Is There Relationship Between Thyroid Volume, Hyperparathyroidism and Cardiovascular Risk Factors in Patients Under Hemodialysis?
Article Information
Ali Gürel1, Emin Murat Akba?2, Hünkar Aggül3, Kür?at Kaya4
1Nephrology Department, Medical Faculty, F?rat University, Elaz?g, Turkey
2Endocrinology Department, Medical Faculty, Erzincan Binali Y?ld?r?m University, Erzincan, Turkey
3Intensive Care Department, Medical Faculty, Nam?k Kemal University, Tekirdag, Turkey
4Biochemistry Department, Pharmacy Faculty, Ad?yaman University, Ad?yaman, Turkey
*Corresponding Author: Ali Gürel, Nephrology Department, Medical Faculty, F?rat University, Elaz?g, Turkey
Received: 06 May 2020; Accepted: 18 May 2020; Published: 02 June 2020
Citation: Ali Gürel, Emin Murat Akbaş, Hünkar Ağgül, Kürşat Kaya. Is There Relationship Between Thyroid Volume, Hyperparathyroidism and Cardiovascular Risk Factors in Patients Under Hemodialysis?. Archives of Nephrology and Urology 3 (2020): 017-026.
View / Download Pdf Share at FacebookAbstract
Background: Thyroid dysfunction and hyperparathyroidism are common in with chronic kidney disease (CKD) and under dialysis. It is known that they increase the risk of cardiovascular (CV) diseases in this population.
Objectives: In this study, we aimed to investigate the relationship between thyroid volume, hyperparathyroidism (HPTH), atherogenic index of plasma (AIP), carotis intima-media thickness (CIMT) and uric acid (UA) in hemodialysis (HD) patients.
Methodology: Hemodialysis patients without thyroid dysfunction were divided into three groups as; low (<13.6 pg/mL), target (13.6-61.2 pg/mL) and high (> 61.2 pg/mL) parathyroid hormone (PTH) levels continuing for at least 6 months. Routine laboratory tests, PTH, lipid profile, high sensitive CRP (hs-CRP), TSH, T4, T3, glucose, UA, insulin, C-peptide, AIP, thyroid ultrasonography performed and CIMT were evaluated and recorded.
Results: Total thyroid volume was 21.64 ± 1.83, 15.01 ± 1.60, 19.52 ± 1.41 mL respectively in males, females and whole group. Total thyroid volume, AIP, hs-CRP, UA, bilateral CIMT were all lower in low PTH group in comparison with other groups, but statistically significant only for hs-CRP levels. There was positive correlation between total thyroid volume and bilateral CIMT, hs-CRP; and negative correlation between Kt/V and thyroid volume. Conclusion: In HD patients; thyroid volume may be an indicator of CV risk in harmony with other risk factors.
Keywords
Thyroid volume; Hyperparathyroidism; Uric acid; atherogenic index of plasma; Carotis intima-media thickness; Hemodialysis
Thyroid volume Articles, Hyperparathyroidism Articles, Uric acid Articles, atherogenic index of plasma Articles, Carotis intima-media thickness Articles, Hemodialysis Articles
Thyroid volume articles Thyroid volume Research articles Thyroid volume review articles Thyroid volume PubMed articles Thyroid volume PubMed Central articles Thyroid volume 2023 articles Thyroid volume 2024 articles Thyroid volume Scopus articles Thyroid volume impact factor journals Thyroid volume Scopus journals Thyroid volume PubMed journals Thyroid volume medical journals Thyroid volume free journals Thyroid volume best journals Thyroid volume top journals Thyroid volume free medical journals Thyroid volume famous journals Thyroid volume Google Scholar indexed journals Hyperparathyroidism articles Hyperparathyroidism Research articles Hyperparathyroidism review articles Hyperparathyroidism PubMed articles Hyperparathyroidism PubMed Central articles Hyperparathyroidism 2023 articles Hyperparathyroidism 2024 articles Hyperparathyroidism Scopus articles Hyperparathyroidism impact factor journals Hyperparathyroidism Scopus journals Hyperparathyroidism PubMed journals Hyperparathyroidism medical journals Hyperparathyroidism free journals Hyperparathyroidism best journals Hyperparathyroidism top journals Hyperparathyroidism free medical journals Hyperparathyroidism famous journals Hyperparathyroidism Google Scholar indexed journals Uric acid articles Uric acid Research articles Uric acid review articles Uric acid PubMed articles Uric acid PubMed Central articles Uric acid 2023 articles Uric acid 2024 articles Uric acid Scopus articles Uric acid impact factor journals Uric acid Scopus journals Uric acid PubMed journals Uric acid medical journals Uric acid free journals Uric acid best journals Uric acid top journals Uric acid free medical journals Uric acid famous journals Uric acid Google Scholar indexed journals atherogenic index of plasma articles atherogenic index of plasma Research articles atherogenic index of plasma review articles atherogenic index of plasma PubMed articles atherogenic index of plasma PubMed Central articles atherogenic index of plasma 2023 articles atherogenic index of plasma 2024 articles atherogenic index of plasma Scopus articles atherogenic index of plasma impact factor journals atherogenic index of plasma Scopus journals atherogenic index of plasma PubMed journals atherogenic index of plasma medical journals atherogenic index of plasma free journals atherogenic index of plasma best journals atherogenic index of plasma top journals atherogenic index of plasma free medical journals atherogenic index of plasma famous journals atherogenic index of plasma Google Scholar indexed journals Hemodialysis articles Hemodialysis Research articles Hemodialysis review articles Hemodialysis PubMed articles Hemodialysis PubMed Central articles Hemodialysis 2023 articles Hemodialysis 2024 articles Hemodialysis Scopus articles Hemodialysis impact factor journals Hemodialysis Scopus journals Hemodialysis PubMed journals Hemodialysis medical journals Hemodialysis free journals Hemodialysis best journals Hemodialysis top journals Hemodialysis free medical journals Hemodialysis famous journals Hemodialysis Google Scholar indexed journals Carotis intima-media thickness articles Carotis intima-media thickness Research articles Carotis intima-media thickness review articles Carotis intima-media thickness PubMed articles Carotis intima-media thickness PubMed Central articles Carotis intima-media thickness 2023 articles Carotis intima-media thickness 2024 articles Carotis intima-media thickness Scopus articles Carotis intima-media thickness impact factor journals Carotis intima-media thickness Scopus journals Carotis intima-media thickness PubMed journals Carotis intima-media thickness medical journals Carotis intima-media thickness free journals Carotis intima-media thickness best journals Carotis intima-media thickness top journals Carotis intima-media thickness free medical journals Carotis intima-media thickness famous journals Carotis intima-media thickness Google Scholar indexed journals chronic kidney disease articles chronic kidney disease Research articles chronic kidney disease review articles chronic kidney disease PubMed articles chronic kidney disease PubMed Central articles chronic kidney disease 2023 articles chronic kidney disease 2024 articles chronic kidney disease Scopus articles chronic kidney disease impact factor journals chronic kidney disease Scopus journals chronic kidney disease PubMed journals chronic kidney disease medical journals chronic kidney disease free journals chronic kidney disease best journals chronic kidney disease top journals chronic kidney disease free medical journals chronic kidney disease famous journals chronic kidney disease Google Scholar indexed journals hyperparathyroidism articles hyperparathyroidism Research articles hyperparathyroidism review articles hyperparathyroidism PubMed articles hyperparathyroidism PubMed Central articles hyperparathyroidism 2023 articles hyperparathyroidism 2024 articles hyperparathyroidism Scopus articles hyperparathyroidism impact factor journals hyperparathyroidism Scopus journals hyperparathyroidism PubMed journals hyperparathyroidism medical journals hyperparathyroidism free journals hyperparathyroidism best journals hyperparathyroidism top journals hyperparathyroidism free medical journals hyperparathyroidism famous journals hyperparathyroidism Google Scholar indexed journals end-stage renal disease articles end-stage renal disease Research articles end-stage renal disease review articles end-stage renal disease PubMed articles end-stage renal disease PubMed Central articles end-stage renal disease 2023 articles end-stage renal disease 2024 articles end-stage renal disease Scopus articles end-stage renal disease impact factor journals end-stage renal disease Scopus journals end-stage renal disease PubMed journals end-stage renal disease medical journals end-stage renal disease free journals end-stage renal disease best journals end-stage renal disease top journals end-stage renal disease free medical journals end-stage renal disease famous journals end-stage renal disease Google Scholar indexed journals glomerular filtration rate articles glomerular filtration rate Research articles glomerular filtration rate review articles glomerular filtration rate PubMed articles glomerular filtration rate PubMed Central articles glomerular filtration rate 2023 articles glomerular filtration rate 2024 articles glomerular filtration rate Scopus articles glomerular filtration rate impact factor journals glomerular filtration rate Scopus journals glomerular filtration rate PubMed journals glomerular filtration rate medical journals glomerular filtration rate free journals glomerular filtration rate best journals glomerular filtration rate top journals glomerular filtration rate free medical journals glomerular filtration rate famous journals glomerular filtration rate Google Scholar indexed journals
Article Details
Introduction
Chronic kidney disease (CKD) is a worldwide public health problem with poor results and increasing incidence. It progresses with reduced glomerular filtration rate (GFR) and affects 10-20% of adults worldwide [1]. In patients with end-stage renal disease (ESRD), as renal replacement therapy (RRT) modalities; kidney transplantation, hemodialysis (HD) and peritoneal dialysis (PD) are among the current options [2]. Thyroid dysfunction is common in patients with CKD and under RRT [3]. While low free T3 hormone levels were associated with arterial stiffness in PD patients, high TSH levels near the upper limit of normal range were found to be associated with low subendocardial viability rate (arterial stiffness indicator) in euthyroid PD patients [4]. A positive correlation was observed between thyroid volume and creatinine levels in kidney transplant cases [5]. In recent years, factors such as uric acid (UA), hypoalbuminemia, insulin resistance, dyslipidemia, inflammation, oxidative stress and hyperparathyroidism (HPTH) have been frequently used and used as risk factors for the development of cardiovascular diseases (CVD) in patients with ESRD [6]. It is known that secondary HPTH, the most common cause of which is CKD, causes fractures, decreased quality of life and increased risk of CVD [7].
In this study, it was aimed to investigate the relationship between thyroid gland volume, HPTH and atherogenic index of plasma (AIP) and carotis intima-media thickness (CIMT) in the patient population undergoing RRT, and to evaluate the relation between these parameters, each of which is an independent cardiovascular (CV) risk factor.
2. Methodology
This single-center, prospective study was carried out with the approval of the local ethics committee (Erzincan University Ethics Committee; 07-04-2015/ 64593235-050.01.04-E.14331) and informed consent from the participants. The study included 50 ESRD patients without thyroid dysfunction who were followed by our clinic and under HD treatment. Informed consent forms were signed, thyroid volumes and carotis intima media thicknesses of the patients were measured by ultrasound. Biochemical parameters of patients included in the study for the last 6 months were obtained from medical records. Patients under HD treatment due to ESRD divided into three groups as; low (<13.6 pg/mL), target (13.6-61.2 pg/mL) and high (> 61.2 pg/mL) PTH levels. Patients were also evaluated according to low uric acid and high uric acid levels and low Kt/V and high Kt/V ratios. In addition to the routine laboratory examinations of the patients in the study, laboratory parameters such as parathyroid hormone (PTH), lipid profile, high sensitive CRP, TSH, T4, T3, glucose, UA, insulin, C-peptide, and AIP and also thyroid ultrasonography performed simultaneously by the same Endocrinologist and carotid intima media thickness, which is an indicator of atherosclerosis, was evaluated and recorded.
2.1 Statistic analysis
The data was analyzed using SPSS for Windows version 13. All values were presented as mean+ standard error mean (SEM).Normality for continued variables in groups were determined by the Kolmogorov-Smirnov test. The variance homogeneity of the values showing normal distribution was tested by Levene’s test.The variables that showed normal distribution and equal variance, were analyzed by Independent-Samples T test andOne-Way ANOVA (Scheffe, LSD or Tukey test). The variables that showed normal distribution and unequal variances were analyzed by One-Way ANOVA; Tamhane’s T2.The variables that didn’t show normal distribution were analyzed by Kruskal-Wallis test and Mann–Whitney U-test (The Bonferroni correction was applied).
3. Results
In our study group; mean age of males and females were 58.94 ± 2.84 and 57.5 ± 4.43 respectively (Table 1). Total thyroid volume was 21.64 ± 1.83 mL in males, 15.01 ± 1.60 mL in females and overall thyroid volume was 19.52 ± 1.41 mL (Table 2). When groups were seperated as low (< 13.6 pg/mL), target (13.6-61.2 pg/mL) and high (> 61.2 pg/mL) PTH levels continuing for at least 6 months; total thyroid volume, AIP, hs-CRP, uric acid, bilateral CIMT were all lower in low PTH group in comparison with other groups, but statistically significant only for hs-CRP levels (Table 3). When groups were separated as low (<7 mg/dL) and high (> 7 mg/dL) UA levels continuing for at least 3 months; hs-CRP levels were also high in low UA group, however without stastical significance (Table 4). When groups were seperated as low (<1.2) and high (> 1.2) Kt/V levels for at least 1 year; total thyroid volume (p<0.001), bilateral CIMT (p<0.001) and total cholesterol levels (p=0.002) were all higher in low Kt/V group than high group (Table 5). Also, there was positive correlation between total throid volume and left CIMT, right CIMT, hs-CRP; and negative correlation between Kt/V and thyroid volume (Table 6, Figure 1).
|
|
Age |
Height |
Weight |
BMI |
BSA |
|
Total (n=50) |
58.48 ± 2.37 |
165.02 ± 1.44 |
67.78 ± 2.21 |
24.81 ± 0.73 |
1.73 ± 0.31 |
|
Male (n=34) |
58.94 ± 2.84 |
168.08 ± 1.72 |
69.63 ± 2.42 |
24.62 ± 0.76 |
1.78 ± 0.03 |
|
Female (n=16) |
57.5 ± 4.43 |
158.50 ± 1.79 |
63.85 ± 4.61 |
25.21 ± 1.67 |
1.64 ± 0.05 |
Mean ± SEM; (Body surface area (BSA) was calculated using the Dubois formula)
Table 1: General data of the studied population showing the mean age, weight, height, BMI and BSA.
|
Subjects (number) |
Thyroid volume (mL) |
Left lob volume (mL) |
Right lob volume (mL) |
|
Males (34) |
21.64 ± 1.83* |
10.55 ± 0.94** |
11.09 ± 0.97 |
|
Females (16) |
15.01 ± 1.60 |
6.55 ± 0.77 |
8.45 ± 0.95 |
|
All (50) |
19.52 ± 1.41 |
9.27 ± 0.73 |
10.25 ± 0.74 |
Mean ± SEM; * Males total thyroid volume different from females total thyroid volume, p = 0.009; **Males left lob different from females left lob, p = 0.002
Table 2: Volume of thyroid glands in females, males and all cases.
|
Groups |
Total thyroid volume (mL) |
AIP |
hs-CRP (mg/L) |
TAS |
TAD |
Uric Acid (mg/dL) |
Left CIMT (cm) |
Right CIMT (cm) |
|
Low PTH (< 13.6 pg/mL) (5) |
13.11 ± 2.61 |
0.59 ± 0.12 |
2.04 ± 0.52*† |
95.00 ± 2.23‡° |
64.00 ± 4.00 |
5.58 ± 0.67 |
0.64 ± 0.08 |
0.70 ± 0.06 |
|
Middle PTH (13.6-61.2 pg/mL) (13) |
18.40 ± 2.31 |
0.60 ± 0.05 |
11.05 ± 2.39 |
120.61 ± 0.26 |
71.53 ± 2.96 |
6.23 ± 0.88 |
0.78 ± 0.19 |
0.72 ± 0.04 |
|
High PTH (> 61.2 pg/mL) (32) |
20.98 ± 1.91 |
0.52 ± 0.03 |
11.82 ± 1.74 |
126.00 ± 3.93 |
75.15 ± 2.30 |
6.19 ± 0.23 |
0.75 ± 0.19 |
0.78 ± 0.04 |
Mean ± SEM; PTH; Parathyroid Hormone, AIP; Atherogenic Index of Plasma, hs-CRP; High Sensitivity C-Reactive Protein, TAS; Tension arterial systolic, TAD; Tension arterial diastolic,CIMT; Carotid Artery Intima-Media Thickness, *Significantly different from Middle PTH, p = 0.008; †Significantly different from high PTH, p < 0.001; ‡Significantly different from middle PTH, p < 0.001; °Significantly different from high PTH, p = 0.001
Table 3: Total Thyroid Volume, AIP, hs-CRP, TAS, TAD, Uric Acid, Left CIMT And Right CIMT In Patients With Low, Middle And High PTH Levels.
|
Groups |
Total thyroid volüme (ml) |
AIP |
hs-CRP (mg/L) |
TAS |
Weight (kg) |
Cholesterol (mg/dL) |
|
Low Uric Acid (<7 mg/dL) (39) |
19.77 ± 1.58 |
0.53 ± 0.03 |
11.43 ± 1.63 |
121.05 ± 3.48 |
65.17 ± 2.32* |
155.56 ± 4.29** |
|
High Uric acid (> 7 mg/dL) (11) |
18.63 ± 3.23 |
0.59 ± 0.06 |
7.85 ± 1.50 |
124.72 ± 3.88 |
77.04 ± 5.06 |
198.90 ± 16.44 |
Mean ± SEM; *Significanly different from High Uric Acid p= 0.025; **Significanly different from High Uric Acid p= 0.026
Table 4: Total Thyroid Volume, AIP, hs-CRP, TAS, Weight and Cholesterol in Patients With Low And High Uric Acid Levels.
|
Groups |
Total thyroid volüme (ml) |
Left CIMT (cm) |
Right CIMT (cm) |
Insulin (uU/mL) |
Cholesterol (mg/dL) |
TSH (mIU/L) |
|
Low Kt/v (< 1.2) (11) |
27.09 ± 1.84* |
0.81 ± 0.05** |
0.82 ± 0.04° |
9.27 ± 0.95† |
183.49 ± 8.06†† |
0.77 ± 0.13‡ |
|
High Kt/v (> 1.2) (39) |
16.62 ± 1.26 |
0.69 ± 0.02 |
0.70 ± 0.02 |
23.46 ± 2.72 |
153.05 ± 4.23 |
1.63 ± 0.20 |
Mean ± SEM; *Significantly different from high Kt/v p < 0,001; **Significantly different from high Kt/v p=0,020; °Significantly different from high Kt/v p=0,014;
†Significantly different from high Kt/v p < 0,001; ††Significantly different from high Kt/v p=0,002; ‡Significantly different from high Kt/v p=0,001
Table 5: Total Thyroid Volume, Left CIMT, Right CIMT, Insulin, Cholesterol and TSH in Patients with Low, and High Kt/v Levels.
Bold written ones; correlation is significant (2-tailed). r=Pearson or Spearman correlation, and p=significant/p value
Table 6: Correlation of Thyroid Volume with Kt/v, Left CIMT, Right CIMT, hs-CRP, Weight and TSH in all Patients.
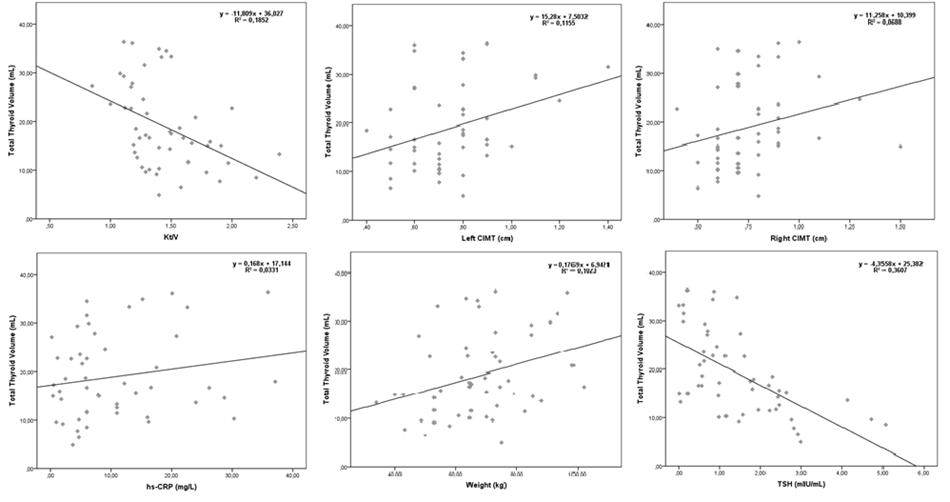
Figure 1: Scatter Plot for Total Thyroid Volume Against Kt/v, Left CIMT, Right CIMT, hs-CRP, Weight and TSH in all Patients.
4. Discussion
The increased frequency of thyroid dysfunction in CKD patients and the increase of thyroid gland volume has been demonstrated with previous studies [3]. In a previous study on healthy adult Turkish population, thyroid volume of males was 14:53 ± 2.55 ml and 12.9 ± 2:05 ml in females, and in all study group was determined as 12.98 ± 2.53 ml and these values are especially recommended as a reference value for Turkey's south-eastern regions [8]. In our study; we found total thyroid volume as 21.64 ± 1.83 mL in men, 15.01 ± 1.60 mL in women and 19.52 ± 1.41 mL in the whole group. We also found that in our HD patient population, thyroid volume increased as serum PTH level increased.
Thyroid diseases are common in CKD. It was found that morphological, functional and autoimmune thyroid diseases are more common in patients with hemoglobin levels below 125 g/ dL in CKD patients under HD treatment [3]. It was found that the average thyroid volume increased in HD patients. There was no significant relationship between the history of HD and thyroid volume. The most common thyroid pathologies in the HD patient population were diffuse and multinodular goiter. In the same patient group, a positive correlation was found between TSH levels and thyroid volume [9]. While low free T3 hormone levels were associated with arterial stiffness in PD patients, high TSH levels near the upper limit of normal range were found to be associated with low subendocardial viability rate in euthyroid PD patients [4].
In a study evaluating 143 patients in Japan, 14% of patients under HD had goiter (thyroid volume > 20 ml), and 59.4% of them, especially in women, had nodular lesions in the thyroid gland [10]. Thyroid hormones have been reported to be effective on kidney function. For this purpose, thyroid hormone and thiamazol, an antithyroid agent, were applied to the rats with renal failure. At the end of 22 weeks, the survival rate was 100% in the tiamazol group, while it was 62.5% in the group given thyroid hormone. Thyroid hormone aggravated tubular changes and interstitial volume increase triggered by adriamycin [11].
Thyroid dysfunction is frequently observed in cases under RRT. In kidney transplant cases, thyroid volume was found higher than HD and SAPD cases; while goiter and thyroid nodules were most frequently observed in transplantation, then HD and at least PD cases. A positive correlation was observed between thyroid volume and creatinine levels in kidney transplant cases [5].
Cardiovascular diseases are the main cause of morbidity and mortality in ESRD patients. When this patient group is evaluated in terms of CV risk factors; in addition to traditional risk factors, we encounter factors such as bone and mineral metabolism disorders, chronic inflammation, oxidative stress and hyperuricemia [12]. High PTH levels are blamed for the etiology of vascular calcification. Increased PTH acts as a uremic toxin; contributes to bone loss, vascular and cardiac valve calcification, anemia, cardiomyopathy, hypertension and glucose intolerance [13]. In studies conducted in the general population, HPTH has been shown to be associated with CV disease [14]. In CKD patients, some studies have shown that there is a higher risk of death due to CVD with increased PTH levels [15], while others have reported that low PTH is associated with a greater risk for CVD [16].
In our study; when groups were seperated as low (< 13.6 pg/mL), target (13.6-61.2 pg/mL) and high (> 61.2 pg/mL) PTH levels continuing for at least 6 months; cardiovascular risk factors such as AIP, hs-CRP, uric acid, bilateral CIMT were all lower in low PTH group in comparison with other groups. Serum UA level has been defined as an independent risk factor for future cardiovascular mortality in the general population [17]. In the literature, there are contradictory data about the role of UA in ESRD patients and its relationship with cardiovascular events, and some studies have found high UA levels [18], and some other studies associated low UA levels with cardiovascular events [19].
In our study group; when groups were seperated as low (<7 mg/dL) and high ((> 7 mg/dL) uric acid levels continuing for at least 3 months; , hs-CRP levels were also high in low uric acid group. When our patient groups were seperated as low (<1.2) and high (> 1.2) Kt/V levels for at least 1 year; total thyroid volume (p<0.001), bilateral CIMT (p<0.001) and total cholesterol levels (p=0.002) were all higher in low Kt/V group than high group as suggesting that adequate dialysis is also important in order to reduce cardiovascular risks.
5. Conclusions
In HD patients; thyroid volume, hyperparathyroidism, uric acid and atherogenic index of plasma may be an indicator of CV risk in harmony with other risk factors. Clinicians should evaluate these parameters during their clinical practices.
Ethics and Consent
Institutional Review board allowed for the project, and informed consent was taken from each participant.
Acknowledgments
None.
Funding Information
There is no source of funding; the project has been run on its own.
Competing Interests
There are no competing interests.
Authors Contribution
All authors contributed to designing the project, data collection, and interpretation, literature review, and gave the final evaluation.
References
- Düzgün E, Alpcan H, Gürel A, et al. The relationship between cardiac risk factors and total bilirubin levels ?n patients with chronic renal failure. European Journal of Biomedical and Pharmaceutical Sciences 5 (2018): 07-12.
- Pecoits-Filho R, Okpechi IG, Donner JA, et al. Capturing and monitoring global differences in untreated and treated end-stage kidney disease, kidney replacement therapy modality and outcomes. Kidney Int Suppl (2020): e3-e9.
- Jusufovic S, Hodzic E, Halilcevic A. Role of renal anemia in the functional, morphological and autoimmune thyroid disorders in patients on chronic hemodialysis. Med Arh 65 (2011): 228-232.
- Tatar E, Sezis Demirci M, Kircelli F, et al. The association between thyroid hormones and arterial stiffness in peritoneal dialysis patients. Int Urol Nephrol 44 (2012): 601-606.
- Lebkowska U, Malyszko J, Mysliwiec M. Thyroid function and morphology in kidney transplant recipients, hemodialyzed, and peritoneally dialyzed patients. Transplant Proc 35 (2003): 2945-2948.
- Harzand A, Tamariz L, Hare JM. Uric acid, heart failure survival, and the impact of xanthine oxidase inhibition. Congestive heart failure (Greenwich, Conn 18 (2012): 179-182.
- Hu P, Xuan Q, Hu B, et al. Fibroblast growth factor-23 helps explain the biphasic cardiovascular effects of vitamin D in chronic kidney disease. International journal of biological sciences 8 (2012): 663.
- Sahin E, Elboga E, Kalender E. Regional reference values of thyroid gland volume in Turkish adults. Srp Arh Celok Lek 143 (2015): 141-145.
- Jusufovic S, Hodzic E. Role of chronic hemodialysis in thyroid gland morphology disorders. Med Arh 65 (2011): 327-329.
- Sanai T, Okamura K, Inoue T, et al. Ultrasonographic detection of thyroid nodules in hemodialysis patients in Japan. Ther Apher Dial 14 (2010): 323-327.
- Sanai T, Hirano T, Nagata M, et al. Effects of thyroid function on the course of experimental chronic renal failure in rats. Ren Fail 27 (2005): 743-750.
- Lindner A, Charra B, Sherrard DJ, et al. Accelerated atherosclerosis in prolonged maintenance hemodialysis. The. New England Journal of Medicine 290 (1974): 697-701.
- Schieppati A, Pisoni R, Remuzzi G. Pathophysiology and management of chronic kidney disease. In: Greenberg A, Cheung. Ak, Coffman TM, Falk RJ, Jennette JCPrimer on Kidney Diseases. 4thPhiladelphia, Elsevier Saunders (ed) (2005): 444:454.
- Nilsson IL, Yin L, Lundgren E, et al. Clinical presentation of primary hyperparathyroidism in Europe nationwide cohort analysis on mortality from nonmalignant causes. Journal of bone and mineral research 17 (2002): 68-74.
- Tentori F, Blayney MJ, Albert JM, et al. Mortality risk for dialysis patients with different levels of serum calcium, phosphorus, and PTH: the Dialysis Outcomes and Practice Patterns Study (DOPPS). American Journal of Kidney Diseases 52 (2008): 519-530.
- Avram MM, Mittman N, Myint MM, et al. Importance of low serum intact parathyroid hormone as a predictor of mortality in hemodialysis and peritoneal dialysis patients: 14 years of prospective observation. American Journal of Kidney Diseases 38 (2001): 1351-1357.
- Zhao G, Huang L, Song M, et al. Baseline serum uric acid level as a predictor of cardiovascular disease related mortality and all-cause mortality: a meta-analysis of prospective studies. Atherosclerosis 231 (2013): 61-68.
- Antunovic T, Stefanovic A, Ratkovic M, et al. High uric acid and low superoxide dismutase as possible predictors of all-cause and cardiovascular mortality in hemodialysis patients. International Urology and Nephrology 45 (2013): 1111-1119.
- Lee SK, Lee AL, Winters TJ, et al. Low serum uric acid level is a risk factor for death in incident hemodialysis patients. American Journal of Nephrology 29 (2009): 79-85.
