Mental Health and Wellbeing of Late Childhood Children in Covid 19 Lockdown in Andhra Pradesh, India
Article Information
Anupama Korlakunta1*, Dharaneedhar2, Praveen Khairkar3, Sarada D4
1Assistant Professor, Department of Psychiatry, Gandhi Medical College and Hospital, Secunderabad, State of Telangana, India
2Postgraduate, Department of Psychiatry, Kamineni Institute of Medical Sciences, Narkatpalle, State of Telangana, India
3Professor, Department of Psychiatry, Kamineni Institute of Medical Sciences, Narkatpalle, State of Telangana, India
4Professor and Rector, Sri Padmavati Mahila Visvavidyalayam, Tirupati, Andhra Pradesh
*Corresponding Author: Dr. Anupama Korlakunta, Assistant Professor, Department of Psychiatry, Gandhi
Medical College and Hospital, Secunderabad, State of Telangana, India
Received: 22 January 2022; Accepted: 04 February 2022; Published: 04 March 2022
Citation:
Anupama Korlakunta, Dharaneedhar, Praveen Khairkar, Sarada D. Mental Health and Wellbeing of Late Childhood Children in Covid 19 Lockdown in Andhra Pradesh, India. Journal of Psychiatry and Psychiatric Disorders 6 (2022): 036-046.
View / Download Pdf Share at FacebookAbstract
Introduction: The impact lockdown on late childhood children may depend on several influencing factors such as the developmental tasks of the age, educational status, special needs, prevailing mental health condition, economical status of the family and family members being quarantined due to infection. These inexorable conditions may affect the mental health and various dimensions of behaviour of children in late childhood and early teens. With this background an attempt was made to study the mental health and wellbeing of late childhood children in COVID 19 lockdown.
Methods: The study was qualitative explorative research conducted in October 2020, using Snow ball method of sampling through online (Google form) questionnaire on mental health and wellbeing of late child hood age group during COVID 19 lockdown, which consisted of 35 items listed under seven mental health dimensions.
Results: Findings indicate that except for temperament, all the other six mental health dimensions were independent of the variable-age of the child as the p values were above the designated alpha value (0.05).
Discussion: The pandemic and efforts of governments to control its’ spread through stringent measures at all levels has created a situation, in which children have lost their precious period of time in home confinement, isolation, restricted movement, want of socialization, lack of academic and other pursuits. These circumstances affected the mental health of late childhood children and manifested in to mental health problems in seven dimensions as examined in this study.
Conclusions: The study allows to recommend appropriate mental health intervention programmes for school children to overcome mental health problems and adjust to the new normal situation in a healthy way.
Keywords
Mental health, Late childhood, School children, COVID19, Mental health dimensions
Mental health articles; Late childhood articles; School children articles; COVID-19 articles; Mental health dimensions articles
Mental health articles Mental health Research articles Mental health review articles Mental health PubMed articles Mental health PubMed Central articles Mental health 2023 articles Mental health 2024 articles Mental health Scopus articles Mental health impact factor journals Mental health Scopus journals Mental health PubMed journals Mental health medical journals Mental health free journals Mental health best journals Mental health top journals Mental health free medical journals Mental health famous journals Mental health Google Scholar indexed journals Late childhood articles Late childhood Research articles Late childhood review articles Late childhood PubMed articles Late childhood PubMed Central articles Late childhood 2023 articles Late childhood 2024 articles Late childhood Scopus articles Late childhood impact factor journals Late childhood Scopus journals Late childhood PubMed journals Late childhood medical journals Late childhood free journals Late childhood best journals Late childhood top journals Late childhood free medical journals Late childhood famous journals Late childhood Google Scholar indexed journals School children articles School children Research articles School children review articles School children PubMed articles School children PubMed Central articles School children 2023 articles School children 2024 articles School children Scopus articles School children impact factor journals School children Scopus journals School children PubMed journals School children medical journals School children free journals School children best journals School children top journals School children free medical journals School children famous journals School children Google Scholar indexed journals COVID19 articles COVID19 Research articles COVID19 review articles COVID19 PubMed articles COVID19 PubMed Central articles COVID19 2023 articles COVID19 2024 articles COVID19 Scopus articles COVID19 impact factor journals COVID19 Scopus journals COVID19 PubMed journals COVID19 medical journals COVID19 free journals COVID19 best journals COVID19 top journals COVID19 free medical journals COVID19 famous journals COVID19 Google Scholar indexed journals Mental health dimensions articles Mental health dimensions Research articles Mental health dimensions review articles Mental health dimensions PubMed articles Mental health dimensions PubMed Central articles Mental health dimensions 2023 articles Mental health dimensions 2024 articles Mental health dimensions Scopus articles Mental health dimensions impact factor journals Mental health dimensions Scopus journals Mental health dimensions PubMed journals Mental health dimensions medical journals Mental health dimensions free journals Mental health dimensions best journals Mental health dimensions top journals Mental health dimensions free medical journals Mental health dimensions famous journals Mental health dimensions Google Scholar indexed journals mental health articles mental health Research articles mental health review articles mental health PubMed articles mental health PubMed Central articles mental health 2023 articles mental health 2024 articles mental health Scopus articles mental health impact factor journals mental health Scopus journals mental health PubMed journals mental health medical journals mental health free journals mental health best journals mental health top journals mental health free medical journals mental health famous journals mental health Google Scholar indexed journals stress articles stress Research articles stress review articles stress PubMed articles stress PubMed Central articles stress 2023 articles stress 2024 articles stress Scopus articles stress impact factor journals stress Scopus journals stress PubMed journals stress medical journals stress free journals stress best journals stress top journals stress free medical journals stress famous journals stress Google Scholar indexed journals Behavioural Disturbance articles Behavioural Disturbance Research articles Behavioural Disturbance review articles Behavioural Disturbance PubMed articles Behavioural Disturbance PubMed Central articles Behavioural Disturbance 2023 articles Behavioural Disturbance 2024 articles Behavioural Disturbance Scopus articles Behavioural Disturbance impact factor journals Behavioural Disturbance Scopus journals Behavioural Disturbance PubMed journals Behavioural Disturbance medical journals Behavioural Disturbance free journals Behavioural Disturbance best journals Behavioural Disturbance top journals Behavioural Disturbance free medical journals Behavioural Disturbance famous journals Behavioural Disturbance Google Scholar indexed journals Psychiatric Disorders articles Psychiatric Disorders Research articles Psychiatric Disorders review articles Psychiatric Disorders PubMed articles Psychiatric Disorders PubMed Central articles Psychiatric Disorders 2023 articles Psychiatric Disorders 2024 articles Psychiatric Disorders Scopus articles Psychiatric Disorders impact factor journals Psychiatric Disorders Scopus journals Psychiatric Disorders PubMed journals Psychiatric Disorders medical journals Psychiatric Disorders free journals Psychiatric Disorders best journals Psychiatric Disorders top journals Psychiatric Disorders free medical journals Psychiatric Disorders famous journals Psychiatric Disorders Google Scholar indexed journals Positive Strength articles Positive Strength Research articles Positive Strength review articles Positive Strength PubMed articles Positive Strength PubMed Central articles Positive Strength 2023 articles Positive Strength 2024 articles Positive Strength Scopus articles Positive Strength impact factor journals Positive Strength Scopus journals Positive Strength PubMed journals Positive Strength medical journals Positive Strength free journals Positive Strength best journals Positive Strength top journals Positive Strength free medical journals Positive Strength famous journals Positive Strength Google Scholar indexed journals
Article Details
1. Background
Development in the brain during late childhood age enable not merely physical maturation, but also contributes to increased reasoning and flexibility in thinking. School assumes an important part of middle and late childhood, and it broadens their world beyond the ambit of their own family, peers play an important role influencing the parent-child relationship.
The children try hard to be accepted by their peers, which causes change their perception of self and may have consequences on emotional development beyond childhood [1].
The COVID-19 lock down has impacted the lives of children around the world in an unforeseen manner. Throughout the world, an essential plan of action for prevention from COVID- 19 pandemic has been self-isolation and social distancing to protect children and adults from the possible infection [2].
Since January, 2020, most of the countries began to impose partial or total lockdown phase wise, the major containment measures include; closure of schools, educational institutions, gyms, play grounds, entertainment and activity centres.
These unavoidable circumstances which are far away from normal experience, causes; stress, anxiety and a feeling of helplessness in most people. These circumstances developed by pandemic may have increased long term adverse effects on children and adolescents [2].
The impact lockdown on late childhood children may depend on several influencing factors such as the developmental tasks of the age, educational status, special needs, prevailing mental health condition, economical status of the family and family members being quarantined due to infection. COVID-19 related problems will affect mental health of children, with greater effect on those with pre-existing mental illness or those who belonged to families facing economic hardships [3, 4].
The Fegert et al., [5] recently indicated the impact of the phases of COVID19 on the mental health of children and adolescents. which include certain consequences and problems that children may have to face in the first phase of the pandemic: lack of access to the usual playgrounds, social group activities are restricted, closure of sports clubs, social relationships are limited to close relatives, physical contact with peers has been prohibited, school closures, online educational programmes with no real practical sessions, and loss of daily structure.
Furthermore, their families are confronted with multiple challenges such as; rescheduling daily life routine, coping with the COVID 19 measures, facing the stress of quarantine and social distancing challenges, meeting the demands of child care and online or offline home schooling, compromising with the space, freedom, privacy, and financial issues [6].
These inexorable conditions may affect the mental health and various dimensions of behaviour of children in late childhood and early teens. With this background an attempt was made to study the mental health and wellbeing of late childhood children in COVID 19 lockdown.
2. Methodology
The study was a qualitative explorative research conducted in October 2020, using Snow ball method of sampling through online (Google form) questionnaire and posted on whatsapp of parents of school going children (5th class to 9th class) with the help of school teachers in the state of Andhra Pradesh, who in turn posted the questionnaire link to other parents. Oral consent of the parents was included in the questionnaire as a first statement and their response as ‘yes’ was considered as their consent.
The questionnaire was developed to appraise the mental health and wellbeing of children as perceived by their parents. The number of statements and the seven dimensions of mental health examined were; Temperament (5items)), Behavioural Disturbance (7 items), Positive Strength (6 items), Attachment (3 items), Socialization (2 items), Coping Mechanism (5 items), Psychiatric Disorders (8 items).
The Google form questionnaire on mental health and wellbeing of late child hood age group during COVID 19 lockdown, consisted of 35 items listed under seven mental health dimensions.
Each family was asked to fill in only one online questionnaire on one child of theirs, who was in the age group of 9-14 years even if there were more than one child in that age group in their family.
The number of parents of 9 to 14 years aged children responded was 187 and 11 were excluded as they were invalid and remaining 186 were included as study sample and the data collected was subjected to statistical analysis using SPSS 21.0 version.
The research community were urged by scientists in the first phase of pandemic to rank the high-quality data on mental health problems and psychosocial impact of COVID-19 pandemic [7, 8].
3. Results
The authors of the present study made an attempt to examine the current pandemic effect on mental health of late childhood children as assessing the mental wellbeing of these children through enquiring directly may not be helpful in knowing the real picture .The data was analyzed to examine the relationship between the age and mental health and also the gender and mental health in seven dimensions.
Among the sample studied (N=186), 107 children were boys (57%) and 79 were girls (43%). Furthermore, the table1 depicts the levels (low, moderate and high) of mental health problems among children under study. The table 2 and figure 1, indicates that the mean scores of all the seven mental health dimensions which are nearer to their median values suggesting that they are at fifty percent of the scores.
In addition, the Standard deviation values of all the seven dimensions of mental health; temperament: 1.057, Behavioural Disturbance: 1.889, Positive Strength: 1.511, Attachment: 0.955, Socialization: 0.659, Coping Mechanism: 1.124, Psychiatric Disorders: 1.075, reveal that the perceived mental health problems by parents in their children did not vary much as the SD values were less than two.
The table 3 presents the relationship between the age and each of the seven mental health dimensions examined using chi-square test. The results showed that there was significant association found between the age of the child and temperament (0.006) at 0.05 alpha level.
In contrary, no significant association was between the age and; Behavioural Disturbance (p=0.929), Positive Strength (p=0.454), Attachment (p=0.519), Socialization (p=0.941), Coping Mechanism (p=0.651), Psychiatric Disorders (p=0.168).These findings indicate that except for temperament, all the other six mental health dimensions were independent of the variable- age of the child as the p values were above the designated alpha value (0.05).
Similarly, the table 4 demonstrates that there was no significant association found between the gender of the children and seven dimensions of their mental health as perceived by their parents, as the p-values were well above the assigned alpha value (0.05).
Thus, the results reflect that age and gender were not associated with most of the mental health dimensions understudy. The earlier research evidence showed that a significant effect on psychological dimensions of children during disasters [9], and data on psychosocial distress among children and adolescents reveals a hike in the COVID-19 pandemic compared to pre-pandemic baseline [3, 10].
|
S.NO |
Mental health dimensions |
Low (%) |
Moderate (%) |
High (%) |
Total (%) |
|
1 |
Temperament |
37.3 |
39.3 |
23.3 |
100.0 |
|
2 |
Behavioural Disturbance |
36.0 |
21.0 |
43.0 |
100.0 |
|
3 |
Positive Strength |
40.3 |
24.3 |
35.3 |
100.0 |
|
4 |
Attachment |
31.0 |
31.0 |
38.0 |
100.0 |
|
5 |
Socialization |
28.0 |
58.7 |
13.3 |
100.0 |
|
6 |
Coping Mechanism |
34.7 |
30.0 |
35.3 |
100.0 |
|
7 |
Psychiatric Disorders |
32.0 |
31.0 |
37.0 |
100.0 |
Table 1: Levels of mental health among 9–14-year-old children.
Table 2: The mean scores and SD of 9-14 year old children in seven dimensions of mental health.
|
Mental health dimensions |
Chi square value |
P value |
|
|
1 |
Temperament |
10.253a |
0.006 S |
|
2 |
Behavioural Disturbance |
0.008a |
0.929 NS |
|
3 |
Positive Strength |
0.560a |
0.454 NS |
|
4 |
Attachment |
0.415a |
0.519 NS |
|
5 |
Socialization |
0.005a |
0.941 NS |
|
6 |
Coping Mechanism |
0.205a |
0.651 NS |
|
7 |
Psychiatric Disorders |
1.905a |
0.168 NS |
- 0 cells (0.0%) have expected count less than 5
Table 3: Association between age and Mental health dimensions 9-14 years.
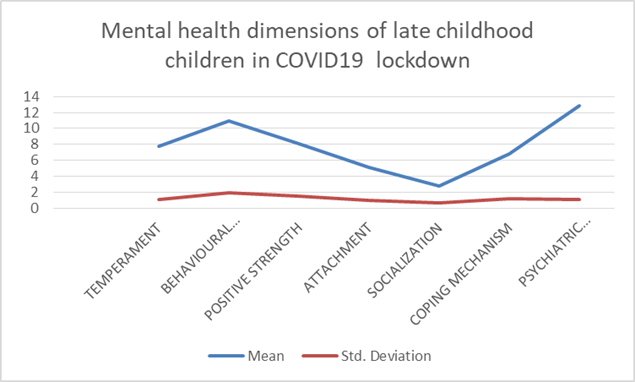
Figure 1: The mean and SD of mental health dimensions scores of children (9-14 years).
|
S. No |
Mental health dimensions |
Chi square value |
P value |
|
1 |
Temperament |
0.129a |
0.720 NS |
|
2 |
Behavioural Disturbance |
0.928a |
0.335 NS |
|
3 |
Positive Strength |
1.122a |
0.290 NS |
|
4 |
Attachment |
0.182a |
0.670 NS |
|
5 |
Socialization |
0.034a |
0.854 NS |
|
6 |
Coping Mechanism |
1.045a |
0.307 NS |
|
7 |
Psychiatric Disorders |
0.205a |
0.651 NS |
- 0 cells (0.0%) have expected count less than 5
Table 4: Association between gender and mental health dimensions 9-14 years.
4. Discussion
The COVID19 lockdown for more than nine months had an effect on normal life of a notable percent of families, making them take several measures to attend to the physical, financial, social and psychological needs of their family members.
This situation has forced the parents to follow disciplinary methods to make their children confine to the four walls of the home and compromise with their regular activities.
The children faced problems in adjustment to the new developments and increased psychosocial and behavioural problems such as; over or under eating, disturbed sleep, irritability, anxiety, distress, lack of attention, clinginess and fear of pandemic [11].
The current study results suggested that a notable percentage of the sample exhibited moderate to high levels of mental health problems in all the seven dimensions ; temperament, Behavioural Disturbance, Positive Strength, Attachment, Socialization, Coping Mechanism, Psychiatric Disorders during the lockdown period as shown in table 1.
This risk in families need attention, though the children and teenagers react in a resilient way to this pandemic situation [12].
Furthermore, children can experience fear of infection, frustration, boredom, lack of socialization with peers and lack of interaction with teachers and lack of space at home, contributes to worrisome consequences that may follow COVID19 pandemic period [13].
The table 2 displayed the means, SDs of all the seven mental health dimension scores based on the perceptions of parents of children , which reveals that children did not vary much in their mental health problems as the SD values were less than two.
For most of children, the acute distress symptoms developed during this pandemic period may not progress to a chronic stress response or an even more serious condition like acute stress disorder or post-traumatic stress disorder.
The resilience factors among children encompass; cognitive skills, empathy and a positive attitude. Results of early research in China indicate an increase in the children presented with symptoms of depression and anxiety during lockdown and home incarceration [14].
Similarly, in a study on general population in China showed that some preventive actions were associated with reporting symptoms of mental health issue [15]. Preventive efforts are the aim of public health interventions that promote knowledge, attitude, and practice (KAP) to improve various health outcomes among the people [16-18].
Resilience in children can be improved through healthy relationships in the family , family support, facilitation by the care givers, positive parenting methods, support from peers and others in the close circle, mentoring by teachers, less stressful academic engagement, community rapport and cultural linkages [19].
The table 3 presents the chi-square test values for age of the late childhood children and levels of mental health problems in seven mental health dimensions, which reveals that statistically significant relationship was found for temperament and age.
Whereas, for all the other six mental health dimensions were independent of the variable- age of the child as the p values were above the designated alpha value (0.05).
Studies showed that current chronic stressors which continue to affect the family may increase the risk of psychological problems and disorders [20, 21]. However, the ongoing economic and social effects of the COVID-19 pandemic like unemployment, continued school closures , lockdown measures ,other restrictions, and an increased chances of domestic violence may cause stress among children and families [22].
The findings in the table 4, connotes that there was no significant association found between the gender of school children and the seven dimensions of mental health problems perceived by their parents in the first phase of COVID19 indicating that there was no relationship between gender of children and mental health problem dimensions studied.
Upcoming evidence on the COVID-19 pandemic also indicates various other factors influencing the mental health and wellbeing of children and adolescents such as: stress and apprehension on their education, missing school, academic pressures (secondary school age),changes and adjustment to new situations, concern about their career and unpredictability about the future among young adults [23-25].
The COVID-19 pandemic is posing challenges to child development due to the chances of illness, protective home detention, social isolation, and the increased stress levels among parents and caregivers.
This conditions give rise to negative childhood experiences and may generate harmful stress, with possible losses for brain development, personal and collective health, and the long-term impairment of cognition, mental and physical health, and productivity as adults in future [26].
The pandemic and efforts of governments to control its’ spread through stringent measures at all levels has created a situation, in which children have lost their precious period of time in home confinement, isolation, restricted movement, want of socialization, lack of academic and other pursuits. These circumstances affected the mental health of late childhood children and manifested in to mental health problems in seven dimensions as examined in this study.
5. Conclusion
The late childhood being a transitional period from childhood to adolescence, the mental health of children in this group was affected by COVID19 lockdown as the levels of mental health problems were perceived by their parents as moderate to high among the sample.
Furthermore, the age and gender of these children was not associated with most of the dimensions of mental health problems of children.
The study allows to recommend appropriate mental health intervention programmes for school children to overcome mental health problems and adjust to the new normal situation in a healthy way.
References
- Lang D. Parenting and family diversity issues. Ames, IA: Iowa State University Digital Press (2020).
- Shen K, Yang Y, Wang T, et al. Global Pediatric Pulmonology Alliance. Diagnosis, Treatment, and Prevention of 2019 Novel Coronavirus Infection In Children: Experts’ Consensus Statement. World Journal of Pediatrics: (WJP) (2020): 1-9.
- Taquet M, Quoidbach J, Fried EI, et al. Mood homeostasis before and during the coronavirus disease 2019 (COVID-19) lockdown among students in the Netherlands. JAMA Psychiatry (2019; 2020): 2019-2021.
- Gassman-Pines A, Ananat EO, Fitz-Henley J. COVID-19 crisis impacts on parent and child psychological well-being. Pediatrics 4 (2020).
- Fegert JM, Vitiello B, Plener PL, et al. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc Psychiatry Ment Health 14 (2020): 20.
- Pizarro-Ruiz JP, Ordóñez-Camblor N. Effects of Covid-19 confinement on the mental health of children and adolescents in Spain. Sci Rep 11 (2021): 11713.
- Holmes EA, O'Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Psychiatry S2215-0366 (2020): 30168-1.
- JJV B, Baicker K, Boggio PS, et al. Using social and behavioural science to support COVID-19 pandemic response. Nat Hum Behav 4 (2020).
- Rolfsnes ES, Idsoe T. School-Based Intervention Programs for PTSD Symptoms: A Review and Meta-Analysis 20 (2007): 251-262.
- Duan L, Shao X, Wang Y, et al. An investigation of mental health status of children and adolescents in China during the outbreak of COVID-19. J Affect Disord 275 (2020): 112-118.
- Bakul J Parekh, Samir H Dalwai. Psychosocial Impact of COVID-19 Pandemic on Children in India. Indian Pediatr 57 (2020): 1107.
- Dvorsky MR, Breaux R, Becker SP. Finding ordinary magic in extraordinary times: Child and adolescent resilience during the COVID-19 pandemic. Eur. Child Adolesc. Psychiatry 1, 3 (2020).
- Cui Y, Li Y, Zheng Y. Mental health services for children in China during the COVID-19 pandemic: Results of an expert-based national survey among child and adolescent psychiatric hospitals. Eur. Child Adolesc. Psychiatry 29 (2020): 743-748.
- Xinyan X, Qi X, Yu Z, et al. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatr 7 (2020): 2-4.
- Shi L, Lu ZA, Que JY, et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw Open 7 (2020): e2014053.
- Werner PD. Implications of Attitude-Behavior Studies for Population Research and Action Author (s): Paul D. Werner Published by: Population Council Stable URL : https://www.jstor.org/stable/1966280 Implications of Attitude-Behavior Studies for Population Researc 8 (2020): 294-299.
- Ajzen I. Perceived behavioral control, self-efficacy, locus of control, and the theory of planned behavior. J Appl Soc Psychol 32 (2002): 665-683.
- Warwick D. The KAP Survey: dictates of Mission versus demands of science. London: Harvard Institute for International Development (1983).
- Gartland D, Riggs E, Muyeen S, et al. What factors are associated with resilient outcomes in children exposed to social adversity? A systematic review. BMJ Open 9 (2019): e024870.
- Shaw JA, Espinel Z, Shultz, JM. Children: Stress, trauma and disaster. Tampa, FL: Disaster Life Support Publishing (2007).
- Bahn GH. Coronavirus disease 2019, school closures and children’s mental health. J Korean Acad Child Adolesc Psychiatry 31 (2020): 74-79.
- Peterman A, Potts A, O’Donnell M, et al. Pandemics and violence against women and children. CGD Working Paper 528. Washington, DC: Center for Global Development (2020).
- Mental Health Foundation. Coronavirus: Mental Health in the Pandemic [Internet] (2020).
- Parliament SY, Scotland YL, Scot Y. LockdownLowdown - what young people in Scotland are thinking about COVID-19 [Internet] (2020).
- Waite P, Moltrecht B, Mcelroy E, et al. Report 02: Covid-19 worries, parent/carer stress and support needs, but child special educational needs and parent/carer work status. Oxford (2020).
- Araújo LA, Veloso CF, Souza MC, et al. The potential impact of the COVID-19 pandemic on child growth and development: a systematic review. J Pediatr (Rio J) (2020).
