Knowledge and Myths about Preeclampsia and Eclampsia and its Influence on Antenatal Service Utilization among Pregnant Women and their Male Partners in Mtwara Regional - Tanzania: A Cross Sectional Analytical Study
Article Information
Aziza S Machenje1*, Stephen M Kibusi2, Nyasiro Gibore3, Athanase Lilungulu4, Fabiola V Moshi2
1Department of clinical Nursing, Division of Nursing and Midwifery Services, MOHCDGEC, Dodoma, Tanzania
2Department of Nursing and Midwifery, College of Health Science of University of Dodoma, Dodoma, Tanzania
3Department of Public Health, College of Health Science of University of Dodoma, Dodoma, Tanzania
4Department of Clinical Medicine, College of Health Science of University of Dodoma, Dodoma, Tanzania
*Corresponding author: Aziza S Machenje, Department of clinical Nursing-Division of Nursing and Midwifery Services, MOHCDGEC, Dodoma, Tanzania
Received: 21 June 2022; Accepted: 04 July 2022; Published: 10 August 2022
Citation: Aziza S Machenje, Stephen M Kibusi, Nyasiro Gibore, Athanase Lilungulu, Fabiola V Moshi. Knowledge and Myths about Preeclampsia and Eclampsia and its Influence on Antenatal Service Utilization among Pregnant Women and their Male Partners in Mtwara Regional - Tanzania: A Cross Sectional Analytical Study. Archives of Internal Medicine Research 5 (2022): 397-411.
View / Download Pdf Share at FacebookAbstract
Background: Pregnancy induced hypertension, including preeclampsia and eclampsia are the major health problem and the main cause of the maternal and perinatal morbidity and mortality in Tanzania. The aim of this study was to assess knowledge and myths about preeclampsia and eclampsia and its influence in Antenatal Clinics (ANC) utilization among pregnant women and their male partiners in Mtwara region.
Method: A community based cross-sectional analytical study conducted in Mtwara Region, a random sampling procedure was employed to obtain a sample size of 384 pregnant women and their male partners a total of 768 participants (male=384 and female =384). Interviewer structured questionnaire was used for data collection and Statistical package for social science (SPSS v.20) software was used for data entry and analysis. Descriptive statistics, cross tabulation, Principal component analysis (PCA) were conducted and inferential statistics was used to test association between variables obtained.
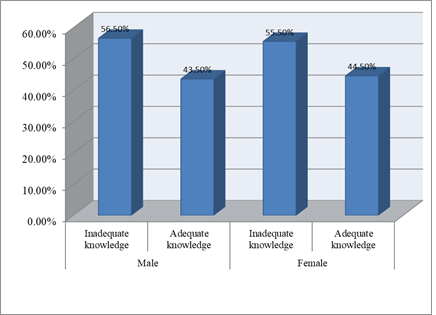
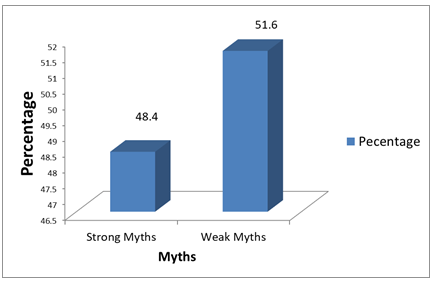
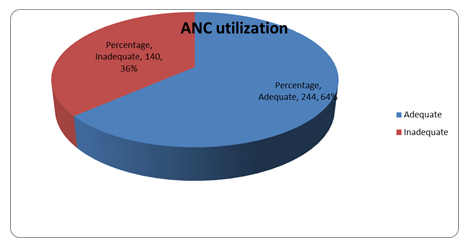
Results: Among 768 participants, male partners 167(43.5%) and pregnant women 171 (44.5%) had adequate knowledge on preeclampsia and eclampsia. More than a half 396(51.6%) of study respondents had weak myths while 372(48.4%) had strong myths on pre-eclampsia and eclampsia. Furthermore, pregnant women 244 (64%) had adequate antenatal care utilization. Study participants who had adequate knowledge on pre-eclampsia and eclampsia were almost 3 times more likely to utilize antenatal care services (AOR = 2.827; CI = 1.719 – 4.651; p<0.001). Study participants who had weak myth on pre-eclampsia and eclampsia were less likely to have adequate antenatal care attendance ( (AOR= 0.370; CI= 0.229; p< 0.001).
Conclusion: The overall knowledge on preeclampsia and eclampsia was low. Majority of the female had adequate antenatal service utilization. Majority of respondents had weak myths
Keywords
Myths, Pregnant Women and their Male Partners (Expecting Couples), ANC Utilization, Preeclampsia, Eclampsia
Article Details
Abbreviations:
ANC: Antenatal Clinic; AIDS: Acquired Immuno Deficiency Syndrome; BEmONC: Basic Emergency Obstetric and Newborn Care; CEMONC: Comprehensive Emergency Obstetric and Newborn Care; DC: District Council; HBM: Health Belief Model; HELLP: Hemolysis, Eleveted Liver enzyme, Low Platelet Count; H/F: Health facility; HSSP: Health Sector Strategic Plan; MDGs: Millennium Development Goals; MOHsw: Ministry of Health and Social warefare; PCA: Principal Component Analysis RCH: Reproductive and Child Health; SPSS: Statistical Package for Social Sciences; TDHS: Tanzania Demographic Health Survey; TC: Town Council; UDOM: University of Dodoma; URT: United Republic of Tanzania; UNFPA: United Nation Fund for Population Activities, UNICEF: United Nation International Children emergence Fund; USA: United State of America; WHO: World Health Organization
1. Background
Globally the Millennium development goals report shows that from 1990 to 2013 there was a decline of maternal deaths by 45% (289,000) per year [1]. However about 830 women died every day due to pregnancy complications or during delivery in 2015, meanwhile, perinatal mortality accounts for 40% of infants death globally [2]. So far, in Sub-Sahara 179 000 women die each year during pregnancy and childbirth [1]. According to the Tanzania Demographic Health Survey, the maternal mortality ratio accounts for 556 deaths per 100,000 live births while the perinatal mortality rate shows 39 deaths per 1000 pregnancies [3].
Pregnancy induced hypertension is a sign of underlying pathology which appears for the first time during pregnancy and it is a common medical complication of pregnancy [4]. Pregnancy induced hypertension , including preeclampsia and eclampsia, are the major health problem and the main cause of the maternal and perinatal morbidity and mortality. In Tanzania, the incidence of preeclampsia and eclampsia is found to be 1.7% [5]. According to the Tanzania Demographic Health survey, it shows that pregnancy induced hypertension is the second leading cause of maternal mortality which accounts for 19% of death [3]. To reduce the problem, the government set many strategies to ensure that the objectives are met. According to the Health sector strategic planning (HSSP IV) 2015- 2020 period, the following should be achieved: increasing skilled birth attendance by 80%, continue to expand provision of quality services during pregnancy, childbirth, and postnatal period, provision of Basic Emergency Obstetric and Newborn care (BEmONC) and Comprehensive Emergency Obstetric and Newborn care (CEMONC), also by the end of 2020, 70% of primary health facilities provide BEmONC and 50% of health centres and 100% of Hospitals provide CEMONC, also to ensure community awareness activities reach every household to achieve SDGs 4&5 [6].
There are several factors that lead to the high maternal and perinatal morbidity and mortality in the Global south such as Tanzania and the reasons are very crucial [7]. In the community perspectives, many factors involved such as knowledge gaps, myths regarding preeclampsia and eclampsia, traditional beliefs and inaccessibility of health care services during pregnancy [8]. Lack of knowledge, myths about danger signs of pregnancy makes the family not to put into considerations the early signs and symptoms of preeclampsia and eclampsia as a results delay to seek health care services [8]. So far, Men in Tanzania have inadequate knowledge regarding reproductive issues compared with women [9]. In turn men are the decision maker in all matters related to family issues including health services utilization which bring a negative impact on the mat ernal and perinatal outcome [10]. Moreover, empowering men with essential information on emergency obstetric condition such as preeclampsia and eclampsia is a vital strategy towards utilization of services in reducing maternal and perinatal morbidity and mortality [11].
Previously study done in Makole Ward Dodoma Tanzania about knowledge on preeclampsia among women results revealed 41% had a low level of knowledge about preeclampsia and eclampsia, half of the respondents agreed that the disease is due to evil spirit and exposure to fire while the remaining disagreed [12]. Another study done in Same District Hospital, the results showed that only 40% had knowledge of preeclampsia while the majority (60%) had no knowledge [13]. A study done in Sindh Pakistan, the findings revealed that preeclampsia was not recognized as a disease; however, women were aware of high blood pressure and can develop during pregnancy. Women believed that stress and weakness were conditions that cause high blood pressure and headache during pregnancy [14]. Little is known on the knowledge and myth on pre-eclampsia and eclampsia and its influence in antenatal attendance in rural community of Tanzania.
2. Methods
hToc18058281">2.1 Study areaThis study was conducted in Mtwara region. The Region covers the total area of 16,710km2 (6,450sqmi). Administratively the Region is divided into nine districts that are Mtwara Municipal, Newala DC, Tandhimba, Masasi DC, Nanyumbu, Masasi TC, Mtwara DC, Newala TC, and Nanyamba TC. The region has a total of 253 health facilities of which there are 6 Hospitals, 22 Health centres and 225 Dispensaries Almost all facilities are providing ANC services like physical examination of pregnant women, Health education about danger signs of pregnancy, testing and counseling for HIV/AIDS, Vaccination of Tetanus toxoid, micronutrients provision and checking for Hemoglobin level etc.
A community based analytical cross sectional study was conducted. The study employed a quantitative research approach. This design was chosen so as to assess the community’ myths about preeclampsia and eclampsia towards Antenatal services utilization.
The study involved 4 districts namely Mtwara DC, Newala, Nanyumbu, and Masasi. In each District two wards were involved, making a total of eight wards, At village level three villages from each ward were involved making a total of 24 villages.
Pregnant women who were in second and third trimester with their Male partners. This group was at risk group for preeclampsia and eclampsia since the women were pregnant and were the one who expected to utilize ANC services. Furthermore male partners are the decision maker in family level even regarding the health of their spouse.
Since there was no any documented study done in Mtwara Region showing the prevalence of preeclampsia and eclampsia, this study used a prevalence of 50% as a standard to calculate the sample size. By using the Kish Leslie formula as follows: -
N=Z2xP (100-P)
E2
Whereby
N= sample size
Z= Confident interval to 95% (1.96)
P= Prevalence (50%)
E= Worst acceptable margin error (0.05)
HENCE:
N= (1.96)2x50/100(100-50/100)
(0.05)2
N= 384.16. Therefore the sample size was 384 couples. Pregnant women and their male partiners. The total participants 768
The region was selected purposively because of an increasing number of preeclampsia and eclampsia and women reported at the health facility while already had eclamptic fit as seen earlier in RCH report of 2018. Then districts, wards, and villages employed multistage sampling. Mtwara Region has nine districts namely Mtwara municipal, Mtwara district, Masasi district, Newala district, Nanyumbu district, Masasi Town council, Newala Town council, Tandahimba district Council and Nanyamba Town Council. The main indigenous ethnic groups in Mtwara Region are Makonde, Makua, Yao, Wamatambwe and Mwela. Makonde is the dominant tribe which is found in all councils except Nanyumbu DC Makonde tribe made 70% of the Population [3]. Generally the people of Mtwara Region share the same characteristics due to their ethinic origin Table 1.
The first stage was a selection of four Districts (Mtwara DC, Nanyumbu, Newala and Masasi DC) out of nine districts within Mtwara Region. Simple random sampling using the lottery method was used to select the districts. A list of all districts was obtained and the names of the districts were listed. Pieces of paper were divided according to the number of districts and the names of the district were written in each small piece of paper then each piece of paper was folded and put together in a box. Then the box was shaken and four pieces were picked at random and names of districts were identified. The second stage was a selection of wards whereby all wards in each district (21 Wards of Mtwara DC, 17 Wards of Nanyumbu district, 22 Wards of Newala district and 34 Wards of Masasi district) were listed. By using the lottery method two wards from each district were selected randomly to obtain a total of 8wards. The third stage was selection of three villages from each selected ward by repeating the same procedure to obtain a total of 24 villages. The fourth stage was a selection of participants from each village whereby a list of pregnant women with gestation age of 24 weeks and above who lived with a male partner was obtained from a ten cell leader and eligible participants were given a number, thereafter by the use of lottery method simple random procedure was employed to select 16 expecting couples who met inclusion criteria from each village.
|
S/N |
Councils |
Major Ethnicity Groups |
|
1 |
Mtwara District |
Makonde |
|
2 |
Newala DC |
Makonde |
|
3 |
Masasi District |
Makua, Yao and Makonde |
|
4 |
Tandahimba DC |
Makonde and Makua |
|
5 |
Mtwara-Mikindani MC |
Makonde, Mwela, Yao and Makua |
|
6 |
Nanyumbu DC |
Makua and Yao |
|
7 |
Masasi TC |
Makua, Makonde, Mwela and Yao |
|
8 |
Nanyamba TC |
Makonde |
|
9 |
Newala TC |
Makonde |
Table 1: Major Tribes by Council, Mtwara Region, 2015.
2.7 Inclusion criteria
All pregnant women including prime gravid and multigravid who were in the second and third trimester, gestation age of 24 weeks and above who lived together with their male partners who were willing to participate in the study. These groups provided valid information on their knowledge and myths about preeclampsia and eclampsia.
Pregnant women and their partners who were very sick, mentally incapable and who refused to be involved in this study.
2.9 Research instruments
The tool used to collect data was a structured questionnaire, with closed ended questions and open-ended questions. The questionnaire was divided into four sections. Social-demographic and social economic characteristics, questions for measuring knowledge, myths and Antenatal service utilization. Social demographic and social economic characteristics adapted from NBS, 2015. The questions were translated in Swahili language and the whole questionnaire took 30 minutes to complete.
2.10 Data collection process
Data were collected through interviewer structured questionnaires. A researcher together with research assistants interviewed the eligible respondents whereby the researcher and research assistant filled the questionnaire the response from the participants. Ten research assistants were involved in data collection after being trained before the process commenced.
2.11 Data processing and analysis
Data obtained were coded manually and then were entered into the computer and cleaned. Data analysis was finally done by using statistical package for the social sciences (SPSS) computer software version 20. Frequencies and cross tabulations were done. Data were summarized into frequency tables, figures and chi square were done to look for an association between demographic variable and outcome variables. Logistic regressions were used to determine the strength of association between selected variables and outcome variable. Moreover, a P-value and confidence interval used to verify the significance of the differences found. A P-value < 0.05 was considered to be statistically significant. The principal component analysis was also done to find out the weighted score of the questions asked. A weighted score of >0.3 was regarded as relevant.
2.12 Measurements of the variables
2.12.1 Level of knowledge about preeclampsia and eclampsia: Knowledge on preeclampsia and eclampsia was measured by nominal scale involving 38 items on knowledge with yes/no answers which were then converted into correct and incorrect. Unnecessary questions were rejected and remained with 11questions for analysis. Then one score for each correct answer and zero score for each wrong answer [12]. Therefore those who scored 50% and above were termed as having adequate knowledge and below 50% inadequate knowledge.
2.12.1 Myths on preeclampsia/eclampsia:
Questionnaires adapted and modified from [17]. This involved 6 open ended questions which made a total of 32 responses regarding myths on preeclampsia and eclampsia. Difference responses were obtained from the respondents. Similar responses were grouped and then coded and 32 responses obtained. Therefore myths were measured by employing principle component analysis Myths were computed by using principal component analysis (PCA). The first analysis was done to 32 responses regarding myths to give weight to each question. During analysis 14 components were obtained and component one was selected since it had a high variance of 9.674. 21 responses had weight less than 0.3 therefore excluded from the component matrix and 11 responses remained. The second analysis was involved with 11 responses and four (4) components obtained whereby the variance of the component one raised from 9.674 to 23.627. All 11responses weighted above 0.3 and no question was excluded from the matrix. Responses which excluded from the component matrix as shown below Table 2. After PCA normality test was done and data were not normally distributed. Then the computed Mean= -0.0866278; Median = -0.1694712; Mode = -0.18007; Standard deviation = 0.79491721; Range = 4.55206; Min = -2.31358; Max = 2.23843. To categorize myths median was used as a cutoff point so as to get those who had strong Myths and those who had weak Myths about preeclampsia and eclampsia below the median weak Myth and above the Median strong Myth.
|
Responses |
Principal component analysis (PCA) |
|
|
First analysis |
Second analysis |
|
|
The local name for preeclampsia and eclampsia is devil` disease |
-0.284* |
|
|
The local name for preeclampsia and eclampsia is mental illness |
0.572 |
0.489 |
|
The local name for preeclampsia and eclampsia is God-made disease |
0.046* |
|
|
The local name for preeclampsia and eclampsia is magic disease |
-0.180* |
|
|
The local name for preeclampsia and eclampsia is big illness |
0.238* |
|
|
The local name for preeclampsia and eclampsia is Homa ya mdudu |
-0.104* |
|
|
The local name for preeclampsia and eclampsia is illness of the moon |
-0.238* |
|
|
Causes of preeclampsia and eclampsia is devils living in the wild, sea &big trees |
0.428 |
0.344 |
|
Causes of preeclampsia and eclampsia is Witch craft |
-0.155* |
|
|
Causes of preeclampsia and eclampsia is Mnyama(animal) |
-0.185* |
|
|
Causes of preeclampsia and eclampsia is mistreatment by in-law |
-0.183* |
|
|
Presentation of preeclampsia and eclampsia is convulsions (kukwijula) |
0.074* |
|
|
Presentation of preeclampsia and eclampsia is eye rolling back |
0.515 |
0.543 |
|
Presentation of preeclampsia and eclampsia is miso makasuku (red eye) |
0.138* |
|
|
Presentation of preeclampsia and eclampsia is Chidudu (headache) |
0.273* |
|
|
Presentation of preeclampsia and eclampsia is chakare( regular falling) |
-0.453 |
-0.585 |
|
Presentation of preeclampsia and eclampsia is Lyuni ( Dizziness) |
-0.183* |
|
|
Presentation of preeclampsia and eclampsia Kyokombe (heart burn) |
-0.220* |
|
|
The consequence of preeclampsia and eclampsia is premature baby (njiti) |
0.509 |
0.474 |
|
The consequence of preeclampsia and eclampsia is kuyiwa (loss of memory) |
0.198* |
|
|
The consequence of preeclampsia and eclampsia is death of the mother |
0.059* |
|
|
The consequence of preeclampsia and eclampsia is mental illness |
0.072* |
|
|
The consequence of preeclampsia and eclampsia Litulilye (intrauterine fetal death) |
-0.643 |
-0.601 |
|
Treatment of preeclampsia and eclampsia is drinking boiled green tree |
-0.274* |
|
|
Treatment of preeclampsia and eclampsia is special dance to expel demons/devils |
-0.395 |
-0.521 |
|
Treatment of preeclampsia and eclampsia is burning leaves or incense (ubani) |
0.380 |
0.371 |
|
Treatment of preeclampsia and eclampsia splashing human urine over the mother’ body with eclampsia |
0.379 |
0.329 |
|
Prevention of preeclampsia and eclampsia locally is tie a string of tree around the waist |
0.331 |
0.430 |
|
Prevention of preeclampsia and eclampsia locally is wear charms (hirizi) around the neck |
0.064* |
|
|
Prevention of preeclampsia and eclampsia locally is wear a black piece of cloth around the wrist |
0.176* |
|
|
Prevention of preeclampsia and eclampsia locally is boil the wood of the trees and bathe |
-0.431 |
0.563 |
|
Prevention of preeclampsia and eclampsia locally lie the pregnant mother under the bed. |
-0.184* |
|
Source: Researcher field data. Key: * Responses excluded from the component matrix.
Table 2: Questions about Myths used in PCA (N = 32Qns).
2.13 Antenatal service utilization
Involved 7 items adapted and modified from [20]. In Tanzania pregnant woman should attend Antenatal clinic at least four visits if she has no any problem until delivery. Therefore from 24 weeks the woman could have 2visits if she really started clinic in time which helped me to measure ANC utilization. First visit started when woman has gestation age of below 16 weeks, second visit 20 to 24 weeks, third visit 26 to 28 weeks and fourth visit 28 to 36 weeks. In inclusion criteria of 24 weeks and above this woman obviously attended ANC clinic not less than two visits. Therefore utilization was measured by number of recommended antenatal visits by WHO guideline. Therefore if the women attended ANC less than two visits was graded as inadequate utilization of ANC services and if attended two or more visits graded as adequate utilization of ANC service [19].
3. Results
3.1 Social- demographic characteristics of the participants
The study involved 384 couples who met inclusion criteria. Among them, female were 384 and male also were 384 which made a total of 768 participants. Results indicated that Majority of the participants 270 (36.0%) were in the age group, The mean age was 31.71 ± 8.056, median age 30.00, minimum age 18 and maximum age was 59. Regarding the education level of the participants, the large proportion of respondents 465 (60.0%) had primary education and a small proportion 92 (12.5%) had secondary education. Majority of the participants 665 (84%) were peasants and those who had three or more children were 260 (33.9%). Majority of the participants 605 (78.0%) had an income of less than 1000 T.shs per day. Large proportion 599 (78.0%) were able to access health facility when they face problems Table 3.
3.2 Level of knowledge about preeclampsia and eclampsia among pregnant women and their male partners
Majority of respondents 217 (56.5%) male and 213 (55.5%) female had inadequate knowledge on pre-eclampsia and eclampsia, only 167 (43.5) of male partners and 171 (44.5) of pregnant women had adequate knowledge on pre-eclampsia and eclampsia Figure 1.
3.3 Responses to specific questions involved in assessing knowledge on pre-eclampsia and eclampsia
Majority of both pregnant women 248 (64.6%) and their male partners 220 (57.3%) did not know whether pre eclampsia is a hypertensive disorder; majority of them did not respond correctly on the risk factors of preeclampsia [268 (69.8% of pregnant women and 302 (78.6) did not know whether pre existing history of high blood pressure can lead to pre eclampsia]; Also majority of respondents failed to repond correctly on the signs of pre-eclampsia [201 (52.3%)of pregnant women and 198 (51.6) responded incorrectly on severe headache; 285 (74.2%) of pregnant women and 269 (70.1%) on visual disturbance] Table 4. The relationship between socio-demographic characteristics and level of knowledge. The variable which showed significant relationship with knowledge were employment status (p<0.001), ethnicity (p<0.001), parity (p<0.001), access to health facility (p<0.001),walking distance to a nearby health facility (p<0.001) and access to mobile phone (p=0.004) Table 5.
3.4 Predictors of knowledge on pre eclampsia and eclampsia
After controlling for confounders, predictors of knowledge were occupation status [Unemployed AOR=0.17at 95% CI=0.049-0.592, p=0.005; self employed AOR=0.095 at 95% CI= 0.024-0.373, p=0.001]; Ethnicity [Makuwa AOR=2.814 at 95% CI= 1.944-4.074,p<0.001; Yao AOR=5.48 at 95% CI=2.977-10.086, p<0.001; Others AOR=4.902 at 95% CI=2.599-9.244, p<0.001]; Parity [One AOR=0.344 at 95% CI=0.203-0.584,p<0.001;Two AOR= 0.4 at 95% CI=0.239-0.668, p<0.001]; Walking distance [5km or more AOR=0.093 at 95% CI=0.02 -0.434, p=0.003] Table 6.
3.5 Myths about preeclampsia and eclampsia among pregnant women and their male partners
The findings revealed that the majority of the participants 236 (30.7%) reported that the local name for preeclampsia and eclampsia is the devils disease and 12 (1.6%) said that it is a big illness. Majority of the participants 286 (37.2%) said preeclampsia and eclampsia is due to devils living in the wild, sea and big trees while 145 (18.9%) said that mistreatment from in-law was the cause. 191 (24.9%) reported that the presentation of preeclampsia and eclampsia is heart burn (Kyokombe) while 139 (18.1%) said eye rolling back. Regarding the consequence of preeclampsia and eclampsia, 392 (51.0%) reported mental illness while 192 (25.0%) reported intrauterine fetal death (Litulilye) Table 7.
3.6 Myths about preeclampsia and eclampsia
The results showed that 51.6% had weak Myths and 48.4% had strong Myths about preeclampsia and eclampsia Figure 2.
3.7 Antenatal care service utilization
The current study was also assessed ANC utilization among expecting mothers in Mtwara region N = 384. ANC utilization was defined as adequate if the women had at least two visits or more otherwise was inadequate keeping in mind that the current study dealt with the women who were in second and third trimester with the gestation age of 24 weeks and above together with their male partners. The total female participants were 384 and their findings regarding ANC services revealed that majority 244 (64%) had an adequate utilization since they attended two or more visits and 140 (36%) had an inadequate utilization as they attended less Figure 3.
3.8 Association between the level of knowledge and antenatal care service utilization
A Chi-square was done to show the relationship between knowledge and antenatal care services utilization then bivariate and Multivariate logistic regression was done. The findings showed that those who had adequate knowledge were all most 3 times more likely to utilize antenatal services compared to those who had inadequate knowledge (AOR = 2.827; CI = 1.719, 4.651; P = 0.000). Also those who had three or more children were 2 times more likely to utilize ANC services compared to those who had no children (AOR = 2.148; CI = 1.030, 4.483; P = 0.042). Other factors showed no association Table 8.
3.9 The association between myths about preeclampsia and eclampsia and antenatal care services utilization
A Chi-square done to show the relationship between Myths about preeclampsia and eclampsia and antenatal care services utilization then Bivariate and Multivariate logistic regression done. The findings showed those who had weak myths were 63% less likely to utilize ANC services compared to those who had strong myths. (AOR = 0.370; CI = 0.229, 0.599; P = 0.000). Furthermore, other factors showed no association Table 9.
|
Variable |
Frequency (n) |
Percentage (%) |
|
Age group |
||
|
18-25 |
197 |
25.0 |
|
26-33 |
270 |
36.0 |
|
34-41 |
188 |
24.0 |
|
42+ |
113 |
15.0 |
|
Sex |
||
|
Male |
384 |
50.0 |
|
Female |
384 |
50.0 |
|
Education level |
||
|
No formal education |
211 |
27.5 |
|
Primary |
465 |
60.5 |
|
Secondary |
92 |
12.5 |
|
Occupation |
||
|
Employed |
16 |
2.1 |
|
Unemployed |
61 |
7.9 |
|
Self employed |
46 |
6.0 |
|
Peasant |
665 |
84.0 |
|
Religion |
||
|
Christian |
161 |
21.0 |
|
Muslim |
607 |
79.0 |
|
Ethnicity |
||
|
Makonde |
285 |
37.1 |
|
Makuwa |
335 |
43.6 |
|
Yao |
82 |
10.7 |
|
Others |
66 |
8.6 |
|
Number of children |
||
|
One |
162 |
21.1 |
|
Two |
193 |
25.1 |
|
Three or more |
260 |
33.9 |
|
None |
153 |
19.9 |
|
Access to health facility |
||
|
Yes |
599 |
78.0 |
|
No |
169 |
22.0 |
|
Distance to health facility |
||
|
< than 5 Kilometer |
586 |
76.3 |
|
>than 5 Kilometer |
182 |
23.7 |
|
Daily income |
||
|
<than 1000 T.shs |
605 |
78.8 |
|
>than 1000 T.shs |
163 |
21.2 |
Table 3: Social-demographic distribution of the participants (N=768).
|
Variable |
Pregnant Women |
Male partners |
||
|
Frequency |
Percent |
Frequency |
Percent |
|
|
Preeclampsia is Hypertension in Pregnancy |
||||
|
Correct response |
136 |
35.4 |
164 |
42.7 |
|
Incorrect response |
248 |
64.6 |
220 |
57.3 |
|
Risk factor for preeclampsia is history of high blood pressure before conception |
||||
|
Correct response |
116 |
30.2 |
82 |
21.4 |
|
Incorrect response |
268 |
69.8 |
302 |
78.6 |
|
Risk factor for preeclampsia is Overweight |
||||
|
Correct response |
152 |
39.6 |
116 |
30.2 |
|
Incorrect response |
232 |
60.4 |
268 |
69.8 |
|
Symptom of preeclampsia is severe headache |
||||
|
Correct response |
183 |
47.7 |
186 |
48.4 |
|
Incorrect response |
201 |
52.3 |
198 |
51.6 |
|
Symptom of preeclampsia is Increase urine out put |
||||
|
Correct response |
240 |
62.5 |
204 |
53.1 |
|
Incorrect response |
144 |
37.5 |
180 |
46.9 |
|
Symptom of preeclampsia is Visual disturbance |
||||
|
Correct response |
99 |
25.8 |
115 |
29.9 |
|
Incorrect response |
285 |
74.2 |
269 |
70.1 |
|
Symptom of preeclampsia is Epigastric pain ( central just below the ribs |
||||
|
Correct response |
131 |
34.1 |
125 |
32.6 |
|
Incorrect response |
253 |
65.9 |
259 |
67.4 |
|
Symptom of preeclampsia is Sudden swelling of the face, hands or feet |
||||
|
Correct response |
135 |
35.2 |
133 |
34.6 |
|
Incorrect response |
249 |
64.8 |
251 |
65.4 |
|
Sign of preeclampsia is Convulsions(fits) |
||||
|
Correct response |
176 |
45.8 |
157 |
40.9 |
|
Incorrect response |
208 |
54.2 |
227 |
59.1 |
|
Sign of preeclampsia is Loss of consciousness |
||||
|
Correct response |
165 |
43 |
151 |
39.3 |
|
Incorrect response |
219 |
57 |
233 |
60.7 |
|
Complication of preeclampsia is Maternal death |
||||
|
Correct response |
121 |
31.5 |
135 |
35.2 |
|
Incorrect response |
263 |
68.5 |
249 |
64.8 |
|
Complication of preeclampsia is Fetal death |
||||
|
Correct response |
193 |
50.3 |
169 |
44 |
|
Incorrect response |
191 |
49.7 |
215 |
56 |
|
Use of salt free diet |
||||
|
Correct response |
194 |
50.5 |
139 |
36.2 |
|
Incorrect response |
190 |
49.5 |
245 |
63.8 |
Table 4: Responses to specific questions involved in assessing knowledge on pre-eclampsia and eclampsia.
|
Variable |
Adequate knowledge n(%) |
Inadequate knowledge n(%) |
X |
P-Value |
|
Education level |
||||
|
No formal education |
86(40.8) |
125(59.2) |
||
|
Primary |
211(45.4) |
254(54.6) |
||
|
Secondary |
41(44.6) |
51(55.4) |
1.269a |
0.53 |
|
Occupation |
||||
|
Employed |
10(62.5) |
6(37.5) |
||
|
Unemployed |
20(32.8) |
41(67.2) |
||
|
Self employed |
9(19.6) |
37(80.4) |
||
|
Peasant |
299(46.4) |
346(53.6) |
17.934a |
<0.001 |
|
Religion |
||||
|
Christian |
63(39.1) |
98(60.9) |
||
|
Muslim |
275(45.3) |
332(54.7) |
1.969a |
0.161 |
|
Ethinicity |
||||
|
Makonde |
85(29.8) |
200(70.2) |
||
|
Makuwa |
167(49.9) |
168(50.1) |
||
|
Yao |
39(47.6) |
43(52.4) |
||
|
Others |
47(71.2) |
19(28.8) |
48.151a |
<0.001 |
|
Parity |
||||
|
One |
52(32.1) |
110(67.9) |
||
|
Two |
73(37.8) |
120(62.2) |
||
|
Three or more |
125(48.1) |
135(51.9) |
||
|
None |
88(57.5) |
65(42.5) |
25.397a |
<0.001 |
|
Access to H/F |
||||
|
Yes |
286(47.7) |
313(52.3) |
||
|
No |
52(30.8) |
117(69.2) |
15.417a |
<0.001 |
|
Walking distance to a nearby H/F |
||||
|
Less than 5KM |
287(49) |
299(51) |
||
|
5Km or more |
51(28) |
131(72) |
24.745a |
<0.001 |
|
Sex |
||||
|
Male |
167(43.5) |
217(56.5) |
||
|
Female |
171(44.5) |
213(55.5) |
.085a |
0.771 |
|
Own Mobile phone |
||||
|
No |
52(34.2) |
100(65.8) |
||
|
Yes |
286(46.6) |
328 (53.4) |
7.561 |
0.004 |
Table 5: The relationship between socio-demographic characteristics and level of knowledge.
|
Variable |
95%CI |
p-value |
||
|
AOR |
Lower |
Upper |
||
|
Occupation |
||||
|
Employed |
1 |
|||
|
Unemployed |
0.17 |
0.049 |
0.592 |
0.005 |
|
Self employed |
0.095 |
0.024 |
0.373 |
0.001 |
|
Peasant |
0.518 |
0.171 |
1.57 |
0.245 |
|
Ethinicity |
||||
|
Makonde |
1 |
|||
|
Makuwa |
2.814 |
1.944 |
4.074 |
<0.001 |
|
Yao |
5.48 |
2.977 |
10.086 |
<0.001 |
|
Others |
4.902 |
2.599 |
9.244 |
<0.001 |
|
Parity |
||||
|
None |
1 |
|||
|
One |
0.344 |
0.203 |
0.584 |
<0.001 |
|
Two |
0.4 |
0.239 |
0.668 |
<0.001 |
|
Three or more |
0.689 |
0.426 |
1.116 |
0.13 |
|
Access to H/F |
||||
|
Yes |
1 |
|||
|
No |
4.518 |
0.955 |
21.382 |
0.057 |
|
Walking distance to a nearby H/F |
||||
|
Less than 5KM |
1 |
|||
|
5Km or more |
0.093 |
0.02 |
0.434 |
0.003 |
|
Yes |
1 |
|||
|
No |
0.715 |
0.474 |
1.08 |
0.111 |
Table 6: Predictors of knowledge on pre eclampsia and eclampsia.
|
Variable |
Frequency |
Percentage |
|
(n) |
(%) |
|
|
Local name for preeclampsia and eclampsia |
||
|
The devil disease |
236 |
30.7 |
|
Snake illness |
180 |
23.4 |
|
God-made disease |
41 |
5.3 |
|
Magic disease |
102 |
13.3 |
|
Big illness |
12 |
1.6 |
|
Homa ya mdudu |
92 |
12 |
|
Illness of the moon |
105 |
13.7 |
|
Myths regarding the cause of preeclampsia and eclampsia |
||
|
Devils living in the wild, sea and big trees. |
286 |
37.2 |
|
Witch craft |
173 |
22.5 |
|
Mnyama (animal) |
164 |
21.4 |
|
Mistreatment by in-law |
145 |
18.9 |
|
The consequence of preeclampsia & eclampsia |
||
|
Njiti (Premature baby) |
88 |
11.5 |
|
Loss of memory (Kuyiwa) |
46 |
6 |
|
Death of the mother |
50 |
6.5 |
|
Mental illness |
392 |
51 |
|
Litulilye (intrauterine fetal death) |
192 |
25 |
|
Local treatment of preeclampsia and eclampsia |
||
|
Drinking boiled green leaves. |
287 |
37.4 |
|
Special dance to expel demons/devils |
190 |
24.7 |
|
Burning leaves or incense (kufukiza ubani) |
141 |
18.9 |
|
Splashing of human urine over the mother`s body with eclampsia |
150 |
19.5 |
|
Local prevention of preeclampsia and eclampsia |
||
|
Tie string of tree on the waist |
173 |
22.5 |
|
Wear charms- (Hirizi) around the neck |
181 |
23.6 |
|
Wear of black clothe on the hand |
78 |
10.2 |
|
Boil the wood of trees and bathe |
157 |
20.4 |
|
Lie the pregnant mother under the bed. |
179 |
23.3 |
Table 7: Myths about preeclampsia and eclampsia (N= 768).
|
Variable |
AOR |
p-value |
95% confident interval |
|
|
Lower |
Upper |
|||
|
Knowledge |
||||
|
Adequate |
2.827 |
0 |
1.719 |
4.651 |
|
Inadequate(Ref) |
||||
|
Occupation |
||||
|
Employed |
0.49 |
0.48 |
0.068 |
3.547 |
|
Unemployed |
0.891 |
0.805 |
0.357 |
2.225 |
|
Self employed |
3.385 |
0.076 |
0.878 |
13.047 |
|
Peasant (Ref.) |
||||
|
Ethnicity |
||||
|
Makonde |
0.304 |
0.062 |
0.087 |
1.063 |
|
Makuwa |
0.37 |
0.122 |
0.105 |
1.306 |
|
Yao |
1.104 |
0.898 |
0.241 |
5.052 |
|
Others (Ref.) |
||||
|
Number of children |
||||
|
One |
1.712 |
0.164 |
0.802 |
3.652 |
|
Two |
1.315 |
0.489 |
0.606 |
2.851 |
|
Three or more |
2.148 |
0.042 |
1.03 |
4.483 |
|
None (Ref.) |
||||
|
Access to health facility |
||||
|
Yes |
2.072 |
0.353 |
0.445 |
9.637 |
|
No (Ref.) |
||||
|
Distance to health facility |
||||
|
Less than 5 kilometer |
0.297 |
0.113 |
0.067 |
1.33 |
|
More than 5 Kilometer (Ref.) |
||||
|
Wealth index |
||||
|
Poorest (Ref.) |
||||
|
Poor |
0.542 |
0.668 |
0.033 |
8.904 |
|
Middle |
1.092 |
0.755 |
0.628 |
1.898 |
|
High |
0.402 |
0.004 |
0.216 |
0.751 |
Table 8: Multivariate logistic regression between knowledge level about preeclampsia and eclampsia and ANC utilization (N =384).
|
Variable |
AOR |
p-value |
95% confident interval |
|
|
Lower |
upper |
|||
|
Myths |
||||
|
Weak myths |
0.37 |
0 |
0.229 |
0.599 |
|
Strong myths (Ref.) |
||||
|
Occupation |
||||
|
Employed |
0.495 |
0.499 |
0.064 |
3.807 |
|
Unemployed |
0.696 |
0.435 |
0.279 |
1.732 |
|
Self employed |
3.816 |
0.05 |
1.002 |
14.533 |
|
Peasant (Ref.) |
||||
|
Ethnicity |
||||
|
Makonde |
0.346 |
0.1 |
0.098 |
1.225 |
|
Makuwa |
0.411 |
0.169 |
0.116 |
1.46 |
|
Yao |
1.467 |
0.62 |
0.323 |
6.66 |
|
Others (Ref.) |
||||
|
Number of children |
||||
|
One |
1.54 |
0.258 |
0.729 |
3.254 |
|
Two |
1.214 |
0.622 |
0.562 |
2.623 |
|
Three or more |
1.772 |
0.125 |
0.853 |
3.68 |
|
None (Ref.) |
||||
|
Access to health facility |
||||
|
Yes |
1.955 |
0.394 |
0.418 |
9.139 |
|
No (Ref.) |
||||
|
Distance to health facility |
||||
|
Less than 5 kilometer |
0.291 |
0.108 |
0.065 |
1.31 |
|
More than 5 Kilometer (Ref.) |
||||
|
Wealth index |
||||
|
Poorest (Ref.) |
||||
|
Poor |
0.407 |
0.539 |
0.023 |
7.185 |
|
Middle |
0.963 |
0.893 |
0.556 |
1.669 |
|
High |
0.361 |
0.001 |
0.194 |
0.672 |
Table 9: Multivariate logistic regression between myths about preeclampsia and eclampsia and ANC utilization N = 384.
4. Discussion
The results of the current study showed that 56.5% of the male partners and 55.5% of the pregnant women had inadequate knowledge about preeclampsia and eclampsia. The results of this study differ in findings of previous work done in Makole Dodoma [12] which revealed that 41% of the respondents had low knowledge. These differences might be due to geographical location where the study conducted as the current study conducted in Rural while the previous conducted in Urban, also it could be due to differences in the study population as the current study dealt with both pregnant women and their male partners while the previous study focused mainly on pregnant women who are attending Antenatal clinic and get health education regarding their status. This finding also differ with [13]. findings which showed 60.0% of the respondents reported to have no knowledge. The findings of the present study showed that those who had adequate knowledge about preeclampsia and eclampsia were 43.5% male partners and 44.5% pregnant women. The present findings seem to be in line with other research done in Same Moshi Tanzania [13] which found that 40% reported having adequate knowledge on preeclampsia and eclampsia [16]. The findings might be due to the unplanned or absence of educational program regarding preeclampsia and eclampsia in the health facility and in the community.
Following the present results, previous studies have demonstrated that the local name was `Rt jho dabao vadhan` meaning that high blood pressure [14]. Another study was done in Southern Mozambique [17] reported that the local name for preeclampsia and eclampsia were falling disease, fainting disease, snake illness or childhood illness. This inconsistency of the findings might be due to the different study area and social demographic characteristics of the participants. Regarding the causes, the current study 37.2% of the participants reported that the cause was the devil living in the wild, sea, and big trees and 22.5% reported to be caused by frequency fever. These findings differ from the previous study [17] who reported the causes were mistreatment by in-laws, marital problems, and excessive thinking or worrying. These differences might be due to the cultural differences of the participants. Another important finding was that 10.5% of the respondents from the current study reported dizziness and Convulsions (kukwijula) were the signs and symptoms of preeclampsia and eclampsia. This is in line with the previous study [14] who reported the same findings. Drinking boiled green leaves was the local treatment of preeclampsia and eclampsia reported in the present study which accounts for 37.4% of the participants, special dance to expel demons/devils 24.7%, burning leaves or incense (ubani) 18.9%. These findings compared by the previous study [18] which showed that traditional treatment of preeclampsia were eating onions, drinking solution of the salt, bodily incisions and prayers. Another study [14] reported that the use of home remedies, spiritual treatment and alternative medicine. These findings imply that local treatment differs regarding culture, ethnicity and beliefs though there are some in common.
Antenatal care utilization among pregnant women who were in second and third trimester starting gestation age of 24 weeks and above. The results of the current study 64% of the pregnant women had adequate antenatal care service utilization. These results agree with the findings of other study done in Jordan [19] in which 63.4% of the respondents had adequate ANC service utilization. It seems possible that these results might be due to an increasing number of health facilities in each village also the effort done by the government to ensure that every pregnant woman should be attended by the trained personnel as well as free services offered to pregnant women. A similar study was done Eastern Napel [20] which showed that 69% of the participants had higher antenatal care service utilization. Furthermore, the current study indicated that those who had inadequate ANC service utilization were 36%. These results differ from the study done in Geita Tanzania [21] which showed the extremely low ANC attendance by 3.62%. This inconsistency might be due to the social cultural beliefs, lack of knowledge regarding the importance of ANC utilization. It might be also the nature of the participants regarding their activities as the majority of the participants in Geita engaged in animal keeping and they tends to move from one place to another to fetch food for their animals. Therefore, this might be the reason for inadequate ANC utilization.
The current study determine the association between knowledge of preeclampsia and eclampsia towards ANC utilization which showed statistically significant association whereby those who had adequate knowledge about preeclampsia and eclampsia were 3 times more likely to utilize antenatal care service compared to those who had inadequate knowledge (P–value <0.05). Different from the study done in Napel [20] which showed that those respondents who had knowledge were 5 times more likely to have antenatal care utilization compared to those who did not have knowledge .These findings seemed to have difference since the current study was conducted in a developing country where the majority of their people had a primary level of education and were not much exposed to social media where can search information compared to the previous study which was conducted in a developed country. Therefore, women should be equipped with knowledge regarding their health and this could facilitate them to utilize antenatal care services. Knowledge can influence an individual to see the importance of seeking health services. The current study showed that only 43.5% of the male partners had adequate knowledge on preeclampsia and eclampsia and are the ones who are decision maker within the family level, therefore empowering men with adequate knowledge about reproductive health issues including preeclampsia and eclampsia will facilitate them to encourage their partners to attend ANC care. The knowledge of preeclampsia and eclampsia will also help the community to Identify the early signs and symptoms of the problem and take appropriate measures without delaying in seeking care as well as motivate them to attend antenatal care since they know the consequence of the problem and eventually reducing maternal morbidity and mortality rate due to preeclampsia and eclampsia in the country.
The findings showed that those who had weak myths were less likely to utilize ANC services compared to those who had strong myths (P = 0.000). These findings differ from the previous study [20] which showed that those who believed from traditional healers were less likely to have antenatal care service utilization than those who did not believe tradition healers . These inconsistency results might be due to lack of adequate knowledge about preeclampsia and eclampsia though the participants had weak myths also resistance in behavior change. It might be also they did not see any benefit obtained through utilizing antenatal services. Furthermore, although the present study showed a number of respondents who had strong myths are low but still more effort is needed to dispel myths and misconceptions in the community at large and ensure all pregnant women are utilizing antenatal services for the benefit of both mother and unborn baby.
5. Conclusion
The overall knowledge about preeclampsia and eclampsia was low. Majority of the participants had weak myths although the different with those who had strong myths was small. The majority of the pregnant women utilized antenatal care services. Furthermore, findings showed that those with adequate knowledge had adequate antenatal services utilization. Moreover, those who had strong myths found to have antenatal care services utilization. Therefore, the community should be educated regarding the facts about preeclampsia and eclampsia in order to dispel the available Myths and misconceptions and ensure ANC services utilization for all pregnant women inorder to prevent complications of pregnancy.
Declarations
Ethical approval and consent to participate
Ethical clearance was obtained from University of Dodoma ethics and committee before commencing the data collection. Also permission to conduct the study obtained from the Regional administrative secretary of Mtwara, District Administrative secretaries of Mtwara District council, Newala, Nanyumbu and Masasi DC. The permission letters obtained were presented to Ward Executive officers, and Village leaders who granted me a permission to conduct study in their respective areas. Written consent was obtained from each participant before data collection.
Consent for publication
Not applicable
Availability of data and materials
The dataset used and /or analyzed during the current study are available from corresponding author on reasonable request.
Competing of interests
The author declares that there was no conflict of interest.
Funding
There was no external source of funding used for this study.
Author’s contributions
SMK senior supervisor assisted in data analysis, NG, FM and AL contributed to the interpretation of data. All authors read, commented on and approved the final manuscript.
Acknowledgements
My sincere gratitude goes to the University of Dodoma, Regional administrative secretary of Mtwara region, Districts administrative secretaries of Mtwara DC, Newala, Nanyumbu and Masasi DC, all Districts executives’ directors (DED), Ward Executive officers (WEO) and Village leaders who granted me a permission to conduct this study in their respective areas. I would also like to extend my deep appreciation and sincere gratitude to my supervisors, my research assistants, and the study participants for their willingness to participate in this study. I would also wishes to thank Dr. Secilia K. Ng`weshemi, Dr. Julius Ntwenya and Mr Ephraim K. Shilla for support and encouragement throughout the course of this study.
Author’s information
1Department of clinical Nursing- Division of Nursing and Midwifery services Ministry of health community development, Gender, Elderly and Children Box 743, Dodoma Tanzania. 2Acting Depute Principal Collage of Health Science, University of Dodoma Box 295 Dodoma Tanzania, 3Department of Public Health, University of Dodoma Box295 Dodoma Tanzania, 4 Department of health services, University of Dodoma Box 295 Dodoma Tanzania and 5 Department of Nursing and Midwifery, University of Dodoma Box 295 Dodoma Tanzania.
References
- WHO, UNICEF, UNFPA, The World Bank UN. Trends in Maternal Mortality: 1990 to 2013 (2014).
- WHO UNICEF, UNFPA WBG and the UN, Division P. Trends in maternal mortality: 1990 to 2015 (2015).
- Demographic and Health Survey and Malaria Indicator Survey (2015).
- Konar H. DC Dutta`s Textbook of Obstetrics. 8th editio. New Delhi London: Jaypee Brothers Medical Publisher (P) Ltd (2015).
- Ajah L, Ozonu N, Ezeonu P, et al. The feto-maternal outcome of preeclampsia with severe features and eclampsia. J Clin Diagn Res (2016).
- Health Sector Strategic Plan July 2015-June 2020 (2015).
- Maternal mortality (2016).
- Ogunjimi L, Ibe T, Ikorok M. Curbing maternal and child mortality. Int J Nurs midwifery 4 (2012).
- Iliyasu Z, Abubakar I, Galadanci H, et al. Birth preparedness, complication readiness and fathers’ participation in maternity care in a northern Nigerian community. Afr J Reprod Heal 14 (2010): 21-32.
- Bhatta D. Involvement of males in antenatal care, birth preparedness, exclusive breast feeding and immunizations for children in Kathmandu, Nepal. BMC Pregnancy Childbirth (2013).
- Nanjala M, Wamalwa D. Determinants of Male Partner Involvement in Promoting Deliveries by Skilled Attendants in Busia, Kenya. Glob J Heal (2012).
- Savage AR, Hoho L. Knowledge of pre-eclampsia in women living in Makole Ward, Dodoma, Tanzania 16 (2016): 412-419.
- Eze ED, Barasa A, Adams MD, et al. Determination, knowledge and prevalence of pregnancy-induced hypertension/eclampsia among women of childbearing age at Same District Hospital in Tanzania 10 (2018): 19-26.
- Khowaja AR, Qureshi RN, Sheikh S, et al. Community ’ s perceptions of pre-eclampsia and eclampsia in Sindh Pakistan?: a qualitative study. Reprod Health 13 (2016).
- 2012 Population and Housing Census. National Bureau of Statistics Microfinance Dar Es Salaam and Office of Chief Government Statistician President’s Office, Finance, Economy and Development Planning Zanzibar (2013).
- Zuo tey chiao, Teng see poh, Keng soon lean, et al. Knowledge of preeclampsia among antenatal women in atertiary referral teaching hospital. Malaysian J Nurs 7 (2016): 8-13.
- Boene H, Vidler M, Sacoor C, et al. Community perceptions of pre-eclampsia and eclampsia in southern Mozambique. Reprod Health 13 (2016).
- Akeju DO, Vidler M, Oladapo OT, et al. Community perceptions of pre-eclampsia and eclampsia in Ogun State , Nigeria?: a qualitative study. Reprod Health 13 (2016).
- Hijazi HH, Alyahya MS, Sindiani AM, et al. Determinants of antenatal care attendance among women residing in highly disadvantaged communities in northern Jordan: a cross-sectional study (2018): 1-18.
- Deo KK, Paudel YR, Khatri RB, et al. Barriers to utilization of antenatal care services in eastern Nepal 3 (2015): 1-7.
- Konje ET, Tito M, Magoma N, et al. Missed opportunities in antenatal care for improving the health of pregnant women and newborns in Geita district , Northwest Tanzania (2018): 1-13.
Appendix A: questionnaires
PART A: Demographic data (Write, circle the correct answer or answers)
Adapted from TDHS 2015/2016
- How old are you? ……….
- Sex A. Male B. Female
- What level of education did you attain?
- No formal education B. Primary C. Secondary D. Collage.
- What is your occupation?
- Employed B. Unemployed C. Self employed D. Peasant
- What is your Religion
- Christian B. Muslim
- Where do you live A. urban B. Rural.
- What is your ethnicity A. Makonde B. Makuwa C. Yao D. Others specify………….
- How many children do have? One B. Two C. Three and above
- What is gestation age of this pregnancy (in months)…….
- Do you able to access and afford to get health facility services A. Yea B. No
- How many kilometers from your home to health facility A. less than 5km B. More than five km.
- What is your daily income A. less than 1000Tshs B. More than 1000Tsh
Household characteristics (Adapted from TDHS 2015/2016) Tick
- What kind of toilet facility does members of your household use?
- Flush or pour flush toilet; Flush to piped sewer system [ ] Flush to septic tank [ ] Flush to pit latrine [ ] Flush to somewhere else [ ] Flush, don’t know where [ ]
- Pit latrine; Ventilated improved pit latrine [ ] Pit latrine with slab (washable) [ ] Pit latrine with slab (not washable) [ ] Pit latrine without slab/open pit [ ]
- Compositing toilet [ ]
- Bucket toilet [ ]
- No toilet/bush/field [ ]
- What type of fuel does your household mainly use for cooking?
- Electricity [ ]
- Bottled gas [ ]
- Parrafin/kerosene [ ]
- Charcoal [ ]
- Firewood [ ]
- Crop residuals [ ]
- Straw [ ]
- Grass [ ]
- Animal dunk [ ]
- No food cooked in household [ ]
- Other (Specify)…………….
- What is the source of energy for lighting in the household?
- Electricity [ ]
- Soler [ ]
- Gas [ ]
- Paraffine/urricane lamp [ ]
- Paraffine pressure lamp [ ]
- Paraffine-wick lamp [ ]
- Firewood [ ]
- Candle [ ]
- Other (specify)……………..
- How many rooms in this house are used for sleeping ………….
- Does any member of the family own any agricultural land? 1) Yes [ ] 2) No [ ]
- How many hectares own? …………..
- Does this house own any livestock? 1) Yes [ ] 2) No [ ]
- How many of the following animal does this house own?
Cows/Bulls ………., Other cattle………… Horses/Donkey/mules………., Goats…………., Sheep…………, Chicken/poultry…………….. None [ ]
- Does your household have;
Electricity [ ] Radio [ ] Television [ ] Non Mobile telephone [ ] Computer [ ] Refrigerator [ ] Battery [ ] Iron [ ]
- Does any member of this house own;
Watch [ ] Mobile phone [ ] Bicycle [ ] Motorcycle/Scooter [ ] Animal-drawn cart [ ] Car/Truck [ ] Boat with motor [ ]
Household observation
- Type of house: 1) Temporary [ ] 2) Permanent[ ] 3)
- Material of the floor 1) Earth/sand [ ] 2) Wood planks [ ] 3) Tiles [ ] 4) Cement/Concrete [ ]
- Material of the roof 1) None roof [ ] 2) Mud [ ] 3) Grass [ ] 4) Iron [ ]
- Material for the wall 1) None wall [ ] 2) Poles with mud [ ] 3) Grass [ ] 4) Stones with mud [ ] 6) Wood/Timber [ ] 7) Cement blocks [ ] 8) Blokes bricks [ ]
PART B: Knowledge about preeclampsia and eclampsia Questionnaire (circle correct answer or answers). 1dapted and modified form Angela Ruth Savage and Lujani Hoho, 2016
|
S/N |
Qn. |
Options |
Yes |
No |
|
1 |
Do you know what preeclampsia is? |
a) Male disorder |
||
|
b) Mental disorder |
||||
|
c) Orthopedic disorder |
||||
|
d) Childhood disorder |
||||
|
e) Hypertension in Pregnancy |
||||
|
2 |
Which of the following are the risk factors for preeclampsia? |
a) diabetes |
||
|
b) Evil sprit |
||||
|
c) A history of high blood pressure before conception |
||||
|
d) Exposure to fire during pregnancy |
||||
|
e) Overweight |
||||
|
f) Singleton pregnancy |
||||
|
3 |
Which of the following symptoms may be experienced in preeclampsia? |
a)severe headache |
||
|
b) Increase urine out put |
||||
|
c) Visual disturbance |
||||
|
d) Epigastric pain ( central just below the ribs |
||||
|
e)severe back pain |
||||
|
f) Sudden swelling of the face, hands or feet |
||||
|
4 |
Which of the following signs may be presented in eclampsia? |
a) Convulsions(fits) |
||
|
b) Loss of consciousness |
||||
|
c) Diarrhea |
||||
|
d) General body pain |
||||
|
e) abdominal pain |
||||
|
5 |
Which of the following are the complications of preeclampsia? |
a) Maternal death |
||
|
b) Risk for low blood pressure in subsequent pregnancy |
||||
|
c) Fetal death |
||||
|
d) Higher than average birth weight |
||||
|
e) Loss of memory after birth |
||||
|
6 |
Which of the following may help to prevent preeclampsia and its serious risks? |
a) Bed rest from 24th week |
||
|
b) Regular clinic attendance |
||||
|
c) Use of salt free diet |
||||
|
d) Regular exercise |
||||
|
e) Taking contraceptive every day |
||||
|
f) Do not know |
||||
|
7 |
Which of the followings are part of management of preeclampsia and eclampsia |
a)Admission to hospital in severe preeclampsia and eclampsia |
||
|
b) Use of medicine to treat infections |
||||
|
c) Early delivery if close to term |
||||
|
d) Use if vitamins c, D and E |
||||
|
e) Use of drugs that prevents fits |
||||
|
f) Return visit 6-8 weeks after delivery |
PART C: Myths open ended Questionnaire: adapted and modified from (Khowaja et al., 2016) and (Boene et al., 2016). This part based on 6 categories of items with open ended questions, thus are local terminology, causes, warning (danger) signs, preventive strategies, consequences and traditional treatments.
- What is/are the local name for preeclampsia and eclampsia in that area?
……………………………………………………………………………………………………………………………………………………………………
- What do you believe is the cause of preeclampsia and eclampsia?
……………………………………………………………………………………………………………………………………………………………………
- How do pregnant women with eclampsia present?
…………………………………………………………………………………………………………………………………………………………………….
- What are the consequences of preeclampsia and eclampsia?
………………………………………………………………….
- How do you treat eclampsia locally?
…………………………………………………………………………………………………………………………………………………………………….
- How do you prevent preeclampsia and eclampsia locally?
…………………………………………………………………………………………………………………………………………………………………………
PART D 1: questionnaire regarding antenatal service utilization. Choose and circle the answer or answers. Adapted and modified from Roseline Dansowaa Doe, 2013. To Be Filled By Pregnant Woman
- Are you living together with your partner?
- Yes B. No
- Does this pregnancy planned?
- Yes B. No
- Did you attend antenatal clinic?
- yes B. No
- When did you start first ANC booking?
- before 3 months B. After 3 months.
- How many times did you attend ANC clinic.
- One B. two or more C. I don’t know.
- Were you accompanied by your partner to the ANC clinic?
- Yes B. No
- How many times did your partner accompanied you to ANC clinic
- Once B. Twice C. Three or more.
Part D2: To be filled by a male partner
- Are you living together with your partner?
- Yes B. No
- Is the pregnancy planned?
- Yes B. No
- Did she attend antenatal clinic?
- yes B. No
- When did she start first ANC booking?
- before 3 months B. After 3 months.
- Were you involved in the decision on where she has antenatal care?
- Yes B .No
- Did you ever accompany your partner to the ANC clinic
- Yes B. No If yes
- How many times did you accompany her to the ANC clinic
- Once B. two or more C. None