Knowledge, Attitude & Practice towards Cervical Cancer Screening among Women Globally – A Systematic Review
Article Information
Neha Malhotra1, Neha Taneja2*, Rajashree Shankar1, Akanksha Pal1, Bhavika Chawla3, Aanchal Anant Awasthi2, Rajiv Janardhanan4
1MPH Student, Amity Institute of Public Health, Amity University, Noida, Uttar Pradesh, India
2Assistant Professor, Amity Institute of Public Health, Amity University, Noida, India
3Research Assistant, Amity Institute of Public Health, Amity University, Noida, India
4Head of Department of Amity Institute of Public Health, Amity University, Noida, India
*Corresponding author: Dr. Neha Taneja, Assistant Professor, Laboratory of Disease Dynamics & Molecular Epidemiology, Laboratory of Health Data Analytics & Visualization Environment, Amity Institute of Public Health, Amity University, Noida- UP, 201304, India
Received: 07 July 2020; Accepted: 17 July 2020; Published: 24 July 2020
Citation:
Neha Malhotra, Neha Taneja, Rajashree Shankar, Akanksha Pal, Bhavika Chawla, Aanchal Anant Awasthi, Rajiv Janardhanan. Knowledge, Attitude & Practice towards Cervical Cancer Screening among Women Globally – A Systematic Review. Journal of Women’s Health and Development 3 (2020): 194-210.
View / Download Pdf Share at FacebookAbstract
Background: Cervical Cancer is the fourth most frequent cancer among women worldwide. Around 500,000 new cases of cervical cancer are diagnosed every year out of which 270,000 women die in developing countries. It is an issue of significant public health concern.
Objective: To review the knowledge, attitude & practice towards cervical cancer screening among women globally.
Methodology: Literature search was done on electronic databases including PubMed and Google scholar for articles published between 2013 to March 2020. Keywords used for the search were (cervical cancer screening) (knowledge) (attitude) (practice). A total of 17 studies were included in the review based on eligibility criteria. The articles included were specific to English language.
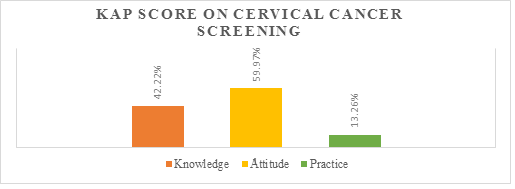
Result: A total of 17 studies were included in the review with a total of 6158 women aged between 15-70 years having varied levels of knowledge, attitude & practice towards cervical cancer screening. 42.22% women had knowledge about the screening process. The source of information was friends & family (26.70%), media (15.92%), health professionals (12.35%). More than half of the participants showed positive attitude towards the cervical cancer screening (59.97%). Only 13.26% had undergone the cervical cancer screening. Most common reason for not undergoing screening was no signs & symptoms (32.78%) followed by no knowledge (28.21%).
Conclusion: There is a dire need to generate awareness and formulate plans for implementation of screening programs in the most cost effective and feasible way, ensuring maximum community participation.
Keywords
Cervical cancer; Screening; Knowledge; Attitude; Practice
Cervical cancer articles, Screening articles, Knowledge articles, Attitude articles, Practice articles
Article Details
1. Introduction
In the modern era, the world is heading towards the rising epidemic of noncommunicable diseases (NCDs). Out of these NCDs, cancer is the second leading cause of death globally [1]. Among all the cancers, cervical cancer is the fourth most frequent cancer among women worldwide. Every year, around 500,000 new cases of cervical cancer are diagnosed out of which 270,000 women die, mostly (85%) in developing countries [2]. According to WHO, in 2018, around 570,000 women were diagnosed with cervical cancer worldwide and about 311,000 women died from the disease. Almost 99% cases of the cervical cancer are associated to infection with human papillomaviruses (HPV). It is a common virus which is transmitted through sexual contact [3]. Cancer of the cervix is the major reproductive health problem in women, especially in emergent nations [4]. It is the major cause of morbidity and mortality in women globally and an issue of significant public health concern [5]. It is a slow growing cancerous disease that generally takes several years to undergo malignant transformation from primary infection by the oncogenic human papillomavirus (HPV) to the various precancerous histological lesions accompanying the persistence of the infection [6]. Cervical cancer takes about 10-15 years to develop [7]. Cervical cancer is a deadly disease once it reaches the invasive stages, but out of all the female genital tract cancers, it is the only preventable cancer if detected at its early stages. Population-based screening with Pap smear is an important secondary preventive measure for cervical cancer that leads to a high-cure rate among cervical cancer patients [8]. Screening of cervical cancer offers protective benefits and is associated with a reduction. Every women must undergo screening of cervical cancer once in three years as advised by the World Health Organisation (WHO) [9]. Therefore, early screening is mandatory to reduce the incidence of malignancy. In emergent nations, the screening coverage is ranging from 0.4% to 14% in rural areas and from 2% to 20.2% in urban areas [7].
Access to screening and treatment services is needed to ensure the success of a cervical cancer prevention program; however, the availability of services is inadequate to guarantee their use. Moreover, clients and people of the community must be familiar with the problem of cervical cancer, their potential risk of developing the illness & the facilities where they can seek services for screening [10]. By providing accessible & low-cost services and encouraging these services among the target population through well-organised, strategically targeted information and education efforts, the use of services can be remarkably increased and the incidence of cervical cancer can be reduced [11]. Despite of suboptimal level of knowledge and positive attitude regarding cervical cancer screening still there is inadequate practice towards the screening methods. Hence, there is a dire need to educate women regarding cervical cancer screening. This review was done to evaluate the knowledge, attitude & practice towards the cervical cancer screening among women globally.
3. Methodology
2.1 Search strategy
A comprehensive search of quantitative literature published from 2013 onwards till March 2020 in the electronic databases PubMed and Google Scholar was conducted. We retrieved all the studies written in English and which contained information on knowledge, attitude & practice towards cervical cancer screening in India & abroad. Articles which included the quantitative data of women's knowledge, attitude & practice of cervical cancer screening in India & abroad were included in the review. The following terms and keywords were used: “cervical cancer” “screening” “knowledge” “attitude” “practice”. The subject search and text word search were done separately in PubMed and Google Scholar and then combined with “OR” and “AND” operators. Combined terms were used, for example, (“cervical cancer screening” or 'cervical screening') AND ('cervical cancer knowledge' or 'cervical cancer attitude'). Additional articles were identified using the bibliography of included articles and some excluded review articles, along with forward citation searches.
2.2 Study selection
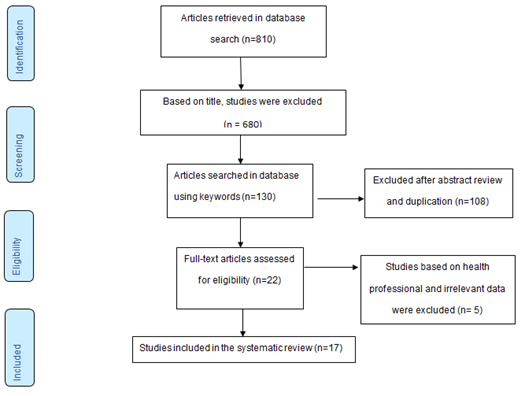
Articles that had reported quantitative evidence data of knowledge, attitude & practice of cervical cancer screening in India & abroad were only included. (Figure 1) shows the selection process of the articles retrieved. This systematic review was done according to PRISMA guidelines [12]. The initial database search retrieved 810 published English language studies. Out of these, 680 studies were excluded based on title. Of the remaining 130 studies, the abstracts were read out of which 108 articles were excluded as they were either duplicate articles, were not cross sectionally designed or published before 2013. Of the remaining 22 studies 5 studies were excluded as they were conducted among health care professionals and provided incomplete information. 17 cross sectional study designs conducted in diverse settings like hospitals or communities published between 2013 and March 2020 that met the inclusion criteria and focused on knowledge, attitude & practice related to cervical cancer screening were finally included for the review [12-28].
2.3 Inclusion criteria
Cross-sectional studies conducted in diverse settings like hospitals or communities published from 2013 till March 2020, English language and in India & abroad based studies of knowledge, attitude, practice of cervical cancer screening.
2.4 Exclusion criteria
Case reports, case series, earlier reviews, and qualitative studies of cervical cancer screening were excluded. Studies published in languages other than English, conducted on specific population i.e. healthcare professionals & studies which showed incomplete information were excluded.
2.5 Data extraction and synthesis
We extracted the following key characteristics of the studies: lead author and country, year published, study design, sampling technique, sample size, age group and knowledge of cervical cancer and screening, knowledge of who should be screened, knowledge regarding frequency of screening, reasons for not screened, attitude & practice towards cervical cancer screening. After the removal of duplicates, primary outcome data of all articles were indexed in Microsoft Excel. Later, interpretation of textual data was extracted to a Microsoft Word document. Full-text articles were identified and assessed for eligibility after applying the inclusion and exclusion criteria. Agreement of the requisite contents of the articles related to quality assessment and data extraction was performed. Statistical software like SPSS-V.23 was used for statistical application.
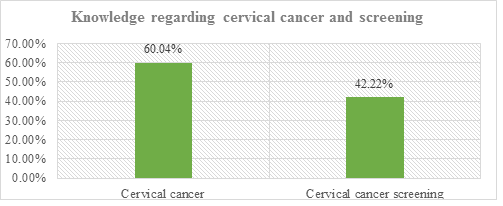
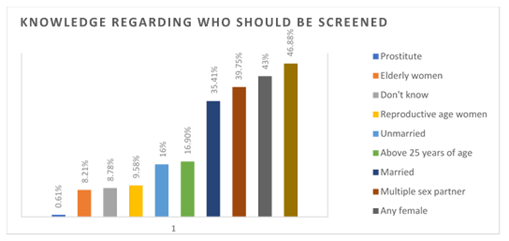
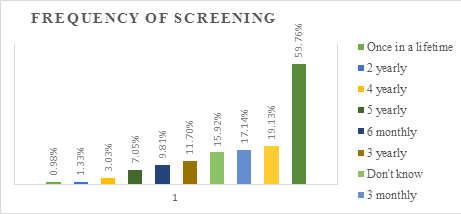
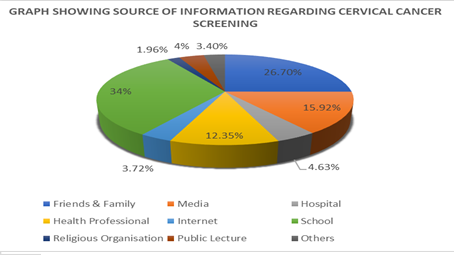
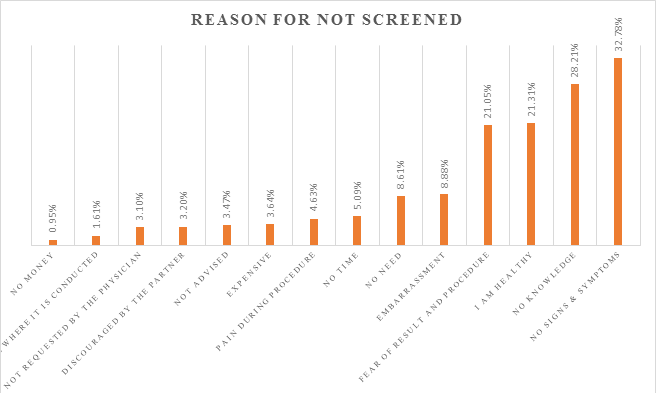
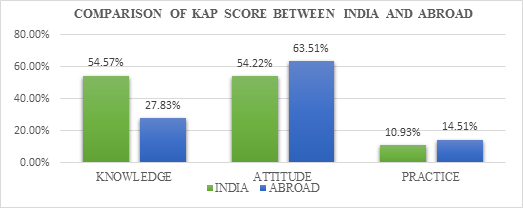
3. Result
The literature search yielded 130 studies, out of which 17 studies met the inclusion criteria. These studies had a total sample size of 6158 women aged between 15-70 years. Out of 17 studies 16 were hospital and community-based studies among women residing in urban as well rural slums globally [12-21, 23-28]. One study was conducted among medical students [22]. The study population included women in which majority were married [12, 13, 15-20, 23-27]. Majority of the studies i.e. 10 out of 17 studies were conducted in abroad [19-28] and rest were in India [12-18]. The illiteracy rate ranged from 2.4% - 78.3% [13, 28] (Table-1). Most reviewed studies showed significant association between the knowledge of cervical cancer screening and the education level of study participants [20, 21, 24, 26-28], marital status [15, 21, 25, 26], age [21, 24, 26], family income [24], occupational status [20]. (Table-1) Among 17 studies reviewed, 14 reported the knowledge on cervical cancer [14-17, 19-28]. The overall knowledge on cervical cancer among women is 60.04%. Among the reviewed studies, 15 reported knowledge on cervical cancer screening [12-17, 18, 20-28]. The overall knowledge on cervical cancer screening among women is 42.22%. (Figure 2). The awareness level of women regarding the person who should be screened is reported from 6 studies [12, 13, 15, 18, 21, 26] that above 30 years of age 46.88%, reproductive age women 9.58%, 39.75%, married 35.4%, any female 43% should be screened. (Figure 3). Out of 17 studies reviewed, 9 reported the knowledge on the awareness level of women regarding frequency of screening [12, 15-18, 21, 24, 26, 27]. The study participants perceived that women must undergo screening every one yearly 476(2488)19.13%, three yearly 408(3487)11.7%, symptomatic 355(594)59.76% (Figure 4). Among the studies reviewed, 9 [12, 13, 15, 18-21, 23, 26] reported that most of the women got the information from the school (34%) followed by friends & family (26.70%), media (15.92%) and health professionals (12.35%) (Figure 5). Based on the review, 9 [12, 15, 18, 19, 21, 22, 23, 26, 27] out of 17 studies reported that a majority of women had various reasons for not undergoing screening. The most common reason for not undergoing screening was no signs & symptoms (32.78%) followed by no knowledge (28.21%) and majority of the women think that they are healthy so there is no need for undergoing screening of cervical cancer (Figure 6). Based on the review it was observed that there is a variation between knowledge, attitude & practice on cervical cancer screening (Figure 7). Despite of limited knowledge about cervical cancer & screening, a large number of participants had positive attitude towards the screening process. The articles reviewed showed disparity between the knowledge, attitude & practice score of India and abroad. When compared it was observed that the knowledge regarding cervical cancer screening is high in India (54.57%) as compared to abroad but the attitude & practice towards cervical cancer screening was higher in abroad when compared to India (Figure 8).
Table 1: Characteristics of the studies included in the review.
4. Discussion
This systematic review revealed that there is suboptimal level of awareness about cervical cancer screening among women globally. Most women residing in urban and rural areas of India and abroad have knowledge about cervical cancer and its screening, yet the uptake of screening of cervical cancer is very low. Most common reason for the low uptake of cervical cancer screening is no signs & symptoms followed by no knowledge, fear of result & procedure [12, 15, 18, 19, 21- 23, 26, 27]. This study showed that 60.04% of population had heard about cervical cancer. Similar results were observed among a hospital-based study conducted in Bhopal by Bansal et al. [30]. However, these results are contrast with a study conducted among women of Ugrachandi Nala, Nepal [31] where the knowledge of cervical cancer is 94.4%. Another study conducted among women in Dabat District, Northwest Ethiopia [32] show that 46.4% of the population had heard about cervical cancer.
In case of Knowledge of cervical cancer screening our study revealed that only 42.22% of the population had knowledge about screening of cervical cancer. This score is inconsistent with 85.8% of the population having knowledge about screening of cervical cancer from the study done among women in Mekelle Zone, Northern Ethiopia [33]. Another study conducted in Bhopal by Bansal et al [30] showed that only 34.5% of the population had knowledge of screening of cervical cancer. Most of the women who had heard about cervical cancer screening stated that they got the information from the school (34%) followed by friends & family (26.70%), media (15.92%) and health professionals (12.35%). Similar results were observed in a study conducted by Acharya Pandey et al in Ugrachandi Nala, Nepal [31] where it was shown that the source of information was family and friends (26.2%) and media (16.6%). Another study conducted in Kerala by S. Aswathy et al [34] showed inconsistent result where the main source of information was media (55.8%) followed by health professionals (33.74%) and family & friends (14.7%). Regarding who should be screened, our study shows that almost half of the population (46.88%) were aware that the women above the age of 30 years should be screened, 43% perceived that any female should undergo screening, 39.75% perceived that women having multiple sexual partners should undergo screening whereas 35.4% believed that married women should be screened. Likewise a study conducted by Ekta et al [35] in tertiary institution of rural India showed consistent result that the women above the age of 30 years should be screened. This study by Ekta et al [35] also showed that 25.1% of the population were aware that only married women should be screened for cervical cancer which is consistent with our result. Another study conducted by HN Harsha Kumar & Shubham Tanya [36] among women in Mangalore City shows that only 20.5% women believed that only married women and 10.8% believed that any female should undergo cervical cancer screening. According to World Health Organisation (WHO), it is believed that all the adult women should undergo periodic cervical cancer screening. With regards to frequency of screening of cervical cancer, 59.76% i.e. three-fifth of the population perceived that screening should be done if the symptoms arise, 19.13% perceived that screening should be done once in a year. Through various studies it was observed that there is an imbalance between the knowledge and actual uptake of screening of cervical cancer among women globally. Many women have adequate knowledge regarding cervical cancer but an unsatisfactory result is observed regarding screening of cervical cancer. Instead of low uptake, a large number of women expressed willingness to undergo screening of cervical cancer.
This study showed that three-fifth of the population had positive attitude towards cervical cancer screening while a study done in a tertiary care hospital of Delhi by M.Singh et al [37] showed that only 18.2% of the respondents has adequate attitude. Another study conducted by Kebadnew Mulatu et al in Ethiopia [38] among female students of Mizan Tepi University showed similar results (61.24%) with our study. This study showed that only 13.26% women had undergone cervical cancer screening in their lifetime. Similar result was observed in a study which was carried out in Outpatient Department of Obstetrics and Gynaecology of secondary care referral Hospital, Bathalapalli, Anantapur district, Andhra Pradesh, India [39]. The study which was conducted in Ethiopia by Kebadnew Mulatu [38] somewhat also showed similar results (14. 83%). The main reasons mentioned for not screened were that there were no signs & symptoms, no knowledge regarding screening process and fear of result & procedure.
In our review it was observed that there is a variation of knowledge, attitude & practice score among the women of India and abroad. From figure-8, it is observed that the knowledge level of India regarding cervical cancer screening is high when compared with studies done in Abroad. This variation of knowledge level between India and abroad could be because of the studies conducted in abroad which are included in this review. The studies included are mainly done in the countries of Africa where the level of education is inadequate. According to UIS UNESCO, sub-Saharan Africa has high-ranking of education exclusion. Almost 60% of youngsters between the ages of 15 and 17 are not in school [40]. This review found out that the level of knowledge of cervical carcinoma was associated with positive attitude but not with practice of screening. To address the heavy burden of cervical cancer it is compulsory to organise awareness campaigns along with state-wide & national level screening efforts. At the same time, it is important to build up the capacity of health systems across urban and rural areas of the country for effective screening among women. For successful screening programs, the health of the country should focus on program participation, processes & outcomes along with referral pathways and follow ups. According to the International Cancer Screening Network, six essential elements of national cancer screening programs must be taken into account: (1) development of a clear screening policy, (2) recognition that screening is part of a continuum of care, not a stand-alone event, (3) strong infrastructure, (4) establishment of a monitoring and evaluation system, (5) a plan policy, (2) recognition that screening is part of a continuum of care, not a stand-alone event, (3) strong infrastructure, (4) establishment of a monitoring and evaluation system, (5) a plan for community engagement, and (6) implementation of scientific evidence in health delivery settings [41].
5. Conclusion and Recommendations
This systematic review concluded that in spite of good knowledge & positive attitude regarding cervical cancer screening there is a huge gap which needs to be filled in terms of practice. This emphasizes the importance of increasing and creating awareness, encouraging searching of health-related data and acquire health information from any information sources regarding cervical cancer [42]. It is a top-priority to initiate a focused educative intervention to enhance the women’s knowledge about cervical cancer. More attention to be paid for the women of old age and for those whose education level is low, especially residing in the undeveloped regions. Besides education, motivation and guidance for health professionals have a major role in imparting awareness to all the females regarding cancer of the cervix by enhancing women’s education level. Women needs to be motivated to undergo cervical cancer screening and detect the cancer at the earliest. Women all around the world must come together, create awareness and help each other out by sharing knowledge.
Limitations
This review has certain limitations, it only focused on the women of several countries around the world therefore the results may not be generalised. Efforts were made to include all the relevant articles but due to the diversification of the studies it was difficult to include them. Further the calculation of result was done on the basis of secondary data as the data was not collected by us which could lead to discrepancy with the result. Also, the data provided by the women could be false because they might not be able to express openly about their problems to an unknown person. However, despite these limitations, the results of this study provide a basis for further planning for creating awareness among women regarding cervical cancer & screening.
Conflicts of Interest
None declared
References
- Available from: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/global-cancer-facts-and-figures/global-cancer-facts-and-figures-3rd-edition.pdf.
- Ganju S, Gautam N, Barwal V, Walia S, Ganju S. Assessment of knowledge and attitude of medical and nursing students towards screening for cervical carcinoma and HPV vaccination in a tertiary care teaching hospital. International Journal Of Community Medicine And Public Health 4 (2017): 4186-4193.
- Cervical Cancer.WHO (2018).
- Eke NO, Ezeama C, Eke CO, Eleje GU, Akabuike JC, Iu E. Knowledge of Cervical Cancer and its Screening Amongst Female Workers In Nnewi, Nigeria. Afri medic J. 2010 1 (2010): 1-6.
- Metwali Z, AlKindi F, Shanbleh S, Al Akshar S, Sarhan F. Evaluating awareness and screening of cervical cancer among women in Sharjah, United Arab Emirates. IOSR J Pharmacy 5 (2015): 57-64.
- Bosch FX, Manos MM, Munoz N, Sherman M, Jansen AM, Peto J, et al. Prevalence of human papillomavirus in cervical cancer: a worldwide perspective. J Natl Cancer Inst 87 (1995): 796-802.
- Louie K S, De Sanjose S, Mayaud P. “Epidemiology and prevention of human papillomavirus and cervical cancer in sub-Saharan Africa: a comprehensive review,”. Tropical Medicine and International Health 14 (2009): 1287-1302.
- Shah V, Vyas S, Singh A, Shrivastava M. Awareness and knowledge of cervical cancer and its prevention among the nursing staff of a tertiary health institute in Ahmedabad, Gujarat, India. Ecancermedicalscience6 (2012): 270.
- Moyer VA, LeFevre ML, Siu AL, Peters JJ, Bibbins-Domingo K, Curry SJ, et al. Screening for cervical cancer:US preventive servicestask force recommendation statement. Ann Intern Med 156 (2012): 880-891.
- Alliance for Cervical Cancer Prevention (ACCP). Planning and Implementing Cervical Cancer Prevention and Control Programs: A MANUAL FOR MANAGERS. Seattle (2004).
- World Health Organization (WHO). Comprehensive cervical cancer control: a guide to essential practice – 2nd ed. Geneva, Switzerland (2014).
- David Moher A L. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Annals of Internal Medicine (2009).
- Gupta Rajiv, Singh Parveen, Langer Bhavna, Kumari Rashmi, Sharma Pawan, Gupta, Riya. Cervical cancer: a hospital based KAP study among women aged 18 years and above in Northern India. International Journal Of Community Medicine And Public Health 6 (2019): 1628.
- Varadheswari T, Dandekar Rahul, Sharanya T. A Study on the Prevalence and KAP Regarding Cervical Cancer Among Women Attending a Tertiary Care Hospital in Perambalur. 1 (2015): 71-78.
- Pattupara AJ, Dhiman N, Singh A, Chaturvedi J. Knowledge, Attitude & Practice Study on Screening of Cervical Cancer Among Women Visiting A Tertiary Care Center. SOJ Gynecol Obstet Womens Health 2 (2016): 3.
- Elamurugan S, Rajendran P, Thangamani S. Cervical cancer screening: Awareness, attitude, and practice of Indian women. Trop J Med Res 19 (2016): 42-46.
- Dahiya N, Aggarwal K, Singh MC, Garg S, Kumar R. Knowledge, attitude, and practice regarding the screening of cervical cancer among women in New Delhi, India. Tzu Chi Med J 31 (2019): 240-243.
- Varughese NR, Samuel CJ, Dabas P. Knowledge and practices of cervical cancer screening among married women in a semi-urban population of Ludhiana, Punjab. CHRISMED J Health Res 3 (2016): 51-54.
- Krishnaveni K, Roy P, Sambathkumar R. Knowledge, attitude and practice related to cervical cancer and screening among women: community based cross - sectional study. Int J Pharm Sci Res 9 (2018): 722-729.
- Tope Olubodun, Oluwakemi Ololade Odukoya, Mobolanle Rasheedat Balogun. Knowledge, attitude and practice of cervical cancer prevention, among women residing in an urban slum in Lagos, South West, Nigeria. Pan African Medical Journal 32 (2019): 130.
- Kassa RT, Gurmessa TO, Lemma TF, Abebe WS. Cervical Cancer and Screening Method: Knowledge, Attitude and Practice among Women Living in Adama Town. J Women's Health Care 8 (2019): 458.
- Kasa AS, Tesfaye TD, Temesgen WA. Knowledge, attitude and practice towards cervical cancer among women in FinoteSelam city administration, West Gojjam Zone, Amhara Region, North West Ethiopia, 2017. Afri Health Sci 18 (2018): 623-636.
- Deborah Akpo, , Priscilla Deji, Victory Idiake, David Otohinoyi, Srinivas Medavarapu. Cervical Cancer: Knowledge, Screening WrAcOcGE and Vaccines among Female Medical Students in the Common Wealth of Dominica. Arch Med 8 (2016): 5.
- Georges K, Armel Herve NK, Simo Richard T, Jeremie MA, Charlette N. Knowledge and behavior of women on cervical cancer in the northern region of Cameroon 2 (2017).
- Liu T, Li S, Ratcliffe J, Chen G. Assessing Knowledge and Attitudes towards Cervical Cancer Screening among Rural Women in Eastern China. International journal of environmental research and public health14 (2017): 967.
- Julius Sama Dohbit, NP Domkao, Nue Mela, Belinga Etienne, Tochie Joel Noutakdie, Tolefac Paul, et al. Knowledge, Attitudes and Practices of Postpartum Women Regarding Cervical Cancer in Maroua, Northern Cameroon. Journal of Gynecology and Womens Health 11 (2018).
- Shrestha J, Saha R, Tripathi N. Knowledge, Attitude and Practice regarding Cervical Cancer Screening Amongst Women visiting Tertiary Centre in Kathmandu, Nepal. Nepal Journal of Medical Sciences2 (2013): 85-90.
- Javaeed A, Shoukat S, Hina S, Hameed Z, Ghauri S K, Ahmed M M. Knowledge, Attitude, and Practices Related to Cervical Cancer Among Adult Women in Azad Kashmir: A Hospital-based Cross-sectional Study. Cureus11 (2019): e4234.
- Almobarak A O, Elbadawi A A, Elmadhoun W M, Elhoweris M H, Ahmed M H. Knowledge, Attitudes and Practices of Sudanese Women Regarding the Pap Smear Test and Cervical Cancer. Asian Pacific journal of cancer prevention: APJCP17 (2016): 625-630.
- Bansal A B, Pakhare A P, Kapoor N, Mehrotra R, Kokane A M. Knowledge, attitude, and practices related to cervical cancer among adult women: A hospital-based cross-sectional study. Journal of natural science, biology, and medicine6 (2015): 324-328.
- Acharya Pandey R, Karmacharya E. Cervical cancer screening behavior and associated factors among women of Ugrachandi Nala, Kavre, Nepal. European journal of medical research22 (2017): 32.
- Eshete Meried, Atta Mohammedbirhan, Yeshita Hedija. Cervical Cancer Screening Acceptance among Women in Dabat District, Northwest Ethiopia, 2017: An Institution-Based Cross-Sectional Study. Obstetrics and Gynecology International (2020): 1-7.
- Bayu H, Berhe Y, Mulat A, Alemu A. Cervical Cancer Screening Service Uptake and Associated Factors among Age Eligible Women in Mekelle Zone, Northern Ethiopia, 2015: A Community Based Study Using Health Belief Model. PloS one11 (2016): e0149908.
- Aswathy S, Quereshi M A, Kurian B, Leelamoni K. Cervical cancer screening: Current knowledge & practice among women in a rural population of Kerala, India. The Indian journal of medical research136 (2012): 205-210.
- Singh E, Seth S, Rani V, Srivastava D K. Awareness of cervical cancer screening among nursing staff in a tertiary institution of rural India. Journal of gynecologic oncology23 (2012): 141-146.
- Harsha Kumar H, Tanya S. A Study on Knowledge and Screening for Cervical Cancer among Women in Mangalore City. Annals of medical and health sciences research4 (2014): 751-756.
- Singh M, Ranjan R, Das B, Gupta K. Knowledge, attitude and practice of cervical cancer screening in women visiting a tertiary care hospital of Delhi. Indian journal of cancer 51 (2014): 319.
- Mulatu K, Motma A, Seid M, Tadesse M. Assessment of Knowledge, Attitude andPractice on Cervical Cancer Screening amongFemale Students of Mizan Tepi University,Ethiopia, 2016 (2017).
- Narayana G, Suchitra MJ, Sunanda G, Ramaiah JD, Kumar BP, Veerabhadrappa KV. Knowledge, attitude, and practice toward cervical cancer among women attending Obstetrics and Gynecology Department: A cross-sectional, hospital-based survey in South India. Indian journal of cancer 54 (2017): 481.
- Education in Africa.uis.unesco.org.
- Vora K, McQuatters L, Saiyed S, Gupta P. Knowledge, attitudes, and barriers to screening for cervical cancer among women in India: a review. WCRJ 7 (2020): e1504.
- Aweke YH, Ayanto SY, Ersado TL. Knowledge, attitude and practice for cervical cancer prevention and control among women of childbearing age in Hossana Town, Hadiya zone, Southern Ethiopia: Community-based cross-sectional study. PLoS One 12 (2017): e0181415.