Mediation by Executive Functions in the Associations Between Perceived Stress, Prenatal Distress, Emotional Control, and Dietary Intake in Overweight or Obese Pregnant Women
Article Information
Mei-Wei Chang1, Alai Tan1, Jonathan Schaffir2, Duane T. Wegener3, Brett Worly2, Katherine Strafford2, Cassandra Sampsell2, Kaleena Kemper2, Loriana Soma2, Maggie Rosen2, Amanthi Ranatunga1, Michelle Challa1
1College of Nursing, The Ohio State University, 1585 Neil Avenue, Columbus, OH 43210, USA
2Department of Obstetrics and Gynecology, The Ohio State University, 395 West 12th Avenue, 5th floor Columbus, OH 43210, USA
3Department of Psychology, The Ohio State University, 1835 Neil Avenue, Columbus, OH 43210, USA
*Corresponding Author: Mei-Wei Chang, Associate Professor, The Ohio State University College of Nursing, 1585 Neil Avenue, Columbus, OH 43210, USA
Received: 01 September 2022; Accepted: 03 October 2022; Published: 28 October 2022
Citation:
Mei-Wei Chang, Alai Tan, Jonathan Schaffir, Duane T. Wegener, Brett Worly, Katherine Strafford, Cassandra Sampsell, Kaleena Kemper, Loriana Soma, Maggie Rosen, Amanthi Ranatunga, Michelle Challa. Mediation by Executive Functions in the Associations Between Perceived Stress, Prenatal Distress, Emotional Control, and Dietary Intake in Overweight or Obese Pregnant Women. Journal of Pediatrics, Perinatology and Child Health 6 (2022): 466-474.
View / Download Pdf Share at FacebookAbstract
Background: The study explored potential mediation by executive functions (behavioral regulation index [BRI] and metacognition index [MI]) in association between perceived stress, prenatal distress, emotional control, and dietary intake (total calorie, total fat, added sugar, fruits, and vegetables).
Methods: 70 overweight or obese pregnant women completed validated online surveys and two 24-hour dietary recalls. Path analyses were performed.
Results: Increased perceived stress was associated with increased BRI both directly (p < 0.001) and indirectly through increased MI (perceived stress to MI: p < 0.001, MI to BRI: p < 0.001). Subsequently, increased BRI was associated with increased total fat intake (p = 0.01). Two-stage mediation was found in the association of prenatal distress with total fat intake. Increased prenatal distress was associated with increased MI (p < 0.001). Higher MI was associated with higher BRI (p < 0.001), and higher BRI was associated with increased total fat intake (p = 0.01).
Conclusions: Future intervention studies for overweight or obese pregnant women might focus on stress management to alleviate perceived stress and prenatal distress or on strategies to boost executive functions, each of which might ultimately help to reduce total fat intake.
Keywords
Executive functions, Dietary fat intake, Perceived stress, prenatal distress, Emotion control
Executive functions articles, Dietary fat intake articles, Perceived stress articles, prenatal distress articles, Emotion control articles
Article Details
Introduction
Maternal dietary intake during pregnancy plays a crucial role in prenatal development, a critical time for establishing health outcomes in offspring later in life [1, 2]. Higher maternal total fat intake during pregnancy is associated with impaired glucose tolerance and gestational diabetes in the mother [3], and higher waist circumference and body mass index (BMI) among male offspring at age 19-21 years [4]. Increased intake of added sugar has been identified as a strong predictor of gestational weight gain [4, 5]. Higher prenatal intake of fruits and vegetables is also associated with decreased risk for adverse maternal outcomes (such as gestational diabetes [6] and preeclampsia [7]) and birth and child outcomes (such as restriction of fetal and infant growth at age of 6 months [8, 9] and developmental delays in offspring aged 2 years [10]). Thus, promotion of healthy eating among pregnant women, especially those who are overweight or obese is imperative, because they are at risk for adverse maternal outcomes [11, 12] and tend to have high total fat but less fruit and vegetable intake [13, 14].
Executive functions, a set of higher order cognitive processes, enables goal-directed action, planning, behavior monitoring, inhibitory control, updating (applying information or strategies), and shifting (cognitive flexibility) to re-prioritize activities and plans [15]. Executive function deficits are more likely to occur in overweight or obese than normal weight women [16-19]. When investigating executive functions as a global concept, executive function deficits are associated with intake of high fat [20] and unhealthy foods [21]. When examining distinct components of executive functions, researchers have reported inverse associations between inhibitory control and higher saturated fat intake [22], increased energy intake [23], percent calories from fat [24, 25], snacking and food intake [26, 27]. Other aspects of executive functions have also been associated with eating behaviors. For example, high levels of task monitoring are positively associated with fruit and vegetable intake [22]; less cognitive flexibility is associated with unhealthy eating behaviors [28]. Executive functions have traditionally been identified as composing 2 broad categories: behavioral regulation and metacognition, both of which interact with each other [15]. Behavioral regulation is referred to as the ability to apply cognitive skills to behavior (inhibitory control, shifting, emotional control, and self-monitoring [29]) and is associated with success in dietary intake modification [30]. Metacognition involves cognitive knowledge (e.g., working memory) and regulation (e.g., planning, task monitoring [31]). The associations between dietary intake, behavior regulation, and metacognition remain under investigation.
Obese adults tend to have difficulties in emotional control [32-34], defined as the use of emotion regulation strategies, such as cognitive reappraisal (reappraisal, changing the way individuals think about potentially emotion-eliciting events) and expressive suppression (suppression, changing the way individuals behaviorally respond [e.g., facial expression] to emotional-eliciting events) [35]. Whereas individuals apply reappraisal to experience more positive emotions, individuals utilize suppression to express fewer facial expressions and positive and negative emotion [36]. Suppression is associated with intake of high fat and calorie foods [37]. Laboratory research has shown that reappraisal and suppression are associated with executive functions [38]. However, it is unclear whether these results reflect relations in a real-world setting.
High levels of perceived stress are highly prevalent in pregnant women [39, 40], partially due to pregnancy-related concerns (prenatal distress) such as fetal health and impending parenthood [41-43]. These can be exacerbated by women’s coexisting stress (e.g., due to their family role, job related stressors, or parenting older children). High levels of perceived stress can increase unhealthy dietary intake (increased intake of energy-dense foods that are high in fat and added sugar, leading to weight gain [44, 45]). Strong evidence has shown that high levels of perceived stress impair executive functions [46-49] and are associated with unhealthy eating behaviors in women [37, 39].
In summary, American overweight or obese pregnant women are likely to have poorer dietary intake, executive function deficits, challenges in emotional control, and higher levels of perceived stress and prenatal distress than healthy weight women. Although there are direct associations among dietary intake, executive functions, emotional control, and perceived stress including prenatal distress, the mechanisms impairing dietary intake in relation to those concepts remains unknown. Using baseline data of a randomized controlled lifestyle behavior intervention for overweight or obese pregnant women, we explored whether executive functions (behavior regulation and metacognition) might mediate the associations between dietary intake and emotional control, perceived stress, and prenatal distress. We hypothesized that decreased emotional control (less use of reappraisal and greater use of suppression), higher levels of perceived stress, and higher levels of prenatal distress would be associated with worse behavior regulation and metacognition. We further hypothesized that poor behavior regulation and metacognition would each be associated with increased caloric, fat, and added sugar intake as well as decreased fruit and vegetable intake.
Methods and Materials
Setting and Participants
Participants were recruited from 5 prenatal care clinics affiliated with The Ohio State University Wexner Medical Center through clinician referral. Inclusion criteria included ≤ 13 week-gestation with a singleton fetus as assessed by ultrasound, pre-pregnancy BMI of 25.0-45.0 kg/m2 (computed using self-reported height and weight), ability to read and speak English, age of 18-45 years, access to a working smart phone with unlimited text messaging, and receiving prenatal care in a collaborating clinic. Participants agreed to commit to the entire 20-week intervention. We excluded women with self-reported history of ≥ 3 miscarriages, multiple gestation, planned termination of the pregnancy, diagnosed hypertension and type 1 or 2 diabetes, history of or current diagnosis of an eating disorder, serious current physical disease (e.g., renal disease or cancer), past bariatric surgery, current or history of substance abuse in the past 6 months, current treatment for a serious psychological disorder (e.g., schizophrenia and bipolar disorder), or contraindications to walking.
Potential participants were screened over the phone using the study criteria. Qualified participants provided demographic information and received informed consent via email to review prior to attending the scheduled Zoom 1 meeting. During the scheduled meeting, the research assistants highlighted the key study requirements and answered questions. Then participants signed an electronic consent form via REDCap. After that, they learned how to complete an online survey via REDCap and 24 dietary recall and wear Actigraph accelerometer on the wrist, followed by scheduling a Zoom 2 meeting. Women who completed the baseline data collection attended the Zoom 2 meeting to be randomized to an intervention or usual care group (1: 1 ratio). In this paper, we focus on baseline online survey and dietary recall data. The study procedure was approved by the Ohio State University Institution Review Board.
Measures
Demographic characteristics: Women self-reported age, race/ethnicity, education, marital status, employment, and participation in government assistance program(s) (e.g., The special Supplemental Nutrition Program for Women, Infants, and Children, Medicaid).
Emotional control: We used the Emotion Regulation Questionnaire (10 items) with previously established validity and reliability to assess emotional control [50]. This survey assesses the emotional regulatory process using reappraisal (6 items) and suppression (4 items) [50]. There were 7 response categories, ranging from 1 = strongly disagree to 7 = strongly agree. We summed responses of all 6 reappraisal items to yield the final reappraisal composite score, ranging from 6 to 42. A higher score indicates the greater use of reappraisal to control negative emotion. After reversing the coding, we summed responses of all 4 suppression items to yield the final suppression composite score, ranging from 4 to 28. A higher score indicates less use of suppression to control negative emotion. Finally, we summed the final scores of reappraisal and suppression to create a total score ranging from 7 to 49. Higher scores mean better emotional control.
Perceived stress: We used the Perceived Stress Scale (10 items) that measures the degree to which situations in one’s life are appraised as stressful to assess perceived stress [51]. Participants were asked about their feelings and thoughts during the past month. There were 5 response categories, ranging from 0 = never to 4 = very often. We summed responses of all 10 items to yield the final composite score, ranging from 0 to 40. Higher scores indicate higher levels of perceived stress.
Prenatal distress: We used the validated Prenatal Distress Questionnaire (17 items) that measures prenatal stress, relating to pregnancy related symptoms [42, 52]. There were 3 response categories, ranging from 0 = not at all to 2 = very much. We averaged responses of all 17 items to yield the final composite score ranging from 0 to 2. Higher scores indicate higher levels of prenatal distress.
Executive functions: We used 75 items from the Behavior Rating Inventory of Executive Function-Adults to access executive functions [53]. This survey with previously established reliability and validity measures executive functions in the everyday environment using 8 components: inhibitory control, shifting, emotional control, self-monitoring, initiative, working memory, planning/organization, and task monitoring. There were 3 responses, ranging from 0 = never to 2 = often. We summed scores from 4 components with 30 items (inhibitory control, shifting, emotional control, and self-monitoring) to yield behavioral regulation index scores, ranging from 0 to 60. Higher scores mean worse behavioral regulation. We also summed scores from 4 components with 45 items (initiate, working memory, planning/organization, and task monitoring) to yield a metacognition index score, ranging from 0 to 90. Higher scores mean worse metacognition.
Dietary intake: We used National Institute of Cancer Automated Self-Administered 24-hour Dietary Recall (ASA 24) to collect dietary intake data. Participants completed two 24-hour dietary recalls. The variables of interest included calories, total fat, added sugar, fruit, and vegetable intakes.
Statistical Analysis
Descriptive statistics were used to summarize the sample demographics and study measures (emotion control, perceived stress, prenatal distress, executive functions, and dietary intake). To examine the potential role of executive functions in helping to explain the associations of emotional control, perceived stress, and prenatal distress with dietary intakes, we first calculated Pearson correlation coefficients and then followed these with mediation analyses. The Pearson correlation coefficients examined the associations of our hypothesized mediators (behavioral regulation and metacognition) with both the predictors (perceived stress and prenatal distress) and outcome variables (dietary intakes: total caloric, total fat, added sugar, fruit, and vegetable). Next, we conducted path analysis to examine potential mediation by the 2 executive function indices (behavior regulation and metacognition) in the path from perceived stress or prenatal distress to total fat intake. The predictors (perceived stress and prenatal distress) and outcomes (dietary fat intake) were chosen for the path analysis because they were significantly associated with behavioral regulation and metacognition in the Pearson correlation analysis. Due to the correlation between perceived stress and prenatal distress (r = 0.47), they were analyzed using separate path models. For each of the predictors (perceived stress and prenatal distress), we started with a full path model based on the hypothesis and Pearson correlation statistics, then derived a reduced final model by removing non-significant paths from the full model. Model fit was assessed using Chi-square statistics, the Comparative fit index (CFI), Tucker-Lewis index (TLI), and root mean squared error of approximation (RMSEA). We used MPlus7 for the path models and SAS 9.4 for all other statistical analysis.
Results
The mean age of the study participants (N =70) was 32.2 years (SD = 4.0). A majority were non-Hispanic White (77.1%), had a bachelor or higher degree (90.0%), were married (90.0%), and employed full-time (80.6%). Of 70 participants, 3 women (4.3%) reported receiving government financial assistance (Table 1).
|
Mean ± SD |
|
|
Age |
32.2 ± 4.0 |
|
N (%) |
|
|
Race |
|
|
Asian |
3 (4.3) |
|
Non-Hispanic Black |
10 (14.3) |
|
Non-Hispanic White |
54 (77.1) |
|
Non-Hispanic Multi-race |
3 (4.3) |
|
Education |
|
|
High school or GED graduated |
1 (1.4) |
|
Some college or technical school, no degree |
2 (2.9) |
|
Associate degree |
4 (5.7) |
|
Bachelor degree |
27 (38.6) |
|
Master degree |
23 (32.9) |
|
Professional degree |
11 (15.7) |
|
Doctoral degree |
2 (2.9) |
|
Marital Status |
|
|
Single/Never married |
6 (8.6) |
|
Married |
63 (90.0) |
|
In a domestic partnership |
1 (1.4) |
|
Employment |
|
|
Employed full-time |
56 (80.6) |
|
Employed part-time |
6 (8.6) |
|
Unemployed |
2 (2.9) |
|
Self-employed |
1 (1.4) |
|
Homemaker |
3 (4.3) |
|
Student |
2 (2.9) |
|
Receiving Government Financial Assistant Program |
|
|
Yes |
3 (4.3) |
|
No |
67 (95.7) |
Table 1: Sample Characteristics (N = 70).
Table 2 summarizes the potential predictors (emotional control, perceived stress, and prenatal distress), outcome measures (dietary intakes) and their associations with executive function indices of behavior regulation and metacognition. Among the predictors, perceived stress and prenatal distress were significantly associated with both behavior regulation and metacognition (r = 0.475 to 0.594, all p values < 0.001). Neither the emotional control subscales (reappraisal and suppression) nor total scales were associated with behavior regulation or metacognition. Among the outcome measures of dietary intake, only total dietary fat intake was significantly associated with behavioral regulation (r = 0.288, p = 0.016), but was not associated with metacognition (r = 0.050, p = 0.683). All other dietary intake (total calorie, added sugar, fruits, and vegetables) were not associated with behavior regulation or metacognition. As expected, behavioral regulation and metacognition were highly correlated (r = 0.707, p < 0.001).
|
Pearson Correlation Coefficient, r (p value) |
|||
|
Mean ± SD |
Executive Functions – Behavior Regulation Index |
Executive Functions – Metacognition Index |
|
|
Emotional Control |
|||
|
Reappraisal |
28.6 ± 5.3 |
-0.032 (p = 0.792) |
-0.003 (p = 0.980) |
|
Suppression |
19.8 ± 4.9 |
0.034 (p = 0.780) |
0.069 (p = 0.569) |
|
Total score |
48.5 ± 6.5 |
-0.000 (p = 0.998) |
0.050 (p = 0.683) |
|
Perceived Stress |
17.0 ± 5.2 |
0.594 (p < 0.001) |
0.500 (p < 0.001) |
|
Prenatal Distress |
0.7 ± 0.4 |
0.475 (p < 0.001) |
0.522 (p < 0.001) |
|
Executive Functions |
|||
|
Behavior regulation index |
47.5 ± 9.3 |
- |
0.707 (p < 0.001) |
|
Metacognition index |
55.0 ± 17.7 |
0.707 (p < 0.001) |
- |
|
Dietary Intake |
|||
|
Total calorie (Kcal) |
1964 ± 545.4 |
0.130 (p = 0.283) |
0.012 (p = 0.920) |
|
Total fat (grams) |
83.6 ± 28.7 |
0.288 (p = 0.016) |
0.139 (p = 0.252) |
|
Total fruit (cups) |
1.1 ± 0.8 |
-0.145 (p = 0.230) |
-0.187 (p = 0.122) |
|
Total vegetable (cups) |
1.9 ± 1.0 |
-0.018 (p = 0.880) |
0.004 (p = 0.973) |
|
Added sugar (grams) |
11.3 ± 9.4 |
-0.008 (p = 0.950) |
0.099 (p = 0.416) |
Note. Higher scores of reappraisal and suppression indicate greater use of reappraisal and less use of suppression to control negative emotion, respectively. The higher emotional control scores reflect better emotional control. The higher behavior regulation index scores mean the worse behavior regulation. The higher metacognition index scores indicate worse metacognition.
Table 2: Correlations of Executive Functions with Emotional Control, Perceived Stress, Prenatal Distress, and Dietary Intake (N = 70).
Figure 1 shows the path models for the mediation analyses involving executive functions (behavior regulation and metacognition) in the association between perceived stress and total fat intake. The full model (Figure 1A) suggested that there were no significant direct effects of perceived stress (standardized coefficient [β] = -0.12, SE = 0.14, p = 0.40) and metacognition (β = -0.11, SE = 0.16, p = 0.49) on total fat intake. Therefore, these paths were deleted to derive the final reduced model (Figure 1B). The final path model suggested 2 potential mediation pathways between perceived stress and total fat intake: (i) increased perceived stress scores were associated with higher behavioral regulation index scores (β = 0.32, SE = 0.09, p < 0.001), and higher behavioral regulation scores were associated with increased total fat intake (β = 0.29, SE = 0.11, p = 0.01); and ii) increased perceived stress scores were associated with higher metacognition index scores (β = 0.50, SE = 0.09, p <0.001). Subsequently higher metacognition index scores were associated with higher behavioral regulation index scores (β = 0.55, SE = 0.08, p <0.001) and then to increased total fat intake (β = 0.29, SE =0.11, p = 0.01). The reduced model fit very well with Chi-square statistic of 1.32 (p = 0.51), both CFI and TLI of 1.00, and RMSEA of 0.00.
Note. The higher perceived stress scores mean higher levels of perceived stress. The higher behavior regulation scores indicate worse behavior regulation. The higher metacognition scores refer to worse metacognition. The higher total fat intake scores mean higher total fat intake.
*p < 0.05, **p < 0.01 ***p < 0.001.
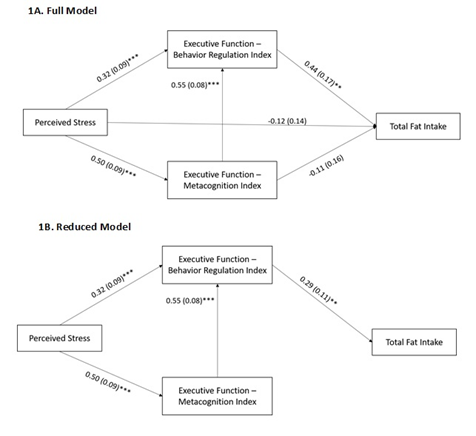
Figure 1: Mediation Analysis of Perceived Stress to Executive Functions to Total Fat Intake.
Figure 2 shows the path models for the mediation analyses involving behavioral regulation and metacognition in the association between prenatal distress and total fat intake. The full model (Figure 2A) suggested that there were no significant direct effects of prenatal distress (β = -0.19, SE = 0.13, p = 0.16) and metacognition (β =-0.06, SE = 0.17, p = 0.72) on total fat intake. There was also no significant direct effect of prenatal distress on behavioral regulation (β =0.15, SE = 0.10, p = 0.14). Therefore, these paths were deleted to derive the final reduced model (Figure 2B). The final path model suggested that increased prenatal distress was associated with worse metacognition (β = 0.52, SE = 0.09, p < 0.001). Subsequently, worse metacognition was associated with worse behavioral regulation (β = 0.71, SE = 0.06, p < 0.001), and worse behavioral regulation was then associated with increased total fat intake (β = 0.29, SE = 0.11, p = 0.01). The reduced model had acceptable fit with Chi-square statistic of 4.75 (p = 0.19), CFI of 0.977, and TLI of 0.954, whereas an RMSEA of 0.09 suggested a marginal fit.
Note. The higher prenatal distress scores mean higher levels of prenatal stress. The higher behavior regulation scores indicate worse behavior regulation. The higher metacognition scores refer to worse metacognition. The higher total fat intake scores mean higher total fat intake.
*p < 0.05, **p < 0.01 ***p < 0.001.
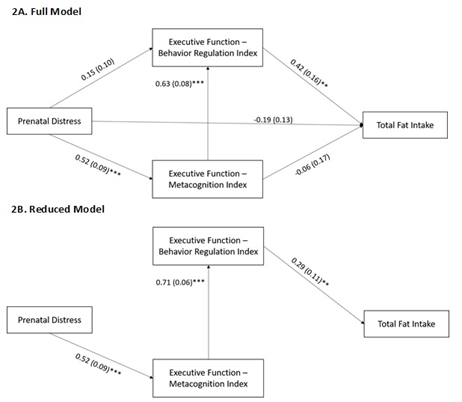
Figure 2: Mediation Analysis of Prenatal Distress to Executive Functions to Total Fat Intake.
Discussion
The present study goes beyond prior research focusing on investigating the direct associations between emotional control, perceived stress, prenatal distress, distinct components of executive functions, and dietary intake. We explored whether executive functions (behavior regulation and metacognition) might help to explain the associations between dietary intake, emotional control, perceived stress, and prenatal distress using mediation analyses. Results of this study partially supported our hypotheses (see discussion below).
Contradictory to our hypothesis, we did not find the mediation by executive functions in the association between emotional control and dietary intake. We also failed to detect associations between emotional control and dietary intake. The non-significant associations between emotional control and the executive functions (behavioral regulation and metacognition) were not supported by previous laboratory results [38]. This might have occurred because the prior research manipulated emotional control followed by using fMRI to measure executive functions in college students [38]. Our study was conducted in a real world setting and used self-reported executive functions. Also, our participants were pregnant and were enrolled during the COVID pandemic. Future research with a large sample size involving pregnant women in a natural setting is needed to further evaluate the associations between emotional control and executive functions, and the association between emotional control and dietary intake.
We found that behavior regulation potentially mediated the association between perceived stress and total fat intake, a finding consistent with our hypothesis. This means that higher levels of perceived stress were associated with worsening behavioral regulation, and that association might help to account for associations between perceived stress and total fat intake. We also found an association between perceived stress and metacognition (which is also associated with behavior regulation, leading to a potential sequential mediation). Higher levels of perceived stress were associated with worsened metacognition, and worsened metacognition was associated with worsened behavioral regulation, which was associated with increased total fat intake. Similarly, we found that higher levels of prenatal distress were negatively associated with metacognition, which potentially then related to total fat intake indirectly through worsened behavior regulation. This finding was generally supportive of our hypothesis, though we did not anticipate the sequential mediation per se, only a role for executive functions in helping to explain relations between stress or prenatal distress and dietary outcomes. Our findings suggest the importance of helping individuals promote metacognition, for example, increased knowledge about strategies for goal attainment, why and when to use a given strategy, and being aware of task performance) [54]. Also, it is crucial to include behavioral regulation, for example, how to resist temptation of high fat foods when available.
We did not find behavior regulation or metacognition to be associated with other dietary intake (total caloric, added sugars, fruit, and vegetable intakes), and neither perceived stress nor prenatal distress was associated with other dietary intakes. Future studies with a larger sample size should seek to validate the negative findings in overweight or obese pregnant women.
If replicated in future research, our positive findings described above might have important clinical and research implications. Literature has documented that increased total fat intake is associated with adverse maternal and child health outcomes [3, 4]. In the present study, overweight and obese pregnant women reported 38.1% and 12.7% of their diet from total and saturated fat (data not shown), respectively. To help overweight or obese pregnant women reduce total fat intake, researchers and community planners might consider including simple and practical strategies to boost executive functions (behavioral regulation and metacognition) in addition to providing stress management to relieve perceived stress and prenatal distress.
Limitations
This study has several study limitations. The sample size might have prevented us from detecting various associations among the variables of interest, especially for any associations that are relatively small. Thus, interpretation of our study findings warrants caution. Also, we used a survey to measure executive functions instead of objective measurements, such as fMRI and task-based assessments, for example, Wisconsin Card Sort Task, Go-No-Go, Trail-making. Our choice was made because the use of fMRI is not practical for studies conducted in a real word setting. Also, in past research, the task-based assessments were not sensitive enough to detect subtle changes in executive functions [55]. Moreover, it is unclear whether results of these task-based assessments can be translated to daily behavior [30]. The cross-sectional design precludes us from drawing a causal relationship. Finally, our participants comprised predominantly middle class non-Hispanic White pregnant women, which limits generalizability of our study findings to broader populations.
Conclusions
We did not find associations between emotional control and executive functions or dietary intake. However, we found that higher levels of perceived stress and prenatal distress were associated with worse behavior regulation and metacognition, and these relations might help to explain associations between stress or prenatal distress and increased total fat intake. Especially if these patterns are replicated in future research, dietary interventions aiming to reduce total fat intake in pregnant women might consider focusing on strategies boosting executive functions and stress management, reducing perceived stress and prenatal distress.
Acknowledgement
This research was funded by Eunice Kennedy Shriver National Institute of Child Health and Human Development. R21HD099380. The authors would like to thank the collaborating office managers for their assistance in distributing the study fliers: Amanda Mccune, Tammy Meade, Alison Novotny, Amanda Perkins, Emily Ruggiero, Danielle Skinner, Laura Tylor. We also thank the following clinicians referred their first trimester pregnant clients to the study: Drs Melissa Goist, Lisa Keder, Kara Malone, Rebecca Rudesill, and Midwife Rebecca Wagner.
Author contribution
Conceptualization: M. Chang, J. Schaffir, A. Tan, D.T. Wegener, B. Worly, K. Strafford, C. Sampsell, K. Kemper, L. Soma, M. Rosen. Methodology: M. Chang, J. Schaffir, A. Tan, D.T. Wegner. Validation: M. Chang, A. Tan. Formal analysis: A. Tan. Investigation. M. Chang, J. Schaffir, A. Tan, D.T. Wegner. Data curation: A Ranatunga, M. Challa. Writing-original draft preparation. M. Chang, A. Tan. Writing-Review & editing. M. Chang, A. J. Schaffir, Tan, D.T. Wegner, B. Worly, K. Strafford, C. Sampsell, K. Kemper, and L. Soma.
Conflicts of Interest
The authors declare no conflict of interest. The sponsor has no role in the design, execution, interpretation, or writing of the study.
References
- Barker DJ: The origins of the developmental origins theory. J Intern Med 261 (2007): 412-417.
- Chia AR, Chen LW, Lai JS, Wong CH, Neelakantan N, van Dam RM, Chong MF: Maternal Dietary Patterns and Birth Outcomes: A Systematic Review and Meta-Analysis. Adv Nutr 10 (2019): 685-695.
- Saldana TM, Siega-Riz AM, Adair LS: Effect of macronutrient intake on the development of glucose intolerance during pregnancy. Am J Clin Nutr 79 (2004): 479-486.
- Maslova E, Rytter D, Bech BH, Henriksen TB, Olsen SF, Halldorsson TI: Maternal intake of fat in pregnancy and offspring metabolic health - A prospective study with 20 years of follow-up. Clin Nutr 35 (2016): 475-483.
- Renault KM, Carlsen EM, Norgaard K, Nilas L, Pryds O, Secher NJ, Olsen SF, Halldorsson TI: Intake of Sweets, Snacks and Soft Drinks Predicts Weight Gain in Obese Pregnant Women: Detailed Analysis of the Results of a Randomised Controlled Trial. PLoS One 10 (2015): e0133041.
- Mirmiran P, Hosseinpour-Niazi S, Moghaddam-Banaem L, Lamyian M, Goshtasebi A, Azizi F: Inverse relation between fruit and vegetable intake and the risk of gestational diabetes mellitus. Int J Vitam Nutr Res 89 (2019): 37-44.
- Brantsaeter AL, Haugen M, Samuelsen SO, Torjusen H, Trogstad L, Alexander J, Magnus P, Meltzer HM: A dietary pattern characterized by high intake of vegetables, fruits, and vegetable oils is associated with reduced risk of preeclampsia in nulliparous pregnant Norwegian women. J Nutr 139 (2009): 1162-1168.
- Yonezawa Y, Obara T, Yamashita T, Sugawara J, Ishikuro M, Murakami K, Noda A, Ueno F, Suzuki S, Suganuma H et al: Fruit and vegetable consumption before and during pregnancy and birth weight of new-borns in Japan: the Tohoku medical megabank project birth and three-generation cohort study. Nutr J 19 (2020): 80.
- Jang W, Kim H, Lee BE, Chang N: Maternal fruit and vegetable or vitamin C consumption during pregnancy is associated with fetal growth and infant growth up to 6 months: results from the Korean Mothers and Children's Environmental Health (MOCEH) cohort study. Nutr J 17 (2018): 105.
- Yonezawa Y, Ueno F, Obara T, Yamashita T, Ishikuro M, Murakami K, Noda A, Onuma T, Sugawara J, Suzuki S et al: Fruit and vegetable consumption before and during pregnancy and developmental delays in offspring aged 2 years in Japan. Br J Nutr 127 (2022): 1250-1258.
- Hedderson MM, Gunderson EP, Ferrara A: Gestational weight gain and risk of gestational diabetes mellitus. Obstet Gynecol 115 (2010): 597-604.
- Ren M, Li H, Cai W, Niu X, Ji W, Zhang Z, Niu J, Zhou X, Li Y: Excessive gestational weight gain in accordance with the IOM criteria and the risk of hypertensive disorders of pregnancy: a meta-analysis. BMC Pregnancy Childbirth 18 (2018): 281.
- Lindsay KL, Heneghan C, McNulty B, Brennan L, McAuliffe FM: Lifestyle and dietary habits of an obese pregnant cohort. Matern Child Health J 19 (2015): 25-32.
- Siega-Riz AM, Bodnar LM, Savitz DA: What are pregnant women eating? Nutrient and food group differences by race. Am J Obstet Gynecol 186 (2002): 480-486.
- Diamond A: Executive functions. Annu Rev Psychol 64 (2013): 135-168.
- Emery RL, Levine MD: Questionnaire and behavioral task measures of impulsivity are differentially associated with body mass index: A comprehensive meta-analysis. Psychol Bull 143 (2017): 868-902.
- Yang Y, Shields GS, Guo C, Liu Y: Executive function performance in obesity and overweight individuals: A meta-analysis and review. Neurosci Biobehav Rev 84 (2018): 225-244.
- Wu M, Brockmeyer T, Hartmann M, Skunde M, Herzog W, Friederich HC: Set-shifting ability across the spectrum of eating disorders and in overweight and obesity: a systematic review and meta-analysis. Psychol Med 144 (2014): 3365-3385.
- Weller RE, Cook EW, 3rd, Avsar KB, Cox JE: Obese women show greater delay discounting than healthy-weight women. Appetite 51 (2008): 563-569.
- Hall PA: Executive control resources and frequency of fatty food consumption: findings from an age-stratified community sample. Health Psychol 31 (2012): 235-241.
- Appelhans BM, Thomas AS, Roisman GI, Booth-LaForce C, Bleil ME: Preexisting Executive Function Deficits and Change in Health Behaviors During the COVID-19 Pandemic. Int J Behav Med 28 (2021): 813-819.
- Allom V, Mullan B: Individual differences in executive function predict distinct eating behaviours. Appetite 80 (2014): 123-130.
- Appelhans BM, Waring ME, Schneider KL, Pagoto SL, DeBiasse MA, Whited MC, Lynch EB: Delay discounting and intake of ready-to-eat and away-from-home foods in overweight and obese women. Appetite 59 (2012): 576-584.
- Daniel TO, Stanton CM, Epstein LH: The future is now: comparing the effect of episodic future thinking on impulsivity in lean and obese individuals. Appetite 71 (2013): 120-125.
- O'Donnell S, Oluyomi Daniel T, LH E: Does goal relevant episodic future thinking amplify the effect on delay discounting? Conscious Cogn 51 (2017): 10-16.
- Dassen FC, Jansen A, Nederkoorn C, Houben K: Focus on the future: Episodic future thinking reduces discount rate and snacking. Appetite 96 (2016): 327-332.
- Vartanian LR, Chen WH, Reily NM, Castel AD: The parallel impact of episodic memory and episodic future thinking on food intake. Appetite 101 (2016): 31-36.
- Allom V, Mullan B, Smith E, Hay P, Raman J: Breaking bad habits by improving executive function in individuals with obesity. BMC Public Health 18 (2018): 505.
- Sektnan M, McClelland MM, Acock A, Morrison FJ: Relations between early family risk, children's behavioral regulation, and academic achievement. Early Child Res Q 25 (2010): 464-479.
- Gettens KM, Gorin AA: Executive function in weight loss and weight loss maintenance: a conceptual review and novel neuropsychological model of weight control. J Behav Med 40 (2017): 687-701.
- Lai ER, Beimers JN, Dolan B: Metacognition: A Literature Review Research Report. In: 2011; 2011.
- Brockmeyer T, Skunde M, Wu M, Bresslein E, Rudofsky G, Herzog W, Friederich HC: Difficulties in emotion regulation across the spectrum of eating disorders. Compr Psychiatry 55 (2014): 565-571.
- Kass AE, Wildes JE, Coccaro EF: Identification and regulation of emotions in adults of varying weight statuses. J Health Psychol 24 (2019): 941-952.
- Ruscitti C, Rufino K, Goodwin N, Wagner R: Difficulties in emotion regulation in patients with eating disorders. Borderline Personal Disord Emot Dysregul 3 (2016).
- Cutuli D: Cognitive reappraisal and expressive suppression strategies role in the emotion regulation: an overview on their modulatory effects and neural correlates. Front Syst Neurosci 8 (2014).
- Gross JJ: The emerging field of emotion regulation: An integrative review. Review of General Psychology 2 (1998): 271-299.
- Chang M, Nitzke S, Guilford E, Adair C, Hazard D: Motivators and barriers to healthful eating and physical activity among low-income overweight and obese mothers. J Am Diet Assoc 108 (2008): 1023-1028.
- Goldin PR, McRae K, Ramel W, Gross JJ: The neural bases of emotion regulation: reappraisal and suppression of negative emotion. Biol Psychiatry 63 (2008): 577-586.
- Chang M, Tan A, Schaffir J: Relationships between stress, demographics and dietary intake behaviours among low-income pregnant women with overweight or obesity. Public Health Nutrition 22 (2019): 1066-1074.
- Glasheen C, Colpe L, Hoffman V, Warren LK: Prevalence of serious psychological distress and mental health treatment in a national sample of pregnant and postpartum women. Matern Child Health J 19 (2015): 204-216.
- Guardino CM, Schetter CD: Coping during pregnancy: a systematic review and recommendations. Health Psychol Rev 8 (2014): 70-94.
- Lobel M, Cannella DL, Graham JE, DeVincent C, Schneider J, Meyer BA: Pregnancy-specific stress, prenatal health behaviors, and birth outcomes. Health Psychol 27 (2008): 604-615.
- Misra DP, O'Campo P, Strobino D: Testing a sociomedical model for preterm delivery. Paediatr Perinat Epidemiol 15 (2001): 110-122.
- Fields SA, Lange K, Ramos A, Thamotharan S, Rassu F: The relationship between stress and delay discounting: a meta-analytic review. Behav Pharmacol 25 (2014): 434-444.
- Araiza AM, Lobel M: Stress and eating: Definitions, findings, explanations, and implications. Social and Personality Psychology Compass (2018).
- Girotti M, Adler SM, Bulin SE, Fucich EA, Paredes D, Morilak DA: Prefrontal cortex executive processes affected by stress in health and disease. Prog Neuropsychopharmacol Biol Psychiatry 85 (2018): 161-179.
- Zelazo PD: Executive Function and Psychopathology: A Neurodevelopmental Perspective. Annu Rev Clin Psychol 16 (2020): 431-454.
- Gothe NP, Keswani RK, McAuley E: Yoga practice improves executive function by attenuating stress levels. Biol Psychol 121 (2016): 109-116.
- O'Neill J, Kamper-DeMarco K, Chen X, Orom H: Too stressed to self-regulate? Associations between stress, self-reported executive function, disinhibited eating, and BMI in women. Eat Behav 39 (2020): 101417.
- Gross JJ, John OP: Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J Pers Soc Psychol 85 (2003): 348-362.
- Cohen S, Kamarck T, Mermelstein R: A global measure of perceived stress. J Health Soc Behav 24 (1983): 385-396.
- Ibrahim SM, Lobel M: Conceptualization, measurement, and effects of pregnancy-specific stress: review of research using the original and revised Prenatal Distress Questionnaire. J Behav Med 43 (2020): 16-33.
- Rouel M, Raman J, Hay P, Smith E: Validation of the Behaviour Rating Inventory of Executive Function - Adult Version (BRIEF-A) in the obese with and without binge eating disorder. Eat Behav 23 (2016): 58-65.
- Lai ER: Metacognition: A literature Review. In. Academia; 41 (2011).
- Fitzpatrick S, Gilbert S, Serpell L: Systematic review: are overweight and obese individuals impaired on behavioural tasks of executive functioning? Neuropsychol Rev 23 (2013): 138-156.
