Left Ventricular Pseudoaneurysmectomy and Mitral Valve Replacement 30 Years after Blunt Polytrauma
Article Information
Karel M. Van Praet1,2*, Markus Kofler1, Lilia Kruse1, Natalia Solowjowa1, Felix Hennig1, Christof Stamm1, Axel Unbehaun1, Christoph Starck1, Stephan Jacobs1, Jörg Kempfert1,2, Volkmar Falk1,2,3,4, Christoph Knosalla1,2
1Department of Cardiothoracic and Vascular Surgery, German Heart Center Berlin (Deutsches Herzzentrum Berlin), Germany
2DZHK (German Center for Cardiovascular Research)-partner site Berlin, Germany
3Department of Cardiothoracic Surgery, Charité – Universitätsmedizin Berlin, Germany
4Berlin Institute of Health (BIH), Germany
*Corresponding Author: Dr. Karel M Van Praet, Department of Cardiothoracic and Vascular Surgery, German Heart Center Berlin, Augustenburger Platz 1, 13353 Berlin, Germany
Received: 29 August 2019; Accepted: 17 September 2019; Published: 28 November 2019
Citation: Karel M. Van Praet, Markus Kofler, Natalia Solowjowa, Felix Hennig, Christof Stamm, Axel Unbehaun, Christoph Starck, Stephan Jacobs, Jörg Kempfert, Volkmar Falk, Christoph Knosalla. Left Ventricular Pseudoaneurysmectomy and Mitral Valve Replacement 30 Years after Blunt Polytrauma. Archives of Clinical and Medical Case Reports 3 (2019): 632-635.
View / Download Pdf Share at FacebookAbstract
Left ventricular (LV) pseudoaneurysms are the consequence of cardiac rupture, usually contained by adherent pericardium or fibrous scar tissue. They represent, from a functional point of view, the acquired blood-filled spaces that are external to the cardiac chambers but communicating with the ventricle. They can occur after transmural myocardial infarction or, albeit less frequently, post-traumatically. This cardiac disease has been a topic of discussion since the pioneering days of heart surgery. We present a case of a posttraumatic LV pseudoaneurysm, in which the causative blunt trauma happened 30 years prior to the onset of symptoms. Severe functional mitral regurgitation (FMR) resulted from leaflet tethering and partial rupture of the posteromedial papillary muscle complex.
Keywords
Pseudoaneurysmectomy; Mitral Valve Insufficiency; Mitral Valve Tethering; Mitral Valve Replacement
Pseudoaneurysmectomy articles, Mitral Valve Insufficiency articles, Mitral Valve Tethering articles, Mitral Valve Replacement articles
Pseudoaneurysmectomy articles Pseudoaneurysmectomy Research articles Pseudoaneurysmectomy review articles Pseudoaneurysmectomy PubMed articles Pseudoaneurysmectomy PubMed Central articles Pseudoaneurysmectomy 2023 articles Pseudoaneurysmectomy 2024 articles Pseudoaneurysmectomy Scopus articles Pseudoaneurysmectomy impact factor journals Pseudoaneurysmectomy Scopus journals Pseudoaneurysmectomy PubMed journals Pseudoaneurysmectomy medical journals Pseudoaneurysmectomy free journals Pseudoaneurysmectomy best journals Pseudoaneurysmectomy top journals Pseudoaneurysmectomy free medical journals Pseudoaneurysmectomy famous journals Pseudoaneurysmectomy Google Scholar indexed journals Mitral Valve Insufficiency articles Mitral Valve Insufficiency Research articles Mitral Valve Insufficiency review articles Mitral Valve Insufficiency PubMed articles Mitral Valve Insufficiency PubMed Central articles Mitral Valve Insufficiency 2023 articles Mitral Valve Insufficiency 2024 articles Mitral Valve Insufficiency Scopus articles Mitral Valve Insufficiency impact factor journals Mitral Valve Insufficiency Scopus journals Mitral Valve Insufficiency PubMed journals Mitral Valve Insufficiency medical journals Mitral Valve Insufficiency free journals Mitral Valve Insufficiency best journals Mitral Valve Insufficiency top journals Mitral Valve Insufficiency free medical journals Mitral Valve Insufficiency famous journals Mitral Valve Insufficiency Google Scholar indexed journals Mitral Valve Tethering articles Mitral Valve Tethering Research articles Mitral Valve Tethering review articles Mitral Valve Tethering PubMed articles Mitral Valve Tethering PubMed Central articles Mitral Valve Tethering 2023 articles Mitral Valve Tethering 2024 articles Mitral Valve Tethering Scopus articles Mitral Valve Tethering impact factor journals Mitral Valve Tethering Scopus journals Mitral Valve Tethering PubMed journals Mitral Valve Tethering medical journals Mitral Valve Tethering free journals Mitral Valve Tethering best journals Mitral Valve Tethering top journals Mitral Valve Tethering free medical journals Mitral Valve Tethering famous journals Mitral Valve Tethering Google Scholar indexed journals Mitral Valve Replacement articles Mitral Valve Replacement Research articles Mitral Valve Replacement review articles Mitral Valve Replacement PubMed articles Mitral Valve Replacement PubMed Central articles Mitral Valve Replacement 2023 articles Mitral Valve Replacement 2024 articles Mitral Valve Replacement Scopus articles Mitral Valve Replacement impact factor journals Mitral Valve Replacement Scopus journals Mitral Valve Replacement PubMed journals Mitral Valve Replacement medical journals Mitral Valve Replacement free journals Mitral Valve Replacement best journals Mitral Valve Replacement top journals Mitral Valve Replacement free medical journals Mitral Valve Replacement famous journals Mitral Valve Replacement Google Scholar indexed journals Haemodynamic articles Haemodynamic Research articles Haemodynamic review articles Haemodynamic PubMed articles Haemodynamic PubMed Central articles Haemodynamic 2023 articles Haemodynamic 2024 articles Haemodynamic Scopus articles Haemodynamic impact factor journals Haemodynamic Scopus journals Haemodynamic PubMed journals Haemodynamic medical journals Haemodynamic free journals Haemodynamic best journals Haemodynamic top journals Haemodynamic free medical journals Haemodynamic famous journals Haemodynamic Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals echocardiography articles echocardiography Research articles echocardiography review articles echocardiography PubMed articles echocardiography PubMed Central articles echocardiography 2023 articles echocardiography 2024 articles echocardiography Scopus articles echocardiography impact factor journals echocardiography Scopus journals echocardiography PubMed journals echocardiography medical journals echocardiography free journals echocardiography best journals echocardiography top journals echocardiography free medical journals echocardiography famous journals echocardiography Google Scholar indexed journals infusion articles infusion Research articles infusion review articles infusion PubMed articles infusion PubMed Central articles infusion 2023 articles infusion 2024 articles infusion Scopus articles infusion impact factor journals infusion Scopus journals infusion PubMed journals infusion medical journals infusion free journals infusion best journals infusion top journals infusion free medical journals infusion famous journals infusion Google Scholar indexed journals patient articles patient Research articles patient review articles patient PubMed articles patient PubMed Central articles patient 2023 articles patient 2024 articles patient Scopus articles patient impact factor journals patient Scopus journals patient PubMed journals patient medical journals patient free journals patient best journals patient top journals patient free medical journals patient famous journals patient Google Scholar indexed journals
Article Details
1. Case Report
A 48-year-old man presented with symptoms of progressive biventricular congestive heart failure despite medical therapy. The patient had attempted suicide by jumping out of a window thirty years previously, for which he received lung and hepatosplenic surgery. On admission, the chest X-ray showed cardiomegaly and pulmonary congestion. A transthoracic echocardiography (TTE) (Figure 1) showed an LV with a posterolateral pseudoaneurysm (75 × 55 mm). The LA was dilated and with severe FMR due to the tethering of the MV apparatus. Additionally, a partial rupture of the posteromedial papillary muscle complex with relative PML prolapse was found. Using 3D-TEE we calculated an EROA of 0.3 cm², a RVol of 31 ml, an LVEDV of 326 ml and an LVESV of 262 ml. The forward SV, as assessed by Doppler, was 33 ml. Therefore, mitral regurgitation was defined as severe due to a regurgitant fraction of 50%.
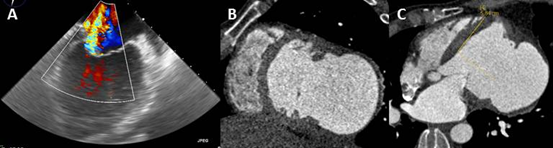
Figure 1: A) TEE showing MV regurgitation. B-C) MSCT revealing a LV-pseudoaneurysm measuring 70 × 80mm. The aneurysm defect area is 38.9 cm².
Coronary angiography confirmed a posterolateral aneurysm of the LV, left dominant supply and no coronary artery stenoses. A multislice CT-scan (Figure 1) revealed a LV pseudoaneurysm measuring 70 × 80 mm. LVEDV without aneurysm volume was 298 ml, LVESV was 219 ml and LVESVI was 113 ml/m². Diastolic aneurysm volume was 204 ml. The LVEF calculated the difference between end-diastolic and end-systolic volume to be 27%. Taking the measured echocardiographic effective forward SV of only 40.3 ml into account, the LVEF was calculated as 13%. MV morphology assessment with MSCT confirmed severe tethering of the mitral apparatus.
1.1 Operation
After a median sternotomy was performed, a previous pericardial rupture at the level of the right pulmonary veins was revealed. A pseudoaneurysmectomy was performed, followed by patch-closure (70 × 40 mm) of the aneurysmal neck according to our institutional treatment algorihthm [2]. MV replacement was performed in a standard fashion with preservation of the chordae tendinae in order to maintain the normal geometry of the mitral subvalvular apparatus. CPB-time, X-clamp-time, and reperfusion-time were 180 min, 126 min, and 34 min, respectively.
1.2 Postoperative course
The postoperative recovery was uneventful. TTE at the time of discharge revealed a LVEDD of 68 mm and a LVESD of 55 mm. The LVEF had improved to 30%. There was diastolic dysfunction grade I, as well as a trace of transvalvular MV and TV insufficiency of less than grade I. Postoperative computed tomographic (Figure 2) LVEDV was 252 ml, LVESV was 169 ml and LVESVI was 84 ml/m². The SV increased to 83 ml and LVEF was measured as 33%. The MRI performed 6 months later revealed a further decrease in LV dimensions with a LVEDD of 52 mm and a LVESD of 36 mm and a normalization of LV volumes and function with an LVEDV of 174 ml (LVEDVI 89.5 ml/m2) and an LVESV of 85 ml (LVESVI 43.8 ml/m2). SV was calculated as 85.2 ml, LVEF 50%, CO 5.5 l/min, and CI 3 l/min/m².
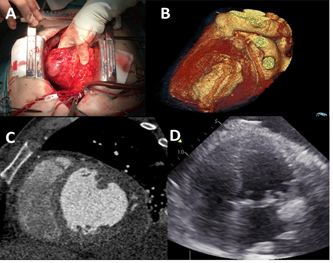
Figure 2: A) Intraoperative aneurysmal left ventricular sac. B) 3D reconstruction of the pseudoaneurysmectomy and reconstruction of the ventricle C) Postoperative CT-scan showing the reconstructed left ventricle. D) Echocardiographic follow-up cross section of the LV.
2. Discussion
LVP typically occur in adults following transmural myocardial infarction and less frequently after trauma [1-3]. Delayed presentation of an adult posttraumatic chest penetration LVP of up to 25 years has been reported, yet our patient presented 30 years after blunt trauma. In general, cardiac contusion can lead to extended myocardial damage and reverse remodelling in such a way that overall cardiac function is impaired [4]. Usually there is a complete clinical recovery with minimal residual scarring [5]. However, in some cases, softening and fibrotic replacement of the contused myocardium is followed by thinning of the scar which leads to dilatation and aneurysm formation [5]. This process may produce a true aneurysm within days or could take up to a number of years [5]. The management of concomitant MV regurgitation in the case of posterolateral LV aneurysms remains a matter of debate. MSCT and TEE are useful tools in guiding the surgical decision making.
The clinical course of patients with an untreated pseudoaneurysm is relatively poor since they have a high tendency to rupture [3]. If the diagnosis is delayed after the initial trauma, the necessity and urgency of surgery depends on the symptoms. Ventricular pseudoaneurysm following a blunt chest injury is associated with complications. These include arrhythmias, rupture, embolization, and congestive heart failure. Therefore, when symptoms are present, surgery should be performed.
Acknowledgement
We thank Anne Gale and Susan Holder for editorial assistance.
References
- Brown SL, Gropler RJ, Harris KM. Distinguishing left ventricular aneurysm from pseudoaneurysm. A review of the literature. Chest 111 (1997): 1403-1409.
- Solowjowa N, Penkalla A, Dandel M, et al. Multislice computed tomography-guided surgical repair of acquired posterior left ventricular aneurysms: demonstration of mitral valve and left ventricular reverse remodelling. Interact Cardiovasc Thorac Surg 23 (2018): 383-390.
- Currie A, Hons M, Hayes N, et al. Delayed Presentation of a Post-Traumatic Left Ventricular Pseudoaneurysm in a Child. ATS 89 (2017): 1633-1635.
- Mujanovic E, Bergsland J, Avdic S, et al. Surgical Treatment of Left Ventricular Pseudoaneurysm. Med Arch 68 (2014): 215.
- Grieco JG, Montoya A, Sullivan HJ, et al. Ventricular aneurysm due to blunt chest injury. Ann Thorac Surg 47 (1989): 322-329.
