. Ann Otol Rhinol Laryngol 114 (2005): 202-206.
- Brüning W. Uber eine neue Behandlungsmethode der Rekurrenslahmung. Verhandlungen des Vereins Deuischer Laryngologen 18 (1911): 93-151.
- Duband S, Govin A, Dumollard JM, et al. Laryngeal teflonoma identified by Fourier-transform infrared microspectroscopy after forensic autopsy: an interesting tool for foreign material identification in forensic cases. Forensic Sci Int 214 (2012): e26-e29.
- Arnold GE. Vocal rehabilitation of paralytic dysphonia. IX Technique of intracordal injection. Archives of Otolaryngology 76 (1962): 358-368.
- Megerian CA, Busaba NY, McKenna MJ, et al. Teflon granuloma presenting as an enlarging, gadolinium enhancing, posterior fossa mass with progressive hearing loss following microvascular decompression. Am J Otol 16 (1995): 783-786.
- Harrigal C, Branstetter BF 4th, Snyderman CH, Maroon J. Teflon granuloma in the nasopharynx: a potentially false-positive PET/CT finding. AJNR Am J Neuroradiol 26 (2005): 417-420.
- Chong JT, Simma-Chiang V. A historical perspective and evolution of the treatment of male urinary incontinence. Neurourol Urodyn 37 (2018): 1169-1175.
- Mittleman RE, Marraccini JV. Pulmonary Teflon granulomas following periurethral Teflon injection for urinary incontinence. Arch Pathol Lab Med 107 (1983): 611-612.
- Malizia AA Jr, Reiman HM, Myers RP, et al. Migration and granulomatous reaction after periurethral injection of polytef (Teflon). JAMA 251 (1984): 3277-3281.
- Solomons NB, Livesey JR. Acute upper airway obstruction following Teflon injection of a vocal cord; the value of nebulized adrenaline and a helium/oxygen mixture in its management. J Laryngol Otol 104 (1990): 654-655.
- McCarthy MP, Gideon JK, Schnadig VJ. A teflon granuloma presenting as an endotracheal nodule. Chest 104 (1993): 311-313.
- Truong MT, Erasmus JJ, Macapinlac HA, et al. Teflon injection for vocal cord paralysis: false-positive finding on FDG PET-CT in a patient with non-small cell lung cancer. AJR Am J Roentgenol 182 (2004): 1587-1589.
- Nakayama M, Ford CN, Bless DM. Teflon vocal fold augmentation: failures and management in 28 cases. Otolaryngol Head Neck Surg 109 (1993): 493-498.
- Ellis JC, McCaffrey TV, DeSanto LW, et al. Migration of Teflon after vocal cord injection. Otolaryngol Head Neck Surg 96 (1987): 63-66.
- Loehrl TA, Smith TL. Inflammatory and granulomatous lesions of the larynx and pharynx. Am J Med 111 (2001): 113S-117S.
- Varvares MA, Montgomery WW, Hillman RE. Teflon granuloma of the larynx: etiology, pathophysiology, and management. Ann Otol Rhinol Laryngol 104 (1995): 511-515.
- Grant N, Wong RJ, Kraus DH, et al. Positron-emission tomography enhancement after vocal fold injection medialization. Ear Nose Throat J 96 (2017): 218-224.
- Pagedar NA, Listinsky CM, Tucker HM. An unusual presentation of Teflon granuloma: case report and discussion. Ear Nose Throat J 88 (2009): 746-747.
- Mahfouz A, Naji M, Mok WY, et al. Silastic injection for vocal fold medialization resulting in a false-positive finding on F18 FDG-PET/CT. Ear Nose Throat J 94 (2015): 400-402.
- Tessonnier L, Fakhry N, Taïeb D, et al. False-positive finding on FDG-PET/CT after injectable elastomere implant (Vox implant) for vocal cord paralysis. Otolaryngol Head Neck Surg 139 (2008): 738-739.
- Ondik MP, Kang J, Bayerl MG, et al. Teflon laryngeal granuloma presenting as laryngeal cancer on combined positron emission tomography and computed tomography scanning. J Laryngol Otol 123 (2009): 575-578.
