Late Presenting Traumatic Obturator Dislocation-A Rare Case Report
Article Information
Ali Mohamed Ali1,2, Faiton Ndesanjo Mandari1,2 *
1Department of Orthopedic and Traumatology, Kilimanjaro Christian Medical Centre, Moshi, United Republic of Tanzania
2Kilimanjaro Christian Medical University College, Moshi, United Republic of Tanzania
*Corresponding Author: Faiton Ndesanjo Mandari, Department of Orthopedic and Traumatology, Kilimanjaro Christian Medical Centre, Moshi, United Republic of Tanzania; Kilimanjaro Christian Medical University College, Moshi, United Republic of Tanzania
Received: 19 July 2021; Accepted: 28 July 2021; Published: 04 August 2021
Citation: Ali Mohamed Ali, Faiton Ndesanjo Mandari. Late Presenting Traumatic Obturator Dislocation-A Rare Case Report. Journal of Orthopaedics and Sports Medicine 3 (2021): 133-139.
View / Download Pdf Share at FacebookAbstract
We describe a case of a traumatic obturator hip dislocation in a 50-year old adult male presenting three weeks after injury. All attempts at closed reduction under general anaesthesia had failed upon which open reduction was successfully accomplished using the minimally invasive anterior approach. The patient was then discharged 5 days post-op and advised to progressively weight bear with crutches as tolerated for a month with limited extension. Follow-up of the patient after 3 months showed satisfactory recovery without signs of avascular necrosis (AVN).
Keywords
Obturator dislocation; Open Reduction (approach); Anterior inferior dislocation
Traumatic hip dislocations articles Traumatic hip dislocations Research articles Traumatic hip dislocations review articles Traumatic hip dislocations PubMed articles Traumatic hip dislocations PubMed Central articles Traumatic hip dislocations 2023 articles Traumatic hip dislocations 2024 articles Traumatic hip dislocations Scopus articles Traumatic hip dislocations impact factor journals Traumatic hip dislocations Scopus journals Traumatic hip dislocations PubMed journals Traumatic hip dislocations medical journals Traumatic hip dislocations free journals Traumatic hip dislocations best journals Traumatic hip dislocations top journals Traumatic hip dislocations free medical journals Traumatic hip dislocations famous journals Traumatic hip dislocations Google Scholar indexed journals Orthopedic articles Orthopedic Research articles Orthopedic review articles Orthopedic PubMed articles Orthopedic PubMed Central articles Orthopedic 2023 articles Orthopedic 2024 articles Orthopedic Scopus articles Orthopedic impact factor journals Orthopedic Scopus journals Orthopedic PubMed journals Orthopedic medical journals Orthopedic free journals Orthopedic best journals Orthopedic top journals Orthopedic free medical journals Orthopedic famous journals Orthopedic Google Scholar indexed journals Spinal anesthesia articles Spinal anesthesia Research articles Spinal anesthesia review articles Spinal anesthesia PubMed articles Spinal anesthesia PubMed Central articles Spinal anesthesia 2023 articles Spinal anesthesia 2024 articles Spinal anesthesia Scopus articles Spinal anesthesia impact factor journals Spinal anesthesia Scopus journals Spinal anesthesia PubMed journals Spinal anesthesia medical journals Spinal anesthesia free journals Spinal anesthesia best journals Spinal anesthesia top journals Spinal anesthesia free medical journals Spinal anesthesia famous journals Spinal anesthesia Google Scholar indexed journals Osteoarthritis articles Osteoarthritis Research articles Osteoarthritis review articles Osteoarthritis PubMed articles Osteoarthritis PubMed Central articles Osteoarthritis 2023 articles Osteoarthritis 2024 articles Osteoarthritis Scopus articles Osteoarthritis impact factor journals Osteoarthritis Scopus journals Osteoarthritis PubMed journals Osteoarthritis medical journals Osteoarthritis free journals Osteoarthritis best journals Osteoarthritis top journals Osteoarthritis free medical journals Osteoarthritis famous journals Osteoarthritis Google Scholar indexed journals Traumatology articles Traumatology Research articles Traumatology review articles Traumatology PubMed articles Traumatology PubMed Central articles Traumatology 2023 articles Traumatology 2024 articles Traumatology Scopus articles Traumatology impact factor journals Traumatology Scopus journals Traumatology PubMed journals Traumatology medical journals Traumatology free journals Traumatology best journals Traumatology top journals Traumatology free medical journals Traumatology famous journals Traumatology Google Scholar indexed journals Lower limb articles Lower limb Research articles Lower limb review articles Lower limb PubMed articles Lower limb PubMed Central articles Lower limb 2023 articles Lower limb 2024 articles Lower limb Scopus articles Lower limb impact factor journals Lower limb Scopus journals Lower limb PubMed journals Lower limb medical journals Lower limb free journals Lower limb best journals Lower limb top journals Lower limb free medical journals Lower limb famous journals Lower limb Google Scholar indexed journals Blunt dissection articles Blunt dissection Research articles Blunt dissection review articles Blunt dissection PubMed articles Blunt dissection PubMed Central articles Blunt dissection 2023 articles Blunt dissection 2024 articles Blunt dissection Scopus articles Blunt dissection impact factor journals Blunt dissection Scopus journals Blunt dissection PubMed journals Blunt dissection medical journals Blunt dissection free journals Blunt dissection best journals Blunt dissection top journals Blunt dissection free medical journals Blunt dissection famous journals Blunt dissection Google Scholar indexed journals Muscle sparing articles Muscle sparing Research articles Muscle sparing review articles Muscle sparing PubMed articles Muscle sparing PubMed Central articles Muscle sparing 2023 articles Muscle sparing 2024 articles Muscle sparing Scopus articles Muscle sparing impact factor journals Muscle sparing Scopus journals Muscle sparing PubMed journals Muscle sparing medical journals Muscle sparing free journals Muscle sparing best journals Muscle sparing top journals Muscle sparing free medical journals Muscle sparing famous journals Muscle sparing Google Scholar indexed journals Rectus femoris articles Rectus femoris Research articles Rectus femoris review articles Rectus femoris PubMed articles Rectus femoris PubMed Central articles Rectus femoris 2023 articles Rectus femoris 2024 articles Rectus femoris Scopus articles Rectus femoris impact factor journals Rectus femoris Scopus journals Rectus femoris PubMed journals Rectus femoris medical journals Rectus femoris free journals Rectus femoris best journals Rectus femoris top journals Rectus femoris free medical journals Rectus femoris famous journals Rectus femoris Google Scholar indexed journals Iliocapsularis muscles articles Iliocapsularis muscles Research articles Iliocapsularis muscles review articles Iliocapsularis muscles PubMed articles Iliocapsularis muscles PubMed Central articles Iliocapsularis muscles 2023 articles Iliocapsularis muscles 2024 articles Iliocapsularis muscles Scopus articles Iliocapsularis muscles impact factor journals Iliocapsularis muscles Scopus journals Iliocapsularis muscles PubMed journals Iliocapsularis muscles medical journals Iliocapsularis muscles free journals Iliocapsularis muscles best journals Iliocapsularis muscles top journals Iliocapsularis muscles free medical journals Iliocapsularis muscles famous journals Iliocapsularis muscles Google Scholar indexed journals Joint capsule articles Joint capsule Research articles Joint capsule review articles Joint capsule PubMed articles Joint capsule PubMed Central articles Joint capsule 2023 articles Joint capsule 2024 articles Joint capsule Scopus articles Joint capsule impact factor journals Joint capsule Scopus journals Joint capsule PubMed journals Joint capsule medical journals Joint capsule free journals Joint capsule best journals Joint capsule top journals Joint capsule free medical journals Joint capsule famous journals Joint capsule Google Scholar indexed journals Fibrous tissue articles Fibrous tissue Research articles Fibrous tissue review articles Fibrous tissue PubMed articles Fibrous tissue PubMed Central articles Fibrous tissue 2023 articles Fibrous tissue 2024 articles Fibrous tissue Scopus articles Fibrous tissue impact factor journals Fibrous tissue Scopus journals Fibrous tissue PubMed journals Fibrous tissue medical journals Fibrous tissue free journals Fibrous tissue best journals Fibrous tissue top journals Fibrous tissue free medical journals Fibrous tissue famous journals Fibrous tissue Google Scholar indexed journals Muscles articles Muscles Research articles Muscles review articles Muscles PubMed articles Muscles PubMed Central articles Muscles 2023 articles Muscles 2024 articles Muscles Scopus articles Muscles impact factor journals Muscles Scopus journals Muscles PubMed journals Muscles medical journals Muscles free journals Muscles best journals Muscles top journals Muscles free medical journals Muscles famous journals Muscles Google Scholar indexed journals Ligaments articles Ligaments Research articles Ligaments review articles Ligaments PubMed articles Ligaments PubMed Central articles Ligaments 2023 articles Ligaments 2024 articles Ligaments Scopus articles Ligaments impact factor journals Ligaments Scopus journals Ligaments PubMed journals Ligaments medical journals Ligaments free journals Ligaments best journals Ligaments top journals Ligaments free medical journals Ligaments famous journals Ligaments Google Scholar indexed journals Acetabular rim articles Acetabular rim Research articles Acetabular rim review articles Acetabular rim PubMed articles Acetabular rim PubMed Central articles Acetabular rim 2023 articles Acetabular rim 2024 articles Acetabular rim Scopus articles Acetabular rim impact factor journals Acetabular rim Scopus journals Acetabular rim PubMed journals Acetabular rim medical journals Acetabular rim free journals Acetabular rim best journals Acetabular rim top journals Acetabular rim free medical journals Acetabular rim famous journals Acetabular rim Google Scholar indexed journals
Article Details
1. Introduction
Traumatic hip dislocations are true orthopedic emergencies that have been associated with long term morbidity which need prompt intervention to reduce risks of complications such as avascular necrosis and secondary osteoarthritis [1].
Majority of hip dislocations in developing countries will present late to Regional referral hospitals due to a number of factors including the healthcare referral system which is geared to work effectively in limited resource settings. This poses a problem for conditions such as hip dislocations which are very time sensitive and require early intervention for conservative approaches to be successful without complications.
2. Case Report
A 50-year old male was referred from a rural hospital, 3 weeks after sustaining injury to the left hip during an accident at work where sand from a truck was offloaded on top of him. It was shortly followed by pain and inability to use the left lower limb or bear weight.
He was then rushed to the rural hospital where attempts at closed reduction were carried out under spinal anesthesia and skeletal traction applied. A control x-ray was done three weeks after, while he was on skeletal traction which showed that prior reduction attempts had failed. He was then referred to our regional referral hospital for further management.
Primary survey was uneventful on arrival at our emergency department. He complained of inability to use his left lower limb associated with pain that is dull, constant and without any specific periodicity not associated with numbness, tingling or loss of function of his left lower limb. The patient was alert, had fair general condition and was oriented to people, place and time. Vitals were within normal range apart from an elevated BP of 161/103mmHg and a heart rate of 106bpm.
On local examination the patient’s left hip was in a fixed flexed (45°), abducted (30°) and externally rotated position (20°) with tenderness around the left hip. There was no neurovascular compromise or neurological impairment. Radiological investigations revealed a left obturator dislocation on AP view of the pelvis as shown (Figure 1).
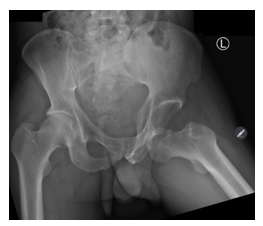
Figure 1: AP view of pelvis showing left obturator dislocation.
The patient was then admitted into the ward and planned for an open reduction. His left limb positioning in theatre can be seen in Figure 2.
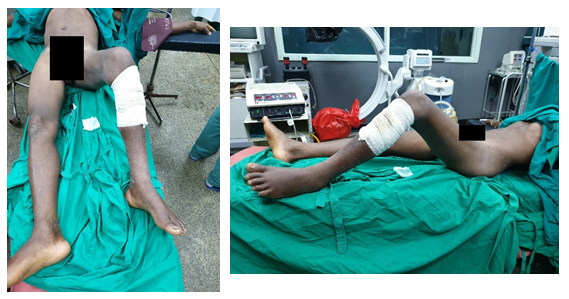
Figure 2: Position of left lower limb at rest in supine position. Hip was flexed (45°), abducted (30°) and externally rotated (20°)
In the theatre, closed reduction under general anesthesia was attempted which failed and necessitated open reduction. The anterior minimally invasive approach of the hip (Figure 3) was used where a 6cm incision was done in between the anterior superior iliac spine and the grater trochanter. Entry to the site of interest was done by blunt dissection with muscle sparing. The sartorius, rectus femoris and iliocapsularis muscles were all retracted medially to visualize the joint capsule.

Figure 3: Anterior approach to the hip used to gain access to the site of dislocation.
Intraoperatively, the observed joint capsule was thickened which necessitated capsulotomy. As nature does not allow a vacuum, there was presence of fibrous tissue inside the acetabulum which was removed and the femoral head guided away from the obturator canal to the acetabulum by manual manipulation after which reduction was achieved. Reduction was successful as shown in the figures below from shots taken by x-ray image intensifier (Figure 4). Stability of the hip was assessed which was found to be satisfactory. The wound was closed in layers after hemostasis was achieved. (Figure 5)
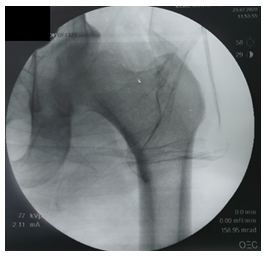
Figure 4: Image showing successful reduction intraoperatively using x-ray image intensifier (C-arm).
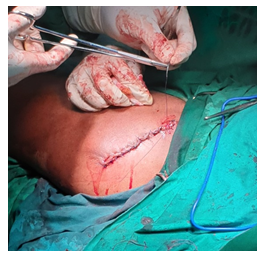
Figure 5: Image showing primary closure of surgical incision.
After the surgery, the patient was discharged as soon as the control x-ray was done (day 5). Post-operative radiographs show a successful reduction (Figure 6) with mild deformity of the femoral head. Patient was then discharged after three weeks to return for follow-up at the orthopedic clinic after two (2) weeks and subsequently at three (3) month intervals or if any new complaints arise before the booked consultation date.
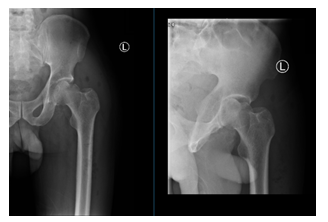
Figure 6: 48-hour Post-operative AP views of the hip showing successful reduction.
At 3 months follow-up the patient was doing well, could walk unassisted and could perform all his activities of daily living without limitation or pain. Range of motion on all axes was normal and the patient was satisfied with the outcome. Serial hip radiograph taken 3 months after was done as shown below (Figure 7).

Figure 7: 3-month post-operative radiographs.
3. Discussion
The hip is a ball and socket joint that has intrinsic stability which is reliant on its depth and support from the joint capsule and surrounding muscles and ligaments. Dislocations of the hip can be classified according to anterior or posterior depending on the displacement of the femoral head relative to the acetabular wall. Posterior Dislocations are the most common (90% of cases) [2] owing to the relative strength of the anterior ligaments stabilizing the hip joint compared to the posterior ones. Epstein classified anterior dislocations into Type A and Type B which are superior (pubic) and inferior (obturator) respectively [3]. This classification was modified by Rockwood and Green into Type 1 - Superior (pubic and subspinous) and Type 2 - Inferior (obturator and perineal) [4].
An obturator dislocation however is considered by a majority of scholars to be a distinct subset due to its rarity, due to the different approach used during reduction of such dislocations when compared to other types of anterior dislocations. The mechanism of injury of obturator dislocations occur from forced abduction, external rotation and flexion of the hip joint with the neck of the femur acting as a fulcrum across the posterosuperior region of the acetabular rim [5]. This is often seen in motor vehicle crashes or falls.
Closed reduction attempts under general anesthesia are considered the treatment of choice for simple dislocations on cases presenting acutely. It should be done preferably done within 6 hours of injury as incidence of AVN increases by 10 fold for reductions done longer than 6 hours [6]. It involves applying traction in line with the femur while slowly flexing the hip followed by gentle internal rotation and adduction with gradual release of longitudinal traction [7]. Further modifications proposed use of a traction table to avoid anesthetizing the patient on the floor [8]. Surgical intervention should only be employed for refractory cases using an Iliofemoral or Ilio-inguinal approach with release of rectus femoris [8]. The approach used in our case necessitated the anterior minimally invasive approach with muscle sparing due to the already compromised bloody supply to the femoral head from the very late presentation. The anterior approach has been shown to be superior to the posterior approach with regards to better respect to soft tissues and better postoperative outcomes albeit requires a high technical competence to avoid its catastrophic complications [9].
Previous post reduction plans involved traction for 3-6 weeks for simple dislocations to give time for capsular healing followed by mobilization with progressive loading [10, 11]. However, recent studies showed that early mobilization in an extension limiting brace avoided all the complications of prolonged immobilization without any increased risk of redislocation or AVN [12].
Follow-up should be done at a minimum of 2 years after hip dislocation with serial radiographs taken every 3 months for the first year followed by 6 months intervals during the second year due to risk of secondary osteoarthritis and AVN.
Counselling on early signs preluding to these conditions must be thoroughly explained to the patient so they can return to the outpatient clinic for further investigations and management.
Acknowledgements
We would like to thank the patient for the participation and approval for the publication of this case report. We would also like to thank Kilimanjaro Christian Medical Centre for allowing us to work closely with our patient and for disclosing all the necessary documents enclosed in the case file.
Conflicts of Interest
Kilimanjaro Christian Medical Centre (KCMC) and Kilimanjaro Christian Medical University College (KCMUCo) as part of the Good Samaritan Foundation receives grants and financial aid from various charitable organizations. They declare that there is no conflict of interest in the publication of this article.
Funding
This research received no funding from any private or government agency.
References
- Brooks RA, Ribbans WJ. Diagnosis and imaging studies of traumatic hip dislocations in the adult. Clin Orthop Relat Res 377 (2000): 15-23.
- Clegg TE, Roberts CS, Greene JW, et al. Hip dislocations--epidemiology, treatment, and outcomes. Injury 41 (2010): 329-334.
- Epstein HC, Wiss DA. Traumatic anterior dislocation of the hip. Orthopedics 8 (1985): 130, 132-134.
- Rockwood and Green. Fractures in adults. Fourth ed. Lippincott, Williams and Wilkins 2: 1756-1763.
- Endo S, Hoshi S, Takayama H, et al. Traumatic bilateral obturator dislocation of the hip joint. Injury 22 (1991): 232-233.
- Hougaard K, Thomsen PB. Traumatic posterior dislocation of the hip--prognostic factors influencing the incidence of avascular necrosis of the femoral head. Arch Orthop Trauma Surg 106 (1986): 32-35.
- Epstein HC. Traumatic dislocations of the hip. Clin Orthop Relat Res 92 (1973): 116-142.
- Toms AD, Williams S, White SH. Obturator dislocation of the hip. J Bone Joint Surg Br 83 (2001): 113-115.
- Kyriakopoulos G, Poultsides L, Christofilopoulos P. Total hip arthroplasty through an anterior approach: The pros and cons. EFORT Open Rev 3 (2018): 574-583.
- Mowery C, Gershuni DH. Fracture dislocation of the femoral head treated by open reduction and internal fixation. J Trauma 26 (1986): 1041-1044.
- Amihood S. Anterior dislocation of the hip. Injury 7 (1975): 107-110.
- Schlickewei W, Elsässer B, Mullaji AB, et al. Hip dislocation without fracture: traction or mobilization after reduction? Injury 24 (1993): 27-31.
