Knowledge of Pregnant Women in Rural Mozambique on Routine Practices to Prevent and Treat Common Conditions at the Antenatal Care Clinic
Article Information
Tacilta Nhampossa1,2*, Khatia Munguambe1,3, Celia Chauque3, Mariza Chivangue1, Maura Mazuze1, Anete Mendes1,Laura Garcia-Otero1,4, Raquel Gonzalez1,4,5 , Esperanca Sevene1,3, Clara Menendez1,4,5, Neusa Torres1
1Centro de Investigacao em Saude de Manhica(CISM), Maputo, Mozambique
2Instituto Nacional de Saude (INS), Ministerio de Saude, Maputo, Mozambique
3Universidade Eduardo Mondlane (UEM),Faculdade de Medicina, Maputo, Mozambique
4Barcelona Institute for Global Health (ISGlobal), Barcelona, Spain, Hospital Clinic-Barcelona University
5Consorcio de Investigacion Biomedica en Red de Epidemiologia y Salud Publica (CIBERESP)
*Corresponding author:Tacilta Nhampossa, Centro de Investigacao em Saude de Manhica (CISM), Vila da Manhica, Rua 12, PO Box 1929, Maputo, Mozambique
Received: February 24, 2023;Accepted: February 27, 2023; Published: March 04, 2023;
Citation: Tacilta Nhampossa, Khátia Munguambe, Célia Chauque, Mariza Chivangue, Maura Mazuze, Anete Mendes, Laura Garcia-Otero1,4, Raquel Gonzalez, Esperança Sevene, Clara Menendez, Neusa Torres. Knowledge of pregnant women in rural Mozambique on routine practices to prevent and treat common conditions at the antenatal care clinic. Obstetrics and Gynecology Research. 6 (2023): 88-99
View / Download Pdf Share at FacebookAbstract
Background:
Despite an increasing proportion of pregnant women accessing antenatal care (ANC) in low-income countries, preventable maternal morbidity and mortality remains high. Limited women’s knowledge on common diseases during pregnancy and on the indications of routine health interventions delivered at the ANC clinic may reduce the compliance and effectiveness of these interventions. We assessed pregnant women’s knowledge on common diseases in pregnancy and on routine interventions delivered at the ANC clinic as well as their compliance with these interventions.
Material & Methods:
From December-2019 to October-2020, we undertook a qualitative study using individual semi-structured and indepth interviews in 79 pregnant women attending the ANC clinic of a rural hospital in Mozambique. Participant’s ability to identify the drugs administrated was assessed by showing them the drugs without the label (antiretroviral, ferrous sulfate, cotrimoxazole, isoniazid, mebendazol and antimalarial). Interviews were recorded, transcribed, coded and a combined Content and Thematic analysis technique used. NVivo 12 software was used to store and retrieve the data.
Results:
Most of the participants recognized that infectious diseases such as HIV, malaria, sexually transmitted infections, tuberculosis and COVID-19, could be harmful in pregnancy. Overall, knowledge on the indication of the prescribed drugs was limited, being higher for antiretroviral drugs and ferrous sulfate, and lower for mebendazol and isoniazid. The general perception was that all drugs prescribed at the ANC clinic prevent or treat malaria infection. Knowledge on the indication of the prescribed drugs was generally higher in HIV-infected pregnant women compared to HIV uninfected women. Forgetting daily medication intake, non-compliance with the drug intake schedule and perceived importan
Keywords
Pregnancy; Mozambique; HIV; Malaria; COVID-19; Pharmacological Interventions
Pregnancy articles Pregnancy Research articles Pregnancy review articles Pregnancy PubMed articles Pregnancy PubMed Central articles Pregnancy 2023 articles Pregnancy 2024 articles Pregnancy Scopus articles Pregnancy impact factor journals Pregnancy Scopus journals Pregnancy PubMed journals Pregnancy medical journals Pregnancy free journals Pregnancy best journals Pregnancy top journals Pregnancy free medical journals Pregnancy famous journals Pregnancy Google Scholar indexed journals Mozambique articles Mozambique Research articles Mozambique review articles Mozambique PubMed articles Mozambique PubMed Central articles Mozambique 2023 articles Mozambique 2024 articles Mozambique Scopus articles Mozambique impact factor journals Mozambique Scopus journals Mozambique PubMed journals Mozambique medical journals Mozambique free journals Mozambique best journals Mozambique top journals Mozambique free medical journals Mozambique famous journals Mozambique Google Scholar indexed journals HIV articles HIV Research articles HIV review articles HIV PubMed articles HIV PubMed Central articles HIV 2023 articles HIV 2024 articles HIV Scopus articles HIV impact factor journals HIV Scopus journals HIV PubMed journals HIV medical journals HIV free journals HIV best journals HIV top journals HIV free medical journals HIV famous journals HIV Google Scholar indexed journals Malaria articles Malaria Research articles Malaria review articles Malaria PubMed articles Malaria PubMed Central articles Malaria 2023 articles Malaria 2024 articles Malaria Scopus articles Malaria impact factor journals Malaria Scopus journals Malaria PubMed journals Malaria medical journals Malaria free journals Malaria best journals Malaria top journals Malaria free medical journals Malaria famous journals Malaria Google Scholar indexed journals COVID-19 articles COVID-19 Research articles COVID-19 review articles COVID-19 PubMed articles COVID-19 PubMed Central articles COVID-19 2023 articles COVID-19 2024 articles COVID-19 Scopus articles COVID-19 impact factor journals COVID-19 Scopus journals COVID-19 PubMed journals COVID-19 medical journals COVID-19 free journals COVID-19 best journals COVID-19 top journals COVID-19 free medical journals COVID-19 famous journals COVID-19 Google Scholar indexed journals Pharmacological Interventions articles Pharmacological Interventions Research articles Pharmacological Interventions review articles Pharmacological Interventions PubMed articles Pharmacological Interventions PubMed Central articles Pharmacological Interventions 2023 articles Pharmacological Interventions 2024 articles Pharmacological Interventions Scopus articles Pharmacological Interventions impact factor journals Pharmacological Interventions Scopus journals Pharmacological Interventions PubMed journals Pharmacological Interventions medical journals Pharmacological Interventions free journals Pharmacological Interventions best journals Pharmacological Interventions top journals Pharmacological Interventions free medical journals Pharmacological Interventions famous journals Pharmacological Interventions Google Scholar indexed journals Antenatal Care articles Antenatal Care Research articles Antenatal Care review articles Antenatal Care PubMed articles Antenatal Care PubMed Central articles Antenatal Care 2023 articles Antenatal Care 2024 articles Antenatal Care Scopus articles Antenatal Care impact factor journals Antenatal Care Scopus journals Antenatal Care PubMed journals Antenatal Care medical journals Antenatal Care free journals Antenatal Care best journals Antenatal Care top journals Antenatal Care free medical journals Antenatal Care famous journals Antenatal Care Google Scholar indexed journals Antiretroviral Therapy articles Antiretroviral Therapy Research articles Antiretroviral Therapy review articles Antiretroviral Therapy PubMed articles Antiretroviral Therapy PubMed Central articles Antiretroviral Therapy 2023 articles Antiretroviral Therapy 2024 articles Antiretroviral Therapy Scopus articles Antiretroviral Therapy impact factor journals Antiretroviral Therapy Scopus journals Antiretroviral Therapy PubMed journals Antiretroviral Therapy medical journals Antiretroviral Therapy free journals Antiretroviral Therapy best journals Antiretroviral Therapy top journals Antiretroviral Therapy free medical journals Antiretroviral Therapy famous journals Antiretroviral Therapy Google Scholar indexed journals Maternal mortality articles Maternal mortality Research articles Maternal mortality review articles Maternal mortality PubMed articles Maternal mortality PubMed Central articles Maternal mortality 2023 articles Maternal mortality 2024 articles Maternal mortality Scopus articles Maternal mortality impact factor journals Maternal mortality Scopus journals Maternal mortality PubMed journals Maternal mortality medical journals Maternal mortality free journals Maternal mortality best journals Maternal mortality top journals Maternal mortality free medical journals Maternal mortality famous journals Maternal mortality Google Scholar indexed journals gestational hypertension articles gestational hypertension Research articles gestational hypertension review articles gestational hypertension PubMed articles gestational hypertension PubMed Central articles gestational hypertension 2023 articles gestational hypertension 2024 articles gestational hypertension Scopus articles gestational hypertension impact factor journals gestational hypertension Scopus journals gestational hypertension PubMed journals gestational hypertension medical journals gestational hypertension free journals gestational hypertension best journals gestational hypertension top journals gestational hypertension free medical journals gestational hypertension famous journals gestational hypertension Google Scholar indexed journals
Article Details
List of abbreviations:
ANC: Antenatal Care; ART: Antiretroviral Therapy; ARV: Antiretroviral; CISM: Centro de Investigação em Saúde de Manhiça; CTXp: Cotrimoxazole Prophylaxis; DSS: Demographic and Health Surveillance System
INTRODUCTION
Maternal mortality rate in Mozambique has dropped from 408 per 100,000 births in 2011 to 289 deaths per 100,000 births in 2017, as result of the considerable improvement during the last years, in coverage of antenatal care (ANC) and institutional deliveries, as well as in the management of obstetric complications and underlying diseases [1]. However, the maternal mortality ratio remains unacceptably high within the country [1,2]. Obstetric hemorrhage, gestational hypertension and infections, such as malaria and HIV/AIDS are among the main causes of maternal mortality and morbidly in Mozambique with a significant number of deaths occurring at health facilities [3–5]. Other contributory of maternal deaths and not directly related to pregnancy, include inadequate human resource for health, delay in seeking care, inadequate equipment, lack of transport, and delay in referrals services [6].
In Mozambique, at the ANC clinic, HIV-infected pregnant women (HIVPW) receive lifelong antiretroviral therapy (ART) plus ferrous-sulfate combined with folic acid for treatment and prevention of anaemia and fetal malformations, cotrimoxazole prophylaxis (CTXp) to prevent opportunistic infections and isoniazid prophylaxis to preventive tuberculosis (TB) [7]. The latter implies, on average, self-administration of four to five tablets from different medications daily during the pregnancy course, which can lead to errors in drug administration and lack of treatment adherence [8,9]. On the other hand, management of HIV-uninfected pregnant women (No-HIVPW) also includes ferrous-sulfate combined with folic acid and intermittent preventive treatment (IPTp) of malaria with sulfadoxine-pyrimethamine [10]. In addition, all women receive mebendazol for deworming at first ANC clinic visit, and other drugs may be prescribed depending on the occurrence of other diseases such as urinary infections, sexually transmitted diseases (STDs) or non-communicable diseases [11,12].
Beyond their clinical efficacy, the effectiveness of the above interventions depends on several factors, including attitudes, behaviour and knowledge of pregnant women and the wider community, which are shaped by social and cultural factors [13]. We hypothesized that limited knowledge on common diseases during pregnancy and on the indications of routine health interventions delivered at the ANC clinic might reduce the compliance and effectiveness of these interventions. In fact, a study conducted in Eswatini revealed that 90% of breastfeeding mothers living with HIV who presented high knowledge of prevention of mother to child transmission (PMTCT) strategies, demonstrated a positive attitude and behaviour towards them [14]. In contrast, a study conducted in Southern Ethiopia has reported that despite pregnant mothers’ knowledge and attitude about malaria and insecticide-treated bed nets (ITNs) was considered fairly good, insecticide-treated nets ownership and utilization was noticeably very low [15]. In addition, there is evidence that illiteracy and misinformation may lead to non-compliance to a recommended measure [16,17]. Therefore, research on knowledge on diseases is a critical step to identify the factors that may be affecting effectiveness of preventive and pharmacological interventions for this same disease [18,19].
In this study we aimed to assess Mozambican HIVPW and No-HIVPW’s awareness of common diseases in pregnancy and their ability to identify and acknowledge the indication of pharmacological interventions delivered at the ANC clinic as well as their compliance with these interventions.
Material & methods
Study design
This is a qualitative descriptive study which included in-depth and semi-structured exit interviews to HIVPW and No-HIVPW attending the ANC clinics of the Manhiça district Hospital (MDH), in southern Mozambique.
Study Setting
The Manhiça District is located 80 kilometers north away from the capital city, Maputo. The Manhiça Health Research Centre (CISM) runs a demographic surveillance system (DSS) since 1996, involving intensive and regular monitoring of a population of about 216,000 inhabitants in covering the entire district an area of around 2891.1 km2 [20,21]. There are 21 healthcare centers, of them, one is a rural hospital, Xinavane Rural Hospital and another one is a referral district hospital, Manhiça District Hospital (MDH). Overall, the coverage of first ANC clinic visit attendance within the district is high (90-93%) but it tends to decrease in subsequent visits [22]. Pregnant women are managed according to Mozambican national guidelines [7,23]. The area is endemic for malaria and the community prevalence of HIV is as high as 30% at ANC [24,25]. Retention on HIV care is a challenge. At the end of 2019, the country reported that among the 97% of all HIVPW receiving ART at ANC clinics, only 77% and 83% were retained in care at 33 days and 99 days, respectively [22]. The completion of this study coincided with the start of the COVID-19 pandemic in Mozambique [26].
Sampling and recruitment strategies
An intentionally non-probabilistic sampling was followed to enroll study participants. Health care workers and nurses working at the ANC from the MDH, supported the team to identify study candidates from women attending their first ANC clinic visit. HIVPW and No-HIVPW were informed about the study objective and invited to undergo the study semi-structured exit interview. Those willing to participate were asked to sign the study informed consent. HIVPW were all participants of an ongoing clinical trial aiming at assessing the efficacy and safety of an antimalarial drug for malaria prevention during pregnancy [27]. Ten women from each group (HIVPW and No- HIVPW) were also invited to participate in the in-depth study interviews. Although the determination of sample size in qualitative studies does not necessarily follow quantitative study models, for this study a sample size was calculated. This was due to the fact that the semi-structured exit interviews would generate quantifiable constructs, and for that the exit interviews were subjected to a sample size calculation of 10% of the number of HIVPW expected to be enrolled in the on-going clinical trial in Mozambique (444 participants). In order to capture visits information related to No- HIVPW, a final sample size was defined by saturation in the subgroup of No- HIVPW.
Data collection and analysis
Using semi-structured exit interviews, the following thematic areas were explored i) the awareness of common diseases during pregnancy, ii) the awareness of the most severe diseases during pregnancy, iii) the ability to distinguish the different drugs prescribed at ANC, iv) the knowledge of the indication of the pharmacological interventions implemented at ANC and v) home compliance to drugs prescribed at ANC. We assessed the participant’s ability to identify the drugs administrated at the ANC by showing the drugs (antiretroviral, ferrous sulfate, cotrimoxazole, isoniazid, mebendazol and fansidar) to the participants, as they were delivered at ANC but without any drug label with the exception of antiretroviral drugs (Figure 1). While we considered “awareness of diseases in pregnancy” if the pregnant women mentioned at least one of the most common and severe diseases in pregnancy, “Accurate knowledge of the indication of pharmacological interventions” was considered if the pregnant woman just gave the correct answer for questions related to knowledge of the indication of each pharmacological interventions (each drug). Home compliance to the drugs prescribed at ANC was explored through in-depth interviews with specific question about forgetting daily medication, non-complying with drug intake schedule and perceived importance given to some drugs. All the interviews were conducted by trained social scientists in the preferred language of the participants. The interviews were recorded after participant’s permission using digital voice recorders, followed the interviews verbatim transcription in MS Word, mostly by the same team members who collected the data. The social sciences team leader performed the data quality checks by reviewing the transcripts while listening to the audio recording. The transcripts were then imported to NVivo version 12 (QSR International Pty. Ltd. 2015) Software. We performed combined Content and Thematic analysis technique through the following steps: generating categories, coding text according to each category; annotating emerging themes and patterns and readjusting the categories and relationships between them [28]. The research team conducted the coding of all Portuguese transcripts at CISM.

Figure 1: Tray containing prescribed medication given to HIV infected and uninfected pregnant women at antenatal care without any identification which were used for women to identify them
Ethics approval and consent to participate
This study was approved by the National Bioethics Committee of Mozambique (311/CNBS/19). After informing the objectives and characteristics of the study, a written informed consent was obtained from each participant. One copy of the consent form was left with the participating women.
Results
The study was conducted from December 2019 to October 2020. A total of 44 HIVPW and 35 No-HIVPW were included in the study.
Socio-demographic and clinical characteristics of the study population
The socio-demographic and clinical characteristics of study participants during the first ANC visit are shown in Table 1. The median age of the women was 27 (IQT 21-32). Fifty-two women (65.8%) were unofficially married and the Christian-Zion was the religion with more believers among the participants. The median gestational age of women was 16 weeks (IQT 13-19) and the median of live children per women was four (IQT 4-5). Fifty-six women (71%) were housewives and 13% had no formal school education (no education or did not complete primary education).
|
Variable |
N (%) |
|
|
Age (years): median (IQR) |
27 (21-32) |
|
|
Age group |
<20 |
11 (14) |
|
20-24 |
20 (25) |
|
|
25-34 |
35 (44) |
|
|
>35 |
13 (17) |
|
|
Education |
No formal education |
10 (13) |
|
Primary |
46 (58) |
|
|
Secondary |
22 (28) |
|
|
University |
1 (1) |
|
|
Religion |
Christian (Zion) |
34 (43) |
|
Christian (Assembly of God) |
16 (20) |
|
|
Christian (Others) |
26 (33) |
|
|
Atheist |
3 (4) |
|
|
Marital status |
Married (in facto union) |
51 (65) |
|
Single |
28 (35) |
|
|
Occupation |
Housewife/Unemployed |
56 (71) |
|
Self-employed (sales woman) |
16 (20) |
|
|
Formally employed |
6 (9) |
|
|
Gestacional age (months): median (IQR) |
4 (4-5) |
|
|
Children currently alive: median (IQR) |
4 (4-5) |
|
|
HIV infection |
Yes |
44 (58) |
|
No |
35 (42) |
|
Table 1: Basic characteristics of interviewed pregnant women at the enrolment
Pregnant women’s knowledge about common diseases during pregnancy
Most women from both HIVPW as well as No-HIVPW groups, mentioned HIV, malaria, STDs, TB and non-specific pain as the most common diseases during pregnancy. A minority (5/79) of women mentioned also anemia and arterial hypertension.
“The diseases I know most about during pregnancy, in a pregnant woman, are HIV, tuberculosis, syphilis, malaria hummmm [calling to mind] … bladder pain.” (HIVPW, 29 years old)
“They may have malaria…they may have HIV. Sometimes a pregnant women come out with a vaginal discharge.” (No-HIVPW, 26 years old)
Very few pregnant women (9/79) reported not knowing any of the most common diseases in pregnancy.
“hummmm [calling to mind], diseases…depends on the person……I don't know because it [referring to diseases] has never happened to me….” (HIVPW, 30 years old)
Compared to No-HIVPW, the HIVPW were aware of many more diseases that may occur during pregnancy (Figure 2).
Common diseases
All pregnant women HIV infected pregnant women
HIV uninfected pregnant women
Severe diseases
All pregnant women HIV infected pregnant women
HIV uninfected pregnant women
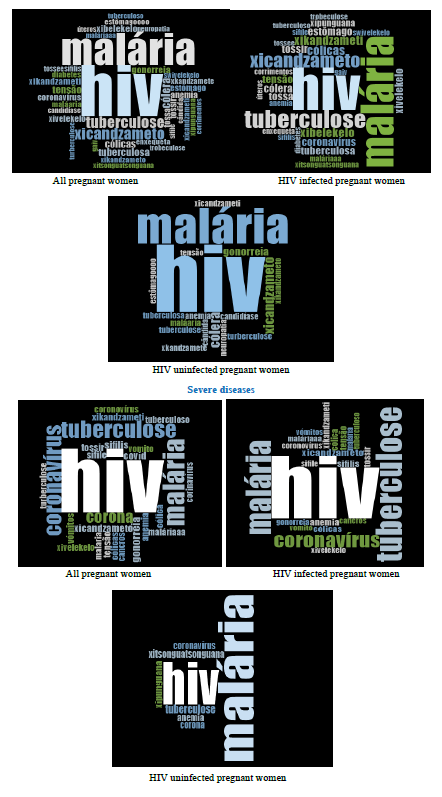
Figure 2: Pregnancy common and severe diseases reported by pregnant women
Pregnant women’s knowledge about the most severe diseases during pregnancy
Pregnant women were also asked to mention the diseases they considered to be the most serious in pregnancy. That is, the realization that a disease can have serious consequences. The HIVPW consider HIV, malaria, STDs, TB and COVID-19 as the most serious diseases during pregnancy, while the No-HIVPW mentioned only HIV, malaria and COVID-19.
For clarity purposes, we have grouped and presented below, the perceived concerns of the first two diseases considered by pregnant women to be the most serious in pregnancy, which at the same time were the focus diseases of the ongoing clinical trial. In addition, despite being a relatively new disease, we presented the participants ‘perceptions about COVID-19 because this was raised as an emergent relevant theme.
Perceived concerns on HIV infection
The perceived risk of transmitting HIV to the baby was the most commonly mentioned concern for all women regardless of HIV infection status.
“It worries me because the child may be at risk of being infected. The baby will not be born with lack of organs but it will not be a child with a pleasant appearance…. It is as they say (Referring to the health providers). We have to take HIV pills, if you refuse and do not follow, the child is born looking not pleasant, even any person can pick him up and see that, really the child is not there pleasant, starting from the pregnancy for not doing the follow-up.” (HIVPW, 35 years old)
“Because it (referring to HIV) can infect my child.” (No-HIVPW, 22 years old)
Other concerns differed according to the pregnant woman's HIV infection status. The risk of the disease leading to the women death constitutes the concern among HIVPW. On the other hand, No-HIVPW stated that they would not be able to endure taking antiretroviral on a daily basis and for the rest of their life and the stigma of being marked as HIV positive.
“Because if you have this disease (referring to HIV), if you don't comply with the medication, you will leave [die] now.” (HIVPW, 27 years old)
“uhh [coughing] because I don't want to be the sick one.” (Referring to the stigma of being marked as HIV positive) (No-HIVPW, 23 years old)
Another No-HIVPW considered the fact that she was too young to have the disease.
“It worries me because I'm still a child. I still have a future; I still want to live.” (No-HIVPW, 22 years old)
Perceived concerns on malaria infection
Regarding malaria, the perceived risks concerns varied according to the pregnant woman's HIV infection status. The HIVPW mentioned maternal death, congenital malaria and miscarriage as consequences of malaria.
“Because malaria kills. Yes, it kills when no…if it is not answered immediately.” (HIVPW, 23 years old)
“Because it (referring to malaria) can abort the pregnancy.” (HIVPW, 29 years old)
Questioned about malaria perceived risks concerns, some No-HIVPW mentioned fear and feeling vulnerable to the disease but were unable to mention severity markers or consequences.
“Interviewer: Malaria. Why are you worried? What makes you afraid of malaria?
Respondent: [silence].
Interviewer: You don't know why you are afraid, but you know that you are afraid of malaria. You don't know why the fear?
Respondent: [silence].” (No-HIVPW, 31 years old)
“And malaria for a pregnant woman is not good. It's dangerous.” (No-HIVPW, 23 years old)
“I'm afraid of malaria because I might have it because there are many mosquitoes.” (No-HIVPW, 38 years old)
Perceived concerns on COVID-19
In relation to COVID-19, perceived risks concerns include easy transmission from individual to individual, non-existence of a curative treatment, risk of death and the fact that it was not known how it could affect the baby.
“It (referring to COVID-19) worries me because I'm not in a normal state…. I'm pregnant...... and this is a heavy disease for me to bear and they (Referring to the health providers) say that for us pregnant women, the disease is serious and easy to catch” (HIVPW, 29 years old)
“…heyshi [worry] coronavirus, its transmission is also easy…it scares me. In the case of buying something… because of the money… if you took the money if you forget to pass the alcon [alcohol] your fingers; the disease is already there. So hey it's a disease hum [laughs and worry] …now hum [worry] corona-vi…as [coronavirus] it's a pandemic for which …the medicine isn't known correctly…” (No-HIVPW, 37 years old)
“Well, it's just that we don't know, or at least the news doesn’t even know… They (Referring to the health providers) don't know how this disease can affect a pregnant woman.” (No-HIVPW, 28 years old)
Pregnant women’s ability to recognize the drugs prescribed at the ANC
Overall, few women were able to identify the drugs by their real names at the first look, at the same time, most of them use an assigned name to identify them (Table 2). Moreover, the results evidence that the interviewed women used the container, format, color, size, stamping and perceived adverse effects based on previous personal experience or that of a relative, to identify the drugs administrated at ANC.
“Because my sister took these pills (referring to antiretroviral drugs)… hummmm [reminding herself] but she died. [Cough]. It's just that she had HIV disease and they gave her those pills.” (HIVPW, 36 years)
“Because when I'm pregnant they always give me these (referring to ferrous-sulphate).” (HIVPW, 36 years old)
“I know them (referring to ferrous-sulphate), but I have a problem that when I take it, it doesn't do me any good… I feel a hunger that is not worth it.” (HIVPW, 22 years old)
|
Medication |
Assigned names (reported by pregnant women) |
|
Ferrous sulfate |
Multivitamin |
|
Fansidar (Sulfadoxine Pyrimethamine) |
Paracetamol (acetaminophen) |
|
Antiretroviral |
HIV pills |
|
Pills to sleep HIV |
|
|
Amoxicillin |
|
|
Cotrimoxazole |
Paracetamol (acetaminophen) |
|
Headache pills |
|
|
Malaria pills |
|
|
Cough pills |
|
|
Isoniazid |
Cotrimoxazole |
|
Mebendazol |
Roundworms |
|
To chew pills |
|
|
Malaria |
|
|
HIV pills |
Table 2: Assigned names to different medication administered in the antenatal care visit
It is noteworthy the fact that antiretroviral drugs are commonly called HIV pills or just antiretroviral but never by its generic name (Table 2).
“They are antiretroviral.” (HIVPW, 32 years old)
“They are HIV pills.” (HIVPW, 18 years old)
Ferrous-sulphate was the drug most frequently identified by its real name, by both groups of pregnant women. In addition, this pill was identified by its red color.
“Because I saw [laughs] because they're red.” (HIVPW, 27 years old)
“I see because it's red.” (No-HIVPW, 38 years old)
“They are ferrous-sulphate.” (HIVPW, ageless)
“They say they are ferrous-sulphate.” (No-HIVPW, 32 years old)
Mebendazol and fansidar tablets administered under direct observation at the ANC visit room together with isoniazid were the least recognized at the first look and the least identified by their real name.
“Hihhh [hesitation], the name I don't know.” (Referring to mebendazol). (HIVPW, 35 years old)
“I don't know the name, it's just that they gave me to prevent malaria, for the baby.” (Referring to fansidar). (No-HIVPW, 18 years old)
The participants distinguished antiretroviral and cotrimoxazole through the type of stamping on the tablet, that is, the existence of a digit and a line on the antiretroviral drugs and cotrimoxazole respectively.
“There's a number.” (Referring to antiretroviral drugs) (HIVPW, 29 years old)
“It's just that the way it is, I already know, I already know. It is round and has a line in
the middle without writing anything.” (Referring to cotrimoxazole) (HIVPW, 29 years
old)
Because of the used marker signs, women very often mistook cotrimoxazole with paracetamol and isoniazid, while ferrous sulphate was mistaken with multivitamin (known as appetite medicine).
“I see by color because all appetites tablets are red.” (Mistaking ferrous sulfate for multivitamin) (HIVPW, 20 years old)
“….but its paracetamol, aah [laughs] you can see that this is paracetamol.” (Mistaking cotrimoxazole for paracetamol) (HIVPW, 27 years old)
Pregnant women’s knowledge and attributed indication of drugs prescribed at ANC Concerning to the pregnant women’s knowledge of the indication of the drugs prescribed at ANC, the results evidence how some participants interestingly mentioned the perceived indication of the drugs by relating them to a specific disease and not mentioning if for either preventive or treatment propose.
“Interviewer: This one? Do you know this pill? (Referring to fansidar used for malaria IPTp)
Respondent: They are for malaria.” (No-HIVPW, 26 years old)
“Interviewer: - Do you know this pill? (Referring to isoniazid used for TB IPTp). They usually come on a paper (card) like this one, but it's white and this one is a little dirty. There are 30.
Respondent: I don't know! Are not they for tuberculosis?” (HIVPW, 38 years old)
Furthermore, with the exception of isoniazid, some participants perceived that all the drugs prescribed at the ANC could also be used to prevent or treat malaria infection (Table 3).
However, attributed indications were found for mebendazol, isoniazid, cotrimoxazole and antiretroviral drugs. On one hand, the results evidence participants tend to attribute several indications to each drug or similar indications for different drugs, for example, the attributed indication to ferrous sulphate included increasing blood, stimulating appetite, protecting and growing the fetus and preventing malaria. Similarly to antiretroviral drugs, both cotrimoxazole and isoniazid were mentioned to have the role of increasing the level of CD4 cells. Conversely, some participants showed poor knowledge of indication for mebendazol and isoniazid.
“…When CD4 went down...hum [calling to mind]… they increase the CD4.” (Referring to cotrimoxazole) (HIVPW, 35 years old)
“At that time I was in the visiting room, they (referring the health providers) told me! They said it [Referring to isoniazid] serves to increase CD4.” (HIVPW, 29 years old)
Table 3: Pregnant women’s knowledge about the indication of prescribed medication given at the antenatal care visit
Home compliance to pharmacological interventions
In our study, we examined the home compliance with medication among the twenty women invited for the in-depth interviews. We used descriptive compliance aspects of the medication intake such as forgetting daily medication, non-compliance with intake schedule and perceived importance given to some drugs compared to others to assess how the participants’ practices could affect compliance to the pharmacological interventions, as well as the strategies used to avoid forgetfulness. Most of the women (14/20) reported taking their medication daily without failure. However, according to the participants, the medication intake time depends on the routine daily activities; in general, the intake time was mentioned to be, for example, right after waking up, after personal hygiene or after breakfast.
“Interviewer: You don't know. Ok. So, how did you remember to take your pills? Did you do anything to remember to take this one, the ferrous salt?
Respondent: I took it in the morning after breakfast” (No-HIVPW, 20 years old)
“I would wake up, shower, brush (teeth) and then take pills.” (No-HIVPW, 32 years old)
When asked which of the medications received at the ANC they considered the most important that they would never fail/forget to take them daily, most HIVPW (8/10) reported they would never forget antiretroviral drugs, while No-HIVPW reported they would never forget ferrous-sulphate, as seen in the quotes below;
“Interviewer: So, which one for you, you never got into your head that you should never fail?
Respondent: It's ferrous-sulphate.” (No-HIVPW, 28 years old)
“Interviewer: No. Okay. So, out of all these pills here, which do you think you should never fail?
Respondent: It's HIV’s.” (HIVPW, 20 years old)
In terms of strategies to avoid missing a dose, the women with predetermined medication intake time, mentioning using a reminder alarm to be able to take the medicine at exactly the same time, daily.
“…like those of mine I take at 7 o'clock. Yes, I did that alarm on my phone.” (HIVPW, 38 years old)
“I looked at the clock. As I always tell myself that at X time, I should take it.” (No-HIVPW, 21 years old)
Notwithstanding, forgetting daily medication intake was common and similar between HIVPW and No-HIVPW. In this case, one of the participants reported having taken the medication as soon as she remembered. Below are some illustrations of the women who reported forgetfulness and failure to daily intake (6/20):
“Interviewer: What pills did you forget to take?
Respondent: The ones I really forgot are the ones I take 2. (Referring to cotrimoxazole).” (HIVPW, 33 years old).
“It was just one day…that I forgot (Referring to ferrous-sulphate)… I remembered while it was the 29th…as soon as I remembered, I took it.” (No-HIVPW, 28 years old)
Discussion
This study aimed at exploring pregnant women’s awareness on diseases in pregnancy and their ability to identify and knowledge the indication of pharmacological interventions prescribed at ANC. In addition we explored pregnant women’s compliance with these interventions. Our findings evidence that, while pregnant women attending ANC in Manhiça district, revealed awareness of the most common diseases in pregnancy, there is limited knowledge of the indication of the pharmacological interventions implemented at ANC. This limited knowledge’s might lead to poor compliance and negatively affect drug efficacy and safety and contributing to the poor effectiveness of MoH strategies for disease control in pregnant women
The perceived most common and severe diseases during pregnancy
The results show that HIV, malaria, STDs, TB and non-specific pain constitute the perceived most common diseases in pregnancy. Nevertheless, it is a concern that compared to No-HIVPW, HIVPW showed more accurate awareness of many more diseases that may occur during pregnancy. These differences may be due to the strong sensitization and awareness campaigns of diseases more targeted to HIVPW in recent years in Mozambique [29–32]. This finding could also be explained by the fact that HIVPW have more frequent contacts with the health facility compared to No-HIVPW women. Therefore, there is a need to intensify health programs for the general population, with special attention to women in childbearing age, to homogenize the level of disease knowledge that may affect pregnant women. Nevertheless, our findings regarding pregnant women’s knowledge about common diseases in pregnancy are similar to those of other authors who investigated malaria, HIV STDs and TB in other African settings [33–36].
Furthermore, HIV, malaria, TB and COVID-19 (indirect causes) were also considered the most severe diseases during pregnancy. Previous studies conducted by the MoH have shown, with exception of COVID-19, that the above diseases are the main causes of maternal mortality in Mozambique; thus, these results indicate that pregnant women from Manhiça District are aware of most severe diseases during pregnancy [3–5]. However, knowledge of direct causes such as hemorrhage, gestational hypertension (also quite frequent in this setting) remains low.
This study was conducted at the beginning of COVID-19 pandemic in Mozambique (on 22 March 2020) when few evidence on the COVID-19 dynamics was available. The participants mentioned COVID-19 as one disease to fear during the pregnancy. Moreover, it is important to mention that during the outbreak of COVID-19, the national health authorities, recommended and implemented the suspension of monthly ANC visits, stating that pregnant women were only recommended to visit the ANC every three months. Although not conclusive, the above-mentioned implemented measure might have an influence on the participant’s fear of contracting COVID-19 during pregnancy. This represents an interesting emerging theme that needs to be taken into consideration, as this has the potential of anticipating insights on acceptability of COVID-19 containing interventions targeted at pregnant women, such as vaccination [37,38]. Furthermore, altogether, it indicates how the social dynamics and the emergence of diseases influence the pregnant women’s knowledge even in a context of non-conclusive and scarce information such as when we conducted this study. New and emerging diseases are important to consider as influencing all or part of women’s knowledge. Therefore, there is a need to always consider the research context and understand how these contexts and its social constructs influence the knowledge’s and health seeking behaviour in Mozambique.
Similarly to what was reported in previous studies, the main criteria for a disease being considered more severe by pregnant women was the risk of affecting their offspring [39,40]. In this study, some participants expressed their fear of contracting diseases such as malaria and HIV in pregnancy not only because it can affect the pregnant women, but mostly because it can affect the fetus. Moreover, the fear of contracting COVID-19, is related to the fact that it was a new disease and less evidence on how it can affect women was available. Strategies aimed at improving drug compliance in pregnant women should emphasize the benefit of specific intervention in protecting their offspring. On the other side, because this study used a more exploratory approach, without previously defining disease severity markers according to its conceptual framework, we observed that No-HIVPW tend to use other disease severity markers and not necessarily the consequences from disease to health. For example, fear of stigma, being too young to be infected and fear of taking lifelong antiretroviral drugs should be taken in account by the health authorities, health promoters and health policy makers when re (designing) interventions for pregnant women in Mozambique.
The knowledge of the drug indication and the recognition of the drugs prescribed at ANC
Through the results of this study, we verified poor ability to identify and knowledge of indication of the drugs prescribed at the ANC which suggests some communication gaps between health care provider and patient during the ANC visits. This is worth considering due to the following challenges frequently encountered in some LMICs such as Mozambique’; i) some drugs prescribed at ANC are dispensed in a small unspecified zip lock plastic or paper made bag identified with a handwriting that easily disappears over time or in paper made bags susceptible to destruction by moisture and time; ii) because of fear of stigma, frequently the tablets are removed by HIV-infected individuals from their original container and put in plastic zip lock bag with no identification or a different identification; iii) finally national illiteracy standing at 45% is almost twice more common in women than in men [41], so that identification of the drugs relies on marker signs such as the container, format, color, size and stamping of the drugs as has been found in a previous study regarding antibiotic use in rural Mozambique [42].
Moreover, due to its multicultural and multilingual characteristics, Mozambique has several local languages whose translation for medical terms is not harmonized [43,44]. It is possible that healthcare providers are using different terminology or explanations for the same drug and this may justify the diversity of drug perception of indications reported by pregnant women for the same drug. In fact, both cotrimoxazole as well as isoniazid were mentioned to have the role of increasing the level of CD4 and it was perceived that all the drugs prescribed at the ANC could serve to treat malaria infection. Therefore, considering only 17% of the country population speak Portuguese as their first language, incorporating local languages into healthcare services and creating opportunities for bilingual local health guideline is key to providing relevant and inclusive health care for all. This would be particularly important in those interventions that requires home intake medication.
All the above-mentioned facts, prompted medicine with the same physical characteristics to cause difficulties in identifying the drugs as well as lead to poor knowledge of the indication of the drugs being prescribed at ANC. Moreover, pregnant women not being able to identify the prescribed drug and its indication, paves the way to medication errors. Future studies should deeply explore the above-mentioned facts and their impact on drug compliance. Meanwhile, strategies such as pictograms are needed to increase and harmonize the information provided to pregnant women at ANC clinics considering the high number of medications prescribed, especially to HIV-infected pregnant women.
Another interesting finding is the fact that some participants mentioned the perceived indication of some pharmacological interventions by relating them to a specific disease and not mentioning if for either preventive or treatment propose. Teaching people about the importance of preventive measures is key to making sure more people get recommended care. In countries such as Mozambique, with limited medical resources, high rates of preventive care would reduce the risk of being sick or either catch diseases before they become too serious, which would drastically reduce the cost of treatment.
Home compliance to the prescribed drugs
Compliance to medication prescription is one the appropriate way of using medicines that prompts good disease outcome and a rational utilization of these valuable substances worldwide. Our study results show that medication compliance practices, specifically related to forgetting daily medication and non-compliance with intake schedule could be affecting effectiveness of ANC pharmacological interventions. Likewise, the perceived importance given to some medication in comparison to others, may affect the compliance. For example, some HIVPW reported not forgetting to take their antiretroviral drugs while No-HIVPW referred the same to ferrous sulphate. However, cotrimoxazole prophylaxis to prevent opportunistic infections was frequently forgotten by some HIVPW. The lack of knowledge and proper practice about medicines among pregnant women is common in many LMICs and have serious impacts on the health of the mother and child. Thus, effective interventions are needed to improve pregnant women's attitude and practices regarding safe and effective medication intake during pregnancy. Both physicians and maternal and child health nurses have an important role by adequately sensitize the pregnant women about illnesses, complications that may arise and the advantages of correct medications intakes. To this end, pregnant women must be familiar with the drugs and the modalities of their use for the optimal therapeutic outcomes [45].
Study limitations
Limitations of this study include the fact that it was carried out in a period of national restrictions due to COVID-19 in the health facilities and that affected the data collection process. The interviews were carried out as quickly as possible and there was no deep enough exploration of some aspects which may have induced bias. Furthermore, this situation did not allow the interviewers to observe compliance-practices related with medication intake schedules. Finally, the semi-structured exit interviews carried out in a hospital environment may have affected the participants' comfort in giving an honest and open opinion, on the other hand, their performance immediately after leaving the office minimized the occurrence of bias memory. Limitations aside, this study brings information that is worth addressing by public health policy and target appropriate interventions in order to improve compliance pharmacological interventions implemented at ANC for pregnant women. At the same time, this study was an opportunity to investigate women's perceptions of the new disease COVID-19.
Conclusion
This study comes to a conclusion that pregnant women knowledge about the pharmacological interventions delivered at ANC and their indication were limited which paves the way to medications intake errors affecting compliance and adherence while compromising the drug efficacy. Strategies are needed to provide clear information regarding the name of the drugs, its specific indication and the advantages to comply with intake instruction, considering the high number of drugs prescribed, especially to HIV-infected pregnant women. Moreover, effectively promoting health and educating the women and the overall community by constantly providing correct information regarding the drugs prescribed as well as its value, is key to raise awareness, improve their knowledge towards the rational use of the drugs while increasing adherence.
Declarations
Ethics approval and consent to participate
This study was performed in accordance with the Declaration of Helsinki and the National Bioethics Committee of Mozambique approved the study protocol in 2011 (327/CNBS/11), with subsequent annual renewals until the year 2020. After informing the pregnant women about the study objectives and methods, women consented for their participation, and that of their children, by signing a written informed consent. One copy of the consent form was handled to the participant.
Consent for publication
Not applicable.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Competing interests
No conflicts of interests to declare
Funding:
CISM is supported by the Government of Mozambique and the Spanish Agency for International Development (AECID). TN (corresponding author) is supported by a career development fellowship also co-funded by the EDCTP (European and Developing Countries Clinical Trials Partnership) and the Calouste Gulbenkian Foundation (grant number: TMA2017CDF-1927 – Preg_multidrug). This study was part of the career development fellowship.
Authors’ contributions
Project conception and protocol design: TN, CM, KM
Coordination of data collection: TN, CC, MC, MM, KM
Data analysis and interpretation: TN, CC, CM, NT, KM, ES
Contributed to the writing of the manuscript: TN, CC, MC, NT, RG, LG, AM, ES, KM, CM
Reviewed the draft and approved the decision to submit the paper: all authors
Acknowledgements:
The authors thank all study participants and the healthcare workers from Centro de Investigação em Saúde de Manhiça and Manhiça District Hospital who assisted with data collection, and the district health authorities for their collaboration on the on-going research activities in the Manhiça district.
REFERENCES
- Mozambique USE in. Maternal and Child Mortality in Decline Since 1990 – United States – Mozambique Partnership is Saving Lives [Internet]. Available from: https://mz.usembassy.gov/maternal-and-child-mortality-in-decline-since-1990-united-states-mozambique-partnership-is-saving-lives/. Accessed 20 January 2022.
- World Data Atlas. Mozambique - Neonatal mortality rate [Internet]. Available from: https://knoema.com/atlas/Mozambique/Neonatal-mortality-rate. Accessed 20 January 2021.
- Menéndez C, Romagosa C, Ismail MR, Carrilho C, Saute F, Osman N, et al. An Autopsy Study of Maternal Mortality in Mozambique: The Contribution of Infectious Diseases. Wright L, editor. PLoS Med. 2008 Feb 19;5(2):e44. .
- Loquiha O, Hens N, Chavane L, Temmerman M, Osman N, Faes C, et al. Mapping maternal mortality rate via spatial zero-inflated models for count data: A case study of facility-based maternal deaths from Mozambique. Ali M, editor. PLoS One. 2018 Nov 9;13(11):e0202186.
- Chavane L, Dgedge M, Degomme O, Loquiha O, Aerts M, Temmerman M. The magnitude and factors related to facility-based maternal mortality in Mozambique. J Obstet Gynaecol (Lahore). 2017 May 19;37(4):464–470. .
- Sevene E, Sharma S, Munguambe K, Sacoor C, Vala A, Macuacua S, et al. Community-level interventions for pre-eclampsia (CLIP) in Mozambique: A cluster randomised controlled trial. Pregnancy Hypertens. 2020 Jul;21:96–105. .
- MISAU. Tratamento Antiretroviral e Infecções Oportunistas do Adulto, Adolescente, Grávida e Criança. 2016. Available from: https://www.childrenandaids.org/Mozambique_Tratamento-Antiretroviral_2016. Accessed 20 December 2021.
- Gebre M, Addisu N, Getahun A, Workye J, Gamachu B, Fekadu G, et al. Medication Errors Among Hospitalized Adults in Medical Wards of Nekemte Specialized Hospital, West Ethiopia: A Prospective Observational Study. Drug Healthc Patient Saf. 2021 Nov;Volume 13:221–228.
- da Silva BA, Krishnamurthy M. The alarming reality of medication error: a patient case and review of Pennsylvania and National data. J Community Hosp Intern Med Perspect. 2016 Jan 7;6(4):31758.
- Lincetto O, Mothebesoane-Anoh S, Gomez P, Munjanja S. Controlo Pré-Natal. In: Oportunidades para os recém-nascidos em Africa. Cape Town; 2006. p. 51–62.
- Siemefo Kamgang F de P, Maise HC, Moodley J. Pregnant women admitted with urinary tract infections to a public sector hospital in South Africa: Are there lessons to learn? South African J Infect Dis. 2016 Jul 18;31(3):79–83.
- Völker F, Cooper P, Bader O, Uy A, Zimmermann O, Lugert R, et al. Prevalence of pregnancy-relevant infections in a rural setting of Ghana. BMC Pregnancy Childbirth. 2017 Dec 6;17(1):172.
- Gysels M, Pell C, Mathanga DP, Adongo P, Odhiambo F, Gosling R, et al. Community response to intermittent preventive treatment of malaria in infants (IPTi) delivered through the expanded programme of immunization in five African settings. Malar J. 2009 Dec 10;8(1):191.
- Dlamini P, Mokoboto-Zwane TS. Knowledge, attitudes and practices associated with post-natal PMTCT in breastfeeding mothers living with HIV. Int J Africa Nurs Sci. 2019;11:100150.
- Fuge TG, Ayanto SY, Gurmamo FL. Assessment of knowledge, attitude and practice about malaria and ITNs utilization among pregnant women in Shashogo District, Southern Ethiopia. Malar J. 2015 Dec 4;14(1):235.
- Miller NH, Hill M, Kottke T, Ockene IS. The Multilevel Compliance Challenge: Recommendations for a Call to Action. Circulation. 1997 Feb 18;95(4):1085–1090.
- Campbell M. Framework for design and evaluation of complex interventions to improve health. BMJ. 2000 Sep 16;321(7262):694–696.
- Demaio AR, Dugee O, Amgalan G, Maximenco E, Munkhtaivan A, Graeser S, et al. Protocol for a national, mixed-methods knowledge, attitudes and practices survey on non-communicable diseases. BMC Public Health. 2011 Dec 30;11(1):961.
- Li D, Huang L, Yang W, Qi C, Shang L, Xin J, et al. Knowledge, attitude and practice level of women at the periconceptional period: a cross-sectional study in Shaanxi China. BMC Pregnancy Childbirth. 2019 Dec 4;19(1):326.
- Sacoor C, Nhacolo A, Nhalungo D, Aponte JJ, Bassat Q, Augusto O, et al. Profile: Manhica Health Research Centre (Manhica HDSS). Int J Epidemiol. 2013;42(5):1309–18.
- Nhacolo A, Jamisse E, Augusto O, Matsena T, Hunguana A, Mandomando I, et al. Cohort profile update: Manhiça health and demographic surveillance system (HDSS) of the Manhiça health research centre (CISM). Int J Epidemiol. 2021 Jan 16;
- MISAU. 2020 HIV/AIDS Report. Mozambique Ministry of Health. 2021. Available from: https://www.misau.gov.mz/index.php/relatorios-anuais2021. Accessed 20 November 2021.
- MISAU. Circular Normas Clínicas 08.03.19 - COMITÉ TARV [Internet]. Available from: https://comitetarvmisau.co.mz/. Accessed 14 October 2021.
- Abellana R, Ascaso C, Aponte J, Saute F, Nhalungo D, Nhacolo A, et al. Spatio-seasonal modeling of the incidence rate of malaria in Mozambique. Malar J. 2008 Dec 31;7(1):228.
- González R, Munguambe K, Aponte J, Bavo C, Nhalungo D, Macete E, et al. High HIV prevalence in a southern semi-rural area of Mozambique: a community-based survey. HIV Med. 2012 Nov;13(10):581–588.
- WHO. World Health Organization: A case of COVID-19 confirmed in Mozambique. Available from: https://www.afro.who.int/news/world-health-organization-case-covid-19-confirmed-mozambique. Accessed 20 December 2021.
- González R, Nhampossa T, Mombo-Ngoma G, Mischlinger J, Esen M, Tchouatieu A-M, et al. Evaluation of the safety and efficacy of dihydroartemisinin–piperaquine for intermittent preventive treatment of malaria in HIV-infected pregnant women: protocol of a multicentre, two-arm, randomised, placebo-controlled, superiority clinical trial (MAMAH. BMJ Open. 2021 Nov 23;11(11):e053197.
- Braun V, Clarke V. What can “thematic analysis” offer health and wellbeing researchers? Int J Qual Stud Health Well-being. 2014;9:26152.
- MISAU. Plano Estratégico Nacional de Combate as ITS, HIV e SIDA (PEN ITS/HIV/SIDA) - sector saúde 2004-2008. 2004. Available from: https://www.afro.who.int/sites/default/files/2017-07/moz-Plano-Estrategico-Nacional-combate-STI-HIV-SIDA.pdf. Accessed 29 October 2021.
- MISAU. MISAU. Plano Estratégico Nacional de Resposta ao HIV e SIDA 2010 - 2014 PEN III. 2010. October 2021.
- MISAU. Plano Estratégico Nacional de Resposta ao HIV e SIDA 2015 - 2019 PEN IV. Available from: www.misau.gov.mz/index.php/planos-estrategicos-hiv?download=83:plano...pdf. Accessed 29 October 2021.
- MISAU. Plano Estratégico Nacional de Resposta ao HIV e SIDA 2021 - 2025 PEN V. Available from:https://www.misau.gov.mz/index.php/planos-estrategicos-do-hiv 2021. Accessed 29 October 2021.
- Goshu YA, Yitayew AE. Malaria knowledge and its associated factors among pregnant women attending antenatal clinic of Adis Zemen Hospital, North-western Ethiopia, 2018. Fischer F, editor. PLoS One. 2019 Jan 10;14(1):e0210221.
- Alemu YM, Habtewold TD, Alemu SM. Mother’s knowledge on prevention of mother-to-child transmission of HIV, Ethiopia: A cross sectional study. Haile ZT, editor. PLoS One. 2018 Sep 11;13(9):e0203043.
- Baldeh A-K, Isara AR. Knowledge of Sexually Transmitted Infections amongst Pregnant Women Attending Antenatal Clinics in West Coast Region of The Gambia. Afr J Reprod Health. 2019 Sep;23(3):49–56.
- Mehta SN, Murrill M, Suryavanshi N, Bhosale R, Naik S, Patil N, et al. TB-related knowledge and stigma among pregnant women in low-resource settings. Int J Tuberc Lung Dis. 2021 Feb 1;25(2):148–50.
- Taye EB, Taye ZW, Muche HA, Tsega NT, Haile TT, Tiguh AE. COVID-19 vaccine acceptance and associated factors among women attending antenatal and postnatal cares in Central Gondar Zone public hospitals, Northwest Ethiopia. Clin Epidemiol Glob Heal. 2022 Mar;14:100993.
- Marbán-Castro E, Pons-Duran C, García-Otero L, Chen H, Herrera LB, Gil M del M, et al. Acceptability of Clinical Trials on COVID-19 during Pregnancy among Pregnant Women and Healthcare Providers: A Qualitative Study. Int J Environ Res Public Health. 2021 Oct 13;18(20):10717.
- Verplanken B, Wood W. Interventions to Break and Create Consumer Habits. J Public Policy Mark. 2006 Apr 2;25(1):90–103.
- Pintye J, Beima-Sofie KM, Kimemia G, Ngure K, Trinidad SB, Heffron RA, et al. “I Did Not Want to Give Birth to a Child Who has HIV”: Experiences Using PrEP During Pregnancy Among HIV-Uninfected Kenyan Women in HIV-Serodiscordant Couples. JAIDS J Acquir Immune Defic Syndr. 2017 Nov 1;76(3):259–265.
- Indexmundi. Mozambique - Literacy rate [Internet]. Available from: ndexmundi.com/facts/mozambique/literacy-rate. Accessed 9 June 2022.
- Cambaco O, Alonso Menendez Y, Kinsman J, Sigaúque B, Wertheim H, Do N, et al. Community knowledge and practices regarding antibiotic use in rural Mozambique: where is the starting point for prevention of antibiotic resistance? BMC Public Health. 2020 Dec 29;20(1):1183.
- Janson T. Languages and language names in Mozambique, 150 years ago and now. In: Globalisation and African Languages. Berlin, New York: DE GRUYTER MOUTON;
- Lopes AJ. The Language Situation in Mozambique. J Multiling Multicult Dev. 1998 Sep;19(5):440–486.
- Schwarz EB, Santucci A, Borrero S, Akers AY, Nikolajski C, Gold MA. Perspectives of primary care clinicians on teratogenic risk counseling. Birth Defects Res Part A Clin Mol Teratol. 2009 Oct;85(10):858–863.
