Low Grade Intraventricular Haemorrhage and Five-Year School Adaptation of Very Preterm Infants
Article Information
Apprioual Géraldine1*, Rozé Jean-Christophe1, Rouger Valérie2, Gascoin Géraldine3, Nail Benallegue4 and Flamant Cyril1
1Department of Neonatology, University Hospital of Nantes, Nantes, France
2Réseau "Grandir Ensemble", University Hospital of Nantes, Nantes, France
3Department of Neonatology, University Toulouse Children’s Hospital, Toulouse, France
4Department of Pediatric Neurology, University Hospital of Nantes, Nantes, France
*Corresponding Author: Apprioual Géraldine, Department of Neonatology, University Hospital of Nantes, Nantes, France.
Received: 19 June 2023; Accepted: 20 July 2023; Published: 31 July 2023
Citation:
Apprioual Géraldine, Rozé Jean- Christophe, Rouger Valérie, Gascoin Géraldine, Nail Benallegue, Flamant Cyril. Low Grade Intraventricular Haemorrhage and Five-Year School Adaptation of Very Preterm Infants. Journal of Pediatrics, Perinatology and Child Health. 7 (2023): 134-141.
View / Download Pdf Share at FacebookAbstract
Objectives: Intraventricular haemorrhage (IVH) is a frequent morbidity in the preterm infant’s population. Low grade IVH’s impact on neurodevelopment is not clear since data on the subject is contradictory. We aimed to study the effect of low grade IVH on school outcome at 5 years of age in a very preterm population.
Study design: Infants born preterm before 33 gestational weeks (GW) with low grade IVH or no IVH and followed in the LIFT (Loire Infant Follow Up Team) cohort with a school evaluation were included in the study. At least an ultrasound screening was performed during the first week of life for all infants. The school outcome is composed of the child’s academic situation and of the teacher’s evaluation of GSA (Global School Adaptation) score at 5 years.
Results: Among the 3206 infants with no IVH or low grade IVH during their initial hospitalisation, 2045 (64%) had a school evaluation at 5 years. No statistical difference on school outcome was found in a univariate analysis between infants without IVH, those with unilateral IVH and those with bilateral IVH (p = 0.542). There was no difference either after a set of logistic regressions for infants with no IVH, unilateral and for bilateral low grade IVH.
Conclusion: Low grade IVH seems to have no significant impact on 5-year neurodevelopment and academic abilities in our very preterm infant’s population. This is an important result for clinicians and parents regarding prognosis of infants with neonatal low grade IVH.
Keywords
Intraventricular haemorrhage; Prematurity; Neurodevelopment; GSA score
Preterm infants articles Preterm infants Research articles Preterm infants review articles Preterm infants PubMed articles Preterm infants PubMed Central articles Preterm infants 2023 articles Preterm infants 2024 articles Preterm infants Scopus articles Preterm infants impact factor journals Preterm infants Scopus journals Preterm infants PubMed journals Preterm infants medical journals Preterm infants free journals Preterm infants best journals Preterm infants top journals Preterm infants free medical journals Preterm infants famous journals Preterm infants Google Scholar indexed journals Neonatology articles Neonatology Research articles Neonatology review articles Neonatology PubMed articles Neonatology PubMed Central articles Neonatology 2023 articles Neonatology 2024 articles Neonatology Scopus articles Neonatology impact factor journals Neonatology Scopus journals Neonatology PubMed journals Neonatology medical journals Neonatology free journals Neonatology best journals Neonatology top journals Neonatology free medical journals Neonatology famous journals Neonatology Google Scholar indexed journals Pediatric neurology articles Pediatric neurology Research articles Pediatric neurology review articles Pediatric neurology PubMed articles Pediatric neurology PubMed Central articles Pediatric neurology 2023 articles Pediatric neurology 2024 articles Pediatric neurology Scopus articles Pediatric neurology impact factor journals Pediatric neurology Scopus journals Pediatric neurology PubMed journals Pediatric neurology medical journals Pediatric neurology free journals Pediatric neurology best journals Pediatric neurology top journals Pediatric neurology free medical journals Pediatric neurology famous journals Pediatric neurology Google Scholar indexed journals Intraventricular haemorrhage articles Intraventricular haemorrhage Research articles Intraventricular haemorrhage review articles Intraventricular haemorrhage PubMed articles Intraventricular haemorrhage PubMed Central articles Intraventricular haemorrhage 2023 articles Intraventricular haemorrhage 2024 articles Intraventricular haemorrhage Scopus articles Intraventricular haemorrhage impact factor journals Intraventricular haemorrhage Scopus journals Intraventricular haemorrhage PubMed journals Intraventricular haemorrhage medical journals Intraventricular haemorrhage free journals Intraventricular haemorrhage best journals Intraventricular haemorrhage top journals Intraventricular haemorrhage free medical journals Intraventricular haemorrhage famous journals Intraventricular haemorrhage Google Scholar indexed journals Neonatologists articles Neonatologists Research articles Neonatologists review articles Neonatologists PubMed articles Neonatologists PubMed Central articles Neonatologists 2023 articles Neonatologists 2024 articles Neonatologists Scopus articles Neonatologists impact factor journals Neonatologists Scopus journals Neonatologists PubMed journals Neonatologists medical journals Neonatologists free journals Neonatologists best journals Neonatologists top journals Neonatologists free medical journals Neonatologists famous journals Neonatologists Google Scholar indexed journals Ventricles articles Ventricles Research articles Ventricles review articles Ventricles PubMed articles Ventricles PubMed Central articles Ventricles 2023 articles Ventricles 2024 articles Ventricles Scopus articles Ventricles impact factor journals Ventricles Scopus journals Ventricles PubMed journals Ventricles medical journals Ventricles free journals Ventricles best journals Ventricles top journals Ventricles free medical journals Ventricles famous journals Ventricles Google Scholar indexed journals Coagulation disorders articles Coagulation disorders Research articles Coagulation disorders review articles Coagulation disorders PubMed articles Coagulation disorders PubMed Central articles Coagulation disorders 2023 articles Coagulation disorders 2024 articles Coagulation disorders Scopus articles Coagulation disorders impact factor journals Coagulation disorders Scopus journals Coagulation disorders PubMed journals Coagulation disorders medical journals Coagulation disorders free journals Coagulation disorders best journals Coagulation disorders top journals Coagulation disorders free medical journals Coagulation disorders famous journals Coagulation disorders Google Scholar indexed journals Gestational age articles Gestational age Research articles Gestational age review articles Gestational age PubMed articles Gestational age PubMed Central articles Gestational age 2023 articles Gestational age 2024 articles Gestational age Scopus articles Gestational age impact factor journals Gestational age Scopus journals Gestational age PubMed journals Gestational age medical journals Gestational age free journals Gestational age best journals Gestational age top journals Gestational age free medical journals Gestational age famous journals Gestational age Google Scholar indexed journals Antenatal corticosteroid therapy articles Antenatal corticosteroid therapy Research articles Antenatal corticosteroid therapy review articles Antenatal corticosteroid therapy PubMed articles Antenatal corticosteroid therapy PubMed Central articles Antenatal corticosteroid therapy 2023 articles Antenatal corticosteroid therapy 2024 articles Antenatal corticosteroid therapy Scopus articles Antenatal corticosteroid therapy impact factor journals Antenatal corticosteroid therapy Scopus journals Antenatal corticosteroid therapy PubMed journals Antenatal corticosteroid therapy medical journals Antenatal corticosteroid therapy free journals Antenatal corticosteroid therapy best journals Antenatal corticosteroid therapy top journals Antenatal corticosteroid therapy free medical journals Antenatal corticosteroid therapy famous journals Antenatal corticosteroid therapy Google Scholar indexed journals Very low birth weight infants articles Very low birth weight infants Research articles Very low birth weight infants review articles Very low birth weight infants PubMed articles Very low birth weight infants PubMed Central articles Very low birth weight infants 2023 articles Very low birth weight infants 2024 articles Very low birth weight infants Scopus articles Very low birth weight infants impact factor journals Very low birth weight infants Scopus journals Very low birth weight infants PubMed journals Very low birth weight infants medical journals Very low birth weight infants free journals Very low birth weight infants best journals Very low birth weight infants top journals Very low birth weight infants free medical journals Very low birth weight infants famous journals Very low birth weight infants Google Scholar indexed journals Neonatal intensive care units articles Neonatal intensive care units Research articles Neonatal intensive care units review articles Neonatal intensive care units PubMed articles Neonatal intensive care units PubMed Central articles Neonatal intensive care units 2023 articles Neonatal intensive care units 2024 articles Neonatal intensive care units Scopus articles Neonatal intensive care units impact factor journals Neonatal intensive care units Scopus journals Neonatal intensive care units PubMed journals Neonatal intensive care units medical journals Neonatal intensive care units free journals Neonatal intensive care units best journals Neonatal intensive care units top journals Neonatal intensive care units free medical journals Neonatal intensive care units famous journals Neonatal intensive care units Google Scholar indexed journals Perinatal articles Perinatal Research articles Perinatal review articles Perinatal PubMed articles Perinatal PubMed Central articles Perinatal 2023 articles Perinatal 2024 articles Perinatal Scopus articles Perinatal impact factor journals Perinatal Scopus journals Perinatal PubMed journals Perinatal medical journals Perinatal free journals Perinatal best journals Perinatal top journals Perinatal free medical journals Perinatal famous journals Perinatal Google Scholar indexed journals Multiple pregnancy articles Multiple pregnancy Research articles Multiple pregnancy review articles Multiple pregnancy PubMed articles Multiple pregnancy PubMed Central articles Multiple pregnancy 2023 articles Multiple pregnancy 2024 articles Multiple pregnancy Scopus articles Multiple pregnancy impact factor journals Multiple pregnancy Scopus journals Multiple pregnancy PubMed journals Multiple pregnancy medical journals Multiple pregnancy free journals Multiple pregnancy best journals Multiple pregnancy top journals Multiple pregnancy free medical journals Multiple pregnancy famous journals Multiple pregnancy Google Scholar indexed journals Periventricular leukomalacia articles Periventricular leukomalacia Research articles Periventricular leukomalacia review articles Periventricular leukomalacia PubMed articles Periventricular leukomalacia PubMed Central articles Periventricular leukomalacia 2023 articles Periventricular leukomalacia 2024 articles Periventricular leukomalacia Scopus articles Periventricular leukomalacia impact factor journals Periventricular leukomalacia Scopus journals Periventricular leukomalacia PubMed journals Periventricular leukomalacia medical journals Periventricular leukomalacia free journals Periventricular leukomalacia best journals Periventricular leukomalacia top journals Periventricular leukomalacia free medical journals Periventricular leukomalacia famous journals Periventricular leukomalacia Google Scholar indexed journals Neurodevelopmental impairment articles Neurodevelopmental impairment Research articles Neurodevelopmental impairment review articles Neurodevelopmental impairment PubMed articles Neurodevelopmental impairment PubMed Central articles Neurodevelopmental impairment 2023 articles Neurodevelopmental impairment 2024 articles Neurodevelopmental impairment Scopus articles Neurodevelopmental impairment impact factor journals Neurodevelopmental impairment Scopus journals Neurodevelopmental impairment PubMed journals Neurodevelopmental impairment medical journals Neurodevelopmental impairment free journals Neurodevelopmental impairment best journals Neurodevelopmental impairment top journals Neurodevelopmental impairment free medical journals Neurodevelopmental impairment famous journals Neurodevelopmental impairment Google Scholar indexed journals
Article Details
Conflicts of interest:
None
1. Introduction
Very preterm infants are at risk for numerous complications during initial hospitalization. One of them is intraventricular haemorrhage (IVH), which can result in significant neurodevelopmental impairment. Whereas progress in perinatal care during the last decades have led to a decreased mortality and morbidity in this high-risk population [1], neurological complications, in particular IVH remain a major concern for neonatologists.
IVH is the most common cerebral injury identified in preterm infants, with an incidence up to 32% in the most immature population [2] and results from a subependymal germinal matrix bleeding which can rupture into the lateral ventricles [3]. This bleeding occurs mostly during the first two weeks of life. It is due to rich vascularity and vessels immaturity in this area, in addition to immature cerebrovascular autoregulation and coagulation disorders [4]. Several risk factors are well known for IVH, including gestational age (GA) and birth weight (BW) [5]. Other factors are implicated in the development of intraventricular haemorrhage, such as intrauterine infection, premature rupture of membranes, mode of delivery and absence of antenatal corticosteroid therapy [4,5].
Papile et al. [6] introduced a classification of IVH used to stratify IVH by severity. Grade I IVH is limited germinal matrix haemorrhage. Grade II IVH corresponds to intraventricular haemorrhage without ventricular dilatation. Grade III is IVH inducing ventricular dilatation and Grade IV is defined by intraventricular haemorrhage associated with intraparenchymal infarction. Grades I and II are considered as low grade IVH whereas grades III and IV are considered as high grade IVH [7].
High grade IVH is known to be a risk factor for poor neurodevelopmental outcome, during neonatal hospitalization [8] and in the long term [9]. The consequences of low grade IVH (grade I and II) are more uncertain which makes it more difficult to inform parents of very preterm infants about their prognosis in case of low grade IVH. A few studies, some of which published before the generalization of surfactant therapy, had shown an impact of low grade IVH on cognitive and school abilities compared with infants born at the same gestational age without IVH in very low birth weight infants (VLBW) population [10]. Payne et al. [11] have studied neurological outcome in a cohort of very preterm infants, comparing those with or without IVH [11]. In this study, at the age of 18 to 24 months of corrected age, no difference was found between preterm infants with low grade IVH and no IVH. In contrast, Patra et al. [12], in a cohort of 362 VLBW infants, have observed that infants with low grade IVH were more at risk for cerebral palsy, deafness and low cognitive scores compared to infants with no IVH [12]. Results of the studies conducted so far are contradictory, and very few are focused on neurodevelopmental status at school age and academic abilities.
Different tools are used to assess neurodevelopment in the preterm population. Among them, the Ages and Stages Questionnaire (ASQ) completed by parents is routinely used to assess the child in his own environment [13]. In this perspective, the Global School Adaptation (GSA) questionnaire was developed to evaluate school achievement and detect school difficulties at five years of age [14]. This easy tool is performed by the child’s teacher and has been showed to be highly consistent with full-scale IQ scores in the preterm population [14].
The large regional LIFT (Loire Infant Follow Up Team) cohort gave us the opportunity to assess the possible impact of low-grade IVH on school outcome at 5 years of age.
2. Methods
2.1 Patients and sources
In this study, we included all surviving children born before 33 gestational weeks (GW), between March 2003 and December 2014, with at least one cranial ultrasound evaluation resulting in no or low grade IVH and enrolled in the regional multicentric LIFT cohort (Pays de Loire, France).
The LIFT network includes 23 maternities of which 3 neonatal intensive care units. It allows a long term follow up for children born preterm [15] with a screening for neurodevelopmental disabilities thanks to a standard assessment.
The LIFT cohort is registered with the French data protection authority in clinical research (Commission Nationale de l’Informatique et des Libertes or CNIL, No. 851117). Written consent was obtained from parents before children were included in the cohort.
Perinatal, demographic, neonatal and socioeconomic data were prospectively collected, in particular GA, sex, BW, antenatal corticosteroids, mode of delivery, multiple pregnancy, Apgar score, the course of hospitalization and parents’ socioeconomic situation.
2.2 Cranial ultrasound evaluation
All children included in the study were evaluated by at least one cranial ultrasound, the first one was performed during the first week of life. IVH was ranked according to Papile’s classification [6]. The most severe IVH grade was considered to classify each infant, and the unilateral/bilateral character of the disease was noted. Infants suffering from other cerebral lesions, as high grade IVH or Periventricular Leukomalacia (PVL) were excluded from the study.
2.3 GSA questionnaire and school outcome
The GSA questionnaire is an assessment tool, designed to evaluate academic and behavioural skills at five years of age [14]. The assessment is performed by the child’s teacher at the age of 5 years (valid for two months either side of target age). This score has been shown to be correlated with the IQ evaluation at 5 years old in the very preterm population [14].
The GSA score is composed of twenty questions: six questions about linguistic competences, five questions about non-verbal abilities, eight questions about the child’s behaviour in class and the 20th question asks the teacher’s opinion about the child’s adaptation to upcoming classes. Each question is worth 1 to 3 points (higher mark for best result), and the total score is obtained by summing the points. It has recently been shown that a non-optimal GSA score below the cut off of 48 points is predictive of a need for educational support at the age of seven [16].
All children included in the present study had a school evaluation at the age of five. Children were considered as having an optimal school outcome if they were enrolled in the expected class for their age with no need for special educational support and if they had an optimal GSA score > 48 at five years.
2.4 Statistical analysis
Descriptive values were reported as means with standard deviations for continuous variables, and number of subjects, frequencies and percentages for categorical variables. First, the neonatal characteristics and morbidities of the assessed population were compared to those of non-assessed population to check for comparability, with test using means comparisons. Second, the same analysis was performed between children with no IVH, unilateral and bilateral IVH.
Finally, tests were used to assess the effect of IVH on school outcome and GSA score at 5 y.o. Imputations were performed on infants followed in the LIFT Cohort but without school assessment at five years to reduce missing data. Multivariate analysis using four consecutive logistic regressions models was performed on complete cases and on imputed cases to adjust for clinically relevant characteristics (GA, BW z-score, gender, socioeconomical status, obstetrical data, head circumference and weight Z-scores at discharge and post-menstrual age at discharge).
The level of statistical significance was set at p < 0.05 for all analyses performed with two-tailed tests. Analyses were performed with SPSS 17.0.
3. Results
Of the 3206 infants screened by cranial ultrasound with no haemorrhage or low grade IVH during their neonatal hospitalisation, 2528 were enrolled in LIFT cohort, of which 2045 children (64%) had a school evaluation at 5 years, and 483 children did not have a school evaluation and were therefore excluded (Figure 1).
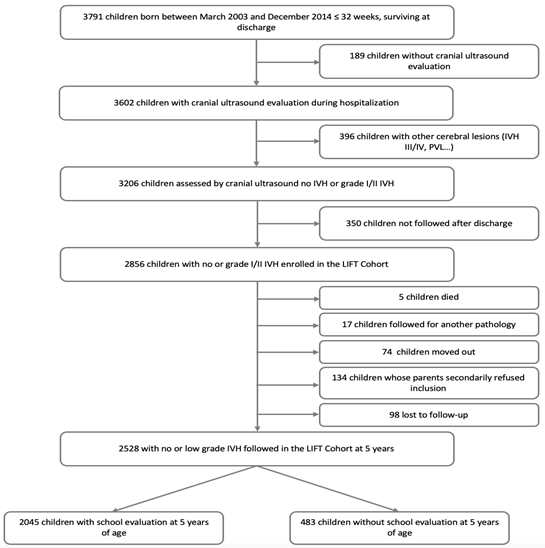
Figure1: Flow Chart.
Among the population of 3206 children with no IVH or low grade IVH, those with school evaluation at 5 years old (N = 2045) were compared with others (N = 1161) (Table 1). Children assessed at 5 years of age were born at an earlier term (29.0 vs. 29.2 GW, p = 0.023), were more likely to be born from a multiple pregnancy (32.7% vs. 27.0% p < 0.001), to have a worse respiratory outcome (p = 0.016) and a worse weight Z-score at the end of the hospitalization (-1.01 vs. -0.83, p < 0.001). These infants were also more often born in families with a high socioeconomic status (p < 0.001). There was otherwise no difference on maternal, neonatal characteristics and complications of prematurity.
Characteristics of the children included in the study were compared according to their neurological status (no IVH, unilateral low grade IVH and bilateral low grade IVH) (Table 2). As compared with the others, children with bilateral low grade IVH had a significantly lower gestational age (p < 0.001), a lower Apgar score at M5 (p = 0.004), had a longer neonatal hospitalization with a higher post-menstrual age at discharge (p = 0.014) and had a lower head circumference Z-score at discharge (p = 0.027). Infants with a unilateral low grade IVH were less likely to be born by a cesarean section (p = 0.001), had a higher birth weight z-score (p = 0.036) and had higher risk for bronchopulmonary dysplasia (p = 0.032) as compared to the others.
|
Male sex |
Assessed (N = 2045) |
Not assessed (N = 1161) |
p value |
|
1078 (52.7%) |
603 (51.9%) |
0.672 |
|
|
Gestational age, mean (weeks) ± SD |
29.0 ± 1.82 |
29.2 ± 1.80 |
0.023 |
|
Antenatal corticosteroid therapy |
1316 (64.4%) |
712 (61.3%) |
0.088 |
|
Multiple pregnancy |
668 (32.7%) |
314 (27.0%) |
< 0.001 |
|
Caesarean section |
950 (46.4%) |
512 (44.1%) |
0.198 |
|
Apgar < 7 at M5 |
197 (9.6%) |
121 (10.4%) |
0.473 |
|
Maternal hypertension |
348 (17.0%) |
202 (17.4%) |
0.783 |
|
Birth weight Z-score ± SD |
-0.18 ± 1.01 |
-0.13 ± 1.02 |
0.17 |
|
Weight Z-score at discharge ± SD |
-1.01 ± 1.04 |
-0.83 ± 1.28 |
< 0.001 |
|
Birth head circumference Z-score ± SD |
-0.08 ± 1.28 |
-0.11 ± 1.30 |
0.606 |
|
Head circumference Z-score at discharge ± SD |
-0.29 ± 1.06 |
-0.25 ± 1.11 |
0.406 |
|
Post-menstrual age at oxygenotherapy discontinuation (weeks) ± SD |
30.0 ± 2.44 |
30.1 ± 2.50 |
0.422 |
|
Post-menstrual age for exclusive enteral feeding (weeks) ± SD |
33.7 ± 3.54 |
33.7 ± 3.44 |
0.867 |
|
Post-menstrual age at discharge (weeks) ± SD |
37.8 ± 2.19 |
37.7 ± 2.30 |
0.047 |
|
Respiratory status |
|||
|
- No oxygenotherapy (O2) support |
1118 (54.7%) |
648 (55.8%) |
0.016 |
|
- O2 support < 28 days |
692 (33.8%) |
401 (34.5%) |
|
|
- O2 support > 28 days without BPD* |
176 (8.6%) |
67 (5.8%) |
|
|
- O2 support > 28 days with BPD |
59 (2.9%) |
45 (3.9%) |
|
|
Socioeconomic status |
|||
|
- High |
474 (23.2%) |
144 (12.4%) |
< 0.001 |
|
- Intermediate |
1288 (63.0%) |
782 (67.4%) |
|
|
- Low |
252 (12.3%) |
198 (17.1%) |
|
|
- Unknown |
31 (1.5%) |
37 (3.2%) |
|
|
*BPD : Bronchopulmonary dysplasia |
|||
Table 1: Neonatal characteristics and morbidities on children with a school evaluation at 5 years in comparison with those not assessed (N = 3206).
|
No IVH |
Low grade unilateral IVH |
Low grade bilateral IVH |
p value |
||
|
N = 2228 |
N = 135 |
N = 165 |
|||
|
Gestational age, mean (weeks) ± SD |
29.1 ± 1.77 |
28.5 ± 2.04 |
28.2 ± 2.10 |
< 0.001 |
|
|
Male sex |
1170 (52.5%) |
69 (51.1%) |
95 (57.6%) |
0.42 |
|
|
Antenatal corticosteroid therapy |
1446 (64.9%) |
80 (59.3%) |
105 (63.6%) |
0.401 |
|
|
Multiple pregnancy |
730 (32.8%) |
38 (28.1%) |
47 (28.5%) |
0.304 |
|
|
Caesarean section |
1067 (47.9%) |
47 (34.8%) |
64 (38.8%) |
0.001 |
|
|
Maternal hypertension |
397 (17.8%) |
16 (11.9%) |
28 (17.0%) |
0.204 |
|
|
Apgar < 7 at M5 |
194 (8.7%) |
15 (11.1%) |
27 (16.4%) |
0.004 |
|
|
Birth weight Z-score ± SD |
-0.20 ± 1.01 |
-0.02 ± 0.93 |
-0.14 ± 1.06 |
0.036 |
|
|
Weight Z-score at discharge ± SD |
-0.99 ± 1.15 |
-0.98 ± 1.04 |
-1.19 ± 0.99 |
0.082 |
|
|
Birth head circumference Z-score ± SD |
-0.09 ± 1.27 |
-0.09 ± 1.30 |
-0.11 ± 1.37 |
0.267 |
|
|
Head circumference Z-score at discharge ± SD |
-0.27 ± 1.08 |
-0.31 ± 1.14 |
-0.51 ± 0.97 |
0.027 |
|
|
Post-menstrual age at oxygenotherapy discontinuation (weeks) ± SD |
30.1 ± 2.4 |
30.2 ± 3.0 |
29.8 ± 3.3 |
0.469 |
|
|
Postmenstrual age for exclusive enteral feeding (weeks) ± SD |
33.7 ± 3.4 |
33.6 ± 3.8 |
34.0 ± 4.2 |
0.483 |
|
|
Post-menstrual age at discharge (weeks) ± SD |
37.8 ± 2.2 |
38.1 ± 2.5 |
38.3 ± 2.1 |
0.014 |
|
|
Respiratory status |
|||||
|
- No oxygenotherapy (O2) support |
1213 (54.4%) |
57 (42.2%) |
79 (47.9%) |
0.032 |
|
|
- O2 support < 28 days |
766 (34.4%) |
56 (41.5%) |
59 (35.8%) |
||
|
- O2 support > 28 days without BPD* |
180 (8.1%) |
14 (10.4%) |
18 (10.9%) |
||
|
- O2 support > 28 days with BPD |
69 (3.1%) |
8 (5.9%) |
9 (5.5%) |
||
|
Socioeconomic status |
|||||
|
- High |
495 (22.2%) 1394 (62.6%) |
35 (25.9%) |
37 (22.4%) |
0.767 |
|
|
- Intermediate |
304 (13.6%) |
79 (58.5%) |
108 (65.5%) |
||
|
- Low |
35 (1.6%) |
18 (13.3%) |
18 (10.9%) |
||
|
- Unknown |
3 (2.2%) |
2 (1.2%) |
|||
Table 2: Neonatal characteristics and morbidities of children without IVH, low grade unilateral IVH and low grade bilateral IVH (N = 2528).
Table 3 shows the impact of low grade IVH on school achievement at the age of five. In this univariate analysis, incidence of optimal school outcome was not significantly different between children with neonatal unilateral or bilateral low grade IVH and children without low grade IVH (p = 0.542) and mean for GSA score was also not different according to their neurological status (p = 0.405).
|
No IVH N = 2228 |
Low grade unilateral IVH N = 135 |
Low grade bilateral IVH N = 165 |
p value |
|
|
GSA score (mean) ± SD |
48.3 ± 8.5 |
47.5 ± 8.7 |
47.6 ± 8.4 |
0.405 |
|
Optimal school evaluation* |
1026 (57.1%) |
63 (55.8%) |
70 (52.2%) |
0.542 |
|
* Optimal school evaluation: children enrolled in the expected class for they age with no need for special educational support or optimal GSA score at 5 years (GSA score > 48) |
||||
Table 3: Impact of low grade unilateral/bilateral IVH at 5 years of age (N = 2528).
Four consecutive logistic regressions were performed on complete cases (Figure 2) and imputed cases (Figure 3). This multivariate analysis showed no statistical difference between infants with bilateral low grade IVH, unilateral low grade IVH or no IVH.
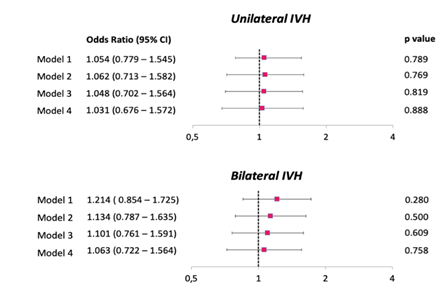
Figure 2: Multivariate analysis of the association between school outcome and unilateral/bilateral low grade IVH (complete cases). Model 1 is not adjusted. Model 2 is adjusted on GA, BW Z-score and economic status. Model 3 is adjusted on those included in model 2 and obstetrical data. Model 4 is adjusted on those included in model 3 and GA at discharge.
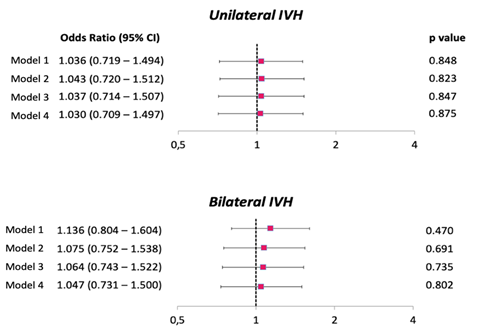
Figure 3: Multivariate analysis of the association between outcome and unilateral/bilateral low grade IVH (imputed cases). Model 1 is not adjusted. Model 2 is adjusted on GA, BW Z-score and economic status. Model 3 is adjusted on those included in model 2 and obstetrical data. Model 4 is adjusted on those included in model 3 and GA at discharge.
4. Discussion
In this large prospective French cohort of very preterm infants, we found no difference at 5 years on school difficulties between children with low grade IVH and children with normal cranial ultrasound screening during the neonatal period. These results could constitute an important element to bring to parents of very preterm infants at the time of diagnosis and may help the clinician to specify the later prognosis of infants who present a low grade intraventricular haemorrhage.
Data regarding low grade IVH in literature is controversial and most studies are targeted on neonatal outcome or short-term outcome with a 18-24 months neurodevelopmental assessment. In a recent meta-analysis by Mukerji et al. [17] comparing infants with low grade IVH to infants with no IVH, and infants with high grade IVH to infants with low grade IVH, the authors found a gradual risk for neurodevelopmental impairment at 18-24 months according to the severity of the IVH. Infants with low grade IVH were more at risk for the composite outcome of death or neurodevelopmental impairment than children with no IVH. An Australian retrospective cohort, including 332 extremely preterm infants with neonatal low grade IVH found an increased rate of neurosensory impairment (developmental delay, severe cerebral palsy or bilateral blindness) at 2 to 3 years of corrected age [18]. These studies are of interest because they provide information about neurodevelopmental outcome in case of low grade IVH neonatal diagnosis, but they are limited in time without further cognitive assessment and school adaptation.
Another recent Australian retrospective cohort by Legge et al. [19] evaluated the neurodevelopmental impact of low grade IVH on a longer term (5 and 8 years). They included 450 newborns < 30 gestational weeks, 15% of whom were diagnosed with intraventricular haemorrhage. No difference was found on Full Scale IQ at 5 years between children affected by low grade IVH and their unaffected matched peers. The 8-year evaluation did not show either any decrease in Full Scale IQ, children with low grade IVH even had better scores than their unaffected peers, which could be explained by the possible impact of early interventions on this specific population [19].
In our study, the unilateral/bilateral character of the low grade IVH did not seem to have an impact on the school outcome of the children. Infants suffering from bilateral low grade IVH had similar overall results than infants with unilateral low grade IVH and infants without IVH. While it is well known that infants with bilateral grade IV IVH have a worse outcome than unilateral grade IV IVH [20], the impact of bilateral low grade IVH compared to unilateral low grade IVH was not shown until now to the best of our knowledge.
One of the strengths of our study is related to the large population-based cohort, with an assessment at school age for more than sixty percent of the children included. The children assessed at 5 years of age were mostly similar to those not included (not assessed or lost to follow-up after their hospital discharge), except that they were born at an earlier term, had a better respiratory outcome and were less likely to be from a lower socio-economic class. Another strength of this study is the statistical analysis using multiple imputations, allowing to reduce the missing data and increasing the size of the sample. Furthermore, in this article, we showed an absence of difference between uni- or bilateral low
grade IVH, which is an information not widely discussed in the literature. However, our study is retrospective and observational with all the limitations inherent to this type of study, especially the risk of confounding factors, which was managed by a set of logistic regressions. In addition, the cranial ultrasound evaluation was not standardized, with potential differences in terms of postnatal age at the time of the cranial ultrasound, number of ultrasound evaluations during the hospital stay, and the ultrasound operator (radiologist or neonatologist), according to the different centres included in the LIFT cohort.
The neurodevelopmental assessment at the age of five allows for a more accurate evaluation than the earlier evaluation because it takes into consideration the acquisition of academic skills and analyses some behavioural and social skills. However, this evaluation is still limited since it takes place before the learning of reading and writing. There might be a benefit to extend the follow-up and evaluate infants later in childhood to screen for more subtle difficulties.
5. Conclusion
In this very preterm population, no impact of low grade IVH was found on a 5-year school outcome, both for unilateral and bilateral IVH. This is an important factor for the clinician to provide to parents of a very preterm infant diagnosed with low grade intraventricular haemorrhage. Further studies are nevertheless needed to sharpen the possible impact of each grade of intraventricular haemorrhage on neurodevelopmental outcome.
References
- Ancel PY, Goffinet F, EPIPAGE-2 Writing Group, et al. Survival and morbidity of preterm children born at 22 through 34 weeks’ gestation in France in 2011: results of the EPIPAGE-2 cohort study. JAMA Pediatr 169 (2015): 230-238.
- Stoll BJ, Hansen NI, Bell EF, et al. Neonatal Outcomes of Extremely Preterm Infants from the NICHD Neonatal Research Network. Pediatrics 126 (2010): 443-456.
- Novak CM, Ozen M, Burd I. Perinatal Brain Injury: Mechanisms, Prevention, and Outcomes. Clin Perinatol 45 (2018): 357-375.
- Ballabh P. Intraventricular hemorrhage in premature infants: mechanism of disease. Pediatr Res 67 (2010): 1-8.
- Linder N, Haskin O, Levit O, et al. Risk factors for intraventricular hemorrhage in very low birth weight premature infants: a retrospective case-control study. Pediatrics 111 (2003): e590-595.
- Papile LA, Burstein J, Burstein R, et al. Incidence and evolution of subependymal and intraventricular hemorrhage: A study of infants with birth weights less than 1,500 gm. J Pediatr 92 (1978): 529-534.
- Scott TE, Aboudi D, Kase JS. Low-Grade Intraventricular Hemorrhage and Neurodevelopmental Outcomes at 24-42 Months of Age. J Child Neurol 35 (2020): 578-584.
- Jashni Motlagh A, Elsagh A, Sedighipoor E, et al. Risk factors and short-term complications of high-grade intraventricular hemorrhages in preterm neonates in training hospitals of Alborz. Iran J Child Neurol 15 (2021): 47-55.
- Calisici E, Eras Z, Oncel MY, et al. Neurodevelopmental outcomes of premature infants with severe intraventricular hemorrhage. J Matern Fetal Neonatal Med 28 (2015): 2115-2120.
- Lowe J, Papile L. Neurodevelopmental performance of very-low-birth-weight infants with mild periventricular, intraventricular hemorrhage. Outcome at 5 to 6 years of age. Am J Dis Child 144 (1990): 1242-1245.
- Payne AH, Hintz SR, Hibbs AM, et al. Neurodevelopmental outcomes of extremely low-gestational-age neonates with low-grade periventricular-intraventricular hemorrhage. JAMA Pediatr 167 (2013): 451-459.
- Patra K, Wilson-Costello D, Taylor HG, et al. Grades I-II intraventricular hemorrhage in extremely low birth weight infants: effects on neurodevelopment. J Pediatr 149 (2006): 169-173.
- Squires J, Bricker D, Potter L. Revision of a parent-completed development screening tool: Ages and Stages Questionnaires. J Pediatr Psychol 22 (1997): 313-328.
- Boussicault G, Nguyen The Tich S, Branger B, et al. The Global School Adaptation score: a new neurodevelopmental assessment tool for very preterm children at five years of age. J Pediatr 163 (2013): 460-464.
- Hanf M, Nusinovici S, Rouger V, et al. Cohort Profile: Longitudinal study of preterm infants in the Pays de la Loire region of France (LIFT cohort). International Journal of Epidemiology 46 (2017): 1396-1397.
- Muller JB, Olivier M, Guimard P, et al. Predictive Value of the Global School Adaptation Questionnaire at 5 Years of Age and Educational Support at 7 Years of Age in Very Preterm Children. J Pediatr 226 (2020): 129-134.e1.
- Mukerji A, Shah V, Shah PS. Periventricular/Intraventricular Hemorrhage and Neurodevelopmental Outcomes: A Meta-analysis. Pediatrics 136 (2015): 1132-1143.
- Bolisetty S, Dhawan A, Abdel-Latif M, et al. Intraventricular hemorrhage and neurodevelopmental outcomes in extreme preterm infants. Pediatrics 133 (2014): 55-62.
- Legge N, Lutz T, Wocadlo C, et al. Long-term neurodevelopmental outcome in preterm infants with intraventricular haemorrhage. J Paediatr Child Health 15 (2022).
- Maitre NL, Marshall DD, Price WA, et al. Neurodevelopmental Outcome of Infants with Unilateral or Bilateral Periventricular Hemorrhagic Infarction. Pediatrics 124 (2009): e1153-1160.
