Klebsiella Pneumoniae Urinary Tract Infection Seen in the Laboratory of the University Hospital of Befelatanana
Article Information
Lalaina Mamenosoa Rakotondraoelina1, Zafindrasoa Domoina Rakotovao-Ravahatra2, Solofo Sarah Rafaramalala3, Andriamiadana Luc Rakotovao4, Andry Rasamindrakotroka5
1Biologist doctor, Laboratory of Anosiala University Hospital Antananarivo, Madagascar
2Biologist doctor, Laboratory of Joseph Raseta Befelatanana University Hospital Antananarivo, Madagascar
3Biologist doctor, Malagasy Medical Analysis Laboratory Androhibe Antananarivo, Madagascar
4Professor in biological hematology, Medical Biology Department of the Faculty of Medicine, University of Antananarivo, Madagascar
5Professor in immunology, Medical Biology Department of the Faculty of Medicine, University of Antananarivo, Madagascar
*Corresponding author: Zafindrasoa Domoina Rakotovao-Ravahatra, Biologist doctor, Laboratory of Joseph Raseta Befelatanana University Hospital Antananarivo, Madagascar.
Received: 09 December 2022; Accepted: 15 December 2022; Published: 24 December 2022
Citation: Zafindrasoa Domoina Rakotovao- Ravahatra, Solofo Sarah Rafaramalala, Lalaina Mamenosoa Rakotondraoelina, Andriamiadana Luc Rakotovao, Andry Rasamindrakotroka. Klebsiella pneumoniae urinary tract infection seen in the laboratory of the University Hospital of Befelatanana. Archives of Microbiology and Immunology 6 (2022): 284-288.
View / Download Pdf Share at FacebookAbstract
Background: Klebsiella pneumoniae (K. pneumoniae) urinary tract infections (UTIs) are common in the community and in hospital. The aims of this study were to evaluate antibiotic resistance and to describe the factors associated with urinary tract infections caused by K. pneumoniae.
Methods: This is a descriptive and cross-sectional study of 524 results of cytobacteriological examinations of urine (CBEU) of pus over a period of 8 months, from January 2022 to August 2022, at the laboratory of the University Hospital of Befelatanana.
Results: Among the 524 CBEU, 157 cases were positive showing a hospital prevalence of 30% of UTI. Among the germs identified, 18 cases (3.4%) were represented by isolates of K. pneumoniae. Regarding the associated factors, subjects aged 60 and over (5.7%) (p=0.20; NS), men (11%)(p=0.07), patients with urinary disorders (13%)(p=0.001) and hospitalized in Internal Medicine departments (9%) (p=0.44; NS) were the most affected by K. pneumoniae UTI. Concerning the results of the antibiograms, the resistances of the isolates of K. pneumoniae varied from 5.6% (amikacin) to 100% (amoxicillin).
Conclusion: Systematic CBEU should be performed in vulnerable hospitalized patients with urinary signs to ensure rapid and effective management of K. pneumoniae UTI. Similarly, hygiene measures must be improved in hospitals in order to reduce the occurrence of nosocomial UTI due to multi-resistant K. pneumoniae.
Keywords
antibiotic resistance, infection, Klebsiella pneumoniae, urine
antibiotic resistance articles, infection articles, Klebsiella pneumoniae articles, urine articles
Article Details
1. Introduction
pneumoniae is a relatively common component of the normal microbiota, having the capacity to colonize various tissues and anatomical structures (e.g., distal urethra, upper respiratory tract, or the gastrointestinal tract). It is considered an opportunistic pathogen, being incriminated in the etiology of severe infections in hospitalized patients, especially in those immunocompromised or who present severe comorbidities [1-2]. The incidence of UTIs caused by K. pneumoniaehas exhibited an increasing trend and has become a high burden for many public health systems, especially in hospital settings [3]. Multidrug resistance associated with the production of extended-spectrum β-lactamases (ESBL) among K. pneumoniaeisolates is common in hospital settings. The emergence of multi-resistant strains reduces the number of effective antibiotics for treating UTIs caused by K. pneumoniae. Many studies should be done about this infection in order to improve the management of patients in hospitals. Thus, the aims of this study were to evaluate antibiotic resistance and to describe the factors associated with UTIs caused by K. pneumoniae.
2. Materials and Methods
2.1 Study design
This is a descriptive and cross-sectional study of 524 results of CBEU of pus over a period of 8 months, from January 2022 to August 2022, at the laboratory of the University Hospital Center Joseph Raseta Befelatanana (CHUJRB) in Antananarivo, Madagascar.
2.2 Study setting
This study was carried out in the laboratory of the CHUJRB which is located in Antananarivo city in the Analamanga, region in Madagascar. This laboratory is a general-purpose medical analysis laboratory open 24 hours a day, 7 days a week. This laboratory receives biological samples from patients hospitalized in Antananarivo hospitals or outpatients. The biological analyzes carried out in this laboratory are represented by hematological, biochemical, immunological, virological, parasitological and bacteriological analyses.
2.3 Participants
The study population was represented by all bacteria identified by the CBEU. All CBEU results with complete records and valid results were included in the study. All CBEU results with incomplete records and invalid results were not included in the study. All CBEU results from other research were excluded from the study.
2.4 Variables
The dependent variable was represented by the positivity of the CBEU showing K. pneumoniae. The independent variables were represented by the age, the gender, the clinical information, the departments and the results of antibiogram.
2.5 Procedures in laboratory
In the laboratory, the urinary samples were cultured in ordinary agar called Uriselect® and incubated in the oven at 37 ° C for 24 hours. After the culture, cytological examination was performed with a kova slide (brand Glassitic® Slide 10 with Grids) to count the leukocytes, erythrocytes, epithelial cells, yeast, crystals, casts parasites…Afterwards, a microscope examination is performed after gram staining to identify bacteria and other microorganisms (yeast, parasite…). After 24 hours, the positivity criteria UTI are the presence of a single type or two types of bacterial colonies ≥ 105 CFUs (colony-forming units) per mL and the number of leukocytes ≥ 104/mL [4]. Then, the bacterial colonies are identified by the various bacterial identification tests available in the laboratory. Finally, the antibiogram corresponding to the identified bacterial species is carried out.
Resistance to antibiotics was determined by the Mueller / Hinton agar diffusion method, according to the recommendations of the “comité de l'antibiogramme de la société française de Microbiologie” (Société Française de Microbiologie, 2019) [5]. For K. pneumoniae isoaltes, the antibiotics tested are represented by penicillins (penicillin G, amoxicillin, ticarcillin), amoxicillin-clavulanic Acid (AMC), 3rd generation cephalosporins (3CG)(ceftazidime, cefotaxime, cefixime), penemes (imipenem), aminoglycosides (gentamycin, tobramycin, amikacin), quinolones (nalidixic acid, ciprofloxacin, levofloxacin), macrolides (erythromycin), lincosamides (lincomycin), cyclins (tetracyclin) , sulfonamides (trimethoprim- sulfamethoxazole : cotrimoxazole) and amphicoles (chloramphenicol).
2.6 Data collection
Data were collected from CBEU request forms, bench forms, register notebooks, antibiogram forms and word files containing patient CBEU results.
2.7 Data analysis
The entry and processing of data were performed on Epi-info 3.5.2 software. Proportions are presented as numbers (percent) and were compared using the chi-square test. Results were considered significant if p was 0.05 or less, with a 95% confidence interval.
2.8 Ethical considerations
The authorization of this study by an ethics committee was not necessary because we analyzed isolates of bacteria. Nevertheless, the authorization of the director of the establishment was obtained before the data were collected in the registers. Likewise, the seizure was done anonymously to maintain confidentiality.
3. Results
3.1 Hospital prevalence of UTIs
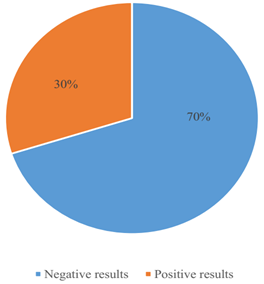
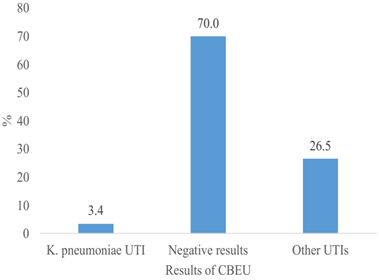
Among the 524 CBEU, 157 cases were positive showing a hospital prevalence of 30% of UTI (figure 1). Among the germs identified, 18 cases (3.4%) were represented by isolates of K. pneumoniae (figure 2).
3.2 Factors associated with K. pneumoniae UTI
Regarding the associated factors, subjects aged 60 and over (5.7%) (p=0.20; NS), men (11%)(p=0.07), patients with urinary disorders (13%)(p=0.001) and hospitalized in Internal Medicine departments (9%) (p=0.44; NS) were the most affected by K. pneumoniae UTI (table 1).
Table 1: Factors associated with K. pneumoniae UTI
|
Associated factors |
K. pneumoniae UTI (N=18) |
Negative results or other UTIs (N=506) |
Total (N=524) |
p-value |
||
|
n |
% |
n |
% |
|||
|
Age (years) |
||||||
|
<20 |
3 |
3.6 |
81 |
96.4 |
84 |
0.2 (NS) |
|
20-39 |
2 |
1.4 |
146 |
98.6 |
148 |
|
|
40-50 |
4 |
3 |
131 |
97 |
135 |
|
|
≥60 |
9 |
5.7 |
148 |
94.3 |
157 |
|
|
Gender |
||||||
|
Female |
7 |
2.3 |
303 |
97.7 |
310 |
0.07 (NS) |
|
Male |
11 |
5.1 |
203 |
94.9 |
214 |
|
|
Departments |
||||||
|
Surgery |
1 |
12.5 |
7 |
87.5 |
8 |
0.44 (NS) |
|
Out-patients |
6 |
3.1 |
188 |
96.9 |
194 |
|
|
Gynecology |
0 |
56 |
100 |
56 |
||
|
Infectious diseases |
1 |
4 |
24 |
96 |
25 |
|
|
Internal Medicine |
9 |
4 |
217 |
96 |
226 |
|
|
Intensive Care Unit |
1 |
6.7 |
14 |
93.3 |
15 |
|
|
Clinical information |
||||||
|
Others |
0 |
0 |
189 |
100 |
189 |
0.001 |
|
Fever |
5 |
3.6 |
133 |
96.4 |
138 |
|
|
Urinary disorders |
13 |
6.6 |
184 |
93.4 |
197 |
|
3.3. Antibiotic resistance of K. pneumoniae responsible for UTI
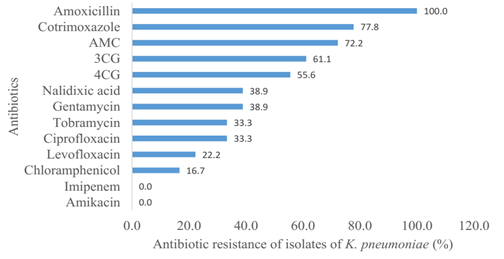
Concerning the results of the antibiograms, the resistances of the isolates of K. pneumoniae varied from 5.6% (amikacin) to 100% (amoxicillin) (figure 3). And 55.6% of cases were represented by ESBL-K. pneumonia (ESBL-Kp).
4. Discussion
4.1 Hospital prevalence of UTIs
This study was showed a hospital prevalence of 30% of UTI. This prevalence is high because the CBEUs carried out in the CHUJRB laboratory come from both outpatients and patients hospitalized at the CHUJRB and in the other hospitals of Antananarivo. According by literature, Healthcare-associated UTI (HAUTI) frequency is 12.9, 19.6 and 24% in the United States, Europe and developing countries, respectively [6]. Among the germs identified, 3.4% of cases were represented by isolates of K. pneumoniae. Even if this rate is low, it must be taken into account because these isolates of K. pneumoniae are often multi-resistant bacteria responsible for the difficulty of management. According to a study carried out in the Moulay Ismail of Meknès, K. pneumoniae is the major ESBL producer (25.8%) within the same species responsible for UTIs [7].
4.2 Factors associated with K. pneumoniae UTI
In this study, subjects aged 60 and over were the most affected by K.pneumoniae UTI without significant difference. However, according to the literature, UTI is a significant but common problem in elderly population. Physicians who care for frail elderly patients must be aware of the challenges in the management of asymptomatic UTI, and identifying symptomatic UTI in this population, and their appropriate management strategies. There is strong need in studies to evaluate non-antimicrobial therapies in the prevention of UTI for the frail elderly population [8]. According to gender, men were the most affected by K.pneumoniae UTI but no significant difference. Other studies showed that women are more affected by UTIs than men [9-10]. Indeed, UTI is one of the most common infections afflicting women. UTI often accompanies vaginal infections and is frequently caused by pathogens originating in the digestive tract like K.pneumoniae. In the United States, 40% of women will develop a UTI during their lifetime, making it one of the most common infections in women [11]. The frequency of UTIs in women could be due to female urinary tract anatomy and female physiological changes such as pregnancy, menstruation, and menopause.
According to the departments, patients hospitalized in Internal Medicine departments were the most affected by K. pneumoniae UTI without significant difference. Thus, K. pneumoniae UTI can affect all patients in all hospital departments. In these departments, there are factors favoring UTI such as urinary catheters, prolonged bed rest and long hospital stay. According to the clinical information, patients with urinary disorders were the most affected by K. pneumoniae UTI with significant difference. Thus, a patient with urinary signs must do an emergency CBEU in order to quickly initiate treatment to avoid complications.
4.3 Antibiotic resistance of K. pneumoniae responsible for UTI
Concerning the antibiotic resistance, 100% of isolates of Staphylococcus aureus were resistant to amoxicillin. Indeed, in Madagascar, the population consumes this class of antibiotics excessively without a medical prescription. This drug is sold in small grocery stores and the population can buy them easily. The literature confirms that the self-medication practiced by the population favors the increase in the resistance of germs to antibiotics [12]. Furthermore, more than half of the isolates were ESBL-Kp. These isolates are resistant to all beta-lactams (penicillins, cephalosporins) except penems (imipenem). The strains of ESBL-Kp responsible for UTI continue to increase all over the world. A study showed that The prevalence of ESBL-Kp UTI increased from 2.4% in 2010 to 10.3% in 2014 (P = 0.01) [13]. In Madagascar, doctors in Basic Health Centers tend to give cephalosporins for empirical treatments when the patient does not have enough money for bacteriological analyses. These treatments lead to excessive and inappropriate use of antibiotics. The literature confirms that the selection pressure of germs linked to their frequent exposure to a class of antibiotic promotes their genetic mutation leading to the emergence of new multi-resistant strains [14].
In this study, quinolones (nalidixic acid, ciprofloxacin, levofloxacin), aminoglycosides (gentamysin) and amphicoles (chloramphenicol) start to become equally ineffective. To avoid the misuse of these classes of antibiotics by empirical treatments, it is important to always perform a CBEU with antibiogram before initiating antibiotic treatment. The results of the antibiograms make it possible to choose the antibiotics effective against the germs.
In this study, no resistance to imipenem and amikacin was observed. Another study also showed that imipenem and amikacin are very effective showing 99.3% and 93.8% sensitivity respectively [15]. Thus, these 2 drugs represent the treatment of choice for multi-resistant K.peumoniae UTIs. The use of these 2 drugs in hospitals must be well controlled and limited as much as possible to preserve their effectiveness and limit the emergence of new strains of multi-resistant K.pneumoniae.
5. Conclusion
This study showed that K. pneumonia UTI is common in hospitals. Hospital hygiene measures are very important in hospital departments to fight against nosocomial infections. Similarly, it is necessary to limit the use of broad-spectrum antibiotics in hospital departments to control the evolution of K. pneumoniae isolates towards increasing antibiotic resistance. In brief, cytobacteriological examination of urines and antibiogram were very important to improve the management of patients with UTI.
Acknowledgements
We extend our sincere thanks to the director of the CHUJRB establishment, to the head of the CHUJRB laboratory department and to the laboratory technicians who participated in the realization of this study.
Conflicts of interest
The authors do not declare any conflict of interest.
References
- Shimasaki T, Seekatz A, Bassis C, Rhee Y, Yelin RD, et al. Increased relative abundance of Klebsiella pneumoniaecarbapenemase-producing Klebsiella pneumoniae within the gut microbiota is associated with risk of bloodstream infection in long-term acute care hospital patients. Clinical Infectious Diseases 68 (2019): 2053–2059.
- Navon-Venezia S, Kondratyeva K, Carattoli A. Klebsiella pneumoniae: A major worldwide source and shuttle for antibiotic resistance. FEMS Microbiology Review 41 (2017): 252–275.
- Miftode IL, Nastase EV, Miftode RS, Miftode EG, Iancu LS, et al. Insights into multidrug-resistant pneumoniaeurinary tract infections: From susceptibility to mortality. Experimental and Therapeutic Medicine. 22 (2021): 1086.
- Aziz SEl, Haraj N, Hassoune S , Obbiba A , Chadli A, et al . Prevalence and urinary tract infections risk factors at theCasablanca University Hospital, Morocco. Médecine des Maladies Métaboliques 8 (2014) : 204-210.
- Société Française de Microbiologie. Tables of critical concentrations for the interpretation of MICs and critical diameters ofinhibition zones. In : CASFM / EUCAST : Société Française de Microbiologie Ed (2019): 38-44.
- Tandogdu Z, Wagenlehner FM. Global epidemiology of urinary tract infections. Current Opinion in Infectious Diseases 29 (2016): 73-79.
- Sbiti M, Lahmadi K, Louzi L. Profil épidémiologique des entérobactéries uropathogènes productrices de bêta-lactamases à spectre élargi [Epidemiological profile of uropathogenic enterobacteria producing extended spectrum beta-lactamases]. The Pan African Medical Journal 13 (2017): 29.
- Zeng G, Zhu W, Lam W, Bayramgil A. Treatment of urinary tract infections in the old and fragile. World Journal of Urology 38 (2020): 2709-2720.
- Czajkowski K, Bros-Konopielko M, Teliga-Czajkowska J. Urinary tract infection in women. Przeglad Menopauzalny. 20 (2021): 40-47.
- Mody L, Juthani-Mehta M. Urinary tract infections in older women: a clinical review. JAMA 311 (2014): 844-854.
- Bono MJ, Leslie SW, Reygaert WC. Urinary Tract Infection. 2022 Jun 15. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing (2022).
- Randriatsarafara FM, Ralamboson J, Rakotoarivelo R, Raherinandrasana A, Andrianasolo R. Antibiotic consumption at Antananarivo University Hospital: prevalence and strategic challenges. Santé Publique 27 (2015): 249- 255.
- Boix-Palop L, Xercavins M, Badía C, Obradors M, Riera M, et al. Emerging extended-spectrum β-lactamase-producing Klebsiella pneumoniae causing community-onset urinary tract infections: a case-control-control study. International Journal of Antimicrobial Agents 50 (2017): 197-202.
- Tello A, Austin B, Telfer TC. Selective pressure of antibiotic pollution on bacteria of importance to public health. Environnemental Health Perspectives 120 (2012): 1100-1106
- Fils PEL, Cholley P, Gbaguidi-Haore H, Hocquet D, Sauget M, Bertrand X. ESBL-producing Klebsiella pneumoniae in a University hospital: Molecular features, diffusion of epidemic clones and evaluation of cross-transmission. PLoS One 16 (2021): e0247875.