Levels of Anxiety and Depression amongst the Frontline Healthcare Workers of COVID-19: A Cross-Sectional Survey with Follow-Up
Article Information
Iftekhar Ahmed1, Muhammad Sohaib Asghar2,*, Sadia Iqbal3, Salma Salman3, Maira Hassan4, Uzma Rasheed4, Mohammed Akram4, Muhammad Saleem5, Ibraj Fatima6, Marium Batool Abbas6
1Professor of Medicine at Dow University Hospital, Dow University of Health Sciences, Karachi, Pakistan
2Resident Physician of Internal Medicine at Dow University Hospital, Dow University of Health Sciences, Karachi, Pakistan
3Assistant Professor of Medicine at Dow University Hospital, Dow University of Health Sciences, Karachi, Pakistan
4Intern of Internal Medicine at Liaquat National Hospital and Medical College, Karachi, Pakistan
5Department of Psychology, Dow University of Health Sciences, Karachi, Pakistan
6Doctoral Student of Dow International Medical College, Dow University of Health Sciences, Karachi, Pakistan
*Corresponding Author: Dr. Muhammad Sohaib Asghar, Resident Physician of Internal Medicine at Dow University Hospital, Dow University of Health Sciences, Karachi, Pakistan
Received: 08 July 2020; Accepted: 16 July 2020; Published: 24 August 2020
Citation: Iftekhar Ahmed, Muhammad Sohaib Asghar, Sadia Iqbal, Salma Salman, Maira Hassan, Uzma Rasheed, Mohammed Akram, Muhammad Saleem, Ibraj Fatima, Marium Batool Abbas. Levels of Anxiety and Depression amongst the Frontline Healthcare Workers of COVID-19: A Cross-Sectional Survey with Follow-Up. Journal of Psychiatry and Psychiatric Disorders 4 (2020): 270-284.
View / Download Pdf Share at FacebookAbstract
Purpose of the study: Outbreaks of infectious diseases are known to have significant psychological effects not only on the general population but on health care workers as well. The COVID-19 pandemic also has been a challenge for Healthcare workers across the globe when it comes to their mental health.
Study design: This is an observational cross-sectional study, carried out amongst the frontline doctors of COVID-19 units, by a well-structured questionnaire using Google Forms. The two scales used measure anxiety and depression among the healthcare workers were the Hamilton anxiety scale (HAM-A), and the hospital anxiety and depression scale (HADS).
Results: The mean age of all the participants in the study was 25.40 ± 1.61, including 57% house officers/interns and 43% medical residents/postgraduate trainees. Both the anxiety and depression scales were significantly higher in house officers as compared to their senior doctors (residents/postgraduate trainees). According to HAM-A, 62% of respondents were in the mild category, 20% mild to moderate, 5% moderate to severe, while 14 respondents (13%) were in severe anxiety category. The HAM-A (P=0.078) and HADS for anxiety was significantly higher in females (P=0.001), while HADS for depression was statistically indifferent among the gender. The means of all scales got improved after the postings in Corona wards. The duration of practice also had an inverse correlation observed with all the studied scales.
Conclusion: Depression and anxiety were seen quite higher in our population of health care workers with significant improvements that were observed after completing the rotations of corona units.
Keywords
Anxiety; Depression; Healthcare workers; Coronavirus; COVID-19; Pandemic; Mental health
Anxiety articles, Depression articles, Healthcare workers articles, Coronavirus articles, COVID-19 articles, Pandemic articles, Mental health articles
Anxiety articles Anxiety Research articles Anxiety review articles Anxiety PubMed articles Anxiety PubMed Central articles Anxiety 2023 articles Anxiety 2024 articles Anxiety Scopus articles Anxiety impact factor journals Anxiety Scopus journals Anxiety PubMed journals Anxiety medical journals Anxiety free journals Anxiety best journals Anxiety top journals Anxiety free medical journals Anxiety famous journals Anxiety Google Scholar indexed journals Depression articles Depression Research articles Depression review articles Depression PubMed articles Depression PubMed Central articles Depression 2023 articles Depression 2024 articles Depression Scopus articles Depression impact factor journals Depression Scopus journals Depression PubMed journals Depression medical journals Depression free journals Depression best journals Depression top journals Depression free medical journals Depression famous journals Depression Google Scholar indexed journals Healthcare workers articles Healthcare workers Research articles Healthcare workers review articles Healthcare workers PubMed articles Healthcare workers PubMed Central articles Healthcare workers 2023 articles Healthcare workers 2024 articles Healthcare workers Scopus articles Healthcare workers impact factor journals Healthcare workers Scopus journals Healthcare workers PubMed journals Healthcare workers medical journals Healthcare workers free journals Healthcare workers best journals Healthcare workers top journals Healthcare workers free medical journals Healthcare workers famous journals Healthcare workers Google Scholar indexed journals Coronavirus articles Coronavirus Research articles Coronavirus review articles Coronavirus PubMed articles Coronavirus PubMed Central articles Coronavirus 2023 articles Coronavirus 2024 articles Coronavirus Scopus articles Coronavirus impact factor journals Coronavirus Scopus journals Coronavirus PubMed journals Coronavirus medical journals Coronavirus free journals Coronavirus best journals Coronavirus top journals Coronavirus free medical journals Coronavirus famous journals Coronavirus Google Scholar indexed journals COVID-19 articles COVID-19 Research articles COVID-19 review articles COVID-19 PubMed articles COVID-19 PubMed Central articles COVID-19 2023 articles COVID-19 2024 articles COVID-19 Scopus articles COVID-19 impact factor journals COVID-19 Scopus journals COVID-19 PubMed journals COVID-19 medical journals COVID-19 free journals COVID-19 best journals COVID-19 top journals COVID-19 free medical journals COVID-19 famous journals COVID-19 Google Scholar indexed journals Pandemic articles Pandemic Research articles Pandemic review articles Pandemic PubMed articles Pandemic PubMed Central articles Pandemic 2023 articles Pandemic 2024 articles Pandemic Scopus articles Pandemic impact factor journals Pandemic Scopus journals Pandemic PubMed journals Pandemic medical journals Pandemic free journals Pandemic best journals Pandemic top journals Pandemic free medical journals Pandemic famous journals Pandemic Google Scholar indexed journals Mental health articles Mental health Research articles Mental health review articles Mental health PubMed articles Mental health PubMed Central articles Mental health 2023 articles Mental health 2024 articles Mental health Scopus articles Mental health impact factor journals Mental health Scopus journals Mental health PubMed journals Mental health medical journals Mental health free journals Mental health best journals Mental health top journals Mental health free medical journals Mental health famous journals Mental health Google Scholar indexed journals Severe acute respiratory syndrome coronavirus 2 articles Severe acute respiratory syndrome coronavirus 2 Research articles Severe acute respiratory syndrome coronavirus 2 review articles Severe acute respiratory syndrome coronavirus 2 PubMed articles Severe acute respiratory syndrome coronavirus 2 PubMed Central articles Severe acute respiratory syndrome coronavirus 2 2023 articles Severe acute respiratory syndrome coronavirus 2 2024 articles Severe acute respiratory syndrome coronavirus 2 Scopus articles Severe acute respiratory syndrome coronavirus 2 impact factor journals Severe acute respiratory syndrome coronavirus 2 Scopus journals Severe acute respiratory syndrome coronavirus 2 PubMed journals Severe acute respiratory syndrome coronavirus 2 medical journals Severe acute respiratory syndrome coronavirus 2 free journals Severe acute respiratory syndrome coronavirus 2 best journals Severe acute respiratory syndrome coronavirus 2 top journals Severe acute respiratory syndrome coronavirus 2 free medical journals Severe acute respiratory syndrome coronavirus 2 famous journals Severe acute respiratory syndrome coronavirus 2 Google Scholar indexed journals personnel protection equipment articles personnel protection equipment Research articles personnel protection equipment review articles personnel protection equipment PubMed articles personnel protection equipment PubMed Central articles personnel protection equipment 2023 articles personnel protection equipment 2024 articles personnel protection equipment Scopus articles personnel protection equipment impact factor journals personnel protection equipment Scopus journals personnel protection equipment PubMed journals personnel protection equipment medical journals personnel protection equipment free journals personnel protection equipment best journals personnel protection equipment top journals personnel protection equipment free medical journals personnel protection equipment famous journals personnel protection equipment Google Scholar indexed journals hospital anxiety and depression scale articles hospital anxiety and depression scale Research articles hospital anxiety and depression scale review articles hospital anxiety and depression scale PubMed articles hospital anxiety and depression scale PubMed Central articles hospital anxiety and depression scale 2023 articles hospital anxiety and depression scale 2024 articles hospital anxiety and depression scale Scopus articles hospital anxiety and depression scale impact factor journals hospital anxiety and depression scale Scopus journals hospital anxiety and depression scale PubMed journals hospital anxiety and depression scale medical journals hospital anxiety and depression scale free journals hospital anxiety and depression scale best journals hospital anxiety and depression scale top journals hospital anxiety and depression scale free medical journals hospital anxiety and depression scale famous journals hospital anxiety and depression scale Google Scholar indexed journals
Article Details
1. Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has been identified to be a causative pathogen for the coronavirus disease 2019 (COVID-19) [1]. This disease was known to emerge in Wuhan, China, and gradually spread across the globe and the WHO declared in March of this year that COVID-19 as pandemic [1].
Outbreaks of infectious diseases are known to have significant psychological effects not only on the general population but on health care workers as well [2]. An example of this is psychological ramifications noted during the SARS outbreak, where studies documented the acute stress reactions experienced by healthcare workers [2]. Evidence from previous studies conducted during the Ebola and SARS outbreaks showed that healthcare workers (HCWs) were likely to suffer from adverse psychological conditions, such as anxiety, fear, and stigmatization [1].
Healthcare workers are subjected to increased amounts of stress during this pandemic [3]. This is due to the very nature of their jobs, such as direct contact and treatment of infected patients [3]. This raises fear for the contraction of the pathogen, the risk of transmitting the virus to their families and working under great pressure because of the increased patient load [3]. The rise in the number of cases, deaths, increased workloads, and exhaustion of personnel protection equipment (PPE) also adds to the psychological stress [3]. Many HCWs have also been reassigned to work within COVID-19 units outside of their usual medical specialties and expertise to manage the huge workload and patient volume. [4] In New York City, HCWs taking care of COVID-19 patients have been reported to commit suicide [4].
Apart from the physical and pathological effects of diseases on the human body, a few symptoms can be attributed to the psychological sequelae of these infectious disease outbreaks [2]. Such symptoms have been noted in the Ebola and SARS virus outbreaks [2]. Studies have reported 10% of HCWs reported having anxiety, feeling depressed, and somatization as a result of working during such outbreaks [3]. A recent Chinese study found that depression, stress-related symptoms, and anxiety were prevalent in 50.7%, 44.7%, and 73.4% respectively of their HCWs [3].
The COVID-19 pandemic has been a challenge for the HCWs across the globe when it comes to their mental health, and the situation seen in Pakistan is no different. Unfortunately, there is a dearth of data regarding the mental health, anxiety, and stress levels being faced by the frontline healthcare workers in the country. This study aims to assess the levels of depression and anxiety among the young HCWs working in corona units of tertiary care hospitals in Pakistan and to compare them with respect to their gender, professional rank, and duration of practice, while the secondary objective was to assess whether those levels of anxiety get better or worse after working in those units.
2. Methodology
This is an observational cross-sectional study, carried out amongst the doctors of Dow University Hospital, and Liaquat National Hospital, Karachi, Pakistan. A well-structured questionnaire was administered by using Google Forms and was made available online (https://forms.gle/1rfD3Z2uJ9usa47R8) [5]. Before our questionnaire, a consent form was attached to allow the use of collected data. The questionnaire consisted of 2 parts, the first being demography (name, age, professional rank, duration of practice, hospital affiliation, etc.) while second part including 2 scales to measure anxiety and depression among the healthcare workers including Hamilton anxiety scale [6], and the hospital anxiety and depression scale (HADS) [7]. There were 27 questions in total, 13 belonged to the Hamilton anxiety scale, while 7 belonged to anxiety assessment and the other 7 to depression assessment by HADS. Each question had 5 responses in Hamilton anxiety scale ranging from not present to severe, while 4 varying responses in HADS, and participants were asked to choose one amongst them. The study participants included were Healthcare workers, that is, postgraduate trainee/medical residents or house officers/interns who were posted specifically in Corona isolation wards and Intensive care units. All those who haven’t worked in Corona related units were excluded from the study. The questionnaire link was then circulated among the healthcare workers through social media platforms (WhatsApp) and was asked to fill before or during their postings in corona units. The bias of receiving irrelevant (non-COVID working doctors) responses was reduced by posting the questionnaire on COVID-doctors’ group only. The participants who completed their postings in corona units were then asked again to fill the questionnaire to compare their anxiety levels before and after working in corona units.
A sample size of 109 was calculated by using OpenEpi sample size calculator [8], in which we used 5% as a margin of error, 95% as confidence interval (CI), 150 as population size and anticipated frequency of outcome factor in the population of 50%. The responses were gathered through a convenient sampling method until the sample size was met. The response percentage of each question has been shown in (Figure 1). The responses were then put into the Hamilton anxiety scale calculator from MDCalc [9] and the HADS calculator from the BGP article [10]. The responses of the study participants were then compared amongst gender, professional rank, and duration of practice. All the analysis was conducted by using the Statistical Package for Social Science (SPSS) version 25.0 (IBM Corp, Chicago, IL, USA). A p-value of <0.05 was considered statistically significant (two-tailed). Chi-square and Fisher exact tests were used respectively to calculate qualitative measures according to the limitation of data, while McNemar Bowker’s test was used for repeated measures. An independent sample t-test was used to estimate quantitative measures amongst the study groups while paired sample t-test for repeated ones.
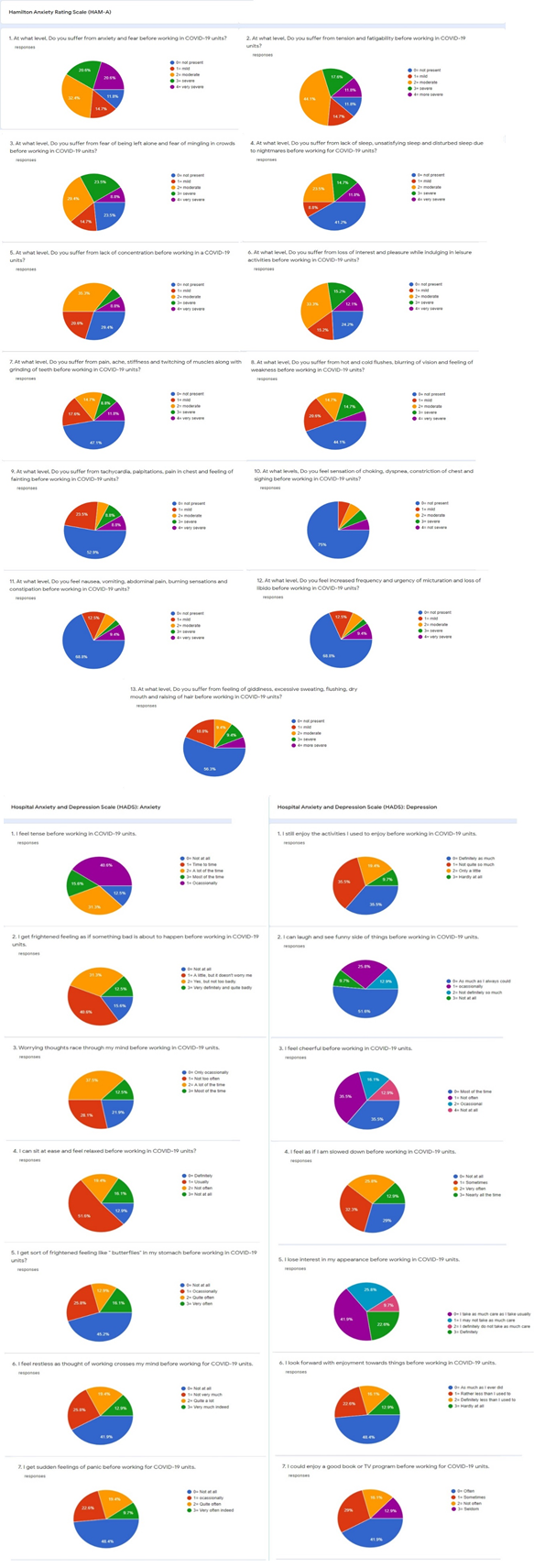
Figure 1: Showing the response percentage of each question by the respondents.
3. Results
The mean age of all the young doctor participants in the study was 25.40 ± 1.61 with an equal male to female ratio as shown in (Table 1). Around 57% of respondents were house officers/interns while 43% were medical residents/postgraduate trainees of various departments. The mean duration of practice of house officers was quite less than that of medical residents (P<0.001) mostly having a training program of 4 years as compared to only 1 year of house job/internship. The Hamilton anxiety scale (HAM-A) (P=0.078) and Hospital anxiety depression scale (HADS) for anxiety was significantly higher in females (P=0.001), while HADS for depression was statistically indifferent among the gender as shown in (Table 2A). Both the anxiety and depression scales were significantly higher in house officers as compared to their senior doctors (residents/postgraduate trainees).
|
S.no |
Table 1: General characteristics of the respondents (n=109). |
p-value |
||
|
1 |
Mean age in years |
25.40 ± 1.61 |
0.170* |
|
|
Males (n=53) |
25.62 ± 1.79 |
|||
|
Females (n=56) |
25.19 ± 1.40 |
|||
|
2 |
Medical profession rank |
House officer/Interns: 62 (56.9%) |
<0.001* |
|
|
Mean age: 24.51 ± 1.06 |
||||
|
Residents/Postgraduate Trainee: 47 (21.21%) |
||||
|
Mean age: 26.57 ± 1.47 |
||||
|
3 |
Durations of Practice (in months) |
11.14 ± 9.84 |
<0.001* |
|
|
House officer/Interns: 5.09 ± 1.77 |
||||
|
Residents/Postgraduate Trainee: 19.12 ± 10.44 |
||||
|
4 |
Distribution of gender amongst professional rank |
House officer/Interns: |
Residents/ Postgraduate Trainee: |
0.955** |
|
Males: 30 (56.6%) Females: 32 (57.1%) |
Males: 23 (43.4%) Females: 24 (48.9%) |
|||
|
* indicates p-value calculated by independent sample t-test. ** indicates p-value calculated by chi-square test. |
||||
|
Table 2A: Anxiety scales used before or during corona ward postings. |
|||||||
|
Variable Scales |
Study groups |
P-value |
|||||
|
Mean |
±SD |
Mean |
±SD |
||||
|
Males |
Females |
||||||
|
Hamilton anxiety scale |
13.39 |
9.20 |
17.05 |
12.01 |
0.078* |
||
|
Hospital anxiety and depression scale (HADS) |
For anxiety |
6.60 |
4.85 |
9.91 |
5.61 |
0.001* |
|
|
For depression |
7.09 |
5.09 |
6.98 |
4.71 |
0.905* |
||
|
- |
House officer/Interns: |
Residents/Postgraduate Trainee |
- |
||||
|
Hamilton anxiety scale |
17.35 |
11.76 |
12.53 |
8.90 |
0.016* |
||
|
Hospital anxiety and depression scale (HADS) |
For anxiety |
10.06 |
5.00 |
5.97 |
5.28 |
<0.001* |
|
|
For depression |
8.12 |
5.10 |
5.59 |
4.19 |
0.005* |
||
|
Table 2B: Anxiety scales after corona ward postings. |
|||||||
|
- |
Males |
Females |
- |
||||
|
Hamilton anxiety scale |
10.24 |
6.51 |
10.58 |
7.21 |
0.795* |
||
|
Hospital anxiety and depression scale (HADS) |
For anxiety |
5.33 |
2.94 |
6.51 |
3.91 |
0.080* |
|
|
For depression |
5.54 |
3.06 |
5.12 |
2.89 |
0.462* |
||
|
- |
House officer/Interns |
Residents/Postgraduate Trainee |
- |
||||
|
Hamilton anxiety scale |
11.14 |
6.76 |
9.46 |
6.93 |
0.208* |
||
|
Hospital anxiety and depression scale (HADS |
For anxiety |
6.77 |
3.54 |
4.85 |
3.18 |
0.004* |
|
|
For depression |
5.85 |
3.18 |
4.63 |
2.54 |
0.029* |
||
|
* indicates p-value calculated by independent sample t-test. |
|||||||
According to Hamilton anxiety scale, 62% respondents were in the mild category, 20% mild to moderate, 5% moderate to severe, while 14 respondents (13%) were in severe anxiety category, out of whom 11 respondents were female house officers (P=0.070), as also demonstrated by a high mean value of female house officers in (Figure 2A). While only 3 male residents reported severe anxiety according to HAM-A as shown in (Table 3). The mean HAM-A of all the respondents was 15.27 ± 10.84 which got improved to 10.42 ± 6.85 post working in corona units (P<0.001), also 90% of the respondents fell into mild anxiety category with massive improvements shown by female house officers (P=0.012) as shown in (Table 4).
|
Table 3: Frequency of anxiety scales grading amongst the study groups. |
|||||
|
Variables |
Scales |
p-value |
|||
|
Hamilton anxiety scales |
|||||
|
Frequency- n (%) |
Mild (≤17) |
Mild to moderate (18-24) |
Moderate to severe (25-30) |
Severe (>30) |
- |
|
All participants |
68 (62%) |
22 (20%) |
5 (4%) |
14 (13%) |
|
|
Males |
33 (62%) |
13 (24%) |
4 (7%) |
3 (6%) |
0.070* |
|
Females |
35 (62%) |
9 (16%) |
1 (2%) |
11 (20%) |
|
|
House officer/ interns |
36 (58%) |
12 (19%) |
3 (5%) |
11 (18%) |
0.378* |
|
Residents/ Postgraduate trainee |
32 (68%) |
10 (21%) |
2 (4%) |
3 (6%) |
|
|
For anxiety |
Hospital anxiety and depression scale (HADS) |
- |
|||
|
Normal (≤7) |
Mild (8-10) |
Moderate (11-14) |
Severe (>15) |
||
|
All participants |
51 (47%) |
21 (19%) |
22 (20%) |
15 (14%) |
|
|
Males |
31 (58%) |
12 (23%) |
7 (13%) |
3 (6%) |
0.012** |
|
Females |
20 (36%) |
9 (16%) |
15 (27%) |
12 (21%) |
|
|
House officer/ interns |
15 (24%) |
18 (29%) |
18 (29%) |
11 (18%) |
<0.001** |
|
Residents/ Postgraduate trainee |
36 (77%) |
3 (6%) |
4 (7%) |
4 (7%) |
|
|
For depression |
Hospital anxiety and depression scale (HADS) |
- |
|||
|
Normal (≤7) |
Mild (8-10) |
Moderate (11-14) |
Severe (>15) |
||
|
All participants |
64 (59%) |
17 (16%) |
19 (17%) |
9 (8%) |
|
|
Males |
30 (57%) |
13 (24%) |
3 (6%) |
7 (13%) |
0.001* |
|
Females |
34 (61%) |
4 (7%) |
16 (29%) |
2 (3%) |
|
|
House officer/ interns |
30 (48%) |
12 (19%) |
12 (19%) |
8 (13%) |
0.047* |
|
Residents/ Postgraduate trainee |
34 (72%) |
5 (11%) |
7 (15%) |
1 (2%) |
|
|
* indicates p-value calculated by Fisher’s exact test. ** indicates p-value calculated by chi-square test. |
|||||
|
Table 4: Comparison of anxiety scales after Corona ward postings. |
||||||
|
Variables and Scales |
Mean ± SD |
P-value |
||||
|
Groups |
||||||
|
Hamilton anxiety scale |
Before |
15.27 ± 10.84 |
<0.001* |
|||
|
After |
10.42 ± 6.85 |
|||||
|
Frequencies |
Mild |
Mild to moderate |
Moderate to severe |
Severe |
- |
|
|
All respondents |
Before |
68 (62%) |
22 (20%) |
5 (4%) |
14 (13%) |
<0.001** |
|
After |
98 (90%) |
4 (4%) |
4 (4%) |
3 (3%) |
||
|
Males |
Before |
33 (62%) |
13 (24%) |
4 (7%) |
3 (6%) |
0.013** |
|
After |
48 (90%) |
3 (6%) |
1 (2%) |
1 (2%) |
||
|
Females |
Before |
35 (62%) |
9 (16%) |
1 (2%) |
11 (20%) |
0.012** |
|
After |
50 (89%) |
1 (2%) |
3 (5%) |
2 (4%) |
||
|
House officer/ Interns |
Before |
36 (58%) |
12 (19%) |
3 (5%) |
11 (18%) |
0.003** |
|
After |
55 (89%) |
3 (5%) |
2 (3%) |
2 (3%) |
||
|
Residents/ Postgraduate trainee |
Before |
32 (68%) |
10 (21%) |
2 (4%) |
3 (6%) |
0.030** |
|
After |
43 (92%) |
1 (2%) |
2 (4%) |
1 (2%) |
||
|
HADS (for anxiety) |
Before |
8.30 ± 5.49 |
<0.001* |
|||
|
After |
5.94 ± 3.51 |
|||||
|
Frequencies |
Normal |
Mild |
Moderate |
Severe |
- |
|
|
All respondents |
Before |
51 (47%) |
21 (19%) |
22 (20%) |
15 (14%) |
<0.001** |
|
After |
81 (74%) |
18 (16%) |
6 (5%) |
4 (4%) |
||
|
Males |
Before |
31 (58%) |
12 (23%) |
7 (13%) |
3 (6%) |
0.047** |
|
After |
43 (81%) |
8 (15%) |
1 (2%) |
1 (2%) |
||
|
Females |
Before |
20 (36%) |
9 (16%) |
15 (27%) |
12 (21%) |
<0.001** |
|
After |
38 (68%) |
10 (18%) |
5 (9%) |
3 (5%) |
||
|
House officer/ Interns |
Before |
15 (24%) |
18 (29%) |
18 (29%) |
11 (18%) |
<0.001** |
|
After |
40 (64%) |
15 (24%) |
4 (7%) |
3 (5%) |
||
|
Residents/ Postgraduate trainee |
Before |
36 (77%) |
3 (6%) |
4 (7%) |
4 (7%) |
0.275** |
|
After |
41 (87%) |
3 (6%) |
2 (4%) |
1 (2%) |
||
|
HADS (for depression) |
Before |
7.03 ± 4.87 |
<0.001* |
|||
|
After |
5.33 ± 2.97 |
|||||
|
Frequencies |
Normal |
Mild |
Moderate |
Severe |
- |
|
|
All respondents |
Before |
64 (59%) |
17 (16%) |
19 (17%) |
9 (8%) |
<0.001** |
|
After |
91 (83%) |
10 (9%) |
5 (5%) |
3 (3%) |
||
|
Males |
Before |
30 (57%) |
13 (24%) |
3 (6%) |
7 (13%) |
0.004** |
|
After |
44 (83%) |
4 (7%) |
4 (7%) |
1 (2%) |
||
|
Females |
Before |
34 (61%) |
4 (7%) |
16 (29%) |
2 (3%) |
<0.001** |
|
After |
47 (84%) |
6 (11%) |
1 (2%) |
2 (3%) |
||
|
House officer/ Interns |
Before |
30 (48%) |
12 (19%) |
12 (19%) |
8 (13%) |
<0.001** |
|
After |
48 (77%) |
8 (13%) |
4 (6%) |
2 (3%) |
||
|
Residents/ Postgraduate trainee |
Before |
34 (72%) |
5 (11%) |
7 (15%) |
1 (2%) |
0.023** |
|
After |
43 (92%) |
2 (4%) |
1 (2%) |
1 (2%) |
||
|
* Paired sample t-test, ** McNemar-Bowker’s test. |
||||||
The mean HADS for anxiety before/during working in corona units was significantly higher (8.30 ± 5.49) which again comprised mostly of females (P=0.012) and house officers (P<0.001), which improved to 5.94 ± 3.51 (P<0.001) post-work, with the least improving pattern seen in male residents as visible in (Figure 2A). The HADS for depression before/during corona posting was also higher with most male respondents were in mild or severe depression, and most female respondents were in moderate depression category (P=0.001). The mean got improved from 7.03 ± 4.87 to 5.33 ± 2.97 post working in corona units (P<0.001), with male residents again least affected while male house officers still having slightly higher mean also showed the highest improvement as well.
The duration of practice had an inverse correlation observed with all the studied scales in the HCWs. (Figure 2B) showing that the anxiety levels are significantly higher in 1st month of internship followed by a second peak in those with 6-8 months of practice, while also in 1st year of residency followed by 3rd year of residency, with 2nd year of residents were having the least scores of anxiety as well as depression. The same pattern can also be seen with significant improvement of scores after corona ward postings as shown in (Figure 2C), massive improvement is visible by those in 7-8 months of practice, while 3rd to 4th year residents showing lowest improvements. The correlation of HAM-A was significant with the duration of practice before/during corona posting as opposed to after posting (Figure 2D). The correlation of HADS for anxiety (before/during posting) was maximum with the duration of practice, r= -0.351 (P<0.001), and after corona postings, r= -0.221 (P=0.021), as shown in (Figure 2E). The HADs for depression were also significantly correlated with the duration of practice both before and after corona ward postings (Figure 2F). Overall, after corona ward postings, significant improvements were seen in all groups of respondents, with no difference in HAM-A among gender (P=0.795) and professional rank (P=0.208), while HADS for anxiety was still found higher in females (P=0.080) and house officers (P=0.004), and HADS for depression was only higher in house officers post improvements (P=0.029) as shown in (Table 2B).
4. Discussion
Our study surveyed the prevalence of anxiety and depression among health care workers comprising of physicians treating sufferers of COVID-19 in hospitals. In our observation, limited studies have been conducted in order to determine mental health symptoms among frontline health care providers working in COVID-19 units. Studies conducted by Lai et al, and others indicated the age of 26 years, thus coinciding with findings of our study [1, 11, 12]. Multiple studies indicated gender predilection among health care providers participating in survey with females in the majority as compared to males, an outcome contrasting our study reporting an equal number of male and female participants [1-3, 11, 12]. A study conducted in a similar pattern reported 50.4% of depression and 44.6% of anxiety among health care providers serving in COVID-19 units of Wuhan, outcomes coinciding with the results of our study [11]. Various studies quoted decreased frequency of anxiety and depression among health care workers when compared with frequencies recorded in our study, meanwhile, a study of Istanbul reported increased frequency for depression and decreased for anxiety, both outcomes not correlating with our results [1-4, 12]. A greater number of studies signified female gender and young health care providers reporting heightened levels of anxiety an outcome consistent with findings of our study [1-3, 11, 12]. Our study reported the incidence of depression heightened among young health care providers, while no gender difference among participants suffering from depression was observed, a finding contrasting outcomes of several studies depicting female gender prominent in acquiring depression [3, 11, 12]. A study observed by Wen Lu, et al. and another study conducted among health care providers of Istanbul depicted lesser mean values of anxiety and depression among participants thus contrasting our results projecting increased mean values [2, 3]. A study conducted in Fujian province of China, quoted 22.6% mild to moderate anxiety among participants an outcome coinciding with our study, while the decreased prevalence of severe anxiety contrasting our results [13], while the same study quoted decreased prevalence of mild, moderate and severe depression, an outcome not synchronizing with our study quoting increased frequencies [13]. Another study reported outcomes regarding frequencies of mild and severe depression among participants correlating with our results, while the increased incidence of moderate depression, an outcome contrasting with our study [3]. Frequencies regarding mild, moderate, and severe anxiety among participants were decreased in the study mentioned above when compared with findings of our study thus contrasting our results [3]. Lastly, a study conducted in the same population recently has identified a 43% prevalence of depression/anxiety among frontline doctors of Pakistan, with many factors linked along with it including increased workload, duty hours, having children amongst household members and decreased knowledge regarding the infectivity of the disease [14].
Despite an improvement in frequencies of anxiety and depression among health care providers after serving their duties in COVID-19 units included in our study, still, the levels of anxiety and depression are recorded higher when compared to other populations. The limitation of the study included the lack of insight by senior faculty members supervising the corona units, as the study focused only on the young frontline doctors.
5. Conclusions
Depression and anxiety were seen quite higher in our population of health care workers with significant improvements that were observed after completing the rotations of corona units. Mental health can play an important role in defining the health care response towards a pandemic. Mental health needs to be a priority for doctors and other health care providers on the frontline, and amidst a global pandemic, it should be one of the key elements of adaptability in a society that is confronted by a perplexing number of challenges. Training programs or short courses/ workshops should be carried out amongst the frontline doctor before corona unit duties for helping them to cope up with the anxiety levels.
Disclosure Statement
The authors declare no conflicts of interest with this article's content.
Funding Statement
This work is not supported by any sponsors. No funding required in this study.
Ethical Approval Statement
Ethical approval was taken in this study from institutional review board, and consent to participate has been taken from all the patient’s guardian with informed written consent.
References
- Liu CY, Yang YZ, Zhang XM, et al. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: a cross-sectional survey. Epidemiol Infect 148 (2020): e98.
- Chew NWS, Lee GKH, Tan BYQ, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak [published online ahead of print, 2020 Apr 21]. Brain Behav Immun 20 (2020): 30523-30527.
- Elbay RY, Kurtulmus A, Arpacioglu S, et al. Depression, anxiety, stress levels of physicians and associated factors in COVID-19 pandemics [published online ahead of print, 2020 May 27]. Psychiatry Res 290 (2020): 113130.
- Shechter A, Diaz F, Moise N, et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen Hosp Psychiatry 66 (2020): 1-8.
- Assessment of anxiety levels among health care providers working for COVID-19 units. Google forms. (2020).
- Hamilton M. The assessment of anxiety scales by rating. Br J Med Psychol 32 (1959): 50-55.
- Wilkinson MJ, Barczak P. Psychiatric screening in general practice: comparison of the general health questionnaire and the hospital anxiety depression scale. J R Coll Gen Pract 38 (1988): 311-313.
- OpenEpi sample size calculator. Open source statistics for public health (2013).
- Hamilton anxiety scale calculator.
- BGP Article. Hospital Anxiety and Depression (HAD) scale update 9.
- Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to corona virus disease 2019. JAMA Network Open 3 (2020): e203976.
- Zhu Z, Xu S, Wang H, et al. COVID-19 in Wuhan: Immediate psychological impact on 5062 health workers. MedRxiv preprint.
- Lu W, Wang H, Lin Y, et al. Psychological status of medical work force during the COVID-19 pandemic: A cross-sectional study. Psychiatry research (2020).
- Amin F, Sharif S, Saeed R, et al. COVID-19 Pandemic- Knowledge, Perception, Anxiety and Depression Among Frontline Doctors of Pakistan. [published online ahead of print, June 2020]. BMC Psychiatry (2020).
