Internal Hemipelvectomy through a Periacetabular Osteotomy Combined with an Extraarticular (Proximal) Femur Resection using A Single Posterolateral approach; The Surgical Technique
Article Information
Robbert JH Van Leeuwen1*, Martin Beck1,4, Bruno Fuchs1,2,3
1Department of Orthopaedic and Trauma Surgery, Luzerner Kantonsspital, Lucerne, Switzerland
2Department of Orthopaedic and Trauma Surgery, Kantonsspital Winterthur, Winterthur, Switzerland
3Department of Plastic Surgery, USZ, University hospital of Zürich, Zürich, Switzerland
4Orthopädische Klinik Luzern, Hirslanden St. Anna, Luzern, Switzerland
*Corresponding Author: Robbert JH Van Leeuwen, Department of orthopaedic and trauma surgery, Luzerner Kantonsspital, Lucerne, Switzerland
Received: 15 April 2022; Accepted: 22 April 2022; Published: 01 June 2022
Citation: Robbert JH Van Leeuwen, Martin Beck, Bruno Fuchs. Internal Hemipelvectomy through a Periacetabular Osteotomy Combined with an Extraarticular (Proximal) Femur Resection using A Single Posterolateral approach; the Surgical Technique. Journal of Surgery and Research 5 (2022): 305-321.
View / Download Pdf Share at FacebookAbstract
To reach the best oncological perspective in intra-articular, periacetabular and/or proximal femur tumors, a radical extra-articular periacetabular resection is necessary. In this case report we present an extra-articular periacetabular resection technique through a posterolateral approach to the hip. This surgical technique is relatively unknown in tumor surgery of Enneking type II lesions.
Cases
Three patients with malignant tumor growth in the hip joint were treated with a wide, extra-articular resection of the hip joint, conducted through a posterolateral approach. Reconstruction was realized in 2 cases with a Burch-Schneider reinforcement cage, in the other case with a LUMIC prosthesis. In all three cases, the short followup showed excellent functional outcome and only one minor complication; a subcutaneous hematoma for which transfusion was necessary.
Conclusion
This approach to the hip joint shows promising results in treating tumors of the periacetabu- lar region. Further research to discover long term functional outcomes is necessary.
Keywords
Surgical Technique, Hemipelvectomy, Hip
Surgical Technique articles Surgical Technique Research articles Surgical Technique review articles Surgical Technique PubMed articles Surgical Technique PubMed Central articles Surgical Technique 2023 articles Surgical Technique 2024 articles Surgical Technique Scopus articles Surgical Technique impact factor journals Surgical Technique Scopus journals Surgical Technique PubMed journals Surgical Technique medical journals Surgical Technique free journals Surgical Technique best journals Surgical Technique top journals Surgical Technique free medical journals Surgical Technique famous journals Surgical Technique Google Scholar indexed journals Hemipelvectomy articles Hemipelvectomy Research articles Hemipelvectomy review articles Hemipelvectomy PubMed articles Hemipelvectomy PubMed Central articles Hemipelvectomy 2023 articles Hemipelvectomy 2024 articles Hemipelvectomy Scopus articles Hemipelvectomy impact factor journals Hemipelvectomy Scopus journals Hemipelvectomy PubMed journals Hemipelvectomy medical journals Hemipelvectomy free journals Hemipelvectomy best journals Hemipelvectomy top journals Hemipelvectomy free medical journals Hemipelvectomy famous journals Hemipelvectomy Google Scholar indexed journals treating tumors articles treating tumors Research articles treating tumors review articles treating tumors PubMed articles treating tumors PubMed Central articles treating tumors 2023 articles treating tumors 2024 articles treating tumors Scopus articles treating tumors impact factor journals treating tumors Scopus journals treating tumors PubMed journals treating tumors medical journals treating tumors free journals treating tumors best journals treating tumors top journals treating tumors free medical journals treating tumors famous journals treating tumors Google Scholar indexed journals local resection articles local resection Research articles local resection review articles local resection PubMed articles local resection PubMed Central articles local resection 2023 articles local resection 2024 articles local resection Scopus articles local resection impact factor journals local resection Scopus journals local resection PubMed journals local resection medical journals local resection free journals local resection best journals local resection top journals local resection free medical journals local resection famous journals local resection Google Scholar indexed journals posterolateral approach articles posterolateral approach Research articles posterolateral approach review articles posterolateral approach PubMed articles posterolateral approach PubMed Central articles posterolateral approach 2023 articles posterolateral approach 2024 articles posterolateral approach Scopus articles posterolateral approach impact factor journals posterolateral approach Scopus journals posterolateral approach PubMed journals posterolateral approach medical journals posterolateral approach free journals posterolateral approach best journals posterolateral approach top journals posterolateral approach free medical journals posterolateral approach famous journals posterolateral approach Google Scholar indexed journals fibrous dysplasia articles fibrous dysplasia Research articles fibrous dysplasia review articles fibrous dysplasia PubMed articles fibrous dysplasia PubMed Central articles fibrous dysplasia 2023 articles fibrous dysplasia 2024 articles fibrous dysplasia Scopus articles fibrous dysplasia impact factor journals fibrous dysplasia Scopus journals fibrous dysplasia PubMed journals fibrous dysplasia medical journals fibrous dysplasia free journals fibrous dysplasia best journals fibrous dysplasia top journals fibrous dysplasia free medical journals fibrous dysplasia famous journals fibrous dysplasia Google Scholar indexed journals Caucasian female patient articles Caucasian female patient Research articles Caucasian female patient review articles Caucasian female patient PubMed articles Caucasian female patient PubMed Central articles Caucasian female patient 2023 articles Caucasian female patient 2024 articles Caucasian female patient Scopus articles Caucasian female patient impact factor journals Caucasian female patient Scopus journals Caucasian female patient PubMed journals Caucasian female patient medical journals Caucasian female patient free journals Caucasian female patient best journals Caucasian female patient top journals Caucasian female patient free medical journals Caucasian female patient famous journals Caucasian female patient Google Scholar indexed journals systematic therapy articles systematic therapy Research articles systematic therapy review articles systematic therapy PubMed articles systematic therapy PubMed Central articles systematic therapy 2023 articles systematic therapy 2024 articles systematic therapy Scopus articles systematic therapy impact factor journals systematic therapy Scopus journals systematic therapy PubMed journals systematic therapy medical journals systematic therapy free journals systematic therapy best journals systematic therapy top journals systematic therapy free medical journals systematic therapy famous journals systematic therapy Google Scholar indexed journals
Article Details
1. Introduction
Resection of periacetabular tumors is challenging and techniques have changed over time. In earlier days, patients underwent a hindquarter resection which was often associated with complications and impaired function [1]. Over the last few decades, internal hemipelvectomy in which the ipsilateral limb is salvaged has become standard practice because of an acceptable rate of local recurrence [2]. Multiple resection and reconstruction possibilities have evolved since then, which is further discussed below. Historically, the approaches to the acetabulum were developed for the treatment of fractures. Some of these are used or modified to resect pelvic malignancies. Already in 1917, the Norwegian Smith-Petersen described the iliofemoral approach [3], which was modified by Judet and Letournel in 1964 [4]. In this modified version, the abdominal muscles were released from the iliac crest, to expose the entire internal surface of the iliac bone. The ilioinguinal approach was described by Letournel in 1961 [5]. Another often used approach is the modified Stoppa approach through a Pfannenstiel incision 1 to 2 centimeters superior to the pubic symphysis [6,7]. The iliofemoral, the ilioinguinal and the modified Stoppa approaches are the three main approaches. Multiple alternatives and modifications have been published [8-12]. Although all these options are documented, the best known surgical approach for internal hemipelvectomy is the utilitarian incision, first described by Enneking in 1978 [13]. This approach, which runs along the iliac crest (from postero-inferior possibly all along to the os pubis) and is extended distally along the femoral vessels, has been often described and is seen as the golden standard in pelvic tumor surgery [14]. Multiple modifications to this surgical approach, such as the T-incision, where the “T” is located more laterally, have been reported [15-18]. Another well-known approach to the acetabulum and proximal femur is the posterolateral approach, better known as the Kocher-Langenbeck approach. Langenbeck in 1867 and Kocher in 1911 first described this approach, which was mentioned as the Kocher-Langenbeck approach in 1954 by Judet [19]. Until now, this approach is mostly used in trauma surgery and elective hip surgery. In these patients, good functional outcome has been documented [20,21]. For resections of tumors of the pelvis, however, this surgical technique as a single approach has so far only been described in a few case reports [22-24]. Most publications focus on reconstruction options, which heavily depend on the type and extent of the resection. Function of the hip after resection depends on the reconstruction and the preservation of muscle attachments. We describe our resection technique for patients with intraarticular tumors of the hip. To reach best possible outcome and reduce the risk of metastasis, wide resection is necessary [25]. With the following three cases, we describe a surgical technique where a wide extracapsular resection of the hip cavity was performed with maximal preservation of muscular function.
2. Case Presentation
Case 1
A 68 year old healthy Caucasian male patient presented himself in our orthopedic outpatient clinic with severe hip pain on the right side. The pain was most severe in active flexion of the right leg, although no functional limitations (e.g. flexion, extension and rotation of the hip) could be determined. The patient's history shows a resection of a right pleural solitary fibrous tumor of 14 centimeters (2017, 3 years ago), which was reported as a SFT with histopathological suspicion for malignant growth (high rates of mitosis and necrosis). The primary resection was performed at an outside institution. A relatively small thoracotomy was performed and the tumor was resected without complications. In the follow-up, no complications or local recurrence were reported either. No other diseases were detected besides this tumor. After first presentation, additional X-rays, a (Positron Emission Tomography (PET-)) CT-scan and MRI of the right hip were conducted (figure 1). In the X-rays no abnormalities were observed, but in the CT-scan a PET-positive 28 x 18 millimeter osteolytic lesion was found in the anterior femoral head. From anterolaterally, three biopsies with an 18 gauge core-needle were gained, which all showed a SFT, malig-nant and likely representing a metastasis from the 2017 pleural SFT. The MRI showed an oedematous bone marrow which in total size was up to 5 cm in diameter, with a disrupted cortex of the femoral head and direct extension into the right hip joint, but without extracapsular growth. Because of the possibility of a metastasis, we decided to perform a complete resection including the contaminated hip joint.
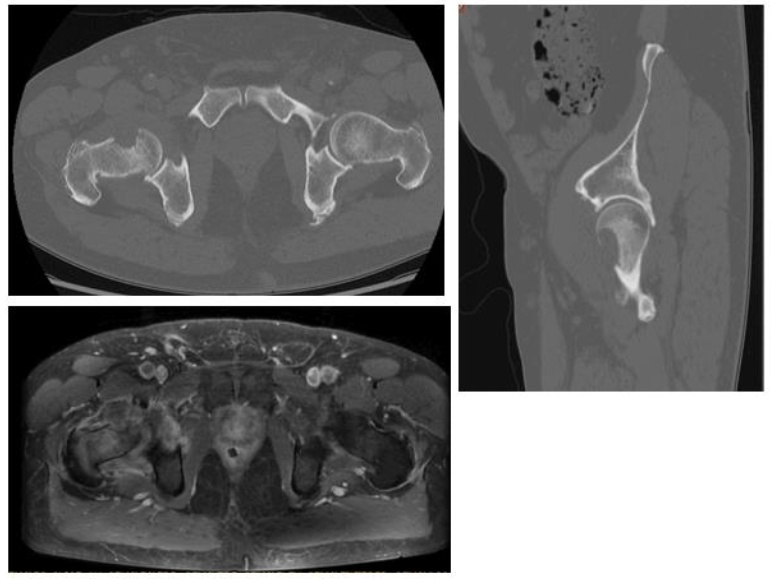
Figure 1: CT-Scan and MRI from the first patient- an intracapsular, 28 x 18 millimeter osteolytic lesion was seen in the proximal Femur.
Case 2
In this case, a 37 year old Caucasian female patient was diagnosed with an asymptomatic local recurrence of a secondary chondrosarcoma based on previous synovial chondromatosis in the left proximal femur. This otherwise healthy patient was previously treated with local resection because of a synovial chondromatosis of the left hip in 2010 and 2013. In 2016, a secondary chondrosarcoma developed and a prox-imal femur resection and a total hip arthroplasty were performed through an ilioinguinal approach (Figure 2a). In addition, the femoral artery and vein were resected and replaced with a vascular prosthesis. After a year without problems and with good functionality, the patient developed an intraarticular chondrosar-coma again (Figure 2b). Because of the intracapsular growth, we decided to resect the total hip joint through a posterolateral approach. No systematic disease was diagnosed.
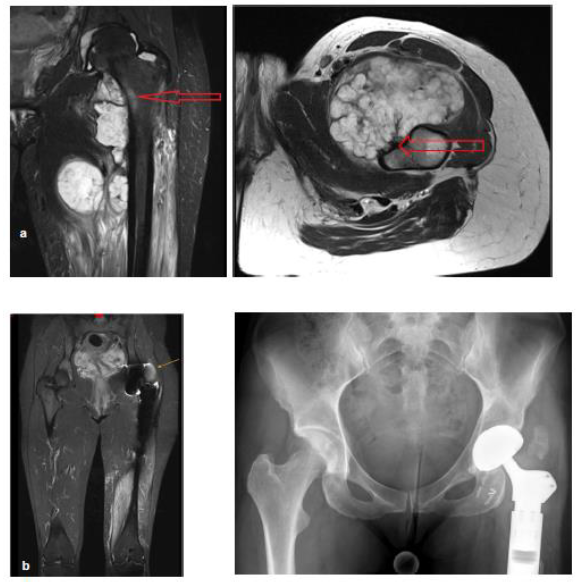
Figure 2: (a) The situation in December 2015 in the second case. The secondary chondrosarcoma, surrounded by the previously known synovial chondromatosis is pointed out. In the transversal cut, the minimal distance to femoral artery and vein and to sciatic nerve is seen. (b) MRI pictures with the intracapsular local recurrence of the secondary chondrosarcoma.
Case 3
The third patient is a 65 year old Caucasian female patient with fibrous dysplasia of both proximal femora. She presented herself in October 2018 with severe right hip pain after a minor trauma. An X-ray showed a possible pathological subtrochanteric fracture of the right femur. Because of a concomitant coxarthrosis, the decision was made to implant a total hip arthroplasty with additional cerclage at the trochanter major. Histological results showed a fibrous dysplasia, without malignant aspects. Therefore, a regular follow up was conducted without adjuvant therapy. The patient was very satisfied with the func-tionality, but around at one year follow up she developed a slowly rising pain in the right hip, and additional imaging was performed. An MRI scan showed a lesion of 10 x 7 x 14 centimeter proximally circumventing the prosthesis, with infiltration of the soft tissues (Figure 3). Through a biopsy, a secondary malignant osteosarcoma was diagnosed, with a few small unspecific bilateral nodules in a CT scan of the chest. No abdominal metastases were found. In our interdisciplinary sarcoma board, a neoadjuvant chemotherapy was suggested. In the first two weeks, Cisplatin and Ifosfamid were given, and for the final week one cycle of Doxorubicin with Ifosfamid was administered according to the Euro-BOSS protocol [26]. At a check-up during neoadjuvant therapy, an MRI showed continued growth of the tumor, which made us decide to perform surgery without further systematic therapy.

Figure 3: Secondary osteosarcoma on pre-existing fibrous dysplasia in the third case. In X-ray, no remarkable changes were seen. In PET-CT and MRI, a 10 x 7 x 14 centimetre was found
3. Surgical technique
Surgery was carried out under general anaesthesia and in lateral decubitus position (Figure 4a). Antibiotic prophylaxis with 2g cefazoline was administered. A Kocher-Langenbeck approach was performed to ap-proach the hip joint. A longitudinal incision of 20 to 25cm was centered over the trochanter. The subcuta-neous tissue was sharply dissected to the fascia latae. The interval between Gluteus maximus and medius, also known as the Gibson interval [27,28], was explored and the fascia latae was split longitudinally. The gluteus maximus was retracted posteriorly. This gave access to the posterior part of gluteus medius, which was followed posteriorly to identify the piriformis tendon. An osteotomy of the greater trochanter was performed with an oscillating saw (Figure 4a). The trochanter fragment was extended distally, to improve bony contact area for refixation of the greater trochanter after resection. The gluteus minimus muscle was detached from the joint capsule. The joint capsule was prepared anteriorly to the anterior acetabular rim. Anteriorly, the rectus origin was detached from the anterior inferior iliac spine (AIIS), which gave access to the base of the pubis and the interval between iliopsoas and joint capsule. The pubis was osteotomized with a straight osteotome at its base. Then the external rotators of the hip were dissected off the capsule posteriorly and inferiorly down to the lesser trochanter. After this preparation the entire circumference of the acetabulum, except the caudal part, became visible. To prepare the caudal part, the femur was osteotomized distally of the tumor, respecting wide margins. Then, the iliopsoas muscle was cleared from the femur and the caudal part of the acetabulum was now visible as well (Figure 4b). With an intact hip capsule, the outline of the acetabular osteotomy was marked with a 4.5mm drill and with a straight chisel the osteotomy was performed, keeping a distance of 1 to 1.5cm to the joint surface (Figure 4c). We used the resection margins as defined by Enneking [13] to reach a wide and complete resection. The clinical and radiological results after resection can be seen in figure 5. Because of prior surgeries, in cases two and three the anatomical situations concerning the level of osteotomy of the femur were different, though the resection procedure was similar. After femurosteotomy, the extracapsular hip joint could be removed and the pelvic bone could be inspected for macroscopic adequate margins. For reconstruction of the hip joint we chose in the first and third case to reconstruct the pelvic defect with a Burch-Schneider reinforcement cage (Zimmer ®, Neu-Ulm, Germany). Distally, the pointed tip of the cage was jammed into the remaining ischium, proximally it was attached with screws to the ilium proximal to the AIIS. An allograft femoral head was morselized and positioned around the cage. In both cases we anticipated a higher risk of instability, so we chose to insert a dual mobility acetabular component, which was implanted and fixated with cement. In the femoral shaft, in the first case a modular revision stem (Mathys Ltd., Bettlach, Switzerland) was inserted and the trochanter refixed with 2 screws and cerclage wires. In the third case, a long revision stem (Implantcast, Buxtehude, Germany) was implanted. In the second case, instead of a Burch-Schneider cage, a cone prosthesis (LUMIC Implantcast, Buxtehude, Germany) was used as described elsewhere [29] combined with an revision stem (Implantcast Buxtehude, Germany). Blood loss was in all three cases in line with expectations (1500ml in the first case, 1000ml in the second and 2500ml in the third), and only in the last case a transfusion of 2 packed cells was necessary. Operation time was 5h 21min in the first case, 6h 14min in the second and 7h 25min in the third.
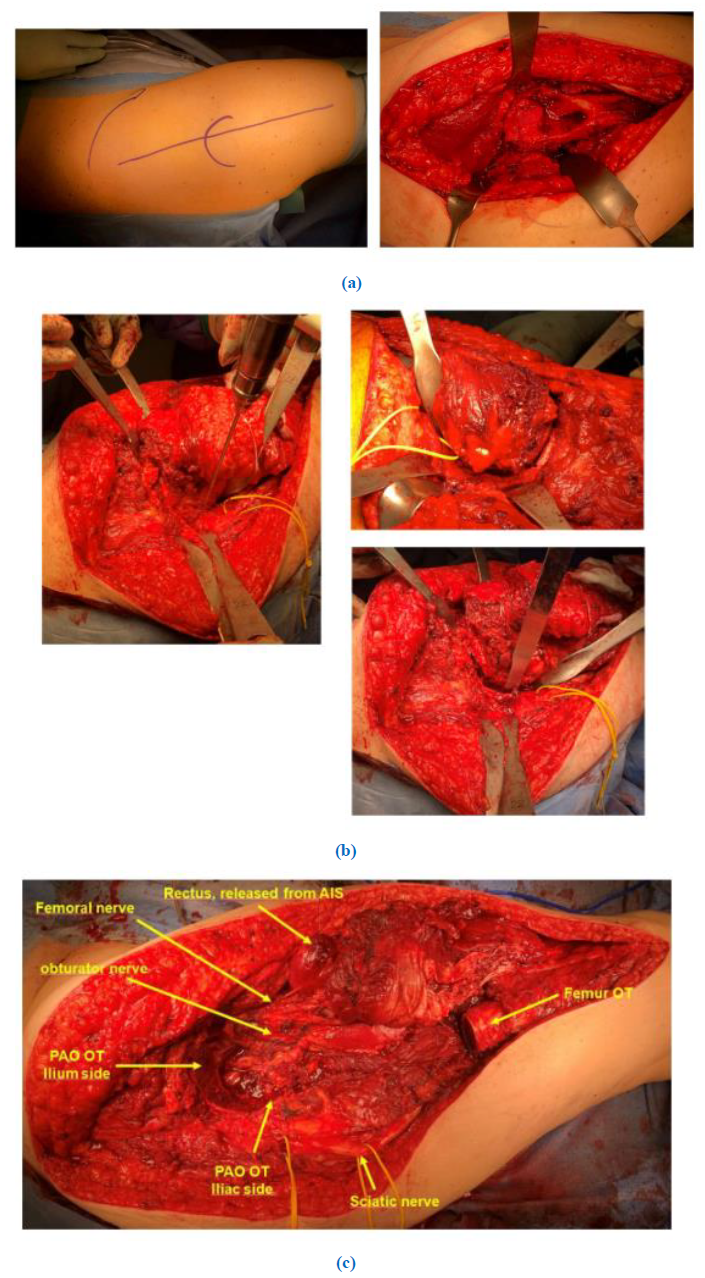
Figure 4 (a): The posterolateral approach, with the trochanter osteotomy to mobilize the femur in the first case.
(b): After femur osteotomy, a mobile hip joint is identified as single structure (case 1, on the left). The periacetabular osteotomy was performed after marking the osteotomy corners with an 4,5 mm drills (case 2 and 3).
(c): After resection of the acetabulum and the proximal femur (case 3).
3.1 Follow-up
For all three patients, only a relatively short term follow up of respectively 12 months, 24 months and 12 months is available. The direct postoperative radiologic images of the patients are shown in figure 6. The first patient was rehabilitated following the standard hip prosthesis protocol, except of a 6 week non weight-bearing schedule in the first 6 weeks. Intensive physiotherapy was conducted to raise muscular strenght. No complications were seen and the mobility of the arthroplastic hip joint was not limited by pain or stiffness. The gait was without problems, as well there was no Trendelenburg sign. After 9 months of follow up, a small pulmonary nodule was found, which was completely resected through a video-assisted thoracoscopic wedge resection. No local recurrence was detected. Functional outcome one year after surgery in this patient was excellent; the MSTS-score (Musculoskeletal Tumor Society-score) was 87%, the TESS (Toronto Extremity Salvage Score) was 80% at the one year follow-up examination. The second patient was last seen 2.5 years after surgery. There were no complications and a good func-tional outcome was seen, except for a persistent weakness of the abductor muscles. The gluteus medius muscle had to be resected to accomplish radical resection margins. However, riding the mountain bike could be performed without problems, and the patient was even thinking of alpine skiing again. No local recurrence or distant metastases were found in this 2.5 year follow up. The functional outcome scores showed moderate to good results; the MSTS score was 57%, TESS 88% at final follow-up 2.5 years post-operative. The third patient developed postoperatively a subcutaneous hematoma, which was treated conservatively, though she needed a blood transfusion. Her range of motion was limited for the first weeks after surgery. In a check up two months postoperative, the hematoma disappeared without intervention as well as the limitation of the functionality of the right hip joint. No local recurrence or distant metastases were observed after one year. Functional outcome after one year postoperative showed a MSTS-score of 53% and a TESS of 72,5%.
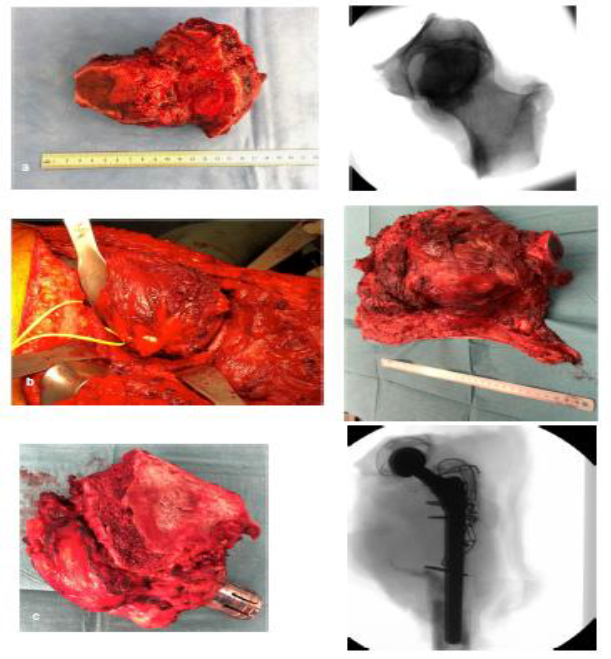
Figure 5: Resection specimens of the three cases, a = case 1, b = case 2 and c = case 3
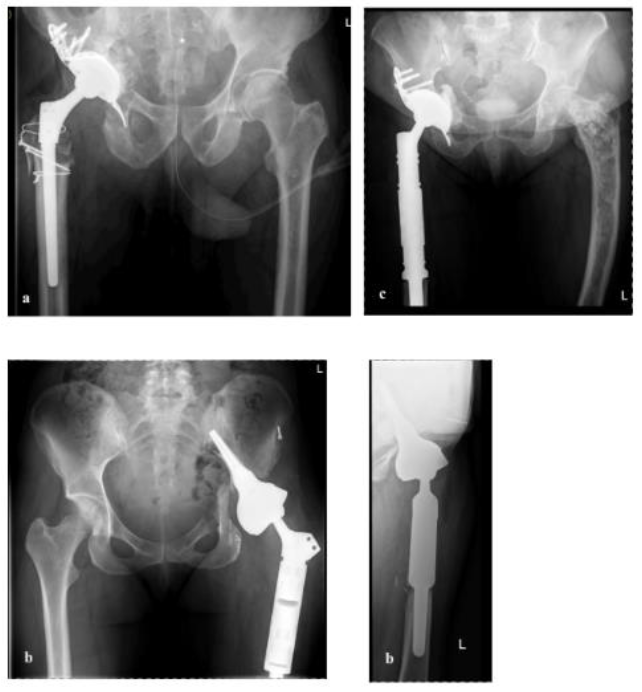
Figure 6: Postoperative images of the three cases. a = first case (a.p. view), b = second case
(a.p and lateral view), c = third case (a.p. view).
4. Discussion
In this paper we present a surgical technique for the resection of malignant intra-articular tumors of the hip joint through a posterior approach with a wide periacetabular extraarticular resection combined with the resection of the proximal femur. So far this technique has not yet gained much attention in the literature [22-24]. One advantage of this technique is that the posterior column remains intact, preserving the stability of the pelvis and therefore enables prosthetic reconstruction with custom implants.
4.1 Discussion of the cases
In these cases, some rare medical conditions were present. An osteolytic bone metastasis from a primary malignant pleural solitary fibrous tumor (SFT) is uncommon, because SFTs normally have low tendency for metastasis [30]. Bone metastases of SFTs are barely described, and when described, the disease is in a late phase [31]. Lung and liver are more common locations for metastasis [32]. In a study by O'Neill, 20 patients with bone metastasis of a primary SFT were described [33]. Nineteen of the 20 subjects (95%) presented with osteolytic bone lesions, although the exact location of metastasis was not mentioned by the authors. In the second and third case, malignant transformation of a synovial chondromatosis into a chondrosar-coma and a fibrous dysplasia into an osteosarcoma were described respectively. According to the literature, these transformations in both synovial chondromatosis as well as in fibrous dysplasia are very rare, but not unobserved [34-37]. In fibrous dysplasia these transformations are rare as well [38], and most of these transformations appear in patients exposed to ionizing radiation [39], which was not the case in our patient.
4.2 Discussion of the literature
In earlier days, extra-articular resections were performed using other approaches such as the T-Incision or combined anterior and posterior approaches [40,41]. Recently, a few case reports presenting an extra-articular resection of the hip joint through a posterolateral approach were published [22-24]. Before these studies were available, the posterior approach was mostly described in pelvic trauma surgery or in tumor surgery where no extraarticular hip resection was performed or pursued [42,43]. Yasuda et al presented a case of a 17 year old girl with an osteoblastic osteosarcoma of the femoral neck. In this case, prior to definitive resection, a pathologic fracture was temporarily fixed by a compression hip screw [22]. After neoadjuvant chemotherapy, the surgical approach for the resection was similar to the one in our cases. In Yasuda’s case though, after the resection of the hip joint, the acetabulum and the femur were pasteurized and re-implanted again. Afterwards, a Kerboull-type plate was used to reconstruct the acetabulum and a total hip arthroplasty was implanted to reconstruct the hip joint [22]. Besides Yasuda's case, two other cases which describe this surgical technique are available. Wells de-scribed a 60 year old male patient with a clear-cell chondrosarcoma of the left hip [23]. In this case, additionally an intraoperative fluoroscopy was performed to guide the periacetabular cuts. After resection, a porous tantalum acetabular shell was used to reconstruct the acetabulum and a regular total hip arthro-plasty could be performed to reconstruct the left hip joint. The last case by Manrique presented a 28 year old male patient with a high grade spindle-cell sarcoma of the left hip as well [24]. For the periacetabular resection, a custom conical cutting guide was produced, so pelvic continuity was maintained and the chance of joint violation was decreased. After resection, the reconstruction was performed with a custom-ized total hip arthroplasty, where the acetabular component was attached with additional screws. In summary, our study in combination with the above mentioned reports show excellent results of extraarticular hip resections in tumor surgery. No infections or other early complications are mentioned, though in tumor surgery high complication rates (around 14%) are observed [44]. In lower extremity tumor surgery, these values have been even higher [44]. This may be an advantage of this approach in com-parison to other approaches. The surgical site is much bigger and therefore the risk of complications may be higher. A possible reason for this advantage may be shorter operation time and less blood loss. Although the other papers presenting this surgical strategy did not present their blood loss and operation time, in our three patients this was at the lower border of mean blood loss in pelvic resections of 3500ml [45]. In the first 30 days, mostly wound problems and infections are the cause for complications. After 30 days, more mechanical complications instead of wound problems and infections are common. Although in our cases, as well as in the reviewed cases in literature, the functional outcome was barely limited, mechanical complications could be a problem after longer follow up [46]. In our cases the functional outcome was acceptable and comparable with available data [25,47]. As well, no mechanical complications were objectified, so it could cautiously be concluded that this approach can be performed safely with low complication rates and promising functional results. Unfortunately, not many studies describing the resection strategy have been published. In the current decade, studies focused more on reconstruction strategies. Two main types of procedures are available to treat pelvic defects after radical tumor resection; (custom) endoprosthesis or osteosynthesis and pelvic reconstructions with autograft bone. In periacetabular resections, a reconstruction with an autograft, for example with fibula and/or pelvic bone block, is rarely used [48] and so most of the described operation techniques include the implantation of different types of prostheses. An example for such prostheses are the saddle prostheses [49], although high risk of complications and poor long-term follow up when using this strategy have been reported [50,51]. Therefore, this is no longer the first choice of treatment. A comparable alternative for saddle prosthesis is the LUMIC prosthesis, which was implanted in the second case that was presented herein. In this prosthesis, a dissatisfying rate of early dislocations (22%) was seen, though mechanical complications and reoperations were relatively low in comparison to other implants [29]. Another option promising positive results for the reconstruction of surgical defects is the use of porous tantalum acetabular implants, which has recently shown good short-term results [2]. These highly porous metal components give a biological solution because it allows osseous ingrowth, even if radiation was performed before surgery [52]. To summarize, multiple types of reconstructions for Type II lesions are described; all of them with their own risks and benefits [53]. However, a golden standard has not been defined until now, most probably because of the heterogeneity in tumor presentation and remaining surgical defects after resection. The posterolateral approach offers the possibility to use all of these reconstruction possibilities, though, and further research has to be conducted to define which treatment option is the best for every specific tumor.
5. Conclusion
Based on the available described cases and our experience, the posterolateral approach for periacetabular extracapsular resection of the hip joint and femur is an excellent and comparatively less invasive way of treating tumors of the proximal femur with growth into the capsular cavity and articular acetabular tumors. Further comparative research is necessary to explore the possibilities and postoperative results of this surgical technique.
Footnote
Conflicts of interest
The authors have no conflicts of interest to declare
Ethical statement
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Grimer RJ, Chandrasekar CR, Carter SR, et al. Hindquarter amputation: is it still needed and what are the outcomes? Bone Joint J 95 (2013): 127-131.
- Abdel MP, Von Roth P, Perry KI, et al. Early Results of Acetabular Reconstruction After Wide Periacetabular Oncologic Resection. J Bone Joint Surg Am 99 (2017): e9.
- Smith-Petersen MN. A new supra-articular subperiosteal approach to the hip joint. JBJS 15 (1917): 15-18.
- Judet R, Judet J, Letournel E. Fractures of the acetabulum: classification and surgical approaches for open reduction. preliminary report. J Bone Joint Surg Am 46 (1964): 1615-1646.
- Letournel E, Judet R. Fractures of the Acetabulum. (2nd edtn), Berlin Germany: Springer-Verlag (1993).
- Hirvensalo E, Lindahl J, Kiljunen V. Modified and new approaches for pelvic and acetabular surgery. Injury 38 (2007): 431-441.
- Cole JD, Bolhofner BR. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach. Description of operative technique and preliminary treatment results. Clin Orthop Relat Res 305 (1994): 112-123.
- Reinert CM, Bosse MJ, Poka A, et al. A modified extensile exposure for the treatment of complex or malunited acetabular fractures. J Bone Joint Surg Am 70 (1988): 329-337.
- Lefaivre KA, Starr AJ, Reinert CM. A modified anterior exposure to the acetabulum for treatment of difficult anterior acetabular fractures. J Orthop Trauma 23 (2009): 370-378.
- Rudert M, Wirtz DC. Limb-sparing surgical techniques in malignant tumors. Operative Orthopadie und Traumatologie. Germany 24 (2012): 173.
- Guo X, Li X, Liu T, e al. Pasteurized autograft reconstruction after resection of periacetabular malignant bone tumours. World J Surg Oncol 15 (2017): 13-18.
- Kurze C, Keel MJB, Kollár A, et al. The pararectus approach-a versatile option in pelvic musculoskeletal tumor surgery. J Orthop Surg Res 14 (2019): 232.
- Enneking WF, Dunham WK. Resection and reconstruction for primary neoplasms involving the innominate bone. J Bone Joint Surg Am 60 (1978): 731-746.
- Bickels J, Malawer M. Musculoskeletal Cancer Surgery: Treatment of Sarcomas and Allied Diseases. Boston, MA: Kluwer Academic Publishers 12 (2001): 405-414.
- Mankin HJ, Hornicek FJ. Internal hemipelvectomy for the management of pelvic sarcomas. Surg Oncol Clin N Am 14 (2005): 381-396.
- Steel HH. Partial or complete resection of the hemipelvis. An alternative to hindquarter amputation for periacetabular chondrosarcoma of the pelvis. J Bone Joint Surg Am 60 (1978): 719-730.
- Lackman RD, Crawford EA, Hosalkar HS, et al. Internal hemipelvectomy for pelvic sarcomas using a T-incision surgical approach. Clin Orthop Relat Res 467 (2009): 2677-2684.
- Karakousis CP. Abdominoinguinal incision and other incisions in the resection of pelvic tumors. Surg Oncol. 9 (2000): 83-90.
- Judet R. Pathologic dislocations of the hip. Presse Med 62 (1954): 83-85.
- Peters RM, Van Beers LWAH, Van Steenbergen LN, et al. Similar superior patient-reported outcome measures for anterior and posterolateral approaches after total hip arthroplasty: postoperative patient-reported outcome measure improvement after 3 months in 12,774 primary total hip arthroplasties using the Ant. J Arthroplasty 33 (2018):1786-1793.
- Hadjicostas PT, Thielemann FW. The use of trochanteric slide osteotomy in the treatment of displaced acetabular fractures. Injury 39 (2008): 907-913.
- Yasuda T, Hori T, Suzuki K, et al. Extracapsular wide resection of a femoral neck osteosarcoma and its reconstruction using a pasteurized autograft-prosthesis composite: A case report. Oncol Lett 6 (2013): 1147-1151.
- Wells JE, Clohisy JC, O’Keefe RJ. Treatment of intra-articular hip malignancy with extra-articular resection, preservation of the acetabular columns, and total hip arthroplasty 4 (2018): 431-435.
- Manrique J, Schiffman CJ, Chan AD, et al. Extra-Articular hip resection and reconstruction with custom acetabular resection guide and implants in a case of high-grade spindle cell sarcoma of the proximal femur: A case report. JBJS Case Connect 10 (2020).
- Fuchs B, Hoekzema N, Larson DR, et al. Osteosarcoma of the pelvis: Outcome analysis of surgical treatment. Clin Orthop Relat Res 467 (2009): 510-518.
- Ferrari S, Bielack SS, Smeland S, et al. EURO-B.O.S.S.: A European study on chemotherapy in bone-sarcoma patients aged over 40: Outcome in primary high-grade osteosarcoma. Tumori 104 (2018): 30-36.
- Gibson A. Posterior exposure of the hip joint. J Bone Joint Surg Br 32 (1950): 183-186.
- Espinosa N, Rothenfluh DA, Beck M, et al. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. J Bone Joint Surg Am 88 (2006): 925-935.
- Bus MPA, Szafranski A, Sellevold S, et al. LUMiC(®) Endoprosthetic Reconstruction After Periacetabular Tumor Resection: Short-term Results. Clin Orthop Relat Res 475 (2017): 686-695.
- Colia V, Provenzano S, Morosi C, et al. Solitary fibrous tumour presenting with a single bone metastasis: report of six cases and literature review. Clin Sarcoma Res 6 (2016): 16.
- Baldi GG, Stacchiotti S, Mauro V, et al. Solitary fibrous tumor of all sites: outcome of late recurrences in 14 patients. Clin Sarcoma Res 3 (2013): 4.
- Casali PG, Abecassis N, Aro HT, et al. Soft tissue and visceral sarcomas: ESMO-EURACAN Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol Off J Eur Soc Med Oncol 29 (2018): 51-67.
- O’Neill AC, Tirumani SH, Do WS, et al. Metastatic Patterns of Solitary Fibrous Tumors: A Single-Institution Experience. AJR Am J Roentgenol 208 (2017): 2-9.
- Ng VY, Louie P, Punt S, et al. Malignant Transformation of Synovial Chondromatosis: A Systematic Review. Open Orthop J 11 (2017): 517-524.
- Boyce AM. Fibrous Dysplasia. In: Feingold KR, Anawalt B, Boyce A, Chrousos G, Dungan K, Grossman A, et al., editors. South Dartmouth (MA); 2000.
- Schwartz DT, Alpert M. The malignant transformation of fibrous dysplasia. Am J Med Sci 247 (1964): 1-20.
- Sun TT, Tao XF, Shi HM. Spontaneous osteosarcoma in craniomaxillofacial fibrous dysplasia: clinical and computed tomographic features in 8 cases. Oral Surg Oral Med Oral Pathol Oral Radiol 118 (2014): e24-31.
- Okuda M, Kobayashi S, Gabata T, et al. Undifferentiated pleomorphic sarcoma arising in a fibrous dysplasia confirmed by GNAS mutation analysis: A Case Report. JBJS Case Connect 10 (2020): 12-15.
- Hansen MR, Moffat JC. Osteosarcoma of the skull base after radiation therapy in a patient with McCune-Albright Syndrome: Case Report. Official journal of North American Skull Base Society 13 (2003): 79-83.
- Li D, Xie L, Guo W, et al. Extra-articular resection is a limb-salvage option for sarcoma involving the hip joint. Int Orthop 42 (2018): 695-703.
- Rüdiger HA, Dora C, Bode-Lesniewska B, et al. Extra-articular resection of the hip with a posterior column-preserving technique for treatment of an intra-articular malignant lesion. A report of two cases. J Bone Joint Surg Am 87 (2005): 2768-2774.
- Vielgut I, Sadoghi P, Gregori M, et al. The modified Harrington procedure for metastatic periacetabular bone destruction. Int Orthop 37 (2013): 1981-1985.
- Nilsson J, Gustafson P, Fornander P, et al. The Harrington reconstruction for advanced periacetabular metastatic destruction: good outcome in 32 patients. Acta Orthop Scand 71 (2000): 591-596.
- Gallaway KE, Ahn J, Callan AK. Thirty-Day outcomes after surgery for primary sarcomas of the extremities: An Analysis of the NSQIP Database. J Oncol 12 (2020): 7282846.
- Tang X, Guo W, Yang R, et al. Evaluation of blood loss during limb salvage surgery for pelvic tumours. Int Orthop 33 (2009): 751-756.
- Puchner SE, Funovics PT, Böhler C, et al. Oncological and surgical outcome after treatment of pelvic sarcomas. PLoS One 12 (2017): e0172203.
- Sherman CE, O’Connor MI, Sim FH. Survival, local recurrence, and function after pelvic limb salvage at 23 to 38 years of followup. Clin Orthop Relat Res 470 (2012): 712-727.
- Tang X, Guo W, Yang R, et al. Acetabular reconstruction with femoral head autograft after intraarticular resection of periacetabular tumors is durable at short-term followup. Clin Orthop Relat Res 475 (2017): 3060-3070.
- Renard AJ, Veth RP, Schreuder HW, et al. The saddle prosthesis in pelvic primary and secondary musculoskeletal tumors: functional results at several postoperative intervals. Arch Orthop Trauma Surg 120 (2000): 188-194.
- Jansen JA, Van de Sande MAJ, Dijkstra PDS. Poor long-term clinical results of saddle prosthesis after resection of periacetabular tumors. Clin Orthop Relat Res 471 (2013): 324-331.
- Donati D, D’Apote G, Boschi M, et al. Clinical and functional outcomes of the saddle prosthesis. J Orthop Traumatol Off J Ital Soc Orthop Traumatol 13 (2012): 79-88.
- Khan FA, Rose PS, Yanagisawa M, et al. Surgical technique: Porous tantalum reconstruction for destructive nonprimary periacetabular tumors. Clin Orthop Relat Res 470 (2012): 594-601.
- Brown TS, Salib CG, Rose PS, et al. Reconstruction of the hip after resection of periacetabular oncological lesions: a systematic review. Bone Joint J 12 (2018): 22-30.
