Level of Hypoalbuminemia as a Prognostic Factor in Patients admitted to a Tertiary Care Intensive Coronary Care Unit
Article Information
Nimrod Perel1*, Louay Taha1, Rivka Farkash1, Yoed Steinmetz1, Fauzi Shaheen1, Nir Levi1, Ziv Dadon1, Hani Karameh1, Mohamed Karmi1, Tomer Maller1, Kamal Hamyil1, Anna Turyan1, Mohamed Manatzra1, Feras Bayya1, Michael Glikson1 and Elad Asher1
1Department of Cardiology, Jesselson Integrated Heart Center, Shaare Zedek Medical Center and Faculty of Medicine, Hebrew University of Jerusalem, Israel
*Corresponding author: Nimrod Perel, Department of Cardiology, Jesselson Integrated Heart Center, Shaare Zedek Medical Center and Faculty of Medicine, Hebrew University of Jerusalem, Israel.
Received: 01 November 2022; Accepted: 15 November 2022; Published: 08 December 2022
Citation:
Nimrod Perel, Louay Taha, Rivka Farkash, Yoed Steinmetz, Fauzi Shaheen, Nir Levi, Ziv Dadon, Hani Karameh, Mohamed Karmi, Tomer Maller, Kamal Hamyil, Anna Turyan, Mohamed Manatzra, Feras Bayya, Michael Glikson and Elad Asher. Level of Hypoalbuminemia as a Prognostic Factor in Patients admitted to a Tertiary Care Intensive Coronary Care Unit. Cardiology and Cardiovascular Medicine 6 (2022): 536-541.
View / Download Pdf Share at FacebookAbstract
Introduction: Hypoalbuminemia is common in acute and chronic diseases. It has been proposed as a potential biomarker of frailty, which itself is associated with worse outcomes. However, data regarding the level of hypoalbuminemia and its prognosis in contemporary intensive coronary care unit (ICCU) patients is scarce.
Materials and Methods: All patients who had albumin level on admission to an ICCU at a tertiary care center between January 1, 2020, and December 31, 2020, were included in the study. Patients were divided into 3 groups according to their albumin level on admission: low (< 3 g/dL), intermediate (3 g/dL≤ and ≤ 4 g/dL) and high albumin level (> 4 g/dL). Survival and in-hospital interventions and complications were compared.
Results: Overall 1,036 consecutive patients were included, mean age was 67±16 years and 70% were males. Of them 88 (8.5%) had low, 739 (71.5%) intermediate and 209 (20%) had high albumin levels. In a multivariate cox proportional hazards analysis, low albumin level was independently associated with higher 1-year mortality rate as compared with high albumin level (HR=9.5; 95% CI: 3.2-25.5, p<0.001). Intermediate albumin level had also a trend toward higher 1-year mortality rate as compared with high albumin level (HR=2.1; 95% CI: 0.9-5.6, p=0.09).
Conclusion: Hypoalbuminemia in ICCU patients is a poor prognostic factor associated with in-hospital complications and an independent risk factor for 1-year mortality rate, while intermediate albumin level shows a trend towards higher 1-year mortality rate as well.
Keywords
Albumin; Acute Coronary Syndrome (ACS); Intensive Coronary Care Unit (ICCU)
Article Details
1. Introduction
Albumin is a protein synthesized by the liver and it is the most common protein in the serum. Albumin has several functions including carrying of water-insoluble molecule and maintaining osmotic pressure gradient, while its role as anti-inflammatory and maintaining the integrity of the vascular endothelium is not as fully understood [1,2]. It has been suggested that albumin can decrease and limit the leakage of water from blood vessels seen during the acute phase of the illness. The proposed mechanisms include preventing endothelial cell apoptosis and changing the glycoprotein distribution in the vessel wall [3,4]. Its synthesis is also influenced by the nutritional status of the body, hormonal and catabolic state [3]. Its level can drop in situations such as acute severe illness or chronic systemic inflammatory disease [5]. The levels of albumin not only can decrease during acute illness but can also remain low until recovery [6]. Low albumin level was associated with a higher mortality rate among hospitalized veteran patients [7]. Furthermore, hypoalbuminemia has also been reported as an independent risk factor for several cardiovascular disease including ischemic heart disease, heart failure, stroke, and venous thromboembolism [1]. In patients with acute coronary syndrome (ACS) low albumin levels at admission were found to be in correlation with an increased in-hospital mortality and high SYNTAX score [8]. Among patients with ST segment myocardial infarction (STEMI) and ACS, low albumin level was an independent predictor for in-hospital mortality, long-term mortality and for heart failure development [9,10]. Nevertheless, data regarding the levels of hypoalbuminemia and prognosis in contemporary intensive coronary care unit (ICCU) patients is limited. Hence, we aimed to investigate the role of hypoalbuminemia as a risk factor for in-hospital complications and 1-year mortality rate among patients admitted to the ICCU in a tertiary care medical center.
2. Methods
All patients admitted to the ICCU at Shaare Zedek Medical Center between January – December 2020 were included in the study. Based on routine albumin level on admission (first 12 hours), patients were categorized into low (<3 g/dL) intermediate (3-4 g/dL) and high (4> g/dL) albumin levels. Although several previous studies have used albumin cutoff level of 3.5 g/dL and divide patients into high or low albumin levels [5,6] , we design the study using 3 different categories to better define and categorized the different patients, and in attempt to better identify patients most at risk. Patients without admission levels of albumin were excluded from the study.
2.1 Study Outcomes
The primary outcome was overall mortality, assessed at 1-year mortality rate from time of index hospitalization. The study secondary outcomes were in-hospital complications during the index hospitalization.
2.2 Data Collection
Data were anonymously documented and prospectively submitted into an electronic case report form (eCRF). Data were then checked for accuracy and out-of-range values by a local coordinator. Demographic data, presenting symptoms, comorbid conditions, and physical examination were systematically recorded as well as laboratory, imaging data. Overall mortality rates were determined from the Israeli Ministry of Internal Affairs. The Shaare Zedek Medical Center Institutional Review Board (IRB) approved the study on the basis of strict maintenance of participants’ anonymity by de-identifying during database analysis. Informed consent was waived by the IRB. Moreover, the authors have no conflict of interest to declare. No Funding was applied for the study and all methods were performed in accordance with the relevant guidelines and regulations.
2.3 Statistical Analyses
Characteristics were described as numbers and percentages for categorical variables and by means ± standard deviations or median with interquartile ranges for continuous variables. Relations between categorical variables were evaluated by chi-square and Fisher’s exact tests. The effect of categorical variables on continuous measurements was tested by student-T and Mann-Whitney tests. The choice of a parametric or nonparametric test depended on the distribution of the continuous variable. Mortality rate was analyzed by applying stepwise backward Cox proportional hazards model adjusted for albumin groups (using the high level of 4> g/dL as a reference group), age, gender, prior cardiac intervention, various cardiac risk factors and left ventricular ejection fraction (EF) <40%. All tests were two-sided with p<0.05 considered as statistically significant. Analyses were performed using SPSS Statistics for Windows, Version 25.0. (IBM Corp, Armonk, NY, USA).
3. Results
3.1 Study Population
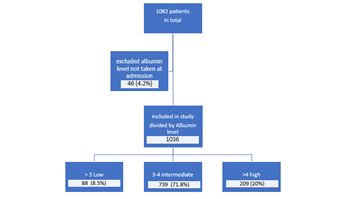
A total of 1082 patients were admitted to the ICCU during the study period. Of them, 1036 (95%) patients had albumin level taken on admission and constitute the study population. Of them, 88 (8.5%) had low, 739 (71.5%) intermediate and 209 (20%) had high albumin levels. Figure 1 describes patients’ enrollment chart.
3.2 Patients Characteristics
Table 1 presents patients characteristics according to albumin levels on admission. Mean age was 67±16 years and 754 (73%) were males. Patients in the high albumin group were significantly younger as compared with patients in the low and intermediate groups (60±15 vs. 69±17 and 69±15 years respectively, p<0.001]. Patients in the higher albumin group also had a higher body mass index (BMI) and a higher rate of active smokers while lower rate of cerebrovascular accident (CVA), peripheral artery disease (PAD), congestive heart failure (CHF), chronic obstructive pulmonary disease (COPD), anemia, renal failure and malignancy.
|
Baseline characteristics |
Total N= 1036 |
Low albumin level (<3 g/dL) N= 88 |
Intermediate albumin level (3-4 g/dL) N= 739 |
High albumin level (>4 g/dL) N= 209 |
p value |
|
|
Age |
<49 |
129 |
11.30% |
10.30% |
12.40% |
|
|
50-59 |
173 |
13.60% |
14.60% |
16.70% |
||
|
60-69 |
246 |
19.30% |
23.70% |
23.70% |
||
|
70-79 |
258 |
25% |
26.80% |
24.90% |
||
|
80-89 |
187 |
27.30% |
19.80% |
18.10% |
||
|
>90 |
43 |
3.40% |
4.90% |
4.20% |
||
|
Gender |
Female |
311 |
45.50% |
30.90% |
30% |
<0.001 |
|
Male |
725 |
54.50% |
69.10% |
70% |
<0.001 |
|
|
HTN, n (%) |
631 |
63.60% |
62.40% |
54.50% |
0.1 |
|
|
DLP |
534 |
53.40% |
52.20% |
48.80% |
0.649 |
|
|
DM |
373 |
31.80% |
37.90% |
31.10% |
0.136 |
|
|
Smoking |
311 |
19.30% |
28.40% |
40.20% |
<0.001 |
|
|
Prior CAD |
300 |
25% |
30.60% |
24.90% |
0.191 |
|
|
Prior CVA |
82 |
11.40% |
8.70% |
3.80% |
0.034 |
|
|
PAD |
59 |
11.40% |
5.70% |
3.30% |
0.25 |
|
|
COPD |
86 |
17% |
8.90% |
2.40% |
<0.001 |
|
|
CHF |
154 |
22.70% |
15.60% |
9.10% |
0.006 |
|
|
CKD |
169 |
27.30% |
17.50% |
7.70% |
<0.001 |
|
|
Prior PE |
9 |
1.10% |
0.90% |
0.50% |
0.78 |
|
|
Malignancy |
98 |
21.60% |
9.30% |
4.80% |
<0.001 |
|
|
Anemia |
57 |
12.50% |
6.10% |
0.50% |
<0.001 |
|
|
Atrial Fibrillation |
145 |
17% |
15.60% |
7.20% |
0.006 |
|
|
Prior CIED |
53 |
8% |
5.10% |
3.80% |
0.0037 |
|
|
Prior CABG |
52 |
5.70% |
5% |
4.80% |
0.949 |
|
|
Prior TAVI |
11 |
3.40% |
0.80% |
1% |
0.79 |
|
Table 1: Patients characteristics according to albumin levels on admission.
HTN- Hypertension; DLP- Dyslipidemia; DM- Diabetes Mellitus; CAD- Coronary Artery Disease; CVA- Cerebrovascular Accident; PAD- Peripheral Artery Disease; COPD-Chronic Obstructive Pulmonary Disease; CHF- Chronic Heart Failure; CKD- Chronic Kidney Disease; PE- Pulmonary Embolism; CIED- Cardiac Implantable Electronic Device; CABG- Coronary Artery Bypass; TAVI- Transfemoral Aortic Valve Implantation
3.3 Diagnosis on Admission
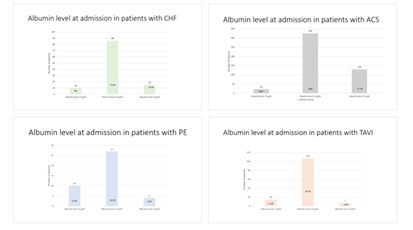
Patients diagnoses on admission are presented in Figure 2. Nearly half of the patients 478 (46%) were admitted with ACS and had a higher rate of high albumin levels as compared with non-ACS patients (63% vs. 37%, p<0.0001). Other common diagnosis at admission were CHF exacerbation and post transcutaneous aortic valve implantation (TAVI). In patients presented with CHF exacerbation there was a lower rate of high albumin level (7.2%, p=0.01). Similarly, patients admitted after TAVI had a lower rate of high albumin level (3.3%, p<0.0001).
3.4 Complication during Hospitalization
Patients in the low albumin group had higher rates of major bleeding during their hospitalization as compared with the intermediate and high albumin groups (11.4% vs. 6.0% and 1.4%, respectively, p<0.002), as well as higher rates of sepsis (5.7% vs. 1.2% and 1%, respectively, p<0.004) invasive mechanical ventilation (20% vs. 4.9% and 4.3%, respectively, p<0.001) and cardiopulmonary resuscitation (CPR) (14% vs 1.9% and 0.5%, respectively, p<0.001).
3.5 Mortality Rate
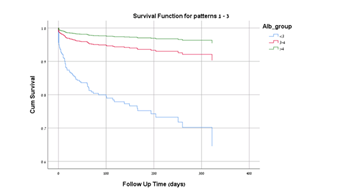
Mortality rate at 1 year was higher in the low albumin group as compared with the intermediate and high groups (29% vs. 8.1% and 2.4%, respectively, p<0.001) as shown in Figure 3. A multivariate cox proportional hazard analysis found that low albumin levels were independently associated with increase mortality as compared with high albumin levels [HR =9.5, 95% CI: )3.2-25.5)].
4. Discussion
This prospective study includes more than a thousand patients admitted to a tertiary care ICCU and demonstrates the following findings: i) low albumin level rates were higher among patients diagnosed with CHF exacerbation, pulmonary embolism, post-TAVI or shock. On the other hand, patients diagnosed with ACS and with myocarditis had higher rates of higher albumin level, which may be attributed to their younger age and general physical condition; ii) low albumin levels correlate with several complications during admission such as bleeding, sepsis, mechanical ventilation and CPR; iii) low albumin level is an independent risk factor for 1-year mortality rate, while intermediate albumin level shows a trend towards higher 1-year mortality rate. Albumin has been investigated as a prognostic marker in several diseases including ulcerative colitis and acquired immunodeficiency syndrome (AIDS) [7,8]. It was also found to be a prognostic marker in several cardiovascular diseases, such as patients hospitalized with CHF exacerbation, where low albumin was level was independently associated with higher mortality at 1 year [9]. Also, in elderly patients undergoing TAVI albumin levels are correlated with survival [11] the pathophysiology of hypoalbuminemia in patients with cardiovascular is diverse and multifactorial. Malnutrition and systemic inflammation and hemodilution in addition to decrease production by the congested liver may cause hypoalbuminemia in patients with heart failure [9,12]. Systemic inflammation was also seen in patients with ACS, renal failure, and malignancy [11, 14-16]. Our finding that a higher number of patients with renal failure and malignancy were in the low albumin group correlates with other studies and gives another emphasis to that. Nevertheless, few studies have shown the association of albumin level and mortality rate as marker in the spectrum of the cardiovascular diseases in the setting of acute care and hospitalization in the ICCU. In addition, instead of the traditional division of the groups into high or low level of albumin based on a single cutoff value (mostly 3.5 g/dL) we used a more comprehensive categorization dividing the groups into high, intermediate, or low level of albumin. This specification can be used as a more accurate marker for acute ill patients in the setting of ICCU. The levels of albumin might be interpreted as a spectrum rather than as a single cut-off value of high or low. In fact, our study shows that not only low albumin level was an independent risk factor for 1-year mortality rate, but intermediate albumin level also associated with higher 1-year mortality rate. Although this trend did not reach statistical significance, it can still emphasize the importance of using albumin level as a spectrum, and hopefully can help physicians to better understand and categorized the ICCU patients risks.
5. Limitations
Our study has several limitations, first the study was a single center study. Second, baseline albumin levels before admission were not available, nevertheless, our aim was to examine the level of albumin at admission regardless of the baseline albumin level, as a predictor of mortality. Finally, the follow-up was limited to 1-year.
6. Conclusions
As with other morbid condition, hypoalbuminemia in a contemporary ICCU patients is a prognostic factor for in hospital morbidity and complications and is independently associated with mortality rate in the first year after hospitalization. Intermediate albumin level as compared with high albumin level, had a trend toward increased mortality risk, although it did not reach statistical significance. The routine use of albumin level as a marker for risk stratification may be considered in ICCU setting.
References
- Arques S. Human serum albumin in cardiovascular diseases. Eur J Intern Med 52 (2018): 8-12.
- Artigas A, Wernerman J, Arroyo V, et al. Role of albumin in diseases associated with severe systemic inflammation: Pathophysiologic and clinical evidence in sepsis and in decompensated cirrhosis. J Crit Care 33 (2016): 62-70.
- Nicholson JP, Wolmarans MR, Park GR. The role of albumin in critical illness. Br J Anaesth 85 (2000): 599-610.
- Demling RH. Effect of plasma and interstitial protein content on tissue edema formation. Curr Stud Hematol Blood Transfus 53 (1986): 36-52.
- Atrash AK, de Vasconcellos K. Low albumin levels are associated with mortality in the critically ill: A retrospective observational study in a multidisciplinary intensive care unit. The Southern African journal of critical care?: the official journal of the Critical Care Society 36 (2020): 74-79.
- Li Y, She Y, Mo W, et al. Albumin Level at Admission to the Intensive Care Unit Is Associated With Prognosis in Cardiac Arrest Patients. Cureus 13 (2021).
- Khan N, Patel D, Shah Y, et al. Albumin as a prognostic marker for ulcerative colitis. World J Gastroenterol 23 (2017): 8008-8016.
- Ronit A, Sharma S, Baker Jv, et al. Serum Albumin as a Prognostic Marker for Serious Non-AIDS Endpoints in the Strategic Timing of Antiretroviral Treatment (START) Study. J Infect Dis 217 (2018): 405-412.
- Uthamalingam S, Kandala J, Daley M, et al. Serum albumin and mortality in acutely decompensated heart failure. Am Heart J 160 (2010): 1149-1155.
- Horwich TB, Kalantar-Zadeh K, MacLellan RW, et al. Albumin levels predict survival in patients with systolic heart failure. Am Heart J 155 (2008): 883-889.
- Bogdan A, Barbash IM, Segev A, et al. Albumin correlates with all-cause mortality in elderly patients undergoing transcatheter aortic valve implantation. EuroIntervention 12 (2016): e1057-e1064.
- Arques S, Ambrosi P. Human serum albumin in the clinical syndrome of heart failure. J Card Fail 17 (2011): 451-458.
- Don BR, Kaysen G. Serum albumin: relationship to inflammation and nutrition. Semin Dial 17 (2004): 432-437.
- Dániel D, András T. Prognostic importance of albumin in oncology. Orv Hetil 159 (2018): 96-106.
- González-Pacheco H, Amezcua-Guerra LM, Sandoval J, et al. Prognostic Implications of Serum Albumin Levels in Patients With Acute Coronary Syndromes. Am J Cardiol 119 (2017): 951-958.
- Wallace SM, Walton BI, Kharbanda RK, et al. Mortality from infective endocarditis: clinical predictors of outcome. Heart 88 (2002): 53-60.