Internet-delivered Parent-Child Interaction Therapy (I-PCIT) in Japan: Case Report of Application to a Maltreating Parent-Child Dyad
Article Information
Masako Kawasaki1*, Toshiko Kamo1
1Japan PCIT Training Center, Tokyo, Japan
*Corresponding Author: Dr. Masako Kawasaki, Japan PCIT Training Center, 9-4, Wakamatsu-cho, Shinjuku-ku, Tokyo, 1620056, Japan
Received: 21 November 2020; Accepted: 26 November 2020; Published: 07 December 2020
Citation:
Masako Kawasaki, Toshiko Kamo. Internet-delivered Parent-Child Interaction Therapy (I-PCIT) in Japan: Case Report of Application to a Maltreating Parent-Child Dyad. Archives of Clinical and Medical Case Reports 4 (2020): 1218-1233
View / Download Pdf Share at FacebookAbstract
Internet-delivered Parent-Child Interaction Therapy (I-PCIT) follows traditional clinic-based PCIT but uses a videoconferencing software to allow therapists to provide therapy remotely to families in their homes. We report the I-PCIT course of treatment for a 4-year-old Japanese boy (K) and his parents, an abusive parent-child dyad. This is the first report examining the applicability of I-PCIT in Japan. Weekly sessions were held for 60-90 minutes. At the end of the treatment, K showed a significant decrease in problematic behaviors, such as screaming, throwing objects, and hitting his parents. I-PCIT may be effective in helping both children and parents of families at high risk of abuse. In addition, parents’ skills are more likely to be generalized because the I-PCIT sessions are held at a site where problematic behaviors usually occur. I-PCIT is also useful for training new therapists; and with the growing need for specific abuse prevention initiatives that can be implemented remotely during the ongoing coronavirus pandemic, the benefits of the widespread use of I-PCIT are invaluable.
Keywords
Internet-delivered Parent-Child Interaction Therapy (I-PCIT); Telehealth; Technology; Maltreatment; Japan PCIT Training Center
Internet-delivered Parent-Child Interaction Therapy (I-PCIT) articles; Telehealth articles; Technology articles; Maltreatment articles; Japan PCIT Training Center articles
Internet-delivered Parent-Child Interaction Therapy articles Internet-delivered Parent-Child Interaction Therapy Research articles Internet-delivered Parent-Child Interaction Therapy review articles Internet-delivered Parent-Child Interaction Therapy PubMed articles Internet-delivered Parent-Child Interaction Therapy PubMed Central articles Internet-delivered Parent-Child Interaction Therapy 2023 articles Internet-delivered Parent-Child Interaction Therapy 2024 articles Internet-delivered Parent-Child Interaction Therapy Scopus articles Internet-delivered Parent-Child Interaction Therapy impact factor journals Internet-delivered Parent-Child Interaction Therapy Scopus journals Internet-delivered Parent-Child Interaction Therapy PubMed journals Internet-delivered Parent-Child Interaction Therapy medical journals Internet-delivered Parent-Child Interaction Therapy free journals Internet-delivered Parent-Child Interaction Therapy best journals Internet-delivered Parent-Child Interaction Therapy top journals Internet-delivered Parent-Child Interaction Therapy free medical journals Internet-delivered Parent-Child Interaction Therapy famous journals Internet-delivered Parent-Child Interaction Therapy Google Scholar indexed journals I-PCIT articles I-PCIT Research articles I-PCIT review articles I-PCIT PubMed articles I-PCIT PubMed Central articles I-PCIT 2023 articles I-PCIT 2024 articles I-PCIT Scopus articles I-PCIT impact factor journals I-PCIT Scopus journals I-PCIT PubMed journals I-PCIT medical journals I-PCIT free journals I-PCIT best journals I-PCIT top journals I-PCIT free medical journals I-PCIT famous journals I-PCIT Google Scholar indexed journals Telehealth articles Telehealth Research articles Telehealth review articles Telehealth PubMed articles Telehealth PubMed Central articles Telehealth 2023 articles Telehealth 2024 articles Telehealth Scopus articles Telehealth impact factor journals Telehealth Scopus journals Telehealth PubMed journals Telehealth medical journals Telehealth free journals Telehealth best journals Telehealth top journals Telehealth free medical journals Telehealth famous journals Telehealth Google Scholar indexed journals Technology articles Technology Research articles Technology review articles Technology PubMed articles Technology PubMed Central articles Technology 2023 articles Technology 2024 articles Technology Scopus articles Technology impact factor journals Technology Scopus journals Technology PubMed journals Technology medical journals Technology free journals Technology best journals Technology top journals Technology free medical journals Technology famous journals Technology Google Scholar indexed journals Maltreatment articles Maltreatment Research articles Maltreatment review articles Maltreatment PubMed articles Maltreatment PubMed Central articles Maltreatment 2023 articles Maltreatment 2024 articles Maltreatment Scopus articles Maltreatment impact factor journals Maltreatment Scopus journals Maltreatment PubMed journals Maltreatment medical journals Maltreatment free journals Maltreatment best journals Maltreatment top journals Maltreatment free medical journals Maltreatment famous journals Maltreatment Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals SARS-COV-2 articles SARS-COV-2 Research articles SARS-COV-2 review articles SARS-COV-2 PubMed articles SARS-COV-2 PubMed Central articles SARS-COV-2 2023 articles SARS-COV-2 2024 articles SARS-COV-2 Scopus articles SARS-COV-2 impact factor journals SARS-COV-2 Scopus journals SARS-COV-2 PubMed journals SARS-COV-2 medical journals SARS-COV-2 free journals SARS-COV-2 best journals SARS-COV-2 top journals SARS-COV-2 free medical journals SARS-COV-2 famous journals SARS-COV-2 Google Scholar indexed journals PCIT Training Center articles PCIT Training Center Research articles PCIT Training Center review articles PCIT Training Center PubMed articles PCIT Training Center PubMed Central articles PCIT Training Center 2023 articles PCIT Training Center 2024 articles PCIT Training Center Scopus articles PCIT Training Center impact factor journals PCIT Training Center Scopus journals PCIT Training Center PubMed journals PCIT Training Center medical journals PCIT Training Center free journals PCIT Training Center best journals PCIT Training Center top journals PCIT Training Center free medical journals PCIT Training Center famous journals PCIT Training Center Google Scholar indexed journals
Article Details
Abbreviations:
I-PCIT- Internet-delivered Parent-Child Interaction Therapy; PCIT- Parent-Child Interaction Therapy; CDI- Child-Directed Interaction; PDI- Parent-Directed Interaction; ECBI- Eyberg Child Behavior Inventory; VTC- Video-Teleconferencing; DPICS-IV- The Dyadic Parent-Child Interaction Cording System Fourth Edition; CLP- Child-Led Play; PLP- Parent Led Play; CU- Clean-Up; PSI-SF- Parental Stress Index-Short Version; PD- Parental Distress; P-CDI- Parent-Child Dysfunctional Interaction; DC- Difficult Child; BDI-II- Beck Depression Inventory-II; ACE- Adverse Childhood Experiences
1. Introduction
Maltreatment refers to the inappropriate nurturing and involvement of adults with children and encompasses physical, sexual, and psychological abuse and neglect. Children who have experienced maltreatment often exhibit problematic behaviors, such as physical aggression, noncompliance to adults, and antisocial behavior [1], which often lead to them consulting counseling agencies and hospitals. Internationally, Parent-Child Interaction Therapy (PCIT) has been effective at reducing rates of maltreatment recurrence and parental stress regarding the parent-child relationship for physically abusive parents with children aged 2-12 [2, 3]. The Kauffman Best Practices Project [4] recommends this as one of the best practices for child trauma treatment. Evidence suggests that patterns of negative and coercive parent-child relationships, lack of parental knowledge, and use of inappropriate discipline are predictive of child maltreatment risk [5]. Abusive and at-risk parents often use ineffective and inconsistent discipline strategies and rely too much on punishment. In the absence of more positive interactions, a hostile parent-child relationship thus develops that is characterized by negative parental attributions and intolerance toward the child, as well as an increasing reliance on harsh physical punishment as discipline [6]. PCIT helps break this cycle by encouraging positive interactions between parents and children and training parents in implementing consistent and nonviolent discipline techniques [7].
1.1 Clinic-based PCIT
PCIT is an evidence-based treatment originally designed for children between 2 and 7 years with disruptive behavior disorders [8]. It is based on developmental and behavioral theories, with elements of attachment and systems theories. One of the most significant features of PCIT is that both parents and children receive treatment together. Most of the treatment is performed in the playroom. Parents wear a “bug-in-the-ear,” and are coached directly by a therapist in the observation room, while playing with their child. PCIT is generally provided in 12 to 20 sessions and is mastery-based rather than time-limited.
PCIT includes two phases: child-directed interaction (CDI) and parent-directed interaction (PDI). The CDI phase focuses on improving the quality of the parent-child relationship. Parents learn to avoid commands, questions, and negative statements and are instead encouraged to use PRIDE skills during special time: Praise, Reflect, Imitate, Describe, and Enjoy. They also learn to apply differential social attention: ignoring inappropriate attention-seeking behaviors and giving specific praise for positive opposite behavior. Once parents reach the mastery criteria clearly defined in the protocol, they move on to the second phase of treatment.
The PDI phase focuses on teaching parents effective discipline strategies to increase child compliance and decrease negative behaviors. Parents learn to give effective commands to the child and provide consistent consequences for both compliance and noncompliance. When a child complies with a parent’s command, the parent is instructed to give a specific praise, “Thank you for listening to me right away” and they return to CDI. In contrast, when a child does not comply, a time-out warning is given. In addition, if the child does not comply with that warning, the parent must follow the time-out procedure. The PDI mastery criteria require parent commands to be at least 75% of all commands that are effective, direct commands and at least 75% of these effective, direct commands have the correct follow-through.
In both phases, parents are taught appropriate interaction skills through explanation, modeling, and role-playing. The criteria for treatment completion are as follows: the Eyberg Child Behavior Inventory (ECBI) score is less than 114 (in Japan, 112) that shows a child's problematic behavior has improved, parents’ CDI and PDI skills have reached the mastery criteria, and parents show confidence in their parenting.
PCIT was first introduced in Japan in 2008, when an open trial was started by Kamo (representative of the Japan PCIT Training Center) and her colleagues in Institute of Women’s Health, Tokyo Women’s Medical University [9,10]. Since being certified as a global trainer of PCIT International in 2015, Kamo and her colleagues have been making progress in disseminating and researching PCIT within the country, and several clinic-based PCIT cases have been reported [11,12]. In Japan, the Child Welfare Law and the Child Abuse Prevention Law banned all corporal punishments by parents in April 2020. In this social context, PCIT is receiving increasing attention in the field of childcare. The rapid dissemination of PCIT is urgent, but at the same time, the quality of therapists must be maintained and improved. Training the trainers, while ensuring program fidelity, is time-consuming; therefore, the program is unfortunately not available to all families who might benefit from it. For example, some families have to wait six months or more to receive PCIT or give up the treatment because their homes are too far from the clinic.
1.2 Internet-delivered PCIT
Telemedicine methods may overcome geographical barriers to mental healthcare access by extending the availability of expert services and overcoming regional healthcare professional shortages [13]. The increased ubiquity of internet access and the rapid technological advancements available to consumers across geographic and economic groups have positioned video-teleconferencing (VTC) as a powerful tool for overcoming barriers to treatment [14].
I-PCIT [13] follows traditional clinic-based PCIT but uses videoconferencing software to allow therapists to provide therapy remotely to families in their homes. Rather than interacting in front of a one-way mirror at a clinic, families use a webcam to relay their home interactions to their therapists, who provide live coaching remotely through a Bluetooth earpiece worn by the parent. Comer et al. [15] provided the first evidence from a controlled trial supporting the use of real-time VTC to remotely deliver behavioral parent training to a home setting. The skills of therapists conducting I-PCIT are essentially the same as those conducting a clinic-based PCIT, but additional expertise in dealing with equipment and communication problems is required.
The purpose of this study was to explore the application of I-PCIT as an effective intervention with a maltreating parent-child dyad, through a case study presentation. This is the first report to examine the application of I-PCIT in Japan.
2. Material and Methods
PCIT is an assessment-driven treatment. Assessments were conducted prior, during, and after treatment by using observational and standardized questionnaires, including the following measures. The ECBI [16] was used to assess child behavior problems. The scale has 36 items and comprises an intensity scale and a problem scale. The intensity scale measures the frequency of various behaviors on a 7-point scale; and the problem scale classifies behavior as either problematic or not (yes or no). The published cutoff scores are 131 for the intensity and 15 for the problem scale [16]. The Japanese version of ECBI has already been standardized by Kamo and the cutoff scores are 124 for the intensity and 13 for the problem scale in Japan [17]. The parents completed the ECBI at each session.
The Dyadic Parent-Child Interaction Cording System Fourth Edition (DPICS-IV) Japanese version [18] was used to assess the quality of parent-child interactions. This was translated by Kamo with the approval of the author, Prof. Eyberg, and is the one officially used in the PCIT International therapist and trainer certification system conducted in Japan. The pre- and post-treatment assessments included a 20-minute DPICS. This is used to code the behaviors of parents and children in three situations with different degrees of parental control or command: 10 minutes of Child-Led Play (CLP), 5 minutes of Parent Led Play (PLP), and Clean-Up (CU). The DPICS-IV was also used to code parent-child interactions during CLP before coaching at each session.
Parental Stress Index-Short Version (PSI-SF) [19] was used to assess parental stress. The scale has 36 items selected from all 120 items of the PSI [20] that fall into three subscales: Parental Distress (PD), which measures the distress a parent is experiencing in their role as a parent as a function of personal factors, Parent-Child Dysfunctional Interaction (P-CDI), which measures the parent’s perception that they feel dissatisfied with their child and their interaction with them, and Difficult Child (DC), which measures the parent’s perception that their child is difficult to take care of. For most items, parents respond by choosing SA (strongly agree), A (agree), NS (not sure), D (disagree), or SD (strongly disagree). Higher scores indicate higher levels of parenting stress. The Japanese version of PSI has been newly developed for use by Japanese parents based on the original version; however, the Japanese translation of the original version was used in this study under the permission of Psychological Assessment Resources and Employment Research Corporation.
Beck Depression Inventory-II (BDI-II) [21] was used to assess parental depressive symptoms. The BDI-II has 21 items, a self-report measure, which assesses depression-related symptoms in the past two weeks. Scores for multiple-choice responses are summed to provide an overall score for depression. It has been translated into Japanese by Kojima and Furukawa [22] and validated. The BDI-II scores may be used to identify the severity of depression: 0-13 (minimal), 14-19 (mild), 20-28 (moderate), and 29-63 (severe).
Adverse Childhood Experiences (ACE) scores were used to assess parental adverse experiences. The ACE study resulted from a study of 17,336 subjects in Southern California and San Diego who listed 10 unfortunate experiences, including violence, neglect, and divorce of their parents, and examined the relationship between the number of childhood experiences and their health status conducted by Centers for Disease Control Prevention and Kaiser Permanente Medical Care Program [23]. Parents select all items out of 10 that apply to them.
I-PCIT Procedures
I-PCIT was conducted using the most current protocol, the 2011 Parent-Child Interaction Therapy protocol Japanese edition [24]. To implement I-PCIT, we used a video conference software called Zoom. Weekly sessions were held for 60-90 minutes. Between sessions, parents were given homework sheets to record their skills’ practice at home every day. Parents sent the completed homework sheets and ECBI to the therapist via email before the start of each session. Each session began with a check-in interview, which included a review of the homework and the current parent-child relationship status. Because the child was often near parents during this time, the therapists were encouraged to praise children for waiting well and sometimes advised parents directly on how to respond to inappropriate behavior. The therapists conducted only CDI or both CDI and PDI coding to assess parents’ mastery of skills after check-in. The therapists then set coaching goals and coached parents based on observation data. During the checkout interview, the therapists shared the progress of the parents’ skills from baseline and discussed areas for reinforcement in their homework.
All sessions were conducted by two PCIT therapists; the first author (MK) served as the leading therapist and the co-therapist’s supervisor. She has been certified by PCIT International as a level 1 trainer. The co-therapist is in training to become a certified therapist, and this was her first case. Both the therapist and the co-therapist took turns coaching the parents at each session.
The purpose and significance of the case report, as well as the content and the method of the presentation, were fully explained to the parents and their consent was obtained, but sufficient consideration was given to privacy to avoid identifying them.
3. Case Presentation
K is a 4-year-old Japanese boy who lives with his father, mother, and a younger brother. Some of the behavioral concerns reported by his parents included throwing tantrums, not listening to adults (both at home and at the kindergarten), and difficulty concentrating. His mother was diagnosed with complex Post-Traumatic Stress Disorder. His father’s parents were divorced. Thus, neither of K’s parents had a good parental model. His parents responded to K by slapping him in the face, grabbing him by the chest, and throwing him onto the futon. His father works full-time and his mother is a stay-at-home mom. They are raising their children with their parents alone as they do not have anyone else’s support. K now attends a kindergarten daily but rarely plays with his friends, and runs away when children his age try to talk to him in the park.
K had never been diagnosed with a developmental delay or a mental illness before, but around the time this PCIT began, he consulted a developmental disability center and was diagnosed with suspected Attention Deficit Hyperactivity Disorder and Autism Spectrum Disorder. K was born at a normal weight of 3010 g. He cried frequently during the night, often for hours at a time, and would also become distressed when his mother held him. When he was one year old, he began walking and uttered his first words. Around 2 years old, he developed a tic where he would close his eyes for long periods. His nighttime crying ceased at around the age of three, but he now chews his nails, sucks his fingers, and puts sand and fallen objects in his mouth.
3.1 Course of Treatment
The family completed 5 CDI sessions and 9 PDI sessions (including two teach sessions) for a total of 14 PCIT sessions. Both parents attended all the sessions. They were highly motivated and engaged in their daily homework throughout the treatment. The homework sheets detailed their daily thoughts and questions. The questions were something like the following, “I tried to draw with K but he refused, so I ignored that behavior. Was that okay?” or “How do I respond to K’s violent attack on his brother?” These questions were answered by the therapist during the check-in interviews.
3.2 Walking Tour
A “walking tour” was conducted prior to the first I-PCIT session with the family. This included using Zoom to see if a consistent audio and screen connection could be established, adjust the camera angle, and set up the play area. Problems such as screen failure, Bluetooth earphones not connected to the device, and screen freezing due to weak Wi-Fi are common in I-PCIT; hence, pre-setup is very important. K’s parents were very familiar with the use of these devices, including Zoom, and the selection of places for parents and children to play was appropriate. In I-PCIT, it is also important to discuss with parents on how to minimize disturbance during the sessions; hence, K’s parents decided that his 5-month-old younger brother would be looked after by the parent who was not involved in coaching.
3.3. Intake Session
The DPICS intake assessment was conducted following the “walking tour.” Appropriate toys for CDI were explained to K’s parents and they set out clay, drawing, Legos, something to build, and Tomica vehicles. For I-PCIT, it is more appropriate to use toys that do not produce any sound, such as soft blocks, clay, or drawings, as these will not interfere with the audio transmission. Pre-DPICS was conducted first by K’s mother and then by his father. K’s mother sometimes repeated K’s words, and there was a lot of eye contact during CLP. She encouraged K to participate in her chosen play through frequent indirect commands during PLP. Then, during the CU, K quickly put his toys away with almost no commands. K’s father was imitating K’s play well while they played with clay together during CLP. There was also a moment where K handed clay to his father. In contrast, when it came to PLP, K ran away from the room, went to his younger brother, and continued to refuse his father’s commands until the CU ended.
3.4. CDI/PDI Teach Sessions
Both parents attended teach sessions with enthusiasm. During the CDI teach session, because K’s mother often had to take care of his younger sibling, role-playing was conducted by K’s father and the co-therapist. The co-therapist played the role of the child and K’s father practiced PRIDE skills while watching her over the screen. During the PDI teach session, after the therapist demonstrated the time-out procedure, K’s mother played the child and K’s father played the parent during role play. K’s father was able to practice his lines smoothly and accurately. Interacting with parents or role-playing is not easy during the teach sessions at I-PCIT, but they can be carried out by carefully checking parents’ understanding of and demonstrating role-playing over the screen.
3.5. CDI/PDI Coach Sessions
During the CDI coach sessions, parents learned to use PRIDE skills and reduce avoidance skills during special time. K enjoyed playing with his parents, but sometimes behaved inappropriately. After the second CDI session, a lot of time was spent coaching ignoring skills due to the frequent occurrence of inappropriate behavior. K often escaped from the room, tried to remove the earphones from his father's ears, interfered with his mother's play, and tried to turn off the computer. However, if the parent playing with K used ignoring skills, K would go toward the other parent, making it harder to get across to the child than when it was done in the playroom. Therefore, the way to ignore K’s behavior after declaring something like, “Mom will be quiet until I can talk to you quietly” was tried. As a result, K was crying and giggling, which was clearly different from previous attention-seeking behaviors, and then his inappropriate behavior gradually decreased. K’s father and mother met the mastery criteria for CDI during the third and fourth CDI session, respectively.
During PDI coach sessions, parents learned to give effective commands to the child and to provide consistent consequences for both compliance and noncompliance. During the first PDI coaching session, K could not switch from playing with his mother to father. As he could not obey the command to “sit next to your father,” he was put in a time-out. We set the time-out room in the Japanese-style room, but K started playing with the futon and escaped to the balcony, so we changed it to the bathroom. After being in a time-out chair 10 times and in the time-out room 6 times, K complied with his father’s command. After the time-out procedure, K calmly enjoyed playing with his father. After the coaching, K’s father told us that, in the past, he would have stopped trying to get K to follow orders in a situation like this. During the checkout of the sixth PDI coaching, house rule was applied because K strongly pushed his younger brother. K was able to sit quietly in a time-out chair for three minutes. Pattern learning was working perfectly, and K’s own emotional control was improving. The last two sessions, the eighth PDI coaching session and the graduation session, were conducted at the clinic. During the eighth PDI coaching session, public behavior was practiced with K and his father. K followed the rule that his father had told him beforehand, “Walk hand in hand with me,” and he cooperated until the end.
4 Assessment Progress
Table 1 shows the pre- and post-intervention scores. The ECBI intensity scores before treatment for K’s mother and father were 154 and 140, respectively; the problem scores for his mother and father were 25 and 15, respectively. This indicated that K’s problematic behavior was in the clinical domain. The ECBI intensity scores after treatment for K’s mother and father were 107 and 72, respectively; and the problem scores for his mother and father were 15 and 2, respectively, which means both parents rated K’s problem behaviors as reducing. Figures 1 and 2 show the ECBI intensity and problem scores over the course of the PCIT, respectively. In terms of BDI-II, K’s mother scored 33 before and 10 after treatment. In contrast, K’s father scored 20 before treatment, but his score went up to 29 after treatment. A similar trend was seen in the PSI-SF scores, with K’s mother’s score dropping from 138 before to 114 after treatment, while K’s father’s DC score dropped by about 10 points; however, his total stress remained virtually unchanged. Despite the apparent decrease in K’s problematic behaviors, a possible reason for this lack of improvement in K’s father’s depressive symptoms and parenting stress may be due to his own mood instability. Regarding ACE scores, K’s mother scored 3, while his father scored 6. Felitti et al. [23] found that persons who had experienced four or more categories of childhood exposure, compared to those who had experienced none, had increased health risks including depression. This suggests that K’s father’s mood instability may have been influenced by his adversity experiences, and he would be able to raise his children with more ease if he had mental support. However, this needs further study.
Regarding the Do and Don't skills scores in the CLP of DPICS-IV at pre- and post-treatment, K’s mother had few behavior descriptions and labeled praise before the treatment, and she had more than 15 of them for each skill after the treatment (Figure 3). About the Don’t skills, there were a lot of questions and a few negative statements before the treatment, but none after the treatment (Figure 4). K’s father had no behavior descriptions at all, little reflections, and labeled praise before the treatment; however, reflections increased significantly (Figure 5) after the treatment. The total number of Don't skills decreased from eight before the treatment to three after the treatment (Figure 6). In the post-treatment CLP, K’s father did not use behavior descriptions nor labeled praise frequently, but he had reached the mastery criteria until the immediately preceding session. This gap may be related to the father’s mental health problems. The parents reported that K’s father had been severely unwell for the past two weeks, at times flipping tables and saying “I want to die” in front of K.
|
Measure |
Pre |
Post |
|
ECBI |
||
|
Intensity Scale (mother's report) |
154 |
107 |
|
Problem Scale (mother's report) |
25 |
15 |
|
Intensity Scale (father's report) |
140 |
72 |
|
Problem Scale (father's report) |
15 |
2 |
|
PSI-SF |
||
|
Parental Distress (mother's report) |
47 |
41 |
|
Parent-Child Dysfunctional Interaction (mother's report) |
37 |
29 |
|
Difficult Child (mother's report) |
54 |
44 |
|
Total Stress (mother's report) |
138 |
114 |
|
Parental Distress (father's report) |
38 |
48 |
|
Parent-Child Dysfunctional Interaction (father's report) |
29 |
30 |
|
Difficult Child (father's report) |
52 |
42 |
|
Total Stress (father's report) |
119 |
120 |
|
BDI-II (mother's report) |
33 |
10 |
|
BDI-II (father's report) |
20 |
29 |
|
ACE Score (mother's report) |
3 |
|
|
ACE Score (father's report) |
6 |
|
Table 1: Pre- and post-treatment assessment results.
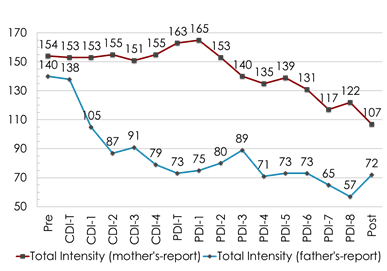
Figure 1: Eyberg Child Behavior Inventory (ECBI) intensity scores. Note. The clinical cut-off for the intensity subscale of the ECBI is 124.
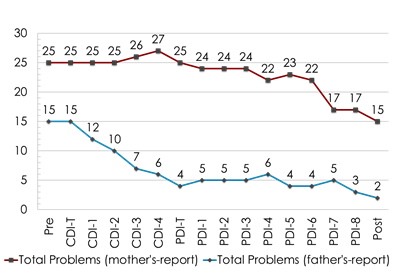
Figure 2: Eyberg Child Behavior Inventory (ECBI) problem scores. Note. The clinical cut-off for the problem subscale of the ECBI is 13.
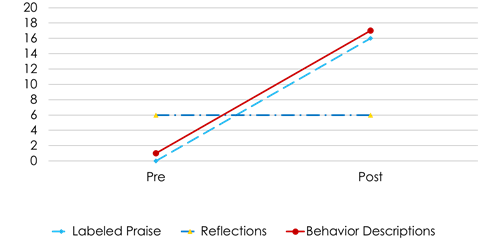
Figure 3: Mother's frequency of Do skills from Pre- and Post-treatment during Child-Led Play (CLP).
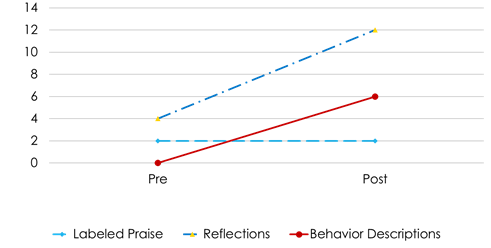
Figure 4: Mother's frequency of Don’t skills from Pre- and Post-treatment during Child- Led Play (CLP).
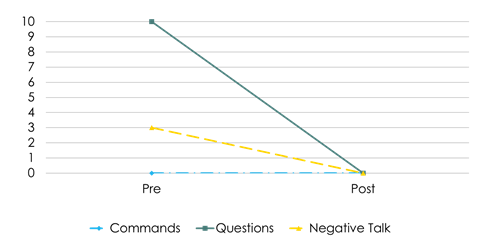
Figure 5: Father's frequency of Do skills from Pre- and Post-treatment during Child-Led Play (CLP).
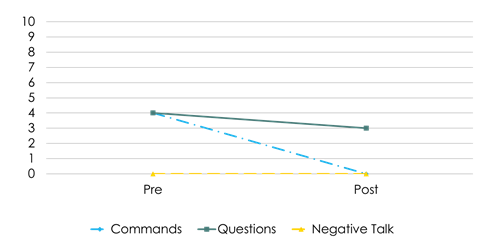
Figure 6: Father's frequency of Don’t skills from Pre- and Post-treatment during Child- Led Play (CLP).
5. Discussion
5.1 Ease of generalization
Comer et al. [15] have suggested that I-PCIT may enhance the treatment’s ecological validity by coaching parents at home where their children’s behaviors are the most problematic. In traditional PCIT, children are sometimes calmer in the clinic than at home, and it can be difficult for the therapist to intervene directly in troubling situations. As parents’ skills improve, generalization progresses and eventually parents are able to cope with their child’s problematic behaviors; however, in cases where the problematic behaviors are severe to begin with, it takes time for generalization to occur, and it sometimes happens that the ECBI scores do not decline until the end of therapy. Alternatively, some parents may be able to use the skills well in coaching situations, but when they return home, they revert to their previous responses, and it takes time for them to be able to use the skills in an environment without a therapist. With I-PCIT, the parents’ skills are more likely to be generalized because the sessions are held at a site where problematic behaviors usually occur. In addition, as children are no longer restrained by the company of a stranger, they are more likely to reproduce behaviors that are troubling to their parents. For this family, the time it took to complete the PCIT was shorter than usual. The introduction of I-PCIT may have facilitated generalization, but it should be verified by increasing the number of cases in the future.
5.2 Expansion of the treatment target population
As I-PCIT disseminates, more families will be able to receive PCIT. In Japan, some families are unable to receive PCIT because of the distance between the clinic and their homes. In the acute phase of the spread of the coronavirus infection, many parents also said that they were afraid to take their children on the train to the city. I-PCIT allows many families to be able to receive PCIT safely and without difficulty. In fact, some families who live far from the Japan PCIT Training Center are receiving I-PCIT.
It also seems that the number of caregivers in the family who receive treatment will increase. In our center, with clinic-based PCIT, most of the time only one parent is treated. However, after the introduction of I-PCIT, the number of families with both parents receiving treatment increased significantly. By connecting two Zoom lines, one parent’s coaching can be observed by the other parent. In fact, due to the modeling effect, the father learned skills at the same speed as the mother, even though the mother spent more time being coached.
I-PCIT and training
When trainers supervised PCIT trainees at a distance, a video recording of the session was previously made and checked by the trainers later. While this method has the advantage of providing careful feedback, it also has the disadvantage of taking time to correct the way things are done, and it is difficult for trainees to understand just a verbal explanation. With I-PCIT, trainers and trainees at a distance can work together on a case, allowing trainees to observe trainers’ coaching and practice right away. In doing so, we saw significant progress in the trainees’ coaching skills. This is absolutely a modeling effect.
In addition, Zoom’s private chat feature is very useful for direct supervision. The trainer can watch the trainee’s coaching and provide written feedback when appropriate. While it is easy to give immediate feedback when the trainer and the trainee are in the same location, the challenge is that the trainer interferes too much and does not encourage the trainee’s independence. The private chat allows the trainer to think about whether to advise right now or wait a little longer. In fact, we experienced several times that trainees had made their own decisions while we were typing the feedback and ultimately, we did not have to give any feedback.
5.4 Feasibility of implementing a hybrid model
Almost all sessions were conducted with I-PCIT due to the coronavirus spread, but in the future, it may be possible to conduct them in combination with clinic-based PCIT. For example, only the initial coaching session can be clinic-based while the rest of the treatment is I-PCIT. There may be a way to introduce I-PCIT from around PDI coaching session 3, which emphasizes generalization. This hybrid method allows for a “step-by-step generalization,” that is, it is easy to conduct for new therapists. However, this approach has challenges in terms of cost. In Japan, many clinics perform PCIT within the framework of insurance coverage, and insurance and self-funding cannot be combined according to the Japanese law. Therefore, to disseminate I-PCIT in Japan, it is essential to have a system that ensures sufficient income for each organization.
5.5 Limitations
Although the findings of this case study serve as preliminary evidence supporting the use of I-PCIT with maltreating parent-child dyads, it has significant limitations. The first limitation of this study is the case study design, which lacks multiple subjects, randomization, and control group comparison. For this reason, I cannot determine whether the findings were due to I-PCIT treatment or were a result of the passage of time or some other unidentified variable. Future research should focus on implementing studies with larger samples, randomization, and experimental design to help establish I-PCIT as an effective intervention for maltreating parent-child dyads.
6. Conclusion
We report a case study of the successful use of I-PCIT on a 4-year-old child who was maltreated and exhibited aggressive and disruptive behaviors. I-PCIT was associated with a clinically significant reduction in K’s disruptive, aggressive, and non-compliant behaviors. In Japan, the demand for I-PCIT is expected to increase further. This paper should be highly influential in promoting the use of I-PCIT.
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Competing Interests
The authors declare that they have no competing interests.
Funding
This work was supported by JST CREST Grant Number JPMJCR18A4, Japan.
References
- Kolko DJ. Characteristics of child victims of physical violence: Research findings and clinical implications. Journal of Interpersonal Violence 7 (1992): 244-276.
- Kennedy SC, Kim JS, Tripodi S, et al. Does parent-child interaction therapy reduce future physical abuse? A meta-analysis. Research on Social Work Practice 26 (2016): 147-156.
- Thomas R, Zimmer-Gembeck MJ. Parent-child interaction therapy: An evidence-based treatment for child maltreatment. Child Maltreatment 17 (2012): 253-266.
- Kauffman Best Practices Project. Closing the Quality Chasm in Child Abuse Treatment: Findings of the Kauffman Best Practices Project to Help Children Heal from Child Abuse. Charleston, SC: National Crime Victims Research and Treatment Center (2004).
- Cicchetti D, Valentino K. An ecological-transactional perspective on child maltreatment: Failure of the average expectable environment and its influence on child development. In Ed: Cicchetti D, Cohen D. Developmental psychopathology, 2nd edition, Volume three. Risk, disorder, and adaptation. New Jersey: John Wiley & Sons Inc. (2006): 129-201.
- Chaffin M, Silovsky JF, Funderburk B, et al. Parent-child interaction therapy with physically abusive parents: Efficacy for reducing future abuse reports. Journal of Consulting and Clinical Psychology 72 (2004): 500-510.
- Child Welfare Information Gateway. Parent-child interaction therapy with at-risk families. Washington, D.C.: U.S. Department of Health and Human Services, Children’s Bureau (2013).
- Eyberg S, Robinson EA. Conduct problem behavior: Standardization of a behavioral rating scale with adolescents. Journal of Clinical Child Psychology 12 (1983): 347-354.
- Kamo T. Rebuilding of the nurturing relationship and parent-child interaction therapy of mothers and children affected by domestic violence (In Japanese). Seishin Shinkeigaku Zasshi/Psychiatria et Neurologia Japonica 112 (2010): 885-889.
- Kamo T, Ujiie Y, Ito F, et al. The Efficacy of parent-child interaction therapy for Japanese mother-child dyads exposed to intimate partner violence (In Japanese). Journal of Tokyo Women's Medical University 86 (2016): 48-58.
- Hosogane N, Kodaira M, Kihara N, et al. Parent-child interaction therapy(PCIT) for young children with attention-deficit hyperactivity disorder (ADHD) in Japan. Annals of General Psychiatry 17 (2018): Article 9.
- Furuzawa A, Yoshinaga N, Hattori K. Parent-child interaction therapy for Japanese working mother and child with behavioral problems: A single case study. Clinical Case Studies 19 (2020): 270-281.
- Comer JS, Furr JM, Cooper-Vince C, et al. Rationale and considerations for the Internet-based delivery of Parent-Child Interaction Therapy. Cognitive and Behavioural Practice 22 (2015): 302-316.
- Cooper-Vince CE, Chou T, Furr JM, et al. Videoteleconferencing early child anxiety treatment: A case study of the Internet-delivered PCIT CALM (I-CALM) program. Evid Based Practice in Child and Adolescent Mental Health 1 (2016): 24-39.
- Comer JS, Furr JM, Miguel EM, et al. Remotely delivering real-time parent training to the home: An initial randomized trial of Internet-delivered Parent-Child Interaction therapy (I-PCIT). Journal of Consulting and Clinical Psychology 85 (2017): 909-917.
- Eyberg S, Pincus D. Eyberg Child Behavior Inventory and Sutter-Eyberg Student Behavior Inventory-revised: Professional manual. Odessa, FL: Psychological Assessment Resources (1999): 1-59.
- Kamo, T. Eyberg Child Behavior Inventory Japanese edition. Tokyo, Japan: Chiba Test Center (2016).
- Eyberg SM, Chase RM, Fernandez MA, Nelson MM, Kamo, T transl. Dyadic Parent-Child Interaction Coding System (DPICS) Clinical Manual Japanese version of the draft. 4th edition. Gainesville, FL: PCIT International (2014).
- Abidin RR. Parenting Stress Index-Short Form Test Manual. Charlottesville, VA: Pediatric Psychology Press (1990).
- Richard, R. A. Parenting stress index. 3rd edition. Florida: Psychological Assessment Resources (1995).
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio: The Psychological Corporation (1996).
- Kojima M, Furukawa TA, Takahashi H, et al. Cross-cultural validation of the Beck Depression Inventory-II in Japan. Psychiatry Research 110 (2002): 291-299.
- Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) Study. American Journal of Preventive Medicine 14 (1998): 245-258.
- Eyberg SM, Funderburk BW, Kamo, T transl. Parent-Child Interaction Therapy protocol Japanese edition. Gainesville, FL: PCIT International (2011).
