Management and Becoming of Chest Pain of Undetermined Origin After Leaving the Emergency Department
Article Information
Fatima BOURICHE1, Dr Aurelia RUF2, Dr Serge YVORRA1, Pr Pierre MICHELET2
1Service de Cardiologie, Centre Hospitalier de Martigues, France
2Service des Urgences, Centre Hospitalo-Universitaire de La Timone, France
*Corresponding author: Fatima BOURICHE, Service de Cardiologie, Centre Hospitalier de Martigues, France.
Received: 11 February 2023; Accepted: 20 February 2023; Published: 22 June 2023
Citation: Dr Fatima BOURICHE, Dr Aurelia RUF, Dr Serge YVORRA, Pr Pierre MICHELET. Management and becoming of chest pain of undetermined origin after leaving the emergency department. Cardiology and Cardiovascular Medicine. 7 (2023): 211-217.
View / Download Pdf Share at FacebookAbstract
Objectives: This retrospective work made it possible to determine the strategy of intra-hospital, extra- hospital management as well as the future of patients consulting emergency patients for chest pain.
Methods: We included 188 patients consulting the emergency and leaving with a diagnosis of chest pain of undetermined origin.
Results: We highlighted that 46.8% of these patients returned home without instructions and it was statistically significantly mostly women. 29.3% of our workforce have received a prescription for additional examinations, with a myocardial ischemia assessment to be performed in 55.8%. 73.1% of the patients were observing in the consultation of a city doctor, 70.5% of the examinations prescribed by the hospital were carried out. In total, the cardiovascular origin is not systematically advanced, as much by the hospital structure as by city doctors. Furthermore, 2.7% of patients have felt a major cardiovascular event only with type of acute coronary syndrome. These were exclusively men and statistically significantly men 50 to 75 years. In addition, 25% of the workforce had non-cardiovascular events major, and in this case it was statistically significantly predominantly women, a fortiori women aged 60 to 75 years. Thus, patients returning home with a symptom of chest pain of undetermined origin comprise two populations at risk, men 50 to 75 years of age for major cardiovascular events such as acute coronary syndrome and women 60 to 75 years for non-major cardiovascular events.
Conclusion: It seems to emerge from our work that 2 populations are particularly to be monitored and that they could justify better coded exit instructions. In any case, these data are to be confirmed by other superior power and methodology studies.
Keywords
Chest Pain; Emergency Department
Article Details
Introduction
Chest pain is a common reason for consultation in emergency units, oscillating between 5 and 20% in France[1]with 40% of chest pain without accurate diagnosis[1]. There are many causes of chest pain, cardiac and extra- cardiac, but also of varying severity[3]. The cardiovascular causes account for about 25% of chest pain etiologies[3]. Thus,a leading doctor emergency challenges lies in the ability to diagnose the good etiology to support the patient in the most optimal way possible clinical, therapeutic and safe[4]. In literature,about half of patients visiting the emergency units for chest pain returns home after a clinical examination unremarkable, reassuring cardiological investigations and in the absence of elements moving towards a non- cardiovascular causes of chest pain[3,5]. However, we find in the literature that the management of these patients is not well defined and left to the discretion of the emergency physician and/or general practioner[3,6]. In addition,there is little data on the impact of liberal medical monitoring on the outcome of these patients[7]. Furthermore, the fate of patients with chest pain of non-specific origin is controversial:some studies[8] showed that there are low rates of mortality and heart disease, while others provide items a higher risk of mortality subsequent cardiac both short term and medium and/or long term[2,6,9]. The main objective of our study was to determine the treatment strategy implemented at the output of the emergencies by the hospital team for patients who presented a chest pain of undetermined origin. Our secondary objectives were to analyze the post hospital care strategy implemented by community practitioners and determine the outcome of these patients by assessing the prevalence of cardiovascular events in six months after the passage at the emergency for chest pain.
Material and Method
This is a retrospective monocentric observational study conducted between January 1, 2018 and June 30, 2018.
Inclusion criteria:
Patients consulting the emergency reception service of the Martigues Hospital Center for a reason of transient chest pain, aged at least 18, with a normal or considered non- pathological electrocardiogram of acute coronary artery disease or disease responsible for chest pain, with a negative troponin bioassay(if the pain had been prolonged by at least 30 minutes and was more than 3 hours old)or with an insignificant troponin cycle (i.e. an elevation less than 30% from the initial value)and returning home with a diagnosis of chest pain of undetermined origin.
Exclusion criteria:
Patients whose ECG was considered pathological, whose troponin cycle was significant, under 18 years of age, whose diagnosis of discharge from the emergency department was other than "chest pain of undetermined origin".
The patients were selected from the “Terminal Urgences” software with the reason for entering “chest pain”. Patients whose exit from the emergency diagnosis was “chest pain of undetermined origin” were retained. The epidemiological data from Emergency visits were collected retrospectively on the computerized patient record. Telephone calls were made to patients entering the study criteria to assess their outpatient follow-up using a standardized questionnaire. They were considered lost to follow-up patients who cannot be reached after 5 telephone calls or whose phone number has not been assigned. Regarding the main objective, was considered as a strategy of intra-hospital management by the emergency team the request for a cardiological opinion and/or the realization of a transthoracic ultrasound. Was considered as discharge order the prescription of additional examinations in external and/or the referral to a city doctor, cardiologist or general practitioner.
For secondary objectives, any mention or realization of an external consultation with a general practitioner or a cardiologist was considered as a strategy for taking care of at the exit of the Emergency Department as well as paraclinical cardiological examination. Regarding the management strategy, it was recorded by standardized questionnaire directly with patients six months after their passage to the emergency department.
Based on the literature[5,10], major cardiovascular events have been considered as the occurrence of death from cardiovascular cause, acute coronary syndrome or cerebrovascular accident. Any other cardiovascular event has been transcribed as a non-major cardiovascular event.
Excel and Sphinx software were used fo statistical tests. Categorical variables were expressed as proportions or percentages and compared with the χ². A p value<0.05 was considered to show statistical significance.
Results
585 patients entered the emergency department for chest pain. 338 patients were excluded because their final diagnosis was different from "chest pain of undetermined origin". 247 patients were contacted by phone(42.2% of the initial workforce): 59 patients never answered our calls and 188 patients agreed to complete our questionnaire, representing a response rate of 76%. The average age of the 188 patients was 50.3 years[±17.9].
The study population had a slight male prevalence(55.3%). 41% of patients had no medical history. 18.1% of patients described typical chest pain. The ECG was abnormal in 29.8%. Troponin was performed in 97.9% of patients and was negative in 52.2% of patients or with a non-significant cycle in 47.8%(Table 1).
|
VARIABLES |
% |
|
|
GENDER |
||
|
Men |
55.3% |
|
|
Women |
44.7% |
|
|
AGE |
||
|
18-39 |
33.4% |
|
|
40-59 |
34.7% |
|
|
EPIDEMIOLOGICAL |
60-74 |
21.8% |
|
CHARACTERISTICS |
>75 |
10.1% |
|
SUBGROUPS |
||
|
Women |
||
|
< 60 years |
30.9% |
|
|
>75 years |
4.8% |
|
|
Men |
||
|
<50 years |
27.1% |
|
|
>75 years |
5.3% |
|
|
None |
41% |
|
|
Other |
18.1% |
|
|
Coronary artery disease |
13.8% |
|
|
Arrythmia |
10.6% |
|
|
BACKGROUND |
Chronic lung disease |
9% |
|
Pericarditis |
2.1% |
|
|
Conduction disorder |
1.6% |
|
|
Pulmonary embolism |
1.6% |
|
|
Heart Failure |
1.1% |
|
|
Myocarditis |
1.1% |
|
|
Active smoking |
32.4% |
|
|
None |
32.4% |
|
|
High blood pressure |
31.9% |
|
|
Dyslipidemia |
18.6% |
|
|
CARDIOVASCULAR RISK |
Diabetes |
12.2% |
|
FACTORS |
Male inheritance |
7.4% |
|
Smoking cessation |
5.9% |
|
|
Overweight |
4.3% |
|
|
Obesity |
4.3% |
|
|
Female inheritance |
1.1% |
|
|
CHEST PAIN |
||
|
Typical |
18.1% |
|
|
CLINICAL AND |
Atypical |
81.9% |
|
PARACLINICAL |
ECG |
|
|
CHARACTERISTICS |
Absence of anomaly |
70.2% |
|
Repolarisation disorder |
14.9% |
|
|
Conduction disorder |
11.7% |
|
|
Arrythmia |
7.4% |
|
|
Left ventricular enlargement |
1.1% |
|
|
TROPONINE |
||
|
Negative |
52.2% |
|
|
Insignificant cycle |
47.8% |
Table 1: Characteristics of the study population
Primary objective
A cardiological opinion clearly specified in the file was requested for 28.7% of patients. Cardiological advice was given on site in the emergency department in 72.2% of cases and by phone in 27.8%. There was no statistically significant difference based on the sex and/or age of the patients. Transthoracic ultrasound was performed in 12.8%. 46.8% of the patients returned home without any specific follow-up instructions. The average age of these patients was 48.1 years ([±18.7]) and 10.2% of them were over 75.
Statistically significantly, more women(52.3%) left home without instructions(p<0.05). The women had an average age of 48.4 years([±19.8]), it was 47.9 years([±17.8]) for men. There was no statistically significant difference correlated with the age of the patients. 35.3% of patients were discharged from emergencies with the instruction to consult a doctor in town(general practitioner and/or cardiologist). The average age was 52.7 years([±17.1]). 38.8% were women whose average age was 51.2 years([±17.2]), 53.6 years([±17.1]) for men. We did not find a statistically significant difference according to the sex and/or the age of the patients. 29.3% of patients left the emergency department with the instruction to carry out at least one additional examination in town. The average age of these patients was 50.2 years([±15.8]). Of these,34.6% were women whose average age was 49.6 years([±17.2]), 50.4 years([±15.2])for men. There was no statistically significant difference based on the sex and/or age of the patients.
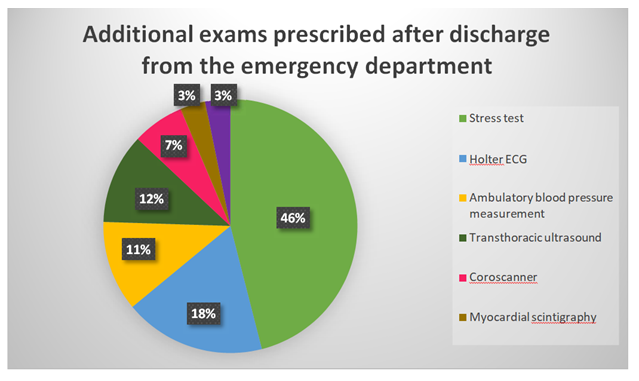
Among the patients who received the prescription for at least one additional examination, 46% received a stress test prescription, the other exams are shown in Figure 1.
Secondary objectives
In total, 35.6% of the patients consulted their general practitioner within six months and 47.9% a cardiologist. 13 patients consulted both. 16.5% had no follow-up after their passage to the emergency department. Among the patients who consulted their general practitioner, 46.3% received an etiological diagnosis:for 26.9% the general practitioner established a diagnosis of somatoform disorder, for 14.9% a parietal origin and for 4.5% gastritis. 29.8% of patients were referred for specialist consultation:16.4% for cardiology consultation, 10.4% for gastroenterology consultation, 1.5% for pulmonology consultation and 1.5% for endocrinology consultation. 6% of patients received a prescription for additional examination with the aim of performing an exercise test for 1.5%, for 1.5% an ambulatory blood pressure measurement, for 1.5% a thyroid assessment and for 1.5% a chest scanner.
For patients who consulted a cardiologist, 40% had a transthoracic ultrasound and 34.4% had an electrocardiogram. As part of the myocardial ischemia assessment, 35.6% of patients had to perform an exercise test, 8.9% a coroscanner, 5.6% a coronary angiography and 4.4% a myocardial scintigraphy. The hypertensive origin was mentioned for 11.1% of patients who received a prescription for an ambulatory blood pressure measurement and 4.4% benefited from an introduction or an adaptation of their antihypertensive treatment. Regarding the management of heart rhythm disorders, 10% of patients received a prescription for an ECG Holter, 3.3% benefited from an introduction or an adaptation of their anti-arrhythmic treatment and 2.2% of patients were eligible for ablative procedure(cryotherapy). 1.1% of patients received a prescription for polysomnography. 3.3% of patients were reassured as to the normality of the exams already performed without indication of an additional exam.
Note that 73.1% of patients instructed to consult a community doctor were observant. 70.5% of the examinations prescribed at the emergency exit were carried out.
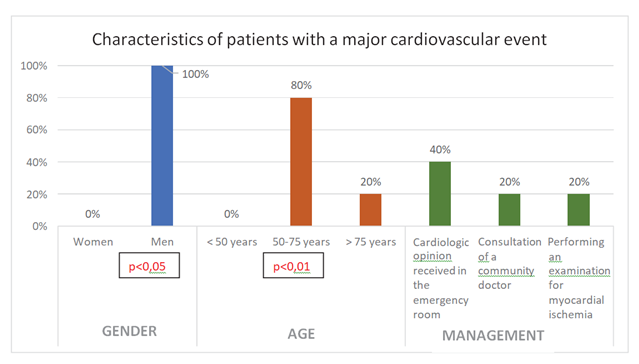
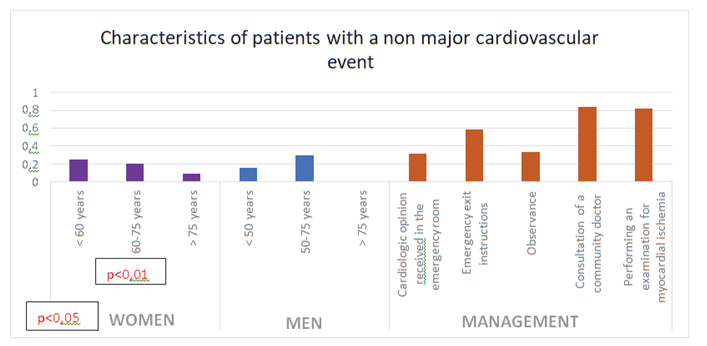
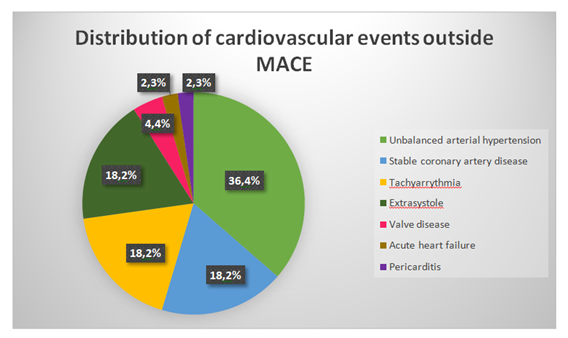
The rate of major cardiovascular events was 2.7% and exclusively for type of acute coronary syndrome(n=5). No patient died from cardiovascular disease and no patient had a stroke. 100% were male with an average age of 63.2 years([± 11]). No patient was under the age of 50 and one of the 5 patients was over 75. Statistically significantly, major cardiovascular events occurred more in men(p<0.05), moreover very significantly in men aged 50 to 75(p<0.01)(Figure 2). 40% of patients with a major cardiovascular event had received a cardiological opinion when they were taken into the emergency department. Out of the 5 MACEs in our study, 2 of the 5 patients had not have discharge orders (40%), 1 of these 2 patients consulted a liberal cardiologist who did not schedule an examination additional thereafter. 1 patient had been instructed to consult a community cardiologist but had not done so, 1 patient had to go to a community cardiologist and perform an exercise test but had not followed these instructions. As for the last patient, an additional investigation prescribed by the emergency department as part of a myocardial ischemia assessment had been carried out and had been found to be pathological, leading to the scheduling of coronary angiography. However, the patient had acute coronary syndrome before in the time between examinations. 23.4% of patients in our cohort presented cardiovascular events outside of MACE. The average age of these patients was 58 years ([±14.7]), 9% were over 75. 54.6% of these patients were women(statistically significant result,p<0.05), with an average age of 61 years([±15.8]). 9.1% were women over 75 and 25% were under 60. Very significantly, non-major cardiovascular events occurred more among women aged 60 to 75(p<0.01). For the male population, the average age was 54.4 years([±12.7]). 15.9% of the men were under 50 and none were over 75. A cardiological opinion was requested for 31.2% of these patients when they went to the emergency department. 59% had received instructions after leaving the emergency department, and 88% of these instructions were followed. Out of all these non-major cardiovascular events, 84.1% of them had consulted a liberal doctor afterwards. 81.8% of these patients had performed additional cardiological examinations and 91.7% of these were adapted to the underlying cardiological pathology(Figure 3). Among these cardiovascular events, we found 36.4% of unbalanced arterial hypertension, 18.2% of stable coronary artery disease or supraventricular tachycardia or extrasystole(Figure 4).
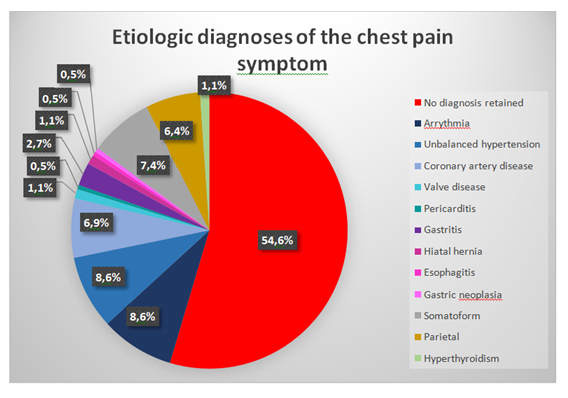
Ultimately, 45.4% of patients received an etiological diagnosis. For 25.7% of the total population, chest pain was labeled cardiovascular.For 4.8% of patients the pain symptom was labeled gastroenterological. The symptom was for 7.4% of somatoform origin, for 6.4% of parietal origin and for 1.1% of endocrine origin. There was no statistically significant difference in the final non- cardiovascular or absent diagnoses based on the sex and/or age of the patients (Figure 5).
Discussion
In our study, 585 patients were admitted to the emergency department for chest pain. 42.2% of them returned home with a diagnosis of discharge of chest pain of undetermined origin, these data being in agreement with those of the literature[3,5]. Almost half of the patients returned home without any specific follow-up instructions. This rate is higher than in the literature(20%)[4,11]. This can be explained by the fact that the cohorts of these authors included more patients with a history of coronary artery disease and/or diabetes and/or dyslipidemia and were therefore at greater risk of a cardiac event. Similarly, we can also correlate this tendency to the fact that the use of a cardiologic opinion in our work is lower than that objectified in the literature, leading by extension to an absence of particular instruction in our case. Patients returning home without particular instruction were more women in our study and this, statistically significant, which to our knowledge has never been established in the literature. All the same, it is well established that the diagnosis of coronary artery disease is more often mentioned in men than women[13]. Our result is all the more important to underline that women are a particular population concerning the acute coronary syndrome[14,15]. Furthermore,we did not find any statistically significant difference in terms of allocation of exit instructions according to the age of patients while certain studies point out the “trap” of the atypical presentation of acute coronary syndromes in young patients (below the pivotal ages of 50 for men and 60 for women, or elderly patients over 75 for both sexes)[15]. 35.3% of the patients in our study returned home with the instruction to follow up with a community doctor without any subgroup according to age or gender being statistically significant. It should be noted that we have not found any data on this subject in the literature. 29.3% of patients left the emergency department with the instruction to carry out at least one additional examination in the city, a rate slightly higher than in the literature[16]. In addition, 55.8% of patients were prescribed a workup myocardial ischemic in the city while in different studies we find rates from 20.4% to 78.7%[4,11,17].
When the general practitioner is consulted, the psychogenic etiology is diagnosed in 26.9% of the patients in our study, while the data in the literature fluctuates between 4 and 18%[13]. We find a rate of pain of parietal origin lower in our study at 14.9%[13,18]. The digestive etiology used by general practitioners is advanced in the same proportions in other works. It is the same for a pulmonary origin[13]. Only 1.5% of the patients in our study received a prescription from their general practitioner to perform an exercise test, the data in the literature on this subject present a very wide scale from 4.2 to 35.7%[7,13,18]. Thus, general practitioners do not seem to be advancing systematically the cardiovascular origin to the thoracic pain episode which led the patients to Emergency. 47.9% of patients in our cohort consulted a cardiologist within 6 months of their chest pain episode. Cardiologists in our study prescribed ischemic explorations for 54.5% of patients against 71.9% in the literature but in a larger cohort[7]. Unlike the data in the literature, our study tends to show that going to the emergency department for a reason of chest pain with reassuring results does not lead mainly to the search for coronary artery disease from the emergency department. This can be explained in particular by the fact that the populations of the various studies in the literature had more cardiovascular risk factors.
The rate of major cardiovascular events in our study is 2.7%, exclusively with type of acute coronary syndrome, and occurred only in men. This rate is similar to some studies[19]. We have shown statistically significantly that men are more likely to have a major cardiovascular event than women, in agreement with the literature[9,14]. We also demonstrated statistically significantly that men aged 50 to 75 years were the most at risk population. Smith et al. as well as Mikhail et al did not find any significant difference concerning the sex and/or age of the patients having presented a major cardiovascular event[5,19]. 23.4% of our patients presented non-major cardiovascular events, higher rate than in the literature(8.8 to 12.8%), however these studies followed up on a shorter period(3 months and less)[12]. We have shown statistically significantly that women aged 60 to 75 were the population most at risk of having a non-major cardiovascular event within six months. We were unable to compare our data with the literature because they have not been described to date. Among these non-major cardiovascular events, we found 36.4% of unbalanced hypertension, 18.2% of stable coronary artery disease, 18.2% of supra-ventricular tachycardia and 18.2% of extrasystole. A cardiological opinion was requested for 31.2% of these patients when they went to the emergency department. 41% of patients who presented with a non-major cardiovascular event had no instructions for leaving the emergency department. Data on this subject was not available in the literature. Thus, women aged 60 to 75 are a second group of patients to whom special attention must be paid.
A final diagnosis was retained for 45.4% of the patients in our study, while the literature seems to do better(55.1 to 62%)[12]. The cardiovascular etiology was retained for 25.7% of the total population(from 13.3 to 21% in litterature)[12]. Furthermore, non-cardiovascular etiologies of our study have been advanced for 19.7% (in litterature from 34.1% to 48.7%)[12]. We found no statistically significant difference concerning the non-cardiovascular or absent final diagnoses according to the sex and/or age of the patients,while Svavarsdottir et al found non-cardiovascular etiologies predominantly in young patients aged 20 to 40 and in female patients[18].
Conclusion
46.8% of patients consulting emergency patients for chest pain returned home without instructions, statistically significantly mostly women. 2.7% of patients have felt a major cardiovascular event only with type of acute coronary syndrome. These were exclusively men and statistically significantly men 50 to 75 years. 25% of the workforce had non-cardiovascular events major, and in this case it was statistically significantly predominantly women, a fortiori women aged 60 to 75 years. It seems to emerge from our work that these 2 populations are particularly to be monitored and that they could justify better coded exit instructions.
Conflict of interest and source of funding:
None declared
References
- Ferretti-Picco E, Govciyan S, Claessens Y-E, et al. Épidémiologie des douleurs thoraciques prises en charge dans le service des urgences du centre hospitalier universitaire de Nice. Ann Fr Med Urgence 3 (2013): 347-352.
- Philippe Staeger, Francis Meier, Daniel Fishman, et al. La douleur thoracique* [Internet]. Revue Médicale Suisse 9 (2013): 997-1004.
- Katz DA, Dawson J, Beshansky JR, et al. Does Concordance with Guideline Triage Recommendations Affect Clinical Care of Patients with Possible Acute Coronary Syndrome? Medical Decision Making 27 (2016): 423-437.
- Prina LD, Decker WW, Weaver AL, et al. Outcome of patients with a final diagnosis of chest pain of undetermined origin admitted under the suspicion of acute coronary syndrome: A report from the Rochester Epidemiology Project. Annals of Emergency Medicine 43 (2004): 59-67.
- Smith SW, Tibbles CD, Apple FS, Zimmerman M. Outcome of low-risk patients discharged home after a normal cardiac troponin I. J Emerg Med 26 (2004): 401-406.
- Stochkendahl MJ, Mickley H, Vach W, et al. Clinical characteristics, myocardial perfusion deficits, and clinical outcomes of patients with non-specific chest pain hospitalized for suspected acute coronary syndrome: A 4-year prospective cohort study. International Journal of Cardiology 182 (2015): 126-131.
- Czarnecki A, Wang JT, Tu JV, et al. The role of primary care physician and cardiologist follow-up for low-risk patients with chest pain after emergency department assessment. American Heart Journal 168 (2014): 289-295.
- Pitts WR, Lange RA, Cigarroa JE, et al. Repeat coronary angiography in patients with chest pain and previously normal coronary angiogram. The American Journal of Cardiology 80 (1997): 1086-1087.
- Geraldine McMahon C, Yates DW, Hollis S. Unexpected mortality in patients discharged from the emergency department following an episode of nontraumatic chest pain. European Journal of Emergency Medicine15 (2008): 3-8.
- Kelly A-M. What is the incidence of major adverse cardiac events in emergency department chest pain patients with a normal ECG, thrombolysis in myocardial infarction score of zero and initial troponin <=99th centile: an observational study? Emerg Med J 30 (2013): 15-18.
- Manini AF, Gisondi MA, van der Vlugt TM, et al. Adverse cardiac events in emergency department patients with chest pain six months after a negative inpatient evaluation for acute coronary syndrome. Acad Emerg Med 9 (2002): 896-902.
- Kam C, Bilbault P, Calvel L, et al. Douleur thoracique à bilan négatif aux urgences : suivi téléphonique à un et trois mois. Journal Européen des Urgences 22 (2009): 57-58.
- Nilsson S, Scheike M, Engblom D, et al. Chest pain and ischaemic heart disease in primary care. Br J Gen Pract 53 (2003): 378-382.
- Hess EP, Perry JJ, Calder LA, et al. Sex differences in clinical presentation, management and outcome in emergency department patients with chest pain. CJEM 12 (2010): 405-413.
- McQuillan BM, Thompson PL. Management of acute coronary syndrome in special subgroups: female, older, diabetic and Indigenous patients. Med J Aust 201 (2014): 91-96.
- Kwok CS, Parwani PJ, Fischman DL, et al. Nonspecific Chest Pain and 30-Day Unplanned Readmissions in the United States (From the Nationwide Readmission Database). The American Journal of Cardiology 123 (2019): 1343-1350.
- Natsui S, Sun BC, Shen E, et al. Evaluation of Outpatient Cardiac Stress Testing After Emergency Department Encounters for Suspected Acute Coronary Syndrome. Annals of Emergency Medicine 74 (2019): 216-223.
- SvavarsdÃ3ttir AE, JÃ3nasson MR, Gudmundsson GH, et al. Chest pain in family practice. Diagnosis and long-term outcome in a community setting. Can Fam Physician 42 (1996): 1122-1128.
- Mikhail MG, Smith FA, Gray M, et al. Cost-Effectiveness of Mandatory Stress Testing in Chest Pain Center Patients. Annals of Emergency Medicine 29 (1997): 88-98.