Long Term Safety Results of LASIK Refractive Surgery: A Twenty-Year Retrospective Study
Article Information
Adam L Hickenbotham1*, Morakot Tanehsakdi2, Ekktet Chansue2
1Rocky Mountain University of Health Professions, (Optometry), Provo, (Utah), USA
2TRSC International LASIK Center, Bangkok, Thailand
*Corresponding Author: Adam L Hickenbotham, Rocky Mountain University of Health Professions, (Optometry), Provo, (Utah), USA
Received: 20 February 2023; Accepted: 27 February 2023; Published: 25 August 2023
Citation: Adam L Hickenbotham, Morakot Tanehsakdi, Ekktet Chansue. Long Term Safety Results of LASIK Refractive Surgery: A Twenty- Year Retrospective Study. Journal of Surgery and Research. 6 (2023): 303-309.
View / Download Pdf Share at FacebookAbstract
Purpose: To evaluate the 20-year safety, efficacy, and satisfaction of LASIK patients treated between 1997 and 2002.
Setting: Private Practice
Design: Randomized Retrospective Study
Methods: A sample of patients who underwent LASIK between 1997 and 2002 was randomly selected during annual follow-up examinations. Study compared pre-operative refractive error and corrected distance visual acuity (CDVA) with measurements at most recent follow-up. Participants completed satisfaction questionnaires at last visit. Retreatments were performed when determined appropriate by both doctor and patient.
Results: 238 patients (468 eyes) had an initial average manifest refraction of -5.16 ±2.86 D sphere (median, -4.75 D) and -0.88 ±0.94 D cylinder (median, -0.75 D). Average manifest refraction at most recent follow-up was -0.33 ±1.08 D sphere (median, 0.00 D) and -0.47 ±0.45 D cylinder (median, -0.50 D). 92.1% of eyes achieved 20/20 or better CDVA at recent follow-up compared to 86.7% achieving 20/20 or better CDVA pre-operatively. 97.4% of participants reported satisfaction with having LASIK. Common problems included distance blur (4.7%), eye dryness (2.0%), and glare/halos (1.3%). All participants reported greater independence from glasses and greater convenience in daily life. Retreatment rate across 22 years was 31.2%.
Conclusions: After over 20 years post-treatment, LASIK refractive surgery was shown to be highly effective with a high level of safety and satisfaction. Mean CDVA was higher after 20 years post-LASIK than prior to surgery. Retreatments were commonly provided to maintain good unaided distance acuity. Overall, potential long-lasting negative side effects of LASIK, such as dryness and halos, were relatively rare.
Keywords
LASIK; Refractive Surgery; Safety; Ophthalmology
LASIK articles; Refractive Surgery articles; Safety articles; Ophthalmology articles
LASIK articles LASIK Research articles LASIK review articles LASIK PubMed articles LASIK PubMed Central articles LASIK 2023 articles LASIK 2024 articles LASIK Scopus articles LASIK impact factor journals LASIK Scopus journals LASIK PubMed journals LASIK medical journals LASIK free journals LASIK best journals LASIK top journals LASIK free medical journals LASIK famous journals LASIK Google Scholar indexed journals Refractive Surgery articles Refractive Surgery Research articles Refractive Surgery review articles Refractive Surgery PubMed articles Refractive Surgery PubMed Central articles Refractive Surgery 2023 articles Refractive Surgery 2024 articles Refractive Surgery Scopus articles Refractive Surgery impact factor journals Refractive Surgery Scopus journals Refractive Surgery PubMed journals Refractive Surgery medical journals Refractive Surgery free journals Refractive Surgery best journals Refractive Surgery top journals Refractive Surgery free medical journals Refractive Surgery famous journals Refractive Surgery Google Scholar indexed journals Ophthalmology articles Ophthalmology Research articles Ophthalmology review articles Ophthalmology PubMed articles Ophthalmology PubMed Central articles Ophthalmology 2023 articles Ophthalmology 2024 articles Ophthalmology Scopus articles Ophthalmology impact factor journals Ophthalmology Scopus journals Ophthalmology PubMed journals Ophthalmology medical journals Ophthalmology free journals Ophthalmology best journals Ophthalmology top journals Ophthalmology free medical journals Ophthalmology famous journals Ophthalmology Google Scholar indexed journals Singapore National Eye Center articles Singapore National Eye Center Research articles Singapore National Eye Center review articles Singapore National Eye Center PubMed articles Singapore National Eye Center PubMed Central articles Singapore National Eye Center 2023 articles Singapore National Eye Center 2024 articles Singapore National Eye Center Scopus articles Singapore National Eye Center impact factor journals Singapore National Eye Center Scopus journals Singapore National Eye Center PubMed journals Singapore National Eye Center medical journals Singapore National Eye Center free journals Singapore National Eye Center best journals Singapore National Eye Center top journals Singapore National Eye Center free medical journals Singapore National Eye Center famous journals Singapore National Eye Center Google Scholar indexed journals myopic patients articles myopic patients Research articles myopic patients review articles myopic patients PubMed articles myopic patients PubMed Central articles myopic patients 2023 articles myopic patients 2024 articles myopic patients Scopus articles myopic patients impact factor journals myopic patients Scopus journals myopic patients PubMed journals myopic patients medical journals myopic patients free journals myopic patients best journals myopic patients top journals myopic patients free medical journals myopic patients famous journals myopic patients Google Scholar indexed journals presbyopia articles presbyopia Research articles presbyopia review articles presbyopia PubMed articles presbyopia PubMed Central articles presbyopia 2023 articles presbyopia 2024 articles presbyopia Scopus articles presbyopia impact factor journals presbyopia Scopus journals presbyopia PubMed journals presbyopia medical journals presbyopia free journals presbyopia best journals presbyopia top journals presbyopia free medical journals presbyopia famous journals presbyopia Google Scholar indexed journals refractive changes articles refractive changes Research articles refractive changes review articles refractive changes PubMed articles refractive changes PubMed Central articles refractive changes 2023 articles refractive changes 2024 articles refractive changes Scopus articles refractive changes impact factor journals refractive changes Scopus journals refractive changes PubMed journals refractive changes medical journals refractive changes free journals refractive changes best journals refractive changes top journals refractive changes free medical journals refractive changes famous journals refractive changes Google Scholar indexed journals retinal image articles retinal image Research articles retinal image review articles retinal image PubMed articles retinal image PubMed Central articles retinal image 2023 articles retinal image 2024 articles retinal image Scopus articles retinal image impact factor journals retinal image Scopus journals retinal image PubMed journals retinal image medical journals retinal image free journals retinal image best journals retinal image top journals retinal image free medical journals retinal image famous journals retinal image Google Scholar indexed journals corneal asphericity articles corneal asphericity Research articles corneal asphericity review articles corneal asphericity PubMed articles corneal asphericity PubMed Central articles corneal asphericity 2023 articles corneal asphericity 2024 articles corneal asphericity Scopus articles corneal asphericity impact factor journals corneal asphericity Scopus journals corneal asphericity PubMed journals corneal asphericity medical journals corneal asphericity free journals corneal asphericity best journals corneal asphericity top journals corneal asphericity free medical journals corneal asphericity famous journals corneal asphericity Google Scholar indexed journals
Article Details
Background
LASIK has a history of nearly 30 years now with over 20 years of high-volume treatments being performed globally. Millions of LASIK procedures are performed each year. The first LASIK procedure was performed in 1992 and the first laser was FDA-approved by the United States for performing LASIK procedures in the United States in 1999. [8]
Despite receiving FDA-approval for safety in the United States, patients have been (and still are) advised by health care providers to delay or avoid having the LASIK procedure. The argument they are often given is that there has still not been enough data gathered on the potential long-term side-effects of having the LASIK procedure. Some suggest that the cornea may be permanently weakened by the procedure which may cause a future drop in vision due to ectasia or similar type ocular pathology which may occur suddenly and unexpectedly in old age.
Despite the hesitance by some health care providers to recommend that their patients have the procedure, approximately, 20 million LASIK procedures have been performed in the United States of America with more than twice that number in the global market [10].
The LASIK Quality of Life Collaboration Project (LQOLCP) was launched in October 2009 in the United States by the USFDA, the U.S. National Eye Institute (NEI), and the United States Department of Defense (DoD) to “help better understand the potential risk of severe problems that can result from LASIK” [9].
The study found that more than 95% of participants were satisfied with their vision following LASIK surgery with less than 1% experiencing “a lot of difficulty” because of visual symptoms after LASIK surgery (such as starburst, halos, or glare). 28% of participants reported having dry eye symptoms at 3 months post-surgery when they had no similar symptoms pre-surgery. Similarly, 40% of participants developed halos at 3 months post-operatively. Participants were also more likely to report symptoms in a questionnaire than to their health care providers [3,5].
In 2006, Reinstein and Waring asked how we can be confident about the long-term safety of LASIK without published long-term results. Various international organizations have questioned the long-term safety of LASIK and even challenged continued approval for the procedure [7].
In 2010, the Singapore National Eye Center (SNEC) published an audit of 37,932 eyes of 19,753 patients who underwent myopic LASIK between 1998 and 2007, including 275 individuals who had the procedure in 1998. Although the study began in 1998, post-operative evaluations were only reported up to 3 months after the initial procedure with a mean follow-up time of only 69 days. [11] A second similar audit of the Singapore National Eye Center (SNEC) was published in 2019 including 53,731 eyes of 27,312 patients. This time, the study covered all the years from 1998 to 2015. Like the previous study, however, the mean follow-up time was relatively short at only 78 days [2]. Both studies concluded that myopic LASIK is safe and effective with a high level of predictability. Long-term studies have generally concluded that treatments with laser refractive surgery stabilize after 3 months and remain generally stable for at least 10 years [1]. A study in the United Kingdom concluded that while 65-75% of patients who were treated for low myopia using photorefractive keratectomy (PRK) were within 1 Diopter of intended correction after 12 years, high myopic patients treated with PRK only had 22-25% of patients within 1 Diopter of intended correction after 12 years. Additionally, 12% of patients had persistent nighttime halos and 3% had dry eyes [6]. In a more recent study conducted at three Department of Veteran Affairs hospital sites, long-term post-operative data was available from 4 to 17 years post-operatively for 80 patients who underwent LASIK (15%) and PRK (85%). At their post-operative examination (range 3–14 months, mean 4 months), 82% of patients had uncorrected visual acuity (UDVA) of 20/20 or better, and their average manifest refraction was −0.08 D (SD ± 0.48 D). At the time of the long-term post-operative examination (range 4–11 years, mean of 8.2 years), 49% of patients had an UDVA of 20/20 or better and an average manifest refraction was −0.64 D (SD ± 0.69 D) [4]. Despite the excellent track record of LASIK with millions of satisfied customers, there are still individuals who consider LASIK to be unpredictable across the life of a patient and warn against having the procedure. This study will evaluate a longer period of follow-up (mean time of 21.4 ±1.25 years) to determine the safety, efficacy, and satisfaction of LASIK refractive surgery.
Methods
From 1997 to 2002, 8,686 patients (17,043 eyes) had LASIK refractive surgery at TRSC International LASIK Center in Bangkok, Thailand. Of these original patients, 1,923 individuals (3,762 eyes) or 22.4% of patients returned for their annual follow-up examination approximately twenty years since their first surgery was completed. Due to time constraints and limited personnel, a smaller number of participants (238 patients, 468 eyes) was randomly selected to be part of the study and complete the satisfaction questionnaire and have their data analyzed for safety and efficacy of the LASIK procedure. Although the LASIK procedures were performed by six different surgeons employed by the surgical center during that period, the majority (86.8%) were performed by the founding surgeon, Ekktet Chansue, M.D. At each annual visit, including the initial visit, participants are given an ocular health examination as well as refractive and vision testing. Pre-operative and post-operative refractive errors, uncorrected distance visual acuities (UDVA), and corrected distance visual acuities (CDVA) were recorded at each visit. The randomly selected participants for this study were also given a satisfaction questionnaire that they completed at the most recent visit.
LASIK retreatments are performed at no cost to the patient (except for the price of medications) if, after consultation with the doctor, it is determined that the additional procedure would be safe and effective in improving the patient’s visual needs. All retreatments are tracked in the patients’ electronic medical records. Retreatments may be performed for either blurred vision due to refractive changes or near vision blur due to presbyopia. Medical records were kept in an electronic database which is password protected and only accessible at the clinical site. Data was entered at the time measurements were taken and were reviewed for accuracy prior to analysis.
Results
The mean age of the participants at the time of study was 56.7 ±7.9 years with the youngest participant being 37 years old and the oldest being 84. Participants’ median age was 35 years (mean, 35.3±7.8 years) at the time of the initial LASIK surgery. There were 58 males (24.3%) and 180 females (75.7%) who were randomly selected from among the 1,923 patients who returned for an annual follow-up examination and had their initial LASIK surgery between 1997 and 2002. Mean follow-up time since the initial surgery was 21.4 years (mean, 21.4 ±1.25 years). The mean initial manifest refraction was -5.16 ±2.86 diopters sphere (median, -4.75 D) with -0.88 ±0.94 diopters cylinder (median, -0.75 D). Mean manifest refraction at last follow-up was -0.33 ±1.08 diopters sphere (median, 0.00 D) and -0.47 ±0.45 diopters cylinder (median, -0.50 D).
Corrected Distance Visual Acuity (CDVA)
92.7% of eyes achieved 20/20 or better CDVA at last follow-up compared to 86.8% achieving 20/20 or better CDVA prior to having LASIK. 65.6% of treatments resulted in 1 or more lines of improvement in CDVA at last follow-up compared to 6.2% of treatments resulting in 1 or more lines loss in CDVA. The charts 1-3 below shows the change in CDVA from the pre-operative examination until the last follow-up grouped by manifest refraction. Participants with higher levels of myopia prior to LASIK demonstrated slightly more improved CDVA due to retinal image magnification although they were also at highest risk for reduced CDVA due to potential haze and increases in corneal asphericity. On average, all groups had an average increase in CDVA at last follow-up.
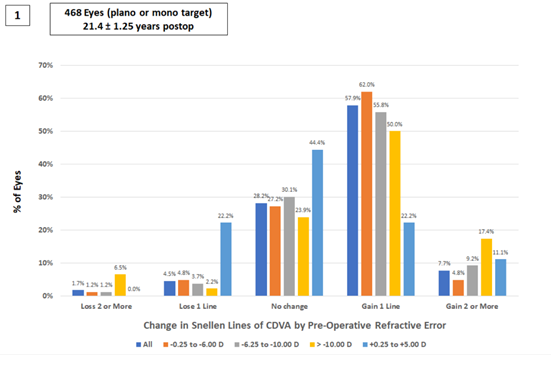
Chart 1: The percentage of participants who had various levels of change in CDVA (Loss of more than 1 line, loss of 1 line, no change, gain 1 line, or gain more than 1 line) at their last follow up (21.4 ±1.25 years after LASIK) grouped by manifest refraction prior to LASIK surgery.
Uncorrected Distance Visual Acuity (UDVA)
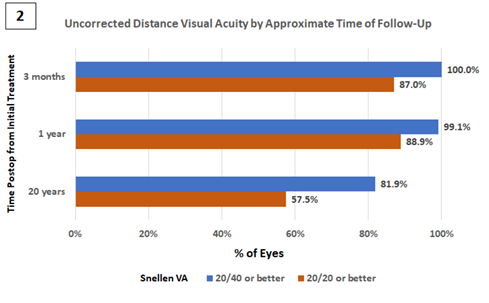
Chart 2: The percentage of participants with an uncorrected distance visual acuity (UDVA) of either “20/20 or better” or “20/40 or better” grouped by the approximate time postop from the initial LASIK surgery. The percent of eyes achieving 20/40 or better unaided visual acuity (UDVA) at the most recent follow-up after approximately 20 years was 81.9% (including retreatments), with 57.5% achieving 20/20 or better. As a comparison, the percent of eyes achieving 20/40 or better unaided visual acuity (UDVA) at the 3-month follow-up was 100%, with 87% achieving 20/20 or better and the percent of eyes achieving 20/40 or better unaided visual acuity (UDVA) at the 1-year follow-up was 99.1%, with 88.9% achieving 20/20 or better.
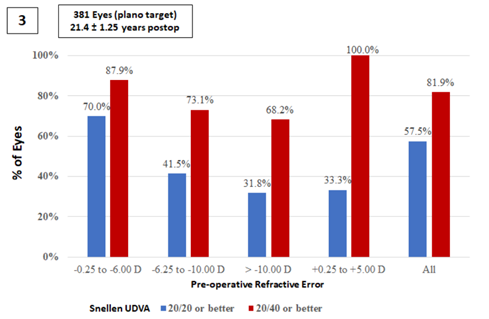
Chart 3: The percentage of participants grouped by pre-operative manifest refraction who demonstrated UDVA of either “20/20 or better” or “20/40 or better” at their last visit. As seen in the chart above patients who had higher levels of myopia prior to initial treatment were more likely to experience myopic regression and reduced UDVA at the last follow-up. 70 percent of participants who had less than -6.00 D of myopia had a UDVA of 20/20 or better at the last follow-up compared to 31.8 percent of patients with greater than -10.00 D of myopia.
Retreatment
146 of the 468 eyes underwent retreatment between 1998 and 2020, with an overall retreatment rate across 22 years of 31.2%. Of these retreatments, 124 eyes were treated for myopic regression (26.5%) and the remaining 22 eyes (4.7%) were treated for the onset of presbyopia with a monovision correction.
Satisfaction
The reported overall final satisfaction after approximately 20 years was 97.4% (225 out of the 231 participants who responded to this question). Only a single participant reporting regret for having done the initial LASIK procedure (out of 234 who responded). The patient who expressed regret for having had the procedure originally was found to have substantial myopic regression over time (pre-op manifest refraction of -6.50 DS compared to a final manifest refraction of -4.00 DS at the last visit approximately 23 years later). The most common vision problems reported by participants as part of the questionnaire were distance blur (4.7%), eye dryness (2%), and glare/halos (1.3%). All participants (236 of 236 responses) reported moderate to high levels of independence from glasses as well as greater convenience in routine daily life and extracurricular activities.
Discussion
Inclusion in the study required that patients return for an eye exam approximately 20 years after the initial LASIK treatment. This requirement makes it uncertain whether the study group would be an accurate representation of all 8,686 patients who had LASIK from 1997 to 2002. As part of the questionnaire, patients were asked if they considered yearly eye exams to be important. The responses on the questionnaire were nearly unanimous (233 out of 234 responses) that participants considered yearly eye exams to be important. It is likely that patients who did not consider eye exams to be important, would not be returning for an eye exam 20 years after having LASIK. This additional factor may demonstrate a difference between all LASIK patients and those patients who were included in this study. It is, however, unknown whether patient who continue to return for eye exams would have better or worse results than those who do not return. One theory would hold that patients who do not return to see their eye doctor are seeing well enough and therefore feel that they have no reason to have an eye examination. Another theory might be that patients who are concerned for the health of their eyes are more likely to consider eye exams important and therefore maintain better care of their eyes and vision. In this case, returning patients might see better overall than patients who do not return.
A further study could determine which of these two hypotheses is more likely. If a second group of patients who had LASIK between 1997 and 2002 could be persuaded to return, their data could be compared with the data from this study. This comparison would be particularly interesting if the second group expressed less importance to having yearly eye exams. Another factor to consider is that TRSC International LASIK Center provides LASIK retreatments at no cost to the patient, except for medication fees. After consultation with the doctor, if it is decided that a LASIK retreatment is safe and has a high likelihood of improving the patient’s vision, the center will perform a LASIK retreatment. This willingness to perform retreatments has resulted in a retreatment rate of 31.2% for the patients in this study who have had their initial LASIK treatment over 20 years ago. It should be noted that 22 of the 146 eyes were being treated with monovision as a method of relieving symptoms of presbyopia. While it is not known whether the patients who did not return for their annual eye exams had a similar rate of myopic regression, these results are similar to those reported by the Department of Veteran Affairs in which 82% of patients saw 20/20 or better at approximately the 1-year mark versus 49% of patients seeing 20/20 or better approximately 8 years later. In this study, 88.9% of patients were seeing 20/20 or better at the 1-year mark and 57.5% of patients were seeing 20/20 or better at the 21-year mark. If more patients could be persuaded to return and have their annual eye exam and those patients were in a group which had not chosen to have a retreatment, it could be determined if myopic regression was a less common occurrence than this study would indicate. Participants were measured to have a mean manifest refraction of -0.33 ±1.08 diopters sphere (median, 0.00 D) and -0.47 ±0.45 diopters cylinder (median, -0.50 D) 20 years or more after their initial LASIK. These numbers include individuals who have had retreatments so the actual amount of regression would be higher if no retreatments had been performed. Even with retreatments, the loss in unaided visual acuity was significant. One year following initial treatment, 88.9% were seeing 20/20 or better. By 20 years, only 57.5% were still seeing 20/20 or better. Any loss in unaided acuity over the twenty-year timespan is most commonly refractive changes rather than pathological changes. Twenty years following LASIK surgery, the best corrected visual acuities of patients were on average the same or better than they were pre-treatment. In fact, 65.6% of study patients had a better CDVA than they did prior to surgery. Some of this improvement could be attributed to a reduction in the refractive spectacle minification that would follow high myopia LASIK treatments. A patient with a -8.00 D prescription could expect a full line of improvement in Snellen acuity due to retinal image magnification in comparison to wearing glasses. Improvements in LASIK technology, including smaller spot sizes, more advanced eye tracking systems, newer flap-making techniques, as well as improved nomograms for laser patterns (including wavefront treatments), have resulted in improved results over the last two decades. It would be unfair to compare the accuracy of LASIK technology from 1997 to that of 2021. The experience of the surgeons has also increased significantly during that time and patients are better selected for those who would most likely benefit from having the LASIK procedure. Finally, it would be important to understand if the high level of satisfaction in the study (97.4%) is similar among individuals who did not return for follow-up. This number (97.4%) is very similar to the percentage found in the LASIK Quality of Life Collaboration Project (95%) which would indicate that even after 20 years, there is very little reduction in patient satisfaction even when unaided visual acuities have reduced over time. Particularly noteworthy is the unanimous response given by the participants in this study indicating a greater level of convenience that comes from increased independence from glasses and contact lenses. While it could be expected that independence from glasses would decrease over time due to either myopic regression or the onset of presbyopia, these changes might be minor compared to the relatively high level of myopia that was experienced by many of the participants prior to LASIK surgery. Myopic regression might also coincide with the onset of presbyopia therefore providing improved near vision. This might lead to continued patient satisfaction with the procedure despite experiencing a gradual blur in the distance vision.
Conclusions
LASIK refractive surgery is determined to be a highly effective long-lasting surgical method for correcting vision and reducing the need for glasses or contact lenses with a high level of safety and satisfaction. It is very rare for someone to express regret for having had LASIK. LASIK patients should not expect to have uncorrected vision of 20/20 or better indefinitely due to the changes that can occur over time, most commonly myopic regression and/or presbyopia. LASIK patients can expect to have greater independence from glasses and greater convenience in life activities even 20 years or more following their initial surgery.
Value Statement
WHAT WAS KNOWN
- Published data consistently shows that LASIK refractive surgery is safe and effective with a high level of patient satisfaction.
- The majority of published papers for LASIK refractive surgery results contain 1 to 3 years of follow-up data and there is a scarcity of data beyond 10 years.
WHAT THIS PAPER ADDS
- This paper provides LASIK surgery results for patients after approximately 20 years from their initial procedure.
LASIK surgery retains its safety and high patient satisfaction after 2 decades
Statements & Declarations
Dr. Adam Hickenbotham is the Dean of the College of Optometry at Rocky Mountain University of Health Professions in Provo, Utah, USA. Dr. Ekktet Chansue is the medical director and chief surgeon of TRSC International LASIK Center. He is an unpaid investigator for Carl Zeiss Meditec but has received travel reimbursements. He has no other financial or proprietary interest in any of the material or methods mentioned. All other authors have no financial or proprietary interest in any of the material or methods mentioned in this study.
Disclosure of public and private support and competing interests
The authors have no other relevant financial or non-financial interests to disclose other than those above.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Authors’ contributions
All authors were involved in the design, analysis, or interpretation of data as well as the manuscript drafting, critical revision, and final approval. The first draft of the manuscript was written by Adam Hickenbotham and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Authors’ information
Adam Hickenbotham, O.D., M.P.H., Ph.D. is the Founding Dean of the Rocky Mountain University of Health Professions in Provo, Utah, USA. He earned a Doctor of Optometry degree and a master’s degree in Public Health from University of California, Berkeley. He also received a Ph.D. in Bioengineering from a joint program with University of California, Berkeley and University of California, San Francisco. Dr. Hickenbotham graduated from Harvard Medical School’s 1-Year Post-Graduate Medical Education Surgical Leadership Program. He also completed the Clinical Research Conduct and Management Program as well as the Clinical Scientist Development Program from University of California, Berkeley.
Morakot Tanehsakdi, O.D., earned a Doctor of Optometry degree from University of California, Berkeley. Dr. Tanehsakdi has been co-managing refractive surgery patients since 2003.
Ekktet Chansue, M.D. is the Medical Director of TRSC International LASIK Center in Bangkok, Thailand. After his Cornea, External Disease & Refractive Surgery fellowship in St. Louis, MO, in 1993, he taught at the Ramathibodi Hospital Faculty of Medicine, Mahidol University, Bangkok, Thailand, for several years. He performed the first LASIK in Thailand in 1994, and has since performed more than 30,000 LASIK procedures. Dr. Chansue also performed the first ReLEx® SMILE in Thailand in 2010. He designed the Chansue ReLEx® Dissector, an instrument to aid in the separation and freeing the lenticule during the ReLEx® procedure (NFI).
Ethics Approval
This study was performed in line with the principles of the Declaration of Helsinki. This is a retrospective study with no identifying data or details for individual patients. The Institutional Review Board at Rocky Mountain University of Health Professions has confirmed that no ethical approval is required.
Consent to participate
Informed consent was obtained from all individual participants whose data is included in this study as part of their treatment. They were informed that no individual details would be provided.
Consent to publish
The authors affirm that human research participants provided informed consent for publication of research from data obtained from their treatments. If identifying information were to be published, further informed consent would be obtained.
References
- Alió JL, Muftuoglu O, Ortiz D, et al. (2008) Ten-year follow-up of laser in situ keratomileusis for myopia of up to -10 diopters. American journal of ophthalmology 145 (2008): 46-54.
- Chua D, Htoon HM, Lim L, et al. Eighteen-year prospective audit of LASIK outcomes for myopia in 53 731 eyes. British Journal of Ophthalmology 103 (2019): 1228-1234.
- Eydelman MB, Tarver ME, Ferris F. Listening to the Patients - The Laser-Assisted In Situ Keratomileusis Quality of Life Collaboration Project. JAMA ophthalmology 135 (2017): 83-84.
- Godiwalla RY, Magone MT, Kaupp SB, et al. Long-term outcomes of refractive surgery performed during the military. Military medicine 184 (2019): e808-812.
- Hays RD, Tarver ME, Spritzer KL, et al. Assessment of the psychometric properties of a questionnaire assessing patient-reported outcomes with laser in situ keratomileusis (PROWL). JAMA ophthalmology 135 (2017): 3-12.
- Rajan MS, Jaycock P, O'Brart D, et al. A long-term study of photorefractive keratectomy: 12-year follow-up. Ophthalmology 111 (2004): 1813-1824.
- Reinstein DZ, Waring III GO. Have you seen the 10-year long-term safety data on LASIK?. Journal of Refractive Surgery 22 (2006): 843.
- Stuart A. A look at LASIK past, present, and future. American academy of ophthalmology (2009).
- United States Food and Drug Administration. LASIK quality of life collaboration project (2018).
- Watson S. Twenty Years Later, LASIK has its pros and cons. WebMD (2019).
- Yuen LH, Chan WK, Koh J, et al. SingLasik Research Group. A 10-year prospective audit of LASIK outcomes for myopia in 37932 eyes at a single institution in Asia. Ophthalmology 117 (2010): 1236-1244.
