Malignant Tumor in Knee Joint Cavity Extra-Articular Resection: Clinical Observation of 4 Cases Series
Article Information
Sayed Abdulla Jami1, Shi Jiandang1*, Md Ariful Haque2, Zhanwen Zhou1
1Department of Spinal Surgery, General Hospital of Ningxia Medical University, Ningxia Medical University, People’s Republic of China
2Department of Orthopedic Surgery, Kunming Medical University, Yunnan, China
*Corresponding Author: Shi Jiandang, Department of Spinal Surgery, General Hospital of Ningxia Medical University, Ningxia Medical University 804 Shengli Street, Xingqing District, Yinchuan, 750004, Ningxia, People’s Republic of China.
Received: 16 December 2019; Accepted: 20 December 2019; Published: 30 December 2019
Citation: Sayed Abdulla Jami, Shi Jiandang, Md Ariful Haque, Zhanwen Zhou. Malignant tumor in knee joint cavity extra-articular resection: clinical observation of 4 cases series. Journal of Orthopaedics and Sports Medicine 1 (2019):098-106
View / Download Pdf Share at FacebookAbstract
Background: The knee is one of the most common places to develop a primary sarcoma. Malignant bone tumors are rare conditions that may be encountered by non-oncologic surgeons only a few times in their careers, but a delay in diagnosis or a misinterpretation of data can have limb and life-threatening consequences.
Methods: A retrospective analysis was conducted on 4 cases of knee joint problems. Patients admitted to the hospital between June 2016 to March 2019. We identified 2 males and 2 females with knee joint malignancy, aged 38 ~76 years. The diagnosis was confirmed by histopathology. All 4 patients underwent total knee joint tumor resection with prosthesis replacement.
Results: The interventions were successfully completed without vascular and nerve injury, but in 1 case, the wound healing was delayed. Knee function was recovered satisfactorily after 24-37 months of follow-up. At the last follow-up, the knee flexion angle range for the 4 patients was 95°, 100°, 100°, and 110°, respectively, and the delay of knee extension was 5°, 10°, 10° and 5°, respectively; tissue tumor association scores were 53%, 77%, 80%, and 83%. Quadriceps muscle strength was grade 4 in two cases and grade 5 in the other two cases. No tumor recurrence or metastasis was detected, and no death occurred.
Conclusion: We identified 4 cases of malignant tumor involving the knee in which total and partial excision and reconstruction were performed.
Keywords
Malignant tumor; Knee joint; Extra-articular resection; Prosthesis implantation; Case series
Knee articles Knee Research articles Knee review articles Knee PubMed articles Knee PubMed Central articles Knee 2023 articles Knee 2024 articles Knee Scopus articles Knee impact factor journals Knee Scopus journals Knee PubMed journals Knee medical journals Knee free journals Knee best journals Knee top journals Knee free medical journals Knee famous journals Knee Google Scholar indexed journals Joint articles Joint Research articles Joint review articles Joint PubMed articles Joint PubMed Central articles Joint 2023 articles Joint 2024 articles Joint Scopus articles Joint impact factor journals Joint Scopus journals Joint PubMed journals Joint medical journals Joint free journals Joint best journals Joint top journals Joint free medical journals Joint famous journals Joint Google Scholar indexed journals Malignant bone tumors articles Malignant bone tumors Research articles Malignant bone tumors review articles Malignant bone tumors PubMed articles Malignant bone tumors PubMed Central articles Malignant bone tumors 2023 articles Malignant bone tumors 2024 articles Malignant bone tumors Scopus articles Malignant bone tumors impact factor journals Malignant bone tumors Scopus journals Malignant bone tumors PubMed journals Malignant bone tumors medical journals Malignant bone tumors free journals Malignant bone tumors best journals Malignant bone tumors top journals Malignant bone tumors free medical journals Malignant bone tumors famous journals Malignant bone tumors Google Scholar indexed journals Articular cartilage articles Articular cartilage Research articles Articular cartilage review articles Articular cartilage PubMed articles Articular cartilage PubMed Central articles Articular cartilage 2023 articles Articular cartilage 2024 articles Articular cartilage Scopus articles Articular cartilage impact factor journals Articular cartilage Scopus journals Articular cartilage PubMed journals Articular cartilage medical journals Articular cartilage free journals Articular cartilage best journals Articular cartilage top journals Articular cartilage free medical journals Articular cartilage famous journals Articular cartilage Google Scholar indexed journals Joint cavity articles Joint cavity Research articles Joint cavity review articles Joint cavity PubMed articles Joint cavity PubMed Central articles Joint cavity 2023 articles Joint cavity 2024 articles Joint cavity Scopus articles Joint cavity impact factor journals Joint cavity Scopus journals Joint cavity PubMed journals Joint cavity medical journals Joint cavity free journals Joint cavity best journals Joint cavity top journals Joint cavity free medical journals Joint cavity famous journals Joint cavity Google Scholar indexed journals Cruciate ligament articles Cruciate ligament Research articles Cruciate ligament review articles Cruciate ligament PubMed articles Cruciate ligament PubMed Central articles Cruciate ligament 2023 articles Cruciate ligament 2024 articles Cruciate ligament Scopus articles Cruciate ligament impact factor journals Cruciate ligament Scopus journals Cruciate ligament PubMed journals Cruciate ligament medical journals Cruciate ligament free journals Cruciate ligament best journals Cruciate ligament top journals Cruciate ligament free medical journals Cruciate ligament famous journals Cruciate ligament Google Scholar indexed journals Swellings articles Swellings Research articles Swellings review articles Swellings PubMed articles Swellings PubMed Central articles Swellings 2023 articles Swellings 2024 articles Swellings Scopus articles Swellings impact factor journals Swellings Scopus journals Swellings PubMed journals Swellings medical journals Swellings free journals Swellings best journals Swellings top journals Swellings free medical journals Swellings famous journals Swellings Google Scholar indexed journals Synovial sarcoma articles Synovial sarcoma Research articles Synovial sarcoma review articles Synovial sarcoma PubMed articles Synovial sarcoma PubMed Central articles Synovial sarcoma 2023 articles Synovial sarcoma 2024 articles Synovial sarcoma Scopus articles Synovial sarcoma impact factor journals Synovial sarcoma Scopus journals Synovial sarcoma PubMed journals Synovial sarcoma medical journals Synovial sarcoma free journals Synovial sarcoma best journals Synovial sarcoma top journals Synovial sarcoma free medical journals Synovial sarcoma famous journals Synovial sarcoma Google Scholar indexed journals Superior patellar articles Superior patellar Research articles Superior patellar review articles Superior patellar PubMed articles Superior patellar PubMed Central articles Superior patellar 2023 articles Superior patellar 2024 articles Superior patellar Scopus articles Superior patellar impact factor journals Superior patellar Scopus journals Superior patellar PubMed journals Superior patellar medical journals Superior patellar free journals Superior patellar best journals Superior patellar top journals Superior patellar free medical journals Superior patellar famous journals Superior patellar Google Scholar indexed journals Osteotomy articles Osteotomy Research articles Osteotomy review articles Osteotomy PubMed articles Osteotomy PubMed Central articles Osteotomy 2023 articles Osteotomy 2024 articles Osteotomy Scopus articles Osteotomy impact factor journals Osteotomy Scopus journals Osteotomy PubMed journals Osteotomy medical journals Osteotomy free journals Osteotomy best journals Osteotomy top journals Osteotomy free medical journals Osteotomy famous journals Osteotomy Google Scholar indexed journals Tibial tubercle articles Tibial tubercle Research articles Tibial tubercle review articles Tibial tubercle PubMed articles Tibial tubercle PubMed Central articles Tibial tubercle 2023 articles Tibial tubercle 2024 articles Tibial tubercle Scopus articles Tibial tubercle impact factor journals Tibial tubercle Scopus journals Tibial tubercle PubMed journals Tibial tubercle medical journals Tibial tubercle free journals Tibial tubercle best journals Tibial tubercle top journals Tibial tubercle free medical journals Tibial tubercle famous journals Tibial tubercle Google Scholar indexed journals Patellar tendon articles Patellar tendon Research articles Patellar tendon review articles Patellar tendon PubMed articles Patellar tendon PubMed Central articles Patellar tendon 2023 articles Patellar tendon 2024 articles Patellar tendon Scopus articles Patellar tendon impact factor journals Patellar tendon Scopus journals Patellar tendon PubMed journals Patellar tendon medical journals Patellar tendon free journals Patellar tendon best journals Patellar tendon top journals Patellar tendon free medical journals Patellar tendon famous journals Patellar tendon Google Scholar indexed journals Tibial prosthesis articles Tibial prosthesis Research articles Tibial prosthesis review articles Tibial prosthesis PubMed articles Tibial prosthesis PubMed Central articles Tibial prosthesis 2023 articles Tibial prosthesis 2024 articles Tibial prosthesis Scopus articles Tibial prosthesis impact factor journals Tibial prosthesis Scopus journals Tibial prosthesis PubMed journals Tibial prosthesis medical journals Tibial prosthesis free journals Tibial prosthesis best journals Tibial prosthesis top journals Tibial prosthesis free medical journals Tibial prosthesis famous journals Tibial prosthesis Google Scholar indexed journals Popliteal muscle articles Popliteal muscle Research articles Popliteal muscle review articles Popliteal muscle PubMed articles Popliteal muscle PubMed Central articles Popliteal muscle 2023 articles Popliteal muscle 2024 articles Popliteal muscle Scopus articles Popliteal muscle impact factor journals Popliteal muscle Scopus journals Popliteal muscle PubMed journals Popliteal muscle medical journals Popliteal muscle free journals Popliteal muscle best journals Popliteal muscle top journals Popliteal muscle free medical journals Popliteal muscle famous journals Popliteal muscle Google Scholar indexed journals Quadriceps muscle articles Quadriceps muscle Research articles Quadriceps muscle review articles Quadriceps muscle PubMed articles Quadriceps muscle PubMed Central articles Quadriceps muscle 2023 articles Quadriceps muscle 2024 articles Quadriceps muscle Scopus articles Quadriceps muscle impact factor journals Quadriceps muscle Scopus journals Quadriceps muscle PubMed journals Quadriceps muscle medical journals Quadriceps muscle free journals Quadriceps muscle best journals Quadriceps muscle top journals Quadriceps muscle free medical journals Quadriceps muscle famous journals Quadriceps muscle Google Scholar indexed journals
Article Details
1. Introduction
The area around the knee joint is a common site of malignant bone tumors. The main treatment for this type of cancer is limb salvage surgery, which involves total resection of the tumor followed by reconstruction of the knee structure. The probability that the tumor will invade the joint cavity is usually low and so in most cases, the swelling around the knee joint is reduced. In rare cases, the malignant mass invades the knee joint cavity as a consequence of biopsy or surgery leading to accidental tumor spread, pathological fractures, invasion of the joint ligament or direct invasion of the joint [1]. The most common procedure for tumor resection Involves opening the joint capsule and reconstructing the affected segment. According to the study of Simon et al. [2] in 16% of cases, the cancerous mass directly penetrates the articular cartilage and invades the articular cavity, while in 9% of cases the tumor grows around the articular cartilage, connect with the joint capsule and enters the joint cavity. Also, in some cases, tumors were found in the intercondylar notch invading the cruciate ligament. When a malignant tumor around the knee joint invades the knee cavity, block resection is required to treat the tumor outside the knee joint. This procedure is complicated and requires very good knowledge of anatomy around the knee joint structures. The evaluation of bone tumors requires a thorough history and physical examination in conjunction with proper utilization and diagnostic understanding of additional tests and procedures. The present study presents data of 4 patients with malignant tumors invading the knee cavity admitted to the department of orthopedics. We performed a retrospective analysis in order to explore the diagnostic features of the disease, total extra-articular knee joint resection technique and clinical effects of the excision.
2. Materials and Methods
2.1 General information
Patient 1 is a 66 years old female who has been complaining of swelling and pain in the left thigh for more than 2 years, which have been aggravating in the 2 months before hospital admission on June 16, 2016. Physical examination on admission identified: claudication, distal left femur palpable, hard mass, local tenderness and limited (0° - 95°) left knee flexion. X-ray film showed osteolytic destruction of the distal femur, with periosteum reaction and soft tissue mass. MRI revealed that the tumor mass protruded into the suprapatellar sac leading to fluid accumulating in the cavity. The myogenic mesenchymal tumor was confirmed by the pathological diagnosis of distal femoral tumor biopsy. Cytologic examination of knee effusion smear revealed malignant tumor cells.
Patient 2 is a 76 years old male who has been complaining of swelling and pain in the right distal femur for years, which started to aggravate 1 month before hospital admission on December 6, 2016. During the physical examination, the patient was found to be bedridden, right distal femur visible swelling was identified as well as palpable, hard mass, tenderness, and limited (0° -30°) right knee flexion. The X-ray showed dilated dissolution of the distal right femur bone destruction, tumor discontinuity with the cortical distal femur, pathological fracture. MRI showed the tumor invaded into the knee joint cavity. The pathological diagnosis of tumor biopsy confirmed a malignant fibrous histiocytoma.
Patient 3 is a 59 years old female with a history of 2 days of left knee joint swelling and pain after fall in 2017. She was admitted to the hospital on February 2. Upon physical examination on admission, the patient lay on the bed, had the left knee joint swollen. The free patellar test was positive, the left external femoral condyle was tender, and the left knee joint was fixed in flexion position due to pain. X-ray and CT showed a lytic destruction of the left femoral condyle with the pathological bone fold. MRI showed tumor invasion of the knee cavity (Figure 1A). Chondrosarcoma diagnosis was confirmed by pathological biopsy examination (Figure 1B).
Patient 4 is a 38 years old male and had right knee pain for half a year, aggravating for 1 month. He was admitted to hospital on August 23, 2017. During the physical examination on admission, no swelling of the right knee joint was identified, floating patellar was negative, and the flexion of the right knee joint was limited (0° - 90°). The X-ray showed the right femur with no significant bone destruction in the tibia. MRI showed intra-articular soft tissue tumors involving inter-condylar fossa and posterior articular capsule. The tumor biopsy was performed under the guidance of b-ultrasound, and the pathological diagnosis was synovial sarcoma.
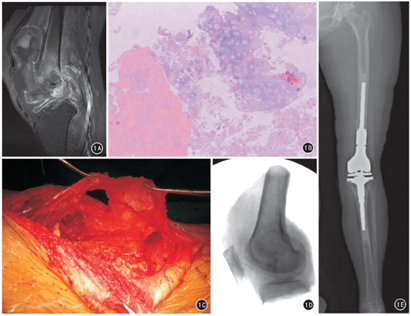
Figure 1: Extra-articular total knee resection combined with artificial tumour type knee prosthesis replacement in a 59 years old female with distal femoral pathological fracture (1A) Pre-operative knee joint sagittal MRI shows bone destruction at the distal femur, tumour invasion of the knee joint and superior patellar. (1B) Preoperative puncture and pathological examination confirmed the disordered arrangement of cartilage and Chondrocyte cells of different sizes invading surrounding bone. (1C) During the operation, the tendon of rectus femoris was retained, the patella was cut open in coronal position, and the patellar tendon was retained. (1D) The specimens were removed during the surgery, and X-ray film showed that resection was successful. (1E) X-ray showing the prosthesis in correct position.
2.2 Surgical methods
All 4 patients in this group underwent excision of the extra-articular tumor and partial resection of the knee joint. In order to perform resection with tumor-free margins, we retained some quadriceps and tibia tendon and we applied a balloon tourniquet. The anterior medial incision of the knee was made, and the biopsy site was removed. The flap should be fully dissociated on both sides and be sharp outside the suprapatellar free quadriceps femoris tendon, avoiding the upper sac in operation. The medial tibial edge was freed using the oscillating saw to perform the coronal osteotomy of the patella cut with swing saw. Dividing the thickness of the tibia ensures that the osteotomy does not enter the knee joint. We dissociated the patellar tendon from the patella between the lower fat pads, we preserved the patellar tendon and we flipped the extensor device (Figure 1C)
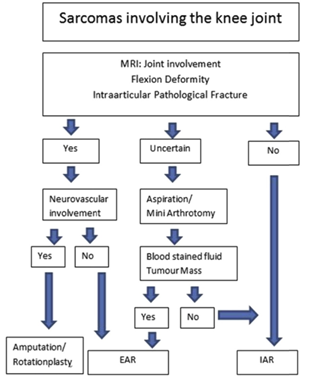
Figure 2: Sarcomas involving the knee joint diagnostic and treatment. EAR represents Extra-articular resection, and IAR represents Intra-articular resection.
Line of femur section bone and preoperative location of the osteotomy plane were determined according to MRI. The distance between the femoral osteotomy and the swollen portion of the knee was 3-5 cm, thus preventing the rupture of the joint cavity. Then, the distal end of the femur was lifted, blood vessels were protected and freed on the inside, and the branches into the joint were ligate and cut. The entire knee joint was raised and separated from the posterior compartment structure. The internal and lateral head of the gastrocnemius anatomizes distally to cover the posterior capsule and obtain a safe margin. At the tibia, the osteotomy plane is level with the tip of the fibula head, approximately 12 mm below the tibial plateau. Tibial tubercle was retained to maintain patellar tendon attachment. Osteotomy plane was situated lower than semi-membrane tendon and posterior articulation ligament and it stops at the tibial attachment, avoiding residual posterior cruciate ligament. On the tibia, the flatness of the osteotomy cuts the popliteal muscle sharply. After a tibial osteotomy, the tumor was entirely removed (Figure 1D). The reconstruction methods were used in combination with artificial tumor knee prosthesis. The prosthesis was intramedullary fixed with bone cement without the use of the tibial prosthesis (Figure 1E).
2.3 Efficacy evaluation
Postoperative knee function was evaluated by the international association of bone and soft tissue tumors (Musculoskeletal Tumour Society, MSTS) scoring criteria. Using muscle strength, the grading method (0 to 5) evaluates the quadriceps muscle strength.
3. Results
All the 4 patients were operated successfully, and the operation time was 2 ~ 2.5 hours. After surgery on the 10th day, there was local necrosis of the skin margin in a patient. After debridement, the skin was sutured and healed again. All of the patient’s surgery area did not appear Infection, patella fracture, prosthesis loosening, and other prosthesis complications. There were no local recurrence and lung metastases observed in the other 3 cases. All the 4 patients were followed up for 7, 8, 9 and 16 months, the range of motion of knee flexion activities was 95°, 100°, 100°, 110°, and the knee extension was delayed 5°, 10°, 10°, and 5°. MSTS scores were 53%, 77%, 80%, and 83% respectively. Quadriceps muscle strength was 4, 4, 5, and 5, respectively.
4. Discussion
4.1 Diagnosis of tumor invasion of the knee cavity
MRI is highly sensitive to the diagnosis of tumor invasion into the joint cavity, especially contrast-enhanced T1 WI. Schima et al. [3] treated 46 patients with osteosarcoma around the joint; Postoperative pathology confirmed that 10 patients had tumor invasion into the articular cavity, which was consistent with the MRI examination results; 11 other patients underwent surgery, preoperative MR suggesting tumor invasion into the joint cavity, but postoperative pathological findings were false positive due to the inflammatory changes around the tumor; it can lead to false statement or result with a specificity of only 69%. Anract et al. [4] performed total extra-articular knee resection on 9 patients, including 2 patients with preoperative MRI showing invasion of femoral trochlear and of the cruciate ligament, but postoperative pathology revealed a false positive result; therefore, the authors suggest that patients with suspected joint cavity invasion, arthroscopy should be specially performed for the lesion located in the joint. In some cases, a preoperative MRI examination could not determine whether the joint was affected or not, so a small incision biopsy was performed to evaluate the properties of joint effusion. After that, it is decided to perform an extra-articular resection for joint repair. [5]. Shahid et al. [6] proposed a detailed diagnostic process: first, perform an MRI check; if MRI cannot clear whether the joint is involved, the next step is to perform puncture cytology or minimally invasive arthroscopic biopsy. In the present study, patients 2 & 3 had pathologic fracture; MRI showed tumor invasion of the joint cavity, and a diagnostic biopsy was performed. Patient 1 MRI showed a tumor protruding into the suprapatellar region; the cytological examination revealed tumor cells as evidence of invasion of the joint cavity. Patient 4 had a tumor in the intercondylar fossa and to prevent the tumor from spreading, we used ultrasound-guided needle biopsy to confirm the diagnosis. We believe that the nature of the tumor should be clearly defined before surgery. In order to determine if the joint cavity is involved, one can use a needle biopsy or minimally invasive check to avoid tumor spread.
4.2 Anatomical and surgical points of total knee arthroplasty
There are 13 synovial sacs around the knee joint. Among them, the synovial sac connection with the knee joint cavity can be detected according to connection probability as follows: the suprapatellar bursa was 80%, the popliteal bursa was 100. 0%, the semi-membrane bursa was 20.0%, and the medial gastrocnemius bursa was 24.1% [7]. Extra-articular total knee resection requires the removal of the synovial capsule, suprapatellar capsule, and the knee extensor device (situated in front of the knee cavity and composed of quadriceps femoris, patella, and patellar ligament).
There are 2 types of extensor device resection: complete and partial resection.
4.2.1 Complete resection of the extensor device
Anract et al. [4] reported 9 patients who underwent resection and reconstruction of the knee extension devices through gastrocnemius medial head flap. Capanna et al. [1] completely resected the knee extension device in 14 patients and reconstructed the knee extension device with composite allograft tibia, patellar tendon, and part of the quadriceps tendon.
4.2.2 Partial resection of the extensor device
The purpose of this resection type is to improve the knee extension function after surgery. During the operation, the quadriceps femoris and the suprapatellar capsule were sharply separated. The superficial quadriceps tendon was retained, the patella was cut in a coronal position, all or part of the patellar tendon was retained, and the subpatellar fat pad was removed together with the tumor. The anatomical basis for retaining the partial knee extensor is the deep subpatellar bursa between the patellar ligament and the subpatellar fat pad; research studies have found that the deep subpatellar bursa does not communicate with the articular cavity [8]. Therefore, theoretically, intraoperative resection of the entire sub-patellar fat pad, joint capsule and the retention of the patellar ligament is possible.
We found 7 articles (147 patients) published during 2000-2016 on total extra-articular knee arthroplasty [1, 4-6, 9-11]; among them, 28 cases underwent complete knee extension device resection and in 125 cases partial excision was performed. All 4 patients from our group received partial resection of the knee extension device. Preoperative MRI helped us to determine the extent of the quadriceps that needed to be removed. The patella was subjected to coronal osteotomy with an oscillating saw to avoid entering the articular cavity and to retain the patellar ligament and the sub-patellar pad was removed along with the tumor. The popliteal, semi-membranous, and medial gastrocnemius sacs are located behind the knee joint on the lateral border of the lateral condyle of the femur, so the popliteal sac is always connected to the knee cavity. To ensure a good surgical incision margin, the popliteal sac cannot be exposed during the operation. The popliteal muscle needs to be cut off in the tibial osteotomy plane. The medial and lateral head of the gastrocnemius is dissected to the distal side, and the semi-membranous muscle is stopped to the proximal end after the joint capsule was covered, the muscle was cut off, and the medial gastrocnemius capsule and semi-membrane muscle capsule were removed simultaneously to safe the margin. The insertion of the posterior cruciate ligament is located below the posterior tibial plateau; as usual, tibial plateau osteotomy was performed by the method of knee joint surface replacement the cruciate ligament, the posterior joint capsule can rupture and cause the tumor to contaminate normal tissue. Yan et al. [12] measured the distance from the farthest end of the tibial attachment of the posterior cruciate ligament to the tip of the fibula separation is (2.8 ± 2.8 mm). Therefore, there is no involvement of the tibia in the extra-articular total knee resection; tibial plateau osteotomy needs to be flat fibula tip level, which can be cut, in addition to the posterior joint capsule and semi-membrane muscle insertion, can retain the patellar ligament insertion. In 2016, Gilg et al. [13] discussed whether extra-articular total knee resection was needed, in addition to a literature review of the upper tibia-fibular joint, identifying 4 articles in which through cadaver studies 10% -4% of the upper tibiofibular bone was detected to be connected with the knee cavity. Also, the upper tibiofibular joint was validated by direct arthrography and a load of muscle capsule was 100% connected with the knee joint cavity. The recurrence rate of upper tibiofibular joint resection was 4%-8%, so it is uncertain whether the removal of the upper tibiofibular joint will reduce local recurrence. In this 4 cases group, the tibia was truncated at the level of fibula micro cephalous in all patients, and the upper tibiofibular joint was not resected. The author believes that although the tibiofibular bone may be connected with the knee joint cavity, whether or not to remove the superior tibiofibular joint should also be carefully examined before surgery, and the signs of distal femoral tumors such as the involvement of the superior tibiofibular bone can be retained intraoperatively. However, the author concludes that extra-articular resection of the knee allows for good oncologic and functional outcomes.
4.3 Clinical outcome of total knee arthroplasty
Because of the need to remove more bone and knee extension devices, total external knee resection was performed. Kendall et al. [9] compared the postoperative results of extra-articular resection and intra-articular resection of tumors in 9 patients. In 56 % of the case, postoperative infection (4 patients) and local recurrence (1 patient) were assessed by MSTS points. Postoperative infection was found in 1 patient after intra-articular resection without local recurrence. In that case, the MSTS score was 80%, and the postoperative function was better than that of the extra-articular resection group (p=0,03). Therefore, preoperative diagnosis of tumor invasion of the joint cavity must be made in support of an appropriate choice of surgical method. Taking into consideration the small number of cases reported in the literature [1, 4], [9-11] the treatment of knee devices varies, with extra-articular total knee resection for swelling. The results differ depending on the ontological or functional point of view.
Most cases of central extra-articular total knee resection were reported by Hardes et al. [5]. Among 59 patients, partial resection of the knee extension device was performed in 55 patients and total resection in 4 patients. During an average follow-up of 56 months, recurrence was observed in 2 cases (3%), infection around the prosthesis in 22 cases and prosthesis wear in 12 cases. There were 10 cases of prosthesis loosening, 6 cases of periprosthetic fracture and 1 case of prosthesis fracture. The MSTS score was 73%, with average knee flexion of 72°. Shahid et al. [6] reported a recurrence rate of 29% in 42 patients with partial knee extension devices, with MSTS score of 86.7%, average knee flexion of 102°, 3° average elongation delay. Soft osteosarcoma was identified in 8 cases and underwent extra-articular surgery, with local recurrence in 4 patients. According to the authors, surgical resection of the entire knee joint in patients with chondrosarcoma should be considered carefully. The 4 patients in this group were followed up for an average of 18.5 months (range 26 to 37 months). No local recurrence or lung metastases were observed. Knee flexion mean curve was 101°, the mean knee extension delay was 7.5 °, and the mean MSTS score was 73%. However, the survival rate, recurrence, and outcomes of each type of malignant bone tumor vary.
5. Conclusion
Careful analysis of preoperative imaging data combined with the necessary intra-articular biopsy is helpful in order to achieve a correct diagnosis of malignant tumor invading the knee cavity. During the procedure, the integrity of the knee capsule was ensured, and the excision of the tumor was completed, followed by prosthesis placement prosthesis and soft tissue reconstruction. We obtained a very good outcome in terms of joint functionality. The sample size discussed in this study is small and therefore, a more comprehensive statistical analysis is not possible. A larger cohort study should provide more detailed information relevant for clinical diagnosis and treatment of this rare type of bone malignancy.
Ethical Approval
Hospital ethical committee approved this manuscript for publication.
Source of Funding
Not applicable.
Abbreviations
Not applicable.
Authors’ Contributions
SAJ, SJ, and MAH designed the manuscript; MAH conducted follow-up procedures; SJ guided and revised manuscript; SAJ, MAH, and ZZ wrote different parts of the manuscript; ZZ helped to translate Chinese to English; All authors approved the final manuscript.
Statement of Informed Consent
Research-informed consent was obtained from the institutional protocol.
Statement of Human and Animal Rights
The ethical standards of the responsible committee on human experimentation (institutional and national) and the recommendations of the Helsinki Declaration of 1975, as revised in 2000 and 2008 were followed accordingly.
References
- Capanna R, Scoccianti G, Campanacci DA, et al. Surgical technique: extraarticular knee resection with prosthesis-proximal tibia-extensor apparatus allograft for tumors invading the knee [J]. Clin Orthop Relat Res 469 (2011): 2905-2914.
- Simon MA, Hecht JD. Invasion of joints by primary bone sarcomas in adults [J]. Cancer 50 (1982): 1649-1655.
- Schima W, Amann G, Stiglbauer R, et al. Preoperative staging of osteosarcoma: efficacy of MR imaging in detecting joint involvement [J]. AJR Am J Roentgenol 163 (1994): 1171- 1175.
- Anract P, Missenard G, Jeanrot C, et al. Knee reconstruction with prosthesis and muscle flap after total arthrectomy [J]. Clin Orthop Relat Res (2001): 208-216.
- Hardes J, Henrichs MP, Gosheger G, et al. Endoprosthetic replacement after extra-articular resection of bone and soft-tissue tumours around the knee [J]. Bone Joint J 95 (2013): 1425-1431.
- Shahid M, Albergo N, Purvis T, et al. Management of sarcomas possibly involving the knee joint when to perform extra-articular resection of the knee joint and is it safe? [J]. Eur J Surg Oncol 43 (2017): 175-180.
- Li wenchun, li zhenqiang, Chen eryu. Morphology and clinical significance of synovial capsule around knee joint [J]. Chinese journal of clinical anatomy 11 (1993): 9-12.
- Laprade RF. The anatomy of the deep infrapatellar bursa of the knee [J]. Am J Sports Med 26 (1998): 129-132.
- Kendall SJ, Singer GC, Briggs TW, et al. A functional analysis of massive knee replacement after extra-articular resections of primary bone tumors [J]. J Arthroplasty 15 (2000): 754-760.
- Zwolak P, Kühnel SP, Fuchs B. Extraarticular knee resection for sarcomas with preservation of the extensor mechanism: surgical technique and review of cases [J]. Clin Orthop Relat Res 469 (2011): 251-256.
- Ieguchi M, Hoshi M, Aono M, et al. Knee reconstruction with endoprosthesis after extra-articular and intra-articular resection of osteosarcoma [J]. Jpn J Clin Oncol 44 (2014): 812-817.
- Yin qin, tao kun, song xixi, et al. Height difference between fibula head and tibia of posterior cruciate ligamentMeasurement of distance and its significance [J]. Chinese journal of orthopaedic surgery 23 (2015).
- Gilg MM, Wibmer C, Andreou D, et al. Is superior tibiofibular joint resection necessary in extraarticular knee resection for sarcomas? Asystematic review [J]. World J Surg Oncol 14 (2016): 28.
