Kikuchi-Fujimoto Disease: A Case Report on a Master Mimicker
Article Information
Kikuchi-Fujimoto Disease: A Case Report on a Master Mimicker
Dr. Pankaj M Buch1, Dr. Mauli D Kansagra2*, Dr. Manali M Patel3
1Professor and Head of Department of Paediatrics, PDU Government Medical College, Rajkot, Gujarat, India
2Assistant Professor of Paediatrics, PDU Government Medical College, Rajkot, Gujarat, India
3Third year resident of Paediatrics, PDU Government Medical College, Rajkot, Gujarat, India
*Corresponding Authors: Dr. Mauli D Kansagra, Assistant Professor of Paediatrics, PDU Government Medical College, Rajkot, Gujarat, India.
Received: 28 July 2025; Accepted: 05 August 2025; Published: 11 August 2025
Citation: Dr. Pankaj M Buch, Dr. Mauli D Kansagra, Dr. Manali M Patel. Kikuchi-Fujimoto Disease: A Case Report on a Master Mimicker. Journal of Pediatrics, Perinatology and Child Health. 9 (2025): 137-139.
View / Download Pdf Share at FacebookAbstract
Any patient presenting with fever, lymphadenopathy and weight loss requires immediate attention and investigation. We often think of common causes like tuberculosis, lymphoma and other infective and autoimmune causes. Here, we present a case which mimics these life-threatening conditions but is actually self-limiting.
Keywords
Fever; Necrotizing lymphadenopathy; Kikuchi-Fujimoto Disease; Weight loss; Life-threatening
Article Details
1. Introduction
Of the numerous cases that we come across in the pediatric OPD, the one of fever with lymphadenopathy certainly raises a red flag and warrants immediate attention and investigation. We immediately think of the common causes like tuberculosis, lymphoma, other acute infective and autoimmune disorders. There is one condition which mimics the above mentioned diseases with its symptoms, but actually tends to be self-limiting. We present you with one such atypical case.
2. Case Report
A 7-year-old male patient presented to our tertiary care hospital with complain of fever, malaise, weight loss since 20 days with swelling and pain on left side of neck. On examination multiple bilateral cervical lymph nodes were palpable with tenderness. On ultrasound, multiple lymph nodes were enlarged at level 2a, 3, 4, and 5, largest measuring 15 mm with preserved fatty hilum. There was no local erythema or warmth, no hepatosplenomegaly, no bone pain and no other positive findings on systemic examination. He had no past history of tuberculosis or tuberculosis contact and was immunized till age [1,2]. As there was no improvement after oral antibiotics we admitted the patient, sent the primary investigations and started higher injectable antibiotics.
On blood investigations, serial blood counts, renal and liver function tests were within normal limits with no cytopenia. ESR was 22 on admission which increased to 95 after 3 weeks. Peripheral smear was normal. HIV ELISA was negative. CT scan of neck was done to rule out retropharyngeal abscess which was normal. FNAC was suggestive of reactive lymphadenitis. CBNAAT of gastric aspirate for tuberculosis was negative and so was brucella IgM. Chest radiograph and echocardiography was normal.
Meanwhile, our patient was having increasing intensity and frequency of fever spikes, progressing to continuous high grade fever despite being on higher antibiotics along with decrease oral intake in interfebrile period and significant weight loss after 3 weeks. His lymphadenopathy progressed from bilateral cervical to bilateral axillary and inguinal region but there was no significant change in serial blood counts and no hepatosplenomegaly. So excision biopsy was done from one of the axillary nodes and sent for histopathology. After 45 days of fever and 25 days of admission, intensity and frequency of fever started decreasing and oral intake started improving.
Finally, excision biopsy report came and was suggestive of necrosis with karyorrhexis along with histiocytic infiltrates, suggestive of Kikuchi fujimoto disease or necrotizing lymphadenitis. Autoimmune workup was done to rule out systemic lupus erythematosus, a common association, which was negative. By this time our patient’s symptoms had resolved spontaneously so steroids were not started. We have kept the patient on a close follow-up. After 2 weeks lymphadenopathy was gradually decreasing in size and he was afebrile.
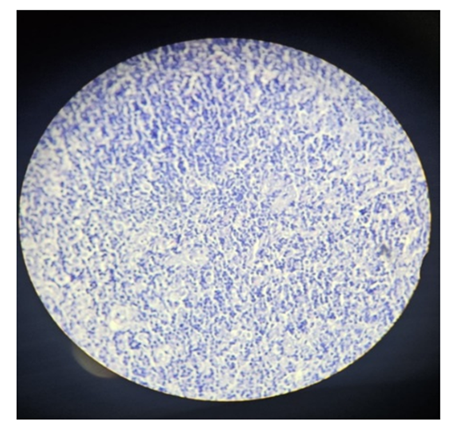
Kikuchi fujimoto disease, also described as Histiocytic necrotizing lymphadenitis is a rare, benign, self-limiting inflammatory condition characterized by fever, cervical or generalized lymphadenopathy and necrotizing lymphadenitis [3]. The etiology is unknown although viral and bacterial infections, environmental factors and autoimmune disease such as SLE have been associated [1]. Disease primarily affects young and pediatric patients of 8 to 16 years of Asia [1]. Clinical presentation is varied with acute or subacute in onset [2]. It can present as unilateral posterior cervical adenitis, fever, malaise, weight loss, like in the current case [1]. Blood picture shows raised ESR, leucopenia and atypical lymphocytosis [1]. Triad of disease includes fever, lymphadenopathy and night sweats which resembles TB and lymphoma [3]. Lymph node size can be from 0.5 to 6cm, painful, tender, mobile, may be multiple involve axillary and supraclavicular lymph nodes [1]. Skin involvement can also be seen in form of diverse non-specific erythematous rashes [2]. Diagnosis made by excision lymph node biopsy [1]. Histologic features include necrosis with karyorrhexis, a histiocytic infiltrate and plasma cytoid dendritic cells [1]. It shows CD123 and TCL1 nuclear reactivity with neutropenia and lymphocytosis [1]. Immunohistochemistry is crucial in confirming diagnosis and exclude other differential causes [2]. It shows positive staining for myeloperoxidase, lysozyme, CD68, CD163 and CD4 [2]. Autoimmune workup to be done to evaluate SLE as it is most common differential diagnosis and associated condition [2,4] (Figure 1).
Figure 1: Histopathological examination of excision biopsy of axillary lymph node, showing necrotizing lymphadenitis.
|
Tuberculosis |
Lymphoma |
Kikuchi Fujimoto Disease |
|
|
Complete blood count |
Normal, DC: lymphocytosis (Neutrophilia in case of severe miliary TB) Anemia of chronic disease may present |
Peripheral lymphocytosis or, eosinophilia, anemia of chronic disease, thrombocytopenia if bone marrow involves |
Leucopenia with atypical lymphocytosis |
|
Erythrocyte sedimentation rate |
Raised |
Can be Raised |
Raised |
|
Histopathology |
Granulomatous inflammation: LANGHANS GIANT CELLS, epithelioid cell clusters Caseous necrosis AFB detected by ZN stain |
Hodgkin’s Lymphoma: REED STERNBERG CELLS Non-Hodgkin’s Lymphoma: Monomorphic abnormal lymphocytes |
Necrosis with karyorrhexis, histiocytic infiltrates and plasma cytoid dendritic cells |
Table 1: Comparison of laboratory and histopathological characteristics of tuberculosis, lymphoma and kikuchi fujimoto disease.
In conclusion, it can be rightly said that fever with lymphadenopathy and weight loss does not always mean tuberculosis or malignancy and one needs to always confirm the diagnosis with excision biopsy rather than fine needle aspiration cytology.
Ethics Approval: Not applicable.
Funding: No funding was required.
Competing Interests: Not applicable.
Data Availability Statement: Not applicable.
Clinical Trial Number: Not applicable.
References
- 517. In: Nelson Textbook of Paediatrics. 21st ed. (2019): pp: 2626-2626.
- Masab M, Surmachevska N, Farooq H. Kikuchi-Fujimoto Disease. [Updated 2023 Oct 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430830/
- Joshi S, Bhatia A, Tayal N, et al. Necrotizing lymphadenitis: Not always tuberculosis, its Kikuchi-Fujimoto’s disease. Indian Journal of Tuberculosis 67 (2020): 383-385.
- Kikuchi-Fujimoto disease. National Organization for Rare Disorders. Available at: https://rarediseases.org/ (Accessed: 20 July 2025).