Lung Hydatid Cysts in Children, Evaluation and Surgical Management
Article Information
Burkan Nasr1,3,4,6, Anwar Al_junaeed1, Ghaleb Al Sady2, Ahmad Al Shehari2, Ali Amri3, Mohammed Issa3, Abdulhakim Al Tamimi6, Saeed Al Bahlooli4, Mohammed Al_Sormi5, Abdulfattah Altam7, Yasser A Obadiel3, Mohammed Al-Shehari3, Ali Hiddan6
1Department General and Laparoscopic surgery Al Thawra Modern General/ Teaching Hospital Sana`a and Suadi Hospital at Hajjah, Yemen
2Department of pediatrician, Saudi Hospital at Hajjah, Yemen
3Department of Surgery, Sana`a University, Yemen
4Department of Surgery, Thamar University. Yemen
5Department of pediatrics surgery, Science Technology Hospital, Sana'a, Yemen
6Department of pediatrics surgery, Aden University, Yemen
7Department of Surgery, 21 September University, Yemen, Sana'a
*Corresponding Author: Burkan Nasr Rashed Shaif, Fellowship MIS, Bariatric and Metabolic Surgery. Consultant General and Laparoscopic surgery Al Thawra Modern General/ Teaching Hospital Sana`a and Suadi Hospital at Hajjah, Yemen.
Received: 29 December 2022; Accepted: 18 January 2023; Published: 03 February 2023
Citation: Burkan Nasr, Anwar Al_junaeed, Ghaleb Al Sady, Ahmad Al Shehari, Ali Amri, Mohammed Issa, Abdulhakim Al Tamimi, Saeed Al Bahlooli, Mohammed Al_Sormi, Abdulfattah Altam, Yasser A Obadiel, Mohammed Al-Shehari, Ali Hiddan. Lung Hydatid Cysts in Children, Evaluation and Surgical Management. Journal of Cancer Science and Clinical Therapeutics. 7 (2023): 25-38.
View / Download Pdf Share at FacebookAbstract
The aim of this study was to review the problems encountered in treating pediatric patients with complicated ruptured lung hydatid cysts and to highlight the risks associated with delays in surgical treatment for lung hydatid disease.
Methods: A prospective analysis of 50 pediatric patients with lung hydatid cysts, surgical management was performed in Saudi Hospital at Hajjah,Yemen. Between April 2015 and April 2022, the patients were divided into two groups, intact noncomplicated (group 1, n = 27) or complicated (group 2, n = 23). A complicated cyst was that had ruptured into a bronchus or into the pleural cavity. Data related to symptoms, preoperative complications, surgical procedures performed, postoperative morbidity, and hospitalization time were collected from patient’s parents, medical record and the group findings were compared.
Result: Fifty surgical procedures were performed: 45 posterolateral thoracotomies, 2 posterolateral thoracotomies with phrenotomy, two posterolateral thoracotomies with laparotomy and one case tube thoracostomy. Cough, chest pain and dyspnea was main presented symptoms in both groups. In addition to these, the patients with complicated cysts presented with expectoration of cystic contents, hemoptysis, productive sputum, and fever. The differences between the groups with respect to the rates of preoperative complications and postoperative morbidity, frequency of decortications, and hospital stay were statistically significant (p < 0.05).
Conclusions: Surgery is the primary mode of treatment for pediatric patients with lung hydatid disease. Complicated cases have higher rates of preoperative and postoperative complications and require longer hospitalization times and more extensive surgical procedures than uncomplicated cases.
Keywords
<p>Children Hydatid Cyst; Lung Hydatid Cyst; Yemen Hydatid Cyst</p>
Children Hydatid Cyst articles; Lung Hydatid Cyst articles; Yemen Hydatid Cyst articles
Children Hydatid Cys articles Children Hydatid Cys Research articles Children Hydatid Cys review articles Children Hydatid Cys PubMed articles Children Hydatid Cys PubMed Central articles Children Hydatid Cys 2023 articles Children Hydatid Cys 2024 articles Children Hydatid Cys Scopus articles Children Hydatid Cys impact factor journals Children Hydatid Cys Scopus journals Children Hydatid Cys PubMed journals Children Hydatid Cys medical journals Children Hydatid Cys free journals Children Hydatid Cys best journals Children Hydatid Cys top journals Children Hydatid Cys free medical journals Children Hydatid Cys famous journals Children Hydatid Cys Google Scholar indexed journals Lung Hydatid Cyst articles Lung Hydatid Cyst Research articles Lung Hydatid Cyst review articles Lung Hydatid Cyst PubMed articles Lung Hydatid Cyst PubMed Central articles Lung Hydatid Cyst 2023 articles Lung Hydatid Cyst 2024 articles Lung Hydatid Cyst Scopus articles Lung Hydatid Cyst impact factor journals Lung Hydatid Cyst Scopus journals Lung Hydatid Cyst PubMed journals Lung Hydatid Cyst medical journals Lung Hydatid Cyst free journals Lung Hydatid Cyst best journals Lung Hydatid Cyst top journals Lung Hydatid Cyst free medical journals Lung Hydatid Cyst famous journals Lung Hydatid Cyst Google Scholar indexed journals Yemen Hydatid Cyst articles Yemen Hydatid Cyst Research articles Yemen Hydatid Cyst review articles Yemen Hydatid Cyst PubMed articles Yemen Hydatid Cyst PubMed Central articles Yemen Hydatid Cyst 2023 articles Yemen Hydatid Cyst 2024 articles Yemen Hydatid Cyst Scopus articles Yemen Hydatid Cyst impact factor journals Yemen Hydatid Cyst Scopus journals Yemen Hydatid Cyst PubMed journals Yemen Hydatid Cyst medical journals Yemen Hydatid Cyst free journals Yemen Hydatid Cyst best journals Yemen Hydatid Cyst top journals Yemen Hydatid Cyst free medical journals Yemen Hydatid Cyst famous journals Yemen Hydatid Cyst Google Scholar indexed journals Hydatidosis articles Hydatidosis Research articles Hydatidosis review articles Hydatidosis PubMed articles Hydatidosis PubMed Central articles Hydatidosis 2023 articles Hydatidosis 2024 articles Hydatidosis Scopus articles Hydatidosis impact factor journals Hydatidosis Scopus journals Hydatidosis PubMed journals Hydatidosis medical journals Hydatidosis free journals Hydatidosis best journals Hydatidosis top journals Hydatidosis free medical journals Hydatidosis famous journals Hydatidosis Google Scholar indexed journals pediatric patients articles pediatric patients Research articles pediatric patients review articles pediatric patients PubMed articles pediatric patients PubMed Central articles pediatric patients 2023 articles pediatric patients 2024 articles pediatric patients Scopus articles pediatric patients impact factor journals pediatric patients Scopus journals pediatric patients PubMed journals pediatric patients medical journals pediatric patients free journals pediatric patients best journals pediatric patients top journals pediatric patients free medical journals pediatric patients famous journals pediatric patients Google Scholar indexed journals pleural cavity articles pleural cavity Research articles pleural cavity review articles pleural cavity PubMed articles pleural cavity PubMed Central articles pleural cavity 2023 articles pleural cavity 2024 articles pleural cavity Scopus articles pleural cavity impact factor journals pleural cavity Scopus journals pleural cavity PubMed journals pleural cavity medical journals pleural cavity free journals pleural cavity best journals pleural cavity top journals pleural cavity free medical journals pleural cavity famous journals pleural cavity Google Scholar indexed journals posterolateral thoracotomies articles posterolateral thoracotomies Research articles posterolateral thoracotomies review articles posterolateral thoracotomies PubMed articles posterolateral thoracotomies PubMed Central articles posterolateral thoracotomies 2023 articles posterolateral thoracotomies 2024 articles posterolateral thoracotomies Scopus articles posterolateral thoracotomies impact factor journals posterolateral thoracotomies Scopus journals posterolateral thoracotomies PubMed journals posterolateral thoracotomies medical journals posterolateral thoracotomies free journals posterolateral thoracotomies best journals posterolateral thoracotomies top journals posterolateral thoracotomies free medical journals posterolateral thoracotomies famous journals posterolateral thoracotomies Google Scholar indexed journals posterolateral thoracotomies articles posterolateral thoracotomies Research articles posterolateral thoracotomies review articles posterolateral thoracotomies PubMed articles posterolateral thoracotomies PubMed Central articles posterolateral thoracotomies 2023 articles posterolateral thoracotomies 2024 articles posterolateral thoracotomies Scopus articles posterolateral thoracotomies impact factor journals posterolateral thoracotomies Scopus journals posterolateral thoracotomies PubMed journals posterolateral thoracotomies medical journals posterolateral thoracotomies free journals posterolateral thoracotomies best journals posterolateral thoracotomies top journals posterolateral thoracotomies free medical journals posterolateral thoracotomies famous journals posterolateral thoracotomies Google Scholar indexed journals thoracostomy articles thoracostomy Research articles thoracostomy review articles thoracostomy PubMed articles thoracostomy PubMed Central articles thoracostomy 2023 articles thoracostomy 2024 articles thoracostomy Scopus articles thoracostomy impact factor journals thoracostomy Scopus journals thoracostomy PubMed journals thoracostomy medical journals thoracostomy free journals thoracostomy best journals thoracostomy top journals thoracostomy free medical journals thoracostomy famous journals thoracostomy Google Scholar indexed journals hemoptysis articles hemoptysis Research articles hemoptysis review articles hemoptysis PubMed articles hemoptysis PubMed Central articles hemoptysis 2023 articles hemoptysis 2024 articles hemoptysis Scopus articles hemoptysis impact factor journals hemoptysis Scopus journals hemoptysis PubMed journals hemoptysis medical journals hemoptysis free journals hemoptysis best journals hemoptysis top journals hemoptysis free medical journals hemoptysis famous journals hemoptysis Google Scholar indexed journals
Article Details
1. Introduction
The Hydatidosis remains endemic to many parts of the world, most notably the South America, Australia, New Zealand, the Mediterranean region and Middle East. Yemen are one of that areas where. hydatid disease is endemic Echinococcosis remains a significant health problem in endemic areas where sheep and cattle are raised, human is incidental intermediate host, become infected from food or water contaminated with canine feces or by direct contact with dogs [1-5]. Hydatid disease, which is caused by parasitic infestation, the Echinococcis granulosus tapeworm and is known as echinococcosis or Hydatidosis [6,7]. Has been acknowledged as a clinical entity since ancient times. Organs of scarified animals were described in the Talmud as bladders full of water, and Hippocrates referred to hydatid disease in the aphorism, when the liver is filled with water and bursts into the epiploon, the belly is filled with water and the patient dies. Rudolphi (1928) first used the term hydatid cyst for the description of echinococcosis in humans. Lungs are the second most common sites for hydatid cysts after the liver, with an incidence of lung hydatid cyst varying between 10% and 40% and liver cyst 60%-80%. Most individuals who contract this parasite are young, and the majority of patients are less than 40 years of age, Children are more likely to develop pulmonary rather than hepatic echinococcus cysts, with male affected more than female [8,9]. However, pulmonary Hydatidosis primarily affects children and young adults, some evidence suggests that echinococcal cysts develop more rapidly in the lungs of children than of adults, which may explain the more common appearance of pulmonary cysts in children. Sometimes the entire hemithorax of young children is occupied by parasitic cysts. In these children, either the contamination must have occurred early after birth or the cysts grew rapidly. Hepatic hydatid disease in patients with pulmonary echinococcosis was found in 10% -30% of the patients, A cyst with a diameter of 10 cm or more consider giant cyst, contains approximately 400 mL of hydatid fluid, and any cyst that grows to a diameter of 5 to 7 cm must be removed. The growth of pulmonary cysts is more rapid than in other organs, mainly because of the negative pressure and the great elasticity of the pulmonary tissue [4,10-16]. The most common areas of involvement of pulmonary echinococcosis are the right lung with lower lobes effected mostly [17]. Multiple cysts have a simultaneous development in either one or both lungs, with a reported incidence of 14% to 24%. [18]. 10%-15% of patients had multiple unilateral cysts and 7%-13% had multiple bilateral cysts [19,20]. The incidence of bilateral pulmonary Hydatidosis varies from 2% to 30% [13,16,21,22]. The clinical manifestations and presentation in these children patients with lung hydatid cyst are directly related to intact or ruptured cyst usually remain asymptomatic until the time of rupture also depend on the site and the size of the cyst. Small peripherally located cysts are usually asymptomatic, whereas large central cysts may manifest with symptoms of compression of adjacent organs. If the patient is symptomatic, the first complaint is often a nonproductive cough; some patients, particularly those with centrally located cysts, may have blood-streaked sputum, although massive hemoptysis does not occur. Some patients complain of a dull or acute chest pain or they present with a sensation of pressure in the chest with no aggravating or relieving features. During infancy the hydatid cyst may disturb the growth of the child. In children who have a supple chest wall, a bulge in the ipsilateral chest may also be observed. Pulmonary hydatid cysts carry significant risk of rupture. Rupture may occur during with factor increase intrathoracic pressure as with attack of chest infection associated with cough, rupture also can occur with chemotherapy or percutaneous aspiration and can lead to severe complications, such as massive hemoptysis, tension pneumothorax or anaphylactic shock. Rupture of the cyst into an adjacent bronchus may be manifested by vigorous coughing and expectoration of salty sputum consisting of mucous hydatid fluid and occasionally fragments of the laminated membrane, generally described as grape skin or frothy blood. In addition, the patient may develop a severe hypersensitivity reaction manifested by generalized rash, high fever, pulmonary congestion, and severe bronchospasm. Occasionally the intrabronchial rupture of the cyst manifests with sudden and severe dyspnea, which may lead to suffocation and death from complete tracheal obstruction by fragments from the hydatid membrane. Diagnosis of rupture of the hydatid cyst is unequivocally made when the hooklets of the parasite are found during microscopic examination of the sputum. Complete intrabronchial evacuation of the hydatid contents may result in cure of the disease in few patients. More often the parasitic membrane and a significant quantity of parasitic fluid remains in the pericystic cavity and the patient experiences complications from local infection. In this case the most usual manifestations are fever, chronic cough, mucopurulent or dark bloody sputum, anorexia, and weight los. [23]. Rupture of the cyst into the pleural cavity is infrequent complication It occurred in 3.5%--5% of the patients. The symptoms are usually insidious and moderate; they consist of dry cough, chest pain, moderate dyspnea, generalized malaise, and fever. These relatively mild clinical manifestations result from preexisting pleural adhesions, which prevent the dissemination of the cyst contents into the whole pleural space. In some patients, particularly those without preexisting pleural adhesions, intrapleural rupture of the cyst produces an acute and dramatic clinical picture consisting of intense chest pain, persistent cough, severe dyspnea and even cyanosis, shock, and suffocation. Frequently symptoms of generalized urticaria, intense pruritus, severe anaphylactic shock, and even death can occur. The symptoms of intrapleural rupture of a hydatid cyst are accompanied by the physical findings of localized or generalized hydropneumothorax. Intrapleural rupture of an infected cyst causes hydatid empyema, which has the clinical signs of a pleural empyema but lacks the allergic manifestations of a simple uninfected cyst [8,24]. Diagnosis of an intact echinococcal cyst is usually based on a suspicion resulting from an unexpected finding on routine chest radiographs. Therefore, the presence of hydatid disease should be considered in a patient who presents with a well-defined spherical density of the lung, or every discrete radiologic lesion observed in any patient over 3 years of age in particularly a patient who has lived or traveled in an endemic area should be considered a hydatid cyst [8,13,16,21,22]. The usual radiographic signs after rupture of a cyst into the bronchi are an air meniscus, water lily sign, and incarcerated membrane [13]. A nodular extra pulmonary appearance suggests secondary hydatidosis of the pleura [13]. Chest CT scanning has added to the diagnosis of hydatid disease of the lung, particularly to the early discovery of coexistent small cysts in the lung and of pending or existing rupture of the cyst. CT scanning also elucidates the cystic nature of a lung mass, particularly one located in the mediastinum. Two diagnostic signs indicating a collapsed parasitic membrane, the serpent sign and the whirl sign. Also, CT scanning appears to be valuable in the follow-up of patients who have had resection or evacuation of hydatid disease of the lung [25]. Ultrasonography and echocardiography are two methods for evaluation of hepatic or pericardial-cardiac cysts it is necessitates investigation for complete diagnosis of a hydatid cyst of the lung to identify other possible locations of cysts [26]. The laboratory diagnosis is complementary to the clinical and radiologic methods. As eosinophilia occurs in 20% to 34% of patients with echinococcosis. Because an increase in eosinophils is also observed in many other diseases, the test has limited diagnostic value. Casoni's intradermal reaction and Weinberg's complement fixation test were widely used in the past. These tests are no longer recommended because of their variable sensitivity and limited specificity a serologic survey is necessary for the follow-up of patients after surgery. Persistently high antibody titers or a secondary increase in the antibody titers 6 to 12 months postoperatively indicate a recurrence [27]. Surgery remains the treatment of choice for hydatid cysts of the lung, it is important in children to use the most conservative surgical methods as possible because children has chance who may be infected a gain, and usually has healthy collapsed lung with great lung capacity for expansion after cyst removed. The objective of the surgical treatment of pulmonary hydatidosis is to eradicate the parasite, to prevent intraoperative rupture of the cyst and subsequent dissemination, and to eliminate the residual cavity, with the maximum preservation of lung tissue. Numerous researchers, prefer as a first choice of treatment lung-sparing operations such as enucleation of the cyst (Barrett's technique) or pericystectomy (Pierez-Fontana technique) with closing of the bronchial openings with or without capitonnage of the pericystic space. Segmental resection, lobectomy and pneumonectomy is rarely indicated for the treatment of hydatid disease of the lung and should be used only when the whole segment, lobe or unilateral lung (respectively) is involved in the disease process. Although the reasons for conservative surgery are well known, different rates of resection are reported. The anatomic resection rate ranges from 4.3%-48.4%, unnecessary resection of the lung must be avoided because the compressed lung is usually healthy and re expands after excision of the cyst [12,16,28-30]. The prognosis and Postoperative complications of lung hydatid cyst in children are influenced by the size and number of cysts and the type of operation. The complication rate ranged between 12.9% and 19% [16,30,31]. With appropriate surgical treatment, the prognosis for children with lung hydatid cyst is excellent, reported that 98.3% of the surviving patients were free of hydatid disease 18 years after the operation [12] The operative mortality in large series doesn't exceed 2% {13,15,31]. While in other series No deaths were encountered [32]. The recurrence rate is also very low. Overall recurrence rate of 2.7% [30]. While in other the series no recurrence was noted [15,16]. The World Health Organization (WHO) conducted multicenter trials of the efficacy of chemotherapy on human hydatidosis. The benzimidazole compounds albendazole (ABZ) and mebendazole (MBZ) exert a direct effect on cumulus oophorous and perhaps also on the wall of the cyst. Report the success rate (partial or total) was 14% in the MBZ group and 30% in the ABZ group. An overall cyst response rate (cure or improvement) of 72.6%. The most common adverse events of patients treated with ABZ according to WHO guidelines are changes in liver enzymes and alopecia. The WHO guidelines recommend chemotherapy for inoperable primary liver or lung echinococcosis and for patients with multiple cysts in two or more organs. Morris (1987) reported that preoperative use of ABZ or MBZ may reduce the risk for recurrence of echinococcosis and facilitate the operation. There are successful results with postoperative chemotherapy in the prevention of postoperative local recurrence. Advocate ABZ postoperatively for complicated hydatidosis and for the treatment of patients with inoperable cysts (10-14 mg/kg/day in cycles of 1 month with 2-week interval between cycles) [33-36].
2. Pathophysiology of Lung Hydatid Cyst
The primary hosts of the infecting organism are the members of the Canidae family, usually dogs, wolves, and coyotes. The primary host contracts echinococcosis by ingesting mature and productive echinococcal cysts in the viscera of an intermediate host (e.g., sheep, goats, cattle, and other herbivorous animals). In the intestines of the primary host the scolices of the hydatid cyst develop into a parasitic worm composed of a scolex, neck, and three proglottids. (i.e., segments). The last proglottid, contains 400 to 800 ova. The proglottid matures and breaks off from the scolex. The ova are released in the feces of the primary host and are then introduced into intermediate hosts (including humans) by ingestion of contaminated grass, water, vegetables. The larval stage, which cannot occur in the main host, begins in the intermediate host and leads to the development of hepatic and pulmonary hydatid cysts. These organs are then ingested by the primary hosts and thus the cycle continues. In the gastrointestinal tract of the intermediate host the chitinous embryophore that surrounds the hexacanth embryo is lysed and the embryo is released. The embryo with the aid of its hooklets attaches to and penetrates the mucosa of the duodenum and jejunum, enters the mesenteric venules, and proceeds to the portal vein. From the portal vein the embryo enters the liver where it becomes embedded, and if it is not destroyed by phagocytosis develops into a cyst [37]. The main pathway the of the parasites' entrance into the lung, though some embryos whose diameters do not exceed 0.3 mm may pass through the sinus capillaries of the liver and by way of the hepatic veins and vena cava proceed to the right side of the heart and the pulmonary capillaries, where there may become embedded. Here, as in the liver, the embryos that survive phagocytosis hypertrophy, the hooklets disappear, and the embryos enter the larval stage and cyst formation, one alternative pathway of the parasites' entrance into the lung is the lymphatic circulation. The embryo enters the lymphatics of the small intestine, proceeds to the thoracic duct, to the central venous system, to the right side of the heart, and then to the lungs. Another possible route is a venovenous anastomosis in the liver and the space of Retzius. The disease can be contracted through the inhalation of air contaminated with echinococcus but rare [12]. Secondary pulmonary cysts may develop when ova enter the venous circulation because of rupture of extrapulmonary cysts. The site of the primary hydatid cyst, producing secondary metastatic pulmonary echinococcus cysts in the heart in 64%, the liver in 26% and the iliac bone in 10%. In such instances, it is difficult to distinguish between primary and secondary cysts (figure 1) [18]. Two types of hydatid cysts occur in humans: the unilocular and the alveolar. This discussion is limited to the unilocular variety, because these are the cysts of clinical importance in the lungs. A hydatid cyst is composed of the wall and the hydatid fluid. There are three layers in the wall of the cyst. Two of these layers, the outer laminated membrane and the inner germinal layer or germinative membrane, derive from the parasite, and one layer, the pericyst or adventitia, is produced by the host. The pericyst or adventitia, is the adventitia, also known as the ectocyst, is rarely thicker than a few millimeters and is composed entirely of the host's cells. It is the result of the inflammatory response of the organ. Functionally this layer provides mechanical protection and nutrition to the parasite. The laminated membrane is 1 to 3 mm thick and is surrounded by a pericystic layer. The membrane is white gelatinous, rich in polysaccharides, and characteristically laminated, which is often obvious to the naked eye. It is composed of hyaline and elastic tissue with no host blood vessels entering into it, and it is easily discernible from the pericystic layer, which is vitally important to the surgeons. When this layer is intact Nutritional and other substances useful to the parasite traverse the membrane by diffusion. The germinal layer (germinal membrane or endocyst) is the inner layer of the cyst wall. It is a thin, transparent, and granular membrane that is lined with small papillae, which are brood capsules at different stages of development. Develop buds of scolices. The scolices have suckers and hooks and represent the mature parasite larvae. The germinative membrane is the living part of the parasite and produces the laminated membrane and reproduces the parasite. Although hydatid cysts of the liver commonly calcify, calcification of such a cyst in the lung is rare. The calcification, which resembles an eggshell, takes place in the adventitia of complicated cysts and does not always indicate that the hydatid is dead. A calcified lung cyst is almost always in communication with the bronchial tree and is probably infected. Some studies report that the remaining pericystic cavity becomes obliterated after the cystic contents are evacuated through the bronchus or after excision of the cyst, others, believe that the residual cavity persists because of epithelialization of the adventitial sacs [17,37,38]. Some studies report that the remaining pericystic cavity becomes obliterated after the cystic contents are evacuated through the bronchus or after excision of the cyst [12,14,32]. Others, believe that the residual cavity persists because of epithelialization of the adventitial sacs [19,31,34].
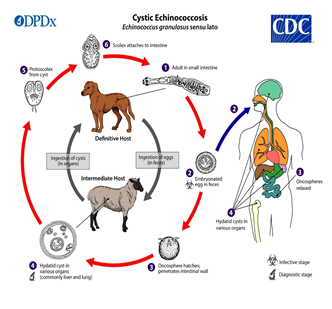
Figure 1: Life cycle of Echinococcus granulosus. (Copy right for Centers for Disease Control and Prevention).
3. Objective
3.1 General
p
To review the clinical presentation and management of lung hydatid cyst, in children patients admitted to Saudi Hospital at Hajjah, Yemen from April, 2015 to April, 2022.
3.2 Specific Aim of our Study
- To identify the frequency of lung hydatid cyst according to age & sex.
- To identify the frequency of lung hydatid cyst according to mode of clinical presentation.
- To identify the Complication possible related to lung hydatid cyst.
- To identify the frequency of different management used in treatment of lung hydatid cyst.
- To identify Hospitalization time used for management lung hydatid cyst.
4. Patients and Methods
A prospective, descriptive study was carried on children patients admitted to Saudi Hospital at Hajjah, Yemen under diagnosis of hydatid lung cyst during the period of April, 2015 through August 30, 2021.
4.1 Patients
A total of 50 patients with clinical diagnosis of hydatid cyst lung were admitted in the surgical ward through surgical outpatient clinic and emergency department. These patients were first assessed clinically by taking history and physical examination. Relevant investigations such as, imaging chest x-ray, chest CT scan, chest U/S, abdomen U/S. The diagnostic evaluations were carried out by variety of radiologist and surgeons but surgical management ware carried by Dr Burkan as single team surgeon.
4.2 Methods
Data were collected from the patient parents, the patient's interview and complete physical examination and specific investigations primarily by the author, with collaborations of the collage surgeons in department of general surgery after training them about variables used, and by medical registers as a secondary source. Data collection outlined on an open close questionnaire specifically prepared for this purpose.
5. The Studied Variables Were
5.1 Hydatid Cyst Lung
Defined as cystic lesion in the lung, infection which is caused by the Echinococcus granulosus parasite.
Type of Hydatid cyst lung: In our study we divided hydatid cyst lung in tow group: -
5.2 Intact Cyst
Cystic lesion without rupture complication was 27 patients, 25 patient's single cyst and 2 patients had multiple, uni and bilateral cyst (Figure 2).

Figure 2: CT scan chest for child 10 Year old with intact Lt Lung hydatid cyst.
5.3 Rupture Cyst
23 of 50 patients (46%) had rupture (group 2). Cyst rupture into the bronchial system occurred in 13 patients (26% of group 2). Cyst rupture into the pleural space occurred in 10 patients (20% of group 2), (6 patients with empyema, 2 lung abscesses, 2 plural effusion), 21 patients single cyst and 2 patients had multiple, uni and bilateral cyst.
5.4 Age
No of years since birth, 4 group intervals will be applied (<6, 6-8, 8-10, 10-12,) with a mean age 7.14 years (range, 5 to 12 years).
5.5 Sex
Represented by Male and Female group the series included 36 females (72%) And 14 males (28%).
5.6 Clinical Presentation
Asymptomatic cyst: 6 patients (12%) from group 1 and 1 patient (2%) from group 2 are asymptomatic Small peripherally located, whereas large central cysts may manifest with symptoms of compression of adjacent organs.
5.7 Cough
If the patient is symptomatic, the first complaint is often a nonproductive cough; some patients, particularly those with centrally located cysts. 12 patients (24%) from group 1 and 20 patients (40%) from group 2 are manifested by cough.
5.8 Chest Pain
Some patients complain of a dull or acute chest pain or they present with a sensation of pressure in the chest with no aggravating or relieving features. Was10 patient (20%) from group 1 and 19 patients (38%) from group 2 are manifested by chest pain.
5.9 Simple Pneumothorax
A 6 patients (12%) from group 2 are presented by simple pneumothorax.
5.10 Tension Pneumothorax
A tension pneumothorax occurs when the pressure on the side of the collapsed lungs builds up to the point where it compresses the heart and compromises circulation. 1 patient from group 2 is presented with tension pneumothorax.
5.11 Empyema
Intrapleural rupture of an infected cyst causes hydatid empyema. 6 patients (12%) from group 2 are presented by empyema.
5.12 Expectoration
Rupture of the cyst into an adjacent bronchus may be manifested by vigorous coughing and expectoration of salty sputum consisting of mucous hydatid fluid and occasionally fragments of the laminated membrane, generally described as grape skin. 5 patients (10%) from group 2 are presented by expectoration of cyst.
5.13 Allergic Manifestation
Generalized urticaria, intense pruritus, severe anaphylactic shock, and even death. 2 patients (4%) from group 2 are presented by allergic manifestation develop severe anaphylactic shock.
Type of Management used:
5.14 Thoracostomy
Tube thoracostomy is performed to evacuate an ongoing production of air/fluid into the pleural space use as definitive treatment for one patient from group 2.
5.14 Thoracotomy
A thoracotomy is a surgical procedure for opening the chest wall to access the lungs. Used 45 cases and associated with phrenotomy in 2 cases and associated with laparotomy in 2 cases only.
6. Statistical Analysis
The distribution of hospital stays in groups 1 and 2 was examined using the Kolmogorov-Smirnow test. This showed that the data from both groups were normally distributed. Once this was confirmed, the mean hospitalization times for groups 1 and 2 were compared using the unpaired t test. Other results were compared using the 12 test and Fisher's exact test as appropriate. The p values less than 0.05 were considered to indicate statistical significance.
7. Result
Prospective study for 50 childern patients with lung hydatid cysts who had operations at surgical department between April 2015 and April 2022 were reviewed. The series included 36 females and 14 male (Table 1). With a mean average age 7.14 years (range, 5 to 12 years), Median 7, Mode 6 and STDEV.P 1.739. Approximately 80% of the patients lived in rural areas. (Hajjah, Hodidh and Amran governorates). Follow-up times for all 50 patients ranged from 2 year to 5 years. The pulmonary cysts were diagnosed by various combinations of chest roentgenogram, thoracic ultrasonography, and thoracic computed tomography. 50 patients undergo of chest roentgenogram, 40 patient chests CT, 15 patient chest Us, 50 patients also undergo abdominal ultrasonography to assess for concomitant hepatic or splenic cysts. Skin and serologic testing were not part of the routine diagnostic workup (Table 2). The patients were divided into two groups based on whether the cyst lesions were intact (group 1, n = 27) or rupture (group 2, n = 23). Any cyst that had ruptured into the bronchus or pleural cavity, with or without infection, was defined as complicated (Figure 2, figure 3). A ruptured cyst was considered to be infected when the patient exhibited accompanying problems of purulent sputum, leukocytosis, fever, and peri cystic pneumonitis with or without lobar and segmental pneumonia. Forty-six patients (92%) of all patients had solitary lung hydatid cysts. A four patients (8%) of all patients had multiple lesions. two of them (4%) of multiple cysts had bilateral lung hydatidosis, and two patients (4%) had unilateral multiple lung hydatidosis. (figure 4). Eight patients (16%) of all patients had unilateral lung lesions and concomitant liver hydatid cyst. One patient had lung, liver, and spleen. Two patients in group 2 had multiple cysts and 21 patients had a single lesion. When the patients were grouped according to their type of hydatid disease (multiple vs. solitary), there was no significant difference in the frequencies of cyst rupture (p> 0.05) but there is correlation between size of cyst and rupture, we found most of cyst rupture with size more than 7 cm. In both groups 1 and 2, the most common symptom was cough, followed by chest pain and dyspnea, respectively (Table 3). There were no differences between the groups with respect to the rates of these symptoms (p> 0.05). Hemoptysis, sputum, and fever were significantly more frequent in group 2 than group 1 (p < 0.05). As previously noted, 23 of 50 patients (46%) had rupture (group 2). Cyst rupture into the bronchial system occurred in 13 patients (26% of group 2). Cyst rupture into the pleural space occurred in 10 patients (20% of group 2), (6 patients diagnosis as empyema, 2 lung abscesses, 2 plural effusion). From both groups, patients who had diagnosis pre-operative pneumonia (n = 17), ((pneumonia+ infected cysts (n = 4), pneumonia+ empyema (n = 2), pneumonia+ infected cysts+ empyema (n = 2), and only pneumonia manifested in (n = 8),)) From group 2 patients who had pre-operative empyema (n = 6), ((empyema+ pneumonia (n=2), empyema+ pneumonia+ infected cysts (n = 2), empyema +pneumothorax (n = 2), Six patients of group 2 presented preoperative with pneumothorax, one as tension pneumothorax. Two patients of group 2 presented with pneumothorax and empyema. All these patients treated by closed-chest tube drainage initially, and further surgical procedures were performed after their general condition had stabilized. One individual presented to the emergency department in septic shock due to empyema and multiple infected hydatid cysts of the lung and with Left liver lobe cyst. A chest tube was placed, and pus drainage through this tube (200 to 500 mL/day) with air babble indicated a bronchopleural fistula. The patient was initially managed by chest tube drainage and antibiotic treatment, and when he showed good response. Later, thoracotomy for lung hydatid cyst, and laparotomy for liver hydatid cyst were performed for this patient in separate time. All group 2 patients received preoperative antibiotic therapy. The course of treatment was a minimum of 7-21 days (mean, 11 days). Third-generation cephalosporins or B-lactamase antibiotics were the usual drugs of choice for empirical therapy. Second or third -generation cephalosporins were administered as postoperative treatment with a duration ranging from 4 to 30 days (mean, 6 days). Efficacy of antibiotic therapy was assessed on the basis of cultures of sputum and pleural fluid and blood and was assessed according to clinical response. Only 10 of 50 patients received preoperative chemotherapy (albendazole), at dose 10-15mg/kg and 1 one patient were referred to our center with a ruptured infected cyst. After surgery, all patients who had complicated or multiple hydatid cysts, or both, were placed on albendazole therapy (10 -15 mg/kg/d) for at least one months. The overall frequency of preoperative complications in group 2 was significantly higher than that in group 1 (p < 0.01) (Table 4). In concern with surgical procedures, decortications were required more for patients in group 2, and this difference between the groups was statistically significant (p = 0.0371).
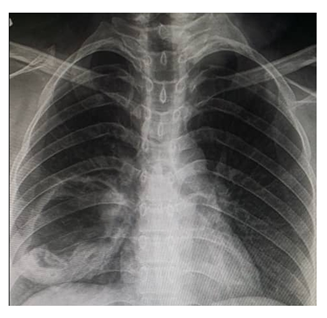
Figure 3: Chest X.ray complicated rupture Rt lung hydatid cyst.
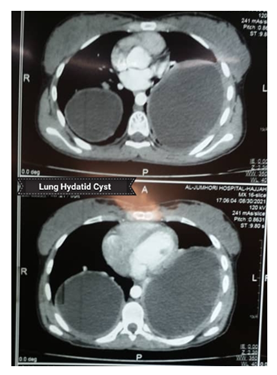
Figure 4: CT scan chest bilateral lung hydatid cyst.
|
Age |
Gender |
% |
Cyst Size |
Median |
||||
|
Group |
Female |
Male |
Total |
|||||
|
|
No |
% |
No |
% |
|
|||
|
<6 yrs |
5 |
10% |
1 |
2% |
6 |
12.00% |
7-14 cm |
10 cm |
|
6-8 yrs |
21 |
42% |
9 |
18% |
30 |
60.00% |
5-15 cm |
10 cm |
|
8-10 yrs |
3 |
6% |
3 |
6% |
6 |
12.00% |
6-13 cm |
7 cm |
|
10-12 yrs |
7 |
14% |
1 |
2% |
8 |
16.00% |
6-12 cm |
7 cm |
|
Total |
36 |
72% |
14 |
28% |
50 |
100 |
||
Table 1: Age groups and gender distribution of the patients and the size of the lung cysts in children.
|
Diagnostic tests |
Count |
|
Chest X-ray |
50 |
|
Chest CT |
40 |
|
Chest US |
15 |
|
Abd US |
50 |
|
Skin and serology test |
0 |
Table 2: Diagnostic tests used for Hydatid Cyst Lung in Children.
|
Clinical Manifestation |
Group 1 |
Group 2 |
P value<0.001 |
||
|
No |
% |
No |
% |
||
|
Asymptomatic |
6 |
12% |
1 |
2% |
p < 0.001 |
|
Cough |
12 |
24% |
20 |
40% |
p > 0.05 |
|
Chest pain |
10 |
20% |
19 |
38% |
p > 0.05 |
|
Dyspnea |
7 |
14% |
12 |
24% |
p > 0.05 |
|
Hemoptysis |
1 |
2% |
3 |
6% |
p < 0.05 |
|
Expectoration of cystic contents |
5 |
10% |
|||
|
Sputum production |
5 |
10% |
8 |
16% |
p < 0.05 |
|
Fever |
5 |
10% |
10 |
20% |
p < 0.05 |
|
Weight loss |
••• |
••• |
2 |
4% |
p > 0.05 |
Table 3: Clinic Manifestation Lung Hydatid Cyst in Children.
|
Preoperative Complications |
Group 1 |
Group 2 |
||
|
No |
% |
No |
% |
|
|
Pneumonia |
7 |
14% |
10 |
20% |
|
Simple pneumothorax |
••• |
••• |
6 |
12% |
|
Tension pneumothorax |
1 |
2% |
||
|
Empyema |
••• |
••• |
6 |
12% |
|
Infected cyst |
••• |
••• |
10 |
20% |
|
Allergic episode |
••• |
••• |
2 |
4% |
|
Lung abscess |
••• |
••• |
2 |
4% |
|
Plural effusion |
2 |
4% |
||
|
Cyst communication |
6 |
12% |
||
Table 4: Preoperative Complication Hydatid Cyst lung in Children.
7.1 Surgical Approach
A total of 50 surgical procedures were performed on the 50 patients (Table 5). The 50 surgical procedures performed; there were 45 posterolateral thoracotomy, 2 Right posterolateral thoracotomy + phrenotomy. These individuals with liver-dome cysts underwent thoracophrenotomy, Two Right thoracotomy and abdomen incision done (one at same cessation and one at separated cessation) and one patient treated by chest tube only because present left lung rupture cyst with plural effusion with dyspnea and fever. Chest tube inserted, cover antibiotic and albendazole used, after 2 weeks improved clinically with shrinkage cystic lesion radiological. After 2 month fellow up X ray was complete cystic resolved.
|
Surgical approach |
No |
% |
|
posterolateral thoracotomy |
4 5 |
90% |
|
Posterolateral thoracotomy +phrenotomy |
2 |
4% |
|
Posterolateral thoracotomy +laparotomy |
2 |
4% |
|
chest tube |
1 |
2% |
|
Total |
50 |
100 |
Table 5: Surgical Approach Hydatid Cyst lung in Children.
7.2 Procedure performed
In 30 patients 60% (intact and rupture group), the specific surgical treatment for pulmonary hydatid cysts was cystectomy with capitonnage. capitonnage refers to emptying the cyst and then closing it by applying sutures so that they approximate the opposing surfaces of the cavity. For this procedure the edges of the surgical wound and the lung surface were protected with wet packs soaked in diluted (10%) hypertonic slain. Due to risks of leakage into the bronchial system and postoperative tracheobronchial irritation or pulmonary edema, other scolicidal agent was not used into the cyst. About 50% of intact cyst enucleation or delevery intact cyst without rupture or evacuated by needle aspiration, (figure 5, figure 6) the others cyst, contents were evacuated by needle aspiration, and the cystic membrane was removed with ring forceps. The remaining cavity was irrigated with saline solution and cleaned with sponges containing diluted (10%) hypertonic slain. Bronchial openings in the cavity were stitched up with 3/0 proline non absorbable sutures in a figure-8 suture. After the bronchial communications were closed, the residual cavity was obliterated with separate purse-string sutures that were placed into the cavity from the deepest level to the surface (capitonnage). In the Complicated cyst exhibited a friable or liquefied pericystic layer and Had damaged the adjacent parenchyma, the closure of bronchial fistulas was done more carefully using deeper sutures and placing them closer together (Table 6). Eight patients 16% of total patient, Endocystectomy only done with closure bronchial communication without cavity closure. Five patients with complicated cysts (10%), a pericystectomy or wedge resection was performed. Lobectomy was performed in 5 patient 10%, one in group 1 and 4 in group 2 as cyst involved whole lobe. One treated by chest tube after that he improved completely and no residual cavity.
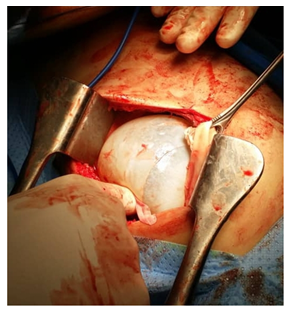
Figure 5: Lt Posterolateral thoracotomy show cystectomy with enucleation or delevery intact Lt Lung hydatid cyst.

Figure 6: post cystectomy for 7 Year child with multiple left lung Hydatid show intact laminated membrane of hydatid cyst.
|
Procedure performed |
No |
% |
|
Endocystectomy with capitonnage |
30 |
60% |
|
Endocystectomy |
8 |
16% |
|
Pericystectomy or Wedge resection |
5 |
10% |
|
Lobectomy |
5 |
10% |
|
Pneumonectomy |
0 |
0% |
|
Chest tube |
1 |
2% |
|
Total |
50 |
100 |
Table 6: Surgical Procedure Lung Hydatid Cyst in Children.
7.3 Postoperative Complications
30 % From total patient, (8%) from in group 1 and (22%) in group 2, develop postoperative complication (p = 0.008) (Table 7). as post-operative complication bronchopleural fistula appears in 4 patients (8%) with prolonged air leak with collapse lung was fail to fistula closure and lung expanded after 3 weeks underwent Re thoracotomy with Decortications and fistula closure was performed in 2 patients (4% in group 2). And 2 other patients refer to thoracic surgeon in another hospital. One patient post right posterolateral thoracotomy with phrenotomy develop biliary pleural fistula with bile leak thought chest tube but improved after 2 weeks with conservative management. There was no postoperative mortality or recurrent cyst during follow up 5 years. The hospitalization times in group 1 ranged from 7 to 19 days (mean, 10 days), whereas those in group 2 ranged from 7 to 60 days (mean, 19 days) (p < 0.05). There was no recurrence in both groups during Five year. Data related to symptoms, preoperative complications, surgical procedures performed, postoperative morbidity, hospitalization time, and cyst recurrence were collected from each patient's parents, hospital documented and daily follow up during admissions and post discharge outpatient clinic follow up.
|
Complication |
Group 1 |
Group 2 |
||
|
No |
% |
No |
% |
|
|
Prolonged air leak (>7 days) (Broncho pleural fistula |
0 |
0 |
4 |
8% |
|
Pneumonia |
2 |
4% |
3 |
6% |
|
Atelectasis |
3 |
6% |
2 |
4% |
|
Pleural effusion |
2 |
4% |
3 |
6% |
|
Wound infection |
0 |
1 |
2% |
|
|
Lung collapse |
2 |
4% |
3 |
6% |
|
Biliary pleural fistula |
1 |
2% |
||
Table 7: Post-Operative Complication Lung Hydatid Cyst in Children.
8. Discussion
The hydatid cyst disease still endemic in Yemen and like other world endemic countries represents a major health problem and The disease is concentrated in the sheep-raising and pastoral areas also in area where street or stray dogs move freely [39-43]. In most of series Pulmonary hydatid disease is more frequent at the early ages and there is predominance in males over females, mostly due to behavioral difference between both sexes, with more exposure of boys [8-12,15,16]. However, in Bulents and cangir report incidence of hydatid cysts was equal in males and females [45,46]. Similar to that in our study children effected by diseases mor than adult, as 50 patient children that represented two third of total patients with lung hydatid cyst and one third was adult patients. But opposite to that in our study the disease predominance in females over males (72%), (28%) respectively. mostly due to more exposure of female to contact with animal, It is not surprising in the Yemeni community since a considerable proportion of females have most activities related to animal breeding and/or agriculture. Similar to previous Yemeni studies ware reported female predominant effected [39-43]. In this study, the finding that there is higher incidence of pulmonary than hepatic hydatid cysts in children and adolescents corresponds with other studies [47,48], The explanation for that is the liver is a compact organ and the hepatobiliary capsules limits the cysts growth and the low resistance of lung tissue provides an excellent medium for rapid growth of hydatid cysts. However, Sehitoqullari [49] believed that liver cysts were more common in childhood and Talaiezadeh [19] found nearly equal incidence of hydatid cysts in lung & liver in children. The age of the youngest patient in this study was 5 years, while in Elburjo study [50], it was three years and in tantawy study [51], it was 21 months and Prashant has reported 6 months [52]. In children the more elastic properties of lung tissue make rapid increase size of cyst in children N. homesh [11], Ali. et al [47] and Burgos [53] defined pulmonary hydatid cysts as giant if it equals nearly half of hemithorax, Was register 26 cm lung hydatid cyst, in our study 15 cm the maximum size of cyst. In this study cough followed by chest pain and dyspnea was most common finding in most patients (64%,58%, 38%) respectively, no significant different in this variable between intact and rupture cyst, with rupture cysts, the clinical picture is variable and depends on the nature of the rupture. Often the cyst ruptures into a bronchus present with all the previously described symptoms and may also exhibit cough-like expectoration of hydatid fluid and remnants of parasitic membrane, recurrent hemoptysis, purulent sputum, or fever, or a combination of some or all of these symptoms Expectoration of cystic contents can lead to severe complications, such as acute respiratory failure, massive hemoptysis, and anaphylactic shock [2,3,32]. In this study Expectoration of cystic contents, hemoptysis, and anaphylactic shock was present in rupture cyst with significant different with p value < 0.05. Rupture of a hydatid cyst into the pleural cavity usually causes pneumothorax, pleural effusion, then empyema. Cyst rupture into the pleural cavity can also result in tension pneumothorax [32], which occurred in 1 of our patients. The documented rates of simple pneumothorax in patients with pulmonary hydatidosis ranged from 4% - 10.2% and Empyema is reported to occur in 6-12% of patients with hydatid disease of the lung [24,31]. In our series, simple pneumothorax occurred preoperatively in 6 cases of group 2 (12% of all patients), and empyema occurred preoperatively in 6 cases of group 2 (12% of all patients). It has been proposed that rupture of a cyst into the pleural cavity or rupture into the bronchial tree may also lead to secondary larval spread or to allergic and anaphylactic reaction [23]. Two of the patients in our series 2 patients (4%) had an allergic episode was came to Emergency department acute cough with membrane expectoration and anaphylactic shock, initial was treated with resuscitation and supportive management and definitive surgery was did after patient became stable. Diagnosis of pulmonary hydatid cyst in endemic area should be suspected in any patient presented with single or multiple opacities on the chest X-ray [54]. In our study Assessment of clinical findings, chest roentgenograms, thoracic computed tomography, and Thoracic ultrasonography led to the correct preoperative diagnosis of pulmonary hydatid disease in 48 patients (96%). The other 2 patients were diagnosed post pneumonia empyema for decortication but intraoperatively we found some hydatid membrane and daughter cyst. However, the accuracy of radiology was 99% in Saleh et al [55], and 94.44% in Ali et al [47]. Some authors report cure rate only 25% to 30% with use oral albendazole or mebendazole against cysts [35, 36] also Wen and Yang [56] found that Chemotherapy weakens the cyst wall, thus increasing the likelihood of cyst rupture.
In addition to the previously mentioned issues in our country these patients tend to be from rural areas where medical care is often inadequate. Our series was not randomized with respect to surgery versus medical treatment, but we believe that due to the possibility of cyst rupture, medical therapy should be used sparingly in patients with pulmonary hydatidosis. This approach should only be used for patients who are high surgical risks or for preventing recurrence after operation. We believe that the most appropriate management for pulmonary hydatidosis are surgery either open or laparoscopy, involving removal of the cyst membrane, closure of the bronchial openings, and capitonnage. However, rupture hydatid cysts tend to cause significant pleural thickening and parenchymal destruction; therefore, more radical surgical procedures, such as decortications, segmentectomy, and lobectomy may be required in these patients [2,13,23]. Reports in the literature note resection rates of 0% to 7% for intact pulmonary hydatid cysts, whereas the corresponding figures for rupture pulmonary hydatid cysts are considerably higher at 19% to 32% [3,4,23]. As previously mentioned, marked pleural thickening due to cyst rupture into the pleural cavity is an important problem. In a study, Aribas and colleagues [31] there study the patients with pulmonary hydatid cysts and associated pleural complications found that decortication was needed in (69.8%) and pulmonary resection was needed in (14%) of patients. In our series, some of the complicated cysts was associated with severe serious parenchymal destruction, or cyst involved whole lobe, therefore 5 lobectomies, 4(8%) in group 2 and one (2%) in group 1. Decortications was performed in 3 patients (6%) in group 2. and one patient (2%) in group I. as intra operative collapsed lung with adhesion and reactive effusion. Rupture pulmonary hydatid cysts are associated with higher postoperative morbidity and mortality than intact cysts [31,13,23]. In Rupture cases, infection and inflammation of the adjacent lung parenchyma may affect wound healing and lead to postoperative complications such as prolonged air leakage, empyema, and pneumonia. In addition, many patients with Rupture pulmonary hydatid cysts require preoperative antibiotic therapy and supportive treatment. In our series 4 patients (8%) in group 1 and 11 patients (22%) in group 2 had postoperative complications (p = 0.008). Bronchopleural fistula or air leak most common complication in 8% of patients was significant in patients with complicated cyst group 2, two patients underwent re thoracotomy with fistula closure and decortication with good result. However, the patients with rupture cysts had higher morbidity and a longer hospital stay. Safioleas and colleagues [7] reported the hospitalization time in their patients with pulmonary hydatidosis (i.e., a 12-day median stay for intact cysts vs. a 21-day median stay for rupture or complicated cases). In our series the hospitalization times in group 1 ranged from 7 to 19 days (mean, 10 days), whereas those in group 2 ranged from 7 to 60 days (mean, 19 days) (p < 0.05). With appropriate surgical management for children with lung hydatid cyst, Overall survival are good with excellent prognosis, the operative mortality and recurrent in large series doesn't exceed 2% [30,31,33]. In our series there was no postoperative mortality in both groups, there was no recurrence in both groups during 2_5year follow up.
9. Conclusions
- Hydatid cyst affect the female more than male, the series included 72% females and 28% male.
- It was presented through all age groups but predominant in children with mean age 7 years (range, 5 to 12 years).
- Approximately 80% of the patients lived in rural areas.
- Clinical findings, chest roentgenograms, thoracic computed tomography, and thoracic ultrasonography lead to the correct preoperative diagnosis of pulmonary hydatid disease.
- Abdominal ultrasonography did for 72% of patient before operation to assess for concomitant hepatic, splenic and other Intra abdominal cysts.
- There is correlation between size of cyst and rupture, we found that increase size of cyst more liability to rupture.
- The most common symptom was cough (64%) followed by chest pain (58%) and dyspnea (38%).
- Intact hydatid cyst (54%) more than rupture cyst (46%).
- Cyst rupture more into the bronchial tree 26% and pleural space occurred in (20%) (12% patients with empyema, 4% as lung abscess, 4% as plural effusion and 4% pleural biliary fistulas).
- The surgery main way for treatment hydatid cyst lung, there were 90% posterolateral thoracotomy, 4% Right posterolateral thoracotomy + phrenotomy. 4% Right thoracotomy + abdomen incision. 2% treated by chest tube only.
- The specific surgical treatment for pulmonary hydatid cysts was cystectomy with capitonnage 60% (intact or ruptured cyst).
- Most common morbidity was found in rupture pulmonary hydatid cysts
- Most common complication post-operative is air leak (26%), mainly after rupture pulmonary hydatid cyst.
- Preoperative used albendazole for 20% of patient, one patient from that came with rupture hydatid cyst, as some series report that chemotherapy (albendazole) weaken the cystic wall thus increasing likelihood cyst rupture.
10. Recommendations
- Surgery is the safest curative treatment for pulmonary hydatid cysts in children although surgical treatment is effective in patients with intact as well as ruptures cysts for treatment of pulmonary Hydatidosis, surgical intervention before rupture of the cysts is essential.
- Regardless of whether symptoms are present, all pulmonary hydatid cysts should be surgically treated as soon as they are diagnosed in order to avoid complications.
- Medical therapy should be used sparingly in patients with pulmonary hydatidosis. This approach should only be used for patients who are high surgical risks with inoperable cysts or for preventing recurrence (10-14 mg/kg/day in cycles of 1 month).
- The objective of the surgical treatment of pulmonary hydatidosis is to eradicate the parasite, to prevent intraoperatively rupture of the cyst and subsequent dissemination, and to eliminate the residual cavity, with the maximum preservation of lung tissue.
- Prefer as a first choice of treatment lung-sparing operations such as enucleating of the cyst (Barrett's technique) or pericystectomy with closing of the bronchial openings with or without capitonnage of the pericystic space.
- The principal indications for lobectomy are large cysts involving more than 50% of the lobe, cysts with severe pulmonary suppuration not responding to preoperative treatment, multiple unilocular cysts, and sequelae of hydatid disease, such as pulmonary fibrosis, bronchiectasis, or severe hemorrhage.
- In a patient with a lung cyst larger than 4 or 5 cm in one lung and a ruptured cyst in the other lung, the intact cyst should be removed first in order to prevent its rupture. The contra lateral lesions are then resected 2 to 4 weeks after the first operation.
- Bi lateral hydatid cyst, a patient with uncomplicated cysts, the lung with the larger cyst or more numerous cysts should be approached firs.
- The most appropriate procedures for pulmonary hydatidosis are surgery either open or laparoscopy, involving removal of the cyst membrane, closure of the bronchial openings, and capitonnage. However, rupture hydatid cysts tend to cause significant pleural thickening and parenchymal destruction; therefore, more radical surgical procedures, such as decortications, segmentectomy, and lobectomy may be required in these patients.
- Marked pleural thickening due to cyst rupture into the pleural cavity is an important problem. Found for that decortication was needed.
- Rupture pulmonary hydatid cysts require preoperative antibiotic therapy and supportive treatment.
- A double-lumen end tracheal tube is used to prevent blockage of the tracheobronchial tree by the cyst contents during the operation.
- CT scanning appears to be valuable in the follow-up of patients who have had resection or evacuation of hydatid disease of the lung.
- Management of a ruptured cyst during the acute stages is mainly directed toward
- The maintenance of the airway free of secretions and cystic tissue by appropriate orotracheal suction or bronchoscopy,
- Evacuation of the hydropneumothorax.
- Treatment of anaphylactic reaction.
Declarations
Ethics Approval and Consent to Participate and Publication
Ethical Considerations and consent In this study, first we obtain verbal consent from the patients parents or relatives, giving assurance to them that the results will be used in our research without mentioning the name, or identity and a feedback was applied, and explain to them, that this research for the benefit of the community and to improve the general health of the population and help to identify the defect in health services, in order to be corrected to decrease the morbidity and mortality of lung hydatid cyst. Our study was approved by the Institutional Ethics Committee of Saudi Hospital at Hajjah. All procedures performed in the study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Availability of Data and Material
All data generated or analyzed during this study are included in this published article.
Competing Interests
The authors declare that they have no competing interests" in this section.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgements
The authors would like to acknowledge Dr Samir.A.Al kafrawy for his guidance in the statistical analysis of our data. Also like to acknowledge all nurses staff in operation rooms and surgical department for their help in the data collection.
Authors' Contributions
Burkan Nasr, made substantial contributions to the concept, design and interpretation of data. AA, GA, AA made contributions to the design, acquisition, analysis and interpretation of data. AA, MI, AT,SB,MS, YA,MS, and AH drafted the work and substantially revised it. All authors have approved the submitted version of the manuscript. All authors have agreed both to be personally accountable for their own contributions and to ensure that questions related to the accuracy or integrity of any part of the work.
References
- Ellaban A, Elzayat S, Elmuzaien M, et al. The effect of preoperative albendazole in the treatment of liver hydatid cysts. Egyptian Journal of Medical Laboratory Sciences 15 (1994): 309-319.
- Ipek Y, Mahmut ER, Bahar O et al. Surgical treatment of hydatid cyst of the lung: review of 30 cases. European Respiratory Journal 13 (1999): 441-444.
- Xanthakis D, et al. Hydatid disease of the chest: report of 91 patients surgically treated. Thorax27(1972): 517-528.
- Adrian S. Surgery of pulmonary hydatid cysts: review of 155 cases. The Journal of Thoracic and Cardiovascular Surgery62 (1971): 663-668.
- Aydm A, Yurdaku Y, Ikizler C, et al. Pulmonary hydatid disease: report of 100 patients. The Annals of thoracic surgery23 (1977): 145-151.
- Kavukcu S, Kilic D, Tokat AO, et al. ReviewParenchyma-preserving surgery in the management of pulmonary hydatid cysts. J Invest Surg 19 (2006): 61-68.
- Michael S, Misiakos EP, Dosios T, et al. Surgical treatment for lung hydatid disease. World journal of surgery23 (1999): 1181-1185.
- Guillermo R, Orduña MD A, Mariano García-yuste MD. Hydatid cyst of the lung: diagnosis and treatment. World journal of surgery25 (2001): 46.
- Todorov T, Boeva V. Echinococcosis in children and adolescents in Bulgaria: a comparative study. Annals of Tropical Medicine & Parasitology94 (2000): 135-144.
- Kalani BP, Ojha SN, Bhargava RK, et al. Hydatid disease in children in Libya. Ann Tropical Pediatr 4 (1984): 195-199.
- Ghallab, Homesh N, Alsabahi AA. Giant viable hydatid cyst of the lung: a case report. Journal of medical case reports359 (2008).
- Raul B, Varela A, Castedo E, et al. Pulmonary hydatidosis: surgical treatment and follow-up of 240 cases. European journal of cardio-thoracic surgery16 (1999): 628-635.
- Dogan R, Yüksel M, Cetin G, et al. Surgical treatment of hydatid cysts of the lung: report on 1055 patients. Thorax44 (1989): 192-199.
- Kalliopi A, Kalavrouziotis G, Loutsidis A, et al. Surgical treatment of echinococcosis by a transthoracic approach: a review of 85 cases. European journal of cardio-thoracic surgery14 (1998): 134-140.
- Petrov DB, Terzinacheva PP, Djambazov VI, et al. Surgical treatment of bilateral hydatid disease of the lung. European journal of cardio-thoracic surgery19 (2001): 918-923.
- Karaoglanoglu, Nurettin, et al. Giant hydatid lung cysts. European journal of cardio-thoracic surgery19 (2001): 914-917.
- Thomas CC. The treatment of mycotic and parasitic diseases of the chest. American Journal of Clinical Pathology(1964).
- Barrett NR, Thomas D. Pulmonary hydatid disease. British Journal of Tuberculosis and Diseases of the Chest38 (1944): 39-95.
- Talaiezadeh, Hassan A, Sharif Maraghi S. Hydatid disease in children: A different pattern than adults. Pakistan Journal of Medical Sciences22 (2006): 329.
- Aubert M, Viard P. Etude statistique sur l’hydatidose pleuropulmonaire dans le basin mediterraneen en 1982. A propos de 8,384 cas. Ann Chir37 (1983): 74-77.
- Hasan S, Ozgen G, Yüksek T, et al. Surgery in hydatid cyst of the lung: A report of 460 cases. Scandinavian journal of thoracic and cardiovascular surgery22 (1988): 101-104.
- Mutaf O, et al. Pulmonary hydatidosis in children. European journal of pediatric surgery4 (1994): 70-73.
- Balci AE, Eren N, Eren S, et al. Ruptured hydatid cysts of the lung in children: clinical review and results of surgery. The Annals of thoracic surgery74 (2002): 889-892.
- Kilani T, Ben Safta Z, Jamoussi M, et al. Pleural complications of hydatid cyst of the lung. Apropos of 16 cases. Annales de chirurgie 42 (1988).
- Faysal AS, Fahl MH, Rizk GK. Computed tomography of pulmonary hydatid disease. Journal of computer assisted tomography10 (1986): 226-232.
- von Sinner, Walther N. New diagnostic signs in hydatid disease; radiography, ultrasound, CT and MRI correlated to pathology." European journal of radiology12 (1991): 150-159.
- Biava MF, Dao A, Fortier B, et al. Laboratory diagnosis of cystic hydatic disease. World journal of surgery25 (2001): 10.
- Topçu S, Kurul IC, Tastepe I, et al. Surgical treatment of pulmonary hydatid cysts in children. The Journal of thoracic and cardiovascular surgery120 (2000): 1097-1101.
- Rajinder S D, Kalkat MS. One-stage surgical procedure for bilateral lung and liver hydatid cysts. The Annals of thoracic surgery64 (1997): 338-341.
- Alvarez AL, Téllez de Peralta G, Burgos Lázaro R, et al. Surgical treatment of pulmonary hydatidosis. The Journal of thoracic and cardiovascular surgery82 (1981): 569-575.
- Aribas OK, Kanat F, Gormus N, et al. Pleural complications of hydatid disease. The Journal of thoracic and cardiovascular surgery123 (2002): 492-497.
- Ibrahim Can K, Atilla E, Nurettin K, et al. Tension pneumothorax associated with hydatid cyst rupture. Journal of thoracic imaging17 (2002): 78-80.
- Davis A, Dixon H, Pawlowski ZS. Multicentre clinical trials of benzimidazole-carbamates in human cystic echinococcosis (phase 2). Bull World Health Organ 67 (1989): 503-508.
- Praveen A, Wali JP. Albendazole in the treatment of pulmonary echinococcosis. Thorax46 (1991): 599-600.
- Horton RJ. Albendazole in treatment of human cystic echinococcosis: 12 years of experience. Acta tropica64 (1997): 79-93.
- Gil-Grande, Lais A, et al. Randomised controlled trial of efficacy of albendazole in intra-abdominal hydatid disease. The Lancet342 (1993): 1269-1272.
- Smyth JD. In vitro studies and host-specificity in Echinococcus. Bulletin of the World Health Organization39 (1968): 5.
- Euphronia M, Schwabe CW. Host-parasite relationships in echinococcosis. The American journal of tropical medicine and hygiene11 (1962): 360-364.
- al-Hureibi AA, Amert A, al-Hureibi MA, et al. Hepatic hydatid cysts: presentation and surgical management in Yemen. J R Coll Surg Edinb 37 (1992): 229-231.
- Azazy AA, Abdelhamid AH. Indirect haemagglutination (IHA) for the diagnosis of hydatid disease in Yemen. J Egypt Soc Parasitol30 (2000): 407-411.
- Alghoury A, El-Hamshary E, Azazy A, et al. Hydatid Disease in Yemeni Patients attending Public and Private Hospitals in Sana'a City, Yemen. Oman Med J 25 (2010): 88-90.
- Saif WN. Survey of the endoparasites of stray dogs in Sana’a- republic of Yemen. Sana’a University, Faculty of Science, MSc Thesis. [Google Scholar][Ref list] Hydatid diseases still high risk in yamen Mainly Hajjah, Imran, Sana’a governorate (2001).
- Al-Shibani L, Al-Eryani SMA, Azazy AA, et al. Cases of hydatidosis in patients referred to Governmental hospitals for cyst removal in Sana’a City, Republic of Yemen. Trop Biomed29 (2012): 18r23.
- Matsaniotis N, Karpathios T, Koutoyzis J, et al. Hydatid disease in Greek children. The American journal of tropical medicine and hygiene32 (1983): 1075-1078.
- Bulent K, Gultekin G, Serdar H, et al. Analysis of Pulmonary Hydatidosis According to Their Segmentary Locations, Clinical Pulmonary Medicine 15 (2008): 8-12.
- Cangir AK, Sahin E, Enön S, et al. Surgical treatment of pulmonary hydatid cysts in children. J Pediatr Surg 36 (2001): 917-920.
- Reza MA, Razavi S, Sadeghian S. Surgical treatment of pulmonary hydatid cyst in 72 children. Tanaffos (2009): 56-61.
- Vahid M, Sokouti M, Rashidi MR. Comparison of pulmonary hydatid disease between children and adults. Tanaffos (2007): 13-18.
- Abidin S. Our results in surgical treatment of hydatid cyst of the lungs. Eur J Gen Med4 (2007): 5-8.
- Mustafa E, Gani EA. Surgical management of pulmonary hydatid cysts in children. Thorax50 (1995): 396-398.
- Ismail MT. Hydatid cysts in children. Annals of Pediatric Surgery6 (2010): 98-104.
- Prashant J, Sanghvi B, Shah H, et al. Thoracoscopic excision of mediastinal cysts in children. Journal of Minimal Access Surgery3 (2007): 123.
- Burgos L, Baquerizo A, Muñoz W, et al. Experience in the surgical treatment of 331 patients with pulmonary hydatidosis. The Journal of thoracic and cardiovascular surgery102 (1991): 427-430.
- Shamji FM, Sachs HJ, Perkins DG. Cystic disease of the lungs. Surgical Clinics of North America68 (1988): 581-620.
- Salih OK, Topcuoglu MS, Celik SK, et al. Surgical treatment of hydatid cysts of the lung: analysis of 405 patients. Canadian journal of surgery41 (1998): 131.
- Hao W, Yang W. Public health importance of cystic echinococcosis in China. Acta Tropica67 (1977): 133-145.
