Interdisciplinary Management of an Endo-Perio Lesion in a Chronic Hepatitis Patient-A Case Report
Article Information
Khyati Chandra, Gayathri GV*, Sartaz Rahman, Mehta DS
Department of Periodontics, Bapuji Dental College and Hospital, Karnataka, India
*Corresponding Author: Gayathri GV, Department of Periodontics, Bapuji Dental College and Hospital, Davangere, 577004, Karnataka, India
Received: 04 August 2019; Accepted: 06 September 2019; Published: 16 September 2019
Citation: Chandra K, Gayathri GV, Rahman S, Mehta DS. Interdisciplinary Management of an Endo-Perio Lesion in a Chronic Hepatitis Patient-A Case Report. Dental Research and Oral Health 2 (2019): 032-037.
View / Download Pdf Share at FacebookAbstract
Management of Endo-perio lesions have always been a dilemma to the dental clinician. In such conditions, apicetomy is usually the treatment of choice when conventional endodontic treatment fails. In the present case scenario, a 42 year old male patient reported with pain and pus exudate in upper left anterior region of the jaw since three months who had a history of trauma and RCT in relation to 23 and 24 five months back. The medical history of the patient revealed that he was a chronic hepatitis patient who had undergone treatment for the same a year ago. A physician was consulted and an interdisciplinary approach was planned. Apicetomy was performed under strict aseptic condition and the osseous defect was treated with Novabone putty, collagen membrane and PRF coagulum. One year follow up revealed, defect fill gain in clinical attachment, improved gingival biotype and increased width of attached gingiva. Hence, it can be said that the synergistic effect of various regenerative materials along with periapical root sealing brings about clinical and radiographic improvement in endo-perio lesions present in chronic hepatitis patients.
Keywords
Endo-perio; Apicetomy; Chronic hepatitis; Tissue regeneration
Endo-perio articles, Apicetomy articles, Chronic hepatitis articles, Tissue regeneration articles
Endo-perio articles Endo-perio Research articles Endo-perio review articles Endo-perio PubMed articles Endo-perio PubMed Central articles Endo-perio 2023 articles Endo-perio 2024 articles Endo-perio Scopus articles Endo-perio impact factor journals Endo-perio Scopus journals Endo-perio PubMed journals Endo-perio medical journals Endo-perio free journals Endo-perio best journals Endo-perio top journals Endo-perio free medical journals Endo-perio famous journals Endo-perio Google Scholar indexed journals Apicetomy articles Apicetomy Research articles Apicetomy review articles Apicetomy PubMed articles Apicetomy PubMed Central articles Apicetomy 2023 articles Apicetomy 2024 articles Apicetomy Scopus articles Apicetomy impact factor journals Apicetomy Scopus journals Apicetomy PubMed journals Apicetomy medical journals Apicetomy free journals Apicetomy best journals Apicetomy top journals Apicetomy free medical journals Apicetomy famous journals Apicetomy Google Scholar indexed journals Chronic hepatitis articles Chronic hepatitis Research articles Chronic hepatitis review articles Chronic hepatitis PubMed articles Chronic hepatitis PubMed Central articles Chronic hepatitis 2023 articles Chronic hepatitis 2024 articles Chronic hepatitis Scopus articles Chronic hepatitis impact factor journals Chronic hepatitis Scopus journals Chronic hepatitis PubMed journals Chronic hepatitis medical journals Chronic hepatitis free journals Chronic hepatitis best journals Chronic hepatitis top journals Chronic hepatitis free medical journals Chronic hepatitis famous journals Chronic hepatitis Google Scholar indexed journals Tissue regeneration articles Tissue regeneration Research articles Tissue regeneration review articles Tissue regeneration PubMed articles Tissue regeneration PubMed Central articles Tissue regeneration 2023 articles Tissue regeneration 2024 articles Tissue regeneration Scopus articles Tissue regeneration impact factor journals Tissue regeneration Scopus journals Tissue regeneration PubMed journals Tissue regeneration medical journals Tissue regeneration free journals Tissue regeneration best journals Tissue regeneration top journals Tissue regeneration free medical journals Tissue regeneration famous journals Tissue regeneration Google Scholar indexed journals periodontal articles periodontal Research articles periodontal review articles periodontal PubMed articles periodontal PubMed Central articles periodontal 2023 articles periodontal 2024 articles periodontal Scopus articles periodontal impact factor journals periodontal Scopus journals periodontal PubMed journals periodontal medical journals periodontal free journals periodontal best journals periodontal top journals periodontal free medical journals periodontal famous journals periodontal Google Scholar indexed journals endodontic therapy articles endodontic therapy Research articles endodontic therapy review articles endodontic therapy PubMed articles endodontic therapy PubMed Central articles endodontic therapy 2023 articles endodontic therapy 2024 articles endodontic therapy Scopus articles endodontic therapy impact factor journals endodontic therapy Scopus journals endodontic therapy PubMed journals endodontic therapy medical journals endodontic therapy free journals endodontic therapy best journals endodontic therapy top journals endodontic therapy free medical journals endodontic therapy famous journals endodontic therapy Google Scholar indexed journals periodontist articles periodontist Research articles periodontist review articles periodontist PubMed articles periodontist PubMed Central articles periodontist 2023 articles periodontist 2024 articles periodontist Scopus articles periodontist impact factor journals periodontist Scopus journals periodontist PubMed journals periodontist medical journals periodontist free journals periodontist best journals periodontist top journals periodontist free medical journals periodontist famous journals periodontist Google Scholar indexed journals osteoblasts articles osteoblasts Research articles osteoblasts review articles osteoblasts PubMed articles osteoblasts PubMed Central articles osteoblasts 2023 articles osteoblasts 2024 articles osteoblasts Scopus articles osteoblasts impact factor journals osteoblasts Scopus journals osteoblasts PubMed journals osteoblasts medical journals osteoblasts free journals osteoblasts best journals osteoblasts top journals osteoblasts free medical journals osteoblasts famous journals osteoblasts Google Scholar indexed journals
Article Details
Clinical Relevance to Interdisciplinary Dentistry
- The Case report depicts an endo-perio lesion in a chronic hepatitis patient which has been managed using a multidisciplinary
- Apicectomy was carried out by an endodontist followed by regenerative therapy performed by the placement of bone graft and PRF membrane by a periodontist keeping in mind the safety protocols as suggested by a
- This collaborative effort has yielded excellent results in tissue regeneration despite the presence of systemic
1. Introduction
The endodontic and periodontal tissues share an embryological, biological and functional concordance. The relationship between periodontal and pulpal disease was first described by Simring and Goldberg in 1964 [1]. Both the tissues are ectomesenchymal in origin and this embryologic association serves as a conduit for anatomical intercommunications between the pulp and periodontium. Hence, inflammatory components in the pulp may lead to widespread destruction of the periodontium and periodontal breakdown may cause pulpitis [1]. These lesions have always presented themselves as perplex situations for the dental clinician.When periodontal pockets are associated with an endodontically compromised teeth, the clinical situation complicates the outcome of the conventional endodontic therapy. Periodontal surgical intervention is indicated, when the ultimate goal of therapy is to eliminate the periapical lesion and allow soft and hard tissue regeneration [3].
According to various studies, paraendodontic surgeries give a success rate of 91.6%, while failure rate is shown to be 4.7% [4]. However, its prognosis can be influenced by several factors such as the presence of systemic conditions such as diabetes, hypertension, chronic bacterial and viral infections like HIV, Chronic hepatitis etc. Among various infectious ailments, chronic viral hepatitis is distinct, as the virus harbours in hepatocytes, leading to necroinflammatory liver disease. This causes altered immunoinflammatory status and impaired wound healing. Quite often, hepatitis results in depressed plasma levels of coagulation factors that need a careful evaluation of hemostasis prior to treatment [5].
The present case report depicts a clinical scenario, in which apicectomy and regenerative periodontal surgery was performed in a patient with chronic hepatitis following conventional endodontic treatment failure. One year postoperative re-evaluation showed affirmative tissue regeneration.
2. Background
A 42 year-old male patient reported to the Department of Periodontology, Bapuji Dental College and Hospital witha chief complaint of pain and pus discharge through gums of the left upper anterior teeth. Patient gave a history of trauma to the upper anterior teeth 1 year back. He had visited a private dental clinic 5 months back for pain and swelling and had undergone root canal treatment for the same. Medical history revealed that he had undergone treatment for hepatitis B one year back and was currently not on any medication.
Intra oral examination revealed that the patient’s oral hygiene maintenance was good (OHIS score-0.4 ). Gingiva in relation to 23 and 24 was erythematous and edematous. There was purulent discharge from the sulcular area, grade 1 mobility, probing depth of 8- 10 mm and vertical tenderness on percussion was present with respect to 23 and 24. Gingival recession of 2 mm was present in relation to 23 and gingival margin was there at the level of Cementoenamel junction (CEJ) in relation to 24. IOPA revealed interdental bone loss till apical one third & existence of residual periapical radiolucency in relation to the RCT treated teeth. The case was diagnosed as primary endodontic lesion with secondary periodontic involvement. Hence it was decided to manage the case with an interdisciplinary approach in association with a physician, an endodontist and a periodontist.Treatment protocol was explained and a written consent was obtained from the patient.Due to his medical history, routine blood investigations were advised and presence of HBsAg was detected. The patient was confirmed to be in an inactive carrier state of Hepatitis after evaluating results of Serum HBV DNA (Hepatitis B Virus Deoxy ribonucleic acid) test, ALT/AST (Alanine transaminase/ Aspartate transaminase) levels and Liver biopsy test. Other investigations including Complete Blood Count, Partial Thromboplastin Time (PTT), International Normalized Ratios, bleeding time, liver function tests, platelet count etc were found to be within normal range. Following physician’s consent, non surgical periodontal treatment was initiated and surgical treatment was scheduled after 3 weeks.
3. Procedure
After administration of local anesthesia(2 % Lidocaine 1: 80,000 adrenaline), a full thickness mucoperiosteal flap was raised by extending vertical incisions from mesial aspect of 23 to mesial aspect of 25 using #15 Bard Parker (B.P) blade and periosteal elevator. Apical curettage was performed. 3.0 mm of the root apex was surgically resected in relation to 23 and 24 using a surgical bur. Ultrasonic tips were used to make a3.0-mm deep retro preparation. After hemostasis was achieved, retropreparation was disinfected and dried. The retrogradefilling was done with Mineral Trioxide Aggregate (MTA fillapex, Dentsply, Germany). Bone Putty (Novabone, UK) was then placed to fill the bony defects. This was succeeded by the placement of collagen and A-PRF membrane on the surgical site. The flap was then repositioned and secured with interrupted sutures by using 4-0 black braided silk (Figure 1).
Amoxicillin 500 mg t.i.d for 5 days, Ibuprofen 400mg t.i.d for 3 days and 0.2% chlorhexidine mouthwash was prescribed postoperatively. Suture removal was done 10 days after the procedure. Patient was comfortable and the operated site revealed uneventful tissue healing on 10th day.
One year post-operative IOPAR, showed increased radiopacity in perapical and interdental area (Figure 1, 7a & 7b). There was also an improvement in the gingival biotype, clinical attachment level and width of attached gingiva (Figure 2, Table 2).
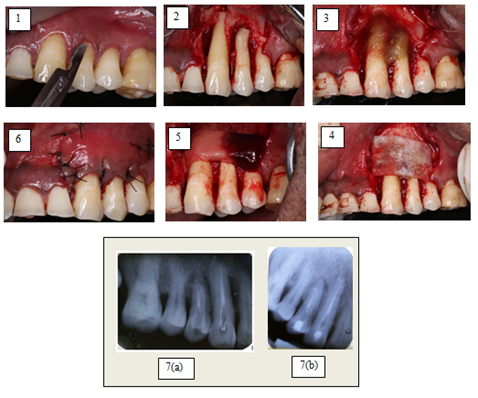
Figure 1: (1) Incision given; (2) Apicetomy cut given; (3) Nova bone putty placed; (4) Collagen membrane placed; (5) PRF membrane placed; (6) Sutures placed; (7a) Immediate post-op intra-oral periapical radiograph; (7b) Intra-oral periapical radiograph after 1 year.
|
Local Anaesthetics : Lidocaine Mepivacaine Prilocaine Bupivacaine |
|
Analgesics: Aspirin Codein Ibuprofen Acetaminophen |
|
Sedatives Diazepam** Barbiturates** |
|
Antibiotics Ampicillin Tetracycline Metronidazole*** Vancomycin*** |
|
Legend *limit dose if severe liver disease or haemostatic abnormalities present **limit dose if severe liver disease or encephalopathy is present *** avoid if liver disease is present |
Table 1: Drugs used in liver disease.
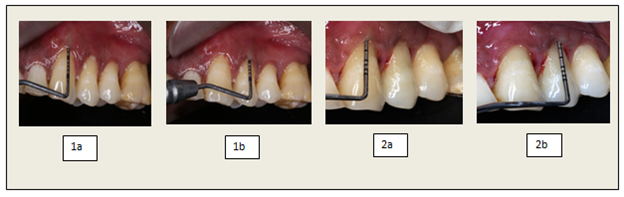
Figure 2: (1a, 1b) Pre-operative probing depth; (2a, 2b) Post-operative probing depth.
|
Tooth number |
|||
|
23 |
24 |
||
|
Probing Depth (PD) |
Pre-op Post-op |
8mm 3mm |
10mm 3mm |
|
Clinical Attachment Loss (CAL) |
Pre-op Post-op |
10mm 5mm |
10mm 3mm |
|
Gingival Biotype |
Pre-op Post-op |
0.5mm 1mm |
0.5mm 1.5mm |
|
Width of the Attached gingiva |
Pre-op Post-op |
1mm 3mm |
0mm 1mm |
Table 2: Clinical parameters for assessing improvements in the affected teeth
4. Discussion
There are many implications for a patient suffering from a liver disorder, when they have to undergo a dental treatment procedure. Thorough medical and dental histories are essential before proceeding with treatment of any sort. It is prudent to discuss the details of the disease with a treating physician, in order to provide the patient with a dental treatment plan that is safe and appropriate for them [5]. The given patient was confirmed to be in an inactive HBsAg carrier state as determined by the following:
- HbsAg positive > 6 months
- HBeAg negative, anti-HBe positive
- Serum HBV DNA <105 copies/mL
- Persistently normal ALT/AST levels
- Liver biopsy confirms absence of significant hepatitis (necroinflammatory score <4). Although the patient was in an inactive carrier state, the risk of transmission cannot be eliminated. Thus the operating clinicians were vaccinated and CDC guidelines were strictly followed and customized drugs (Table 1) were used [5]. Apicectomy can be indicated in several clinical situations, namely persistence of periapical lesion following conventional RCT, perforations, fractured instruments and presence of external resorption. In this case, the apical portion of the root was cut 45º angle to the long axis of the tooth. This inclination degree was appropriate to allow total root surface exposure thus facilitating operative procedures [6].
Novabone has a property of releasing Ca, P and Si ions which stimulates osteoblasts.As ion release progresses, nova bone is transformed into an increasingly porous scaffold with increased surface area, that boosts the natural healing process [7].
Guided tissue regeneration (GTR) membranes have been known to encourage regeneration by preventing epithelial cell migration and facilitate faster wound maturation. They also act as lattice for migrating periodontal ligament fibroblasts thus making them exemplary regenerative materials [8].
PRF, a second generation platelet concentrate releases platelet cytokines and growth factors which particularly favours cell migration and serves as a matrix to accelerate wound healing [9]. Therefore the placement of collagen membrane followed by the use of PRF has been propagated. As the PRF membrane degenerates within 7 to 11 days with release of incorporated growth factors. Since guided periodontal regeneration warrants at least a period of 4 to 6 weeks of epithelial cell exclusion hence use of PRF alone as a barrier membrane may be insufficient [10]. Thus the combination of both the collagen and PRF membrane form an ideal barrier membrane in regenerative therapy.
5. Conclusion
This case report depicts an encouraging milieu in which an interdisciplinary approach with the teamwork of an endodontist, periodontist and physician has brought about both clinical and radiographic improvement in endo-perio lesions present in chronic hepatitis patients.
Conflict of interest
Nil
References
- Simring M, Goldberg M. The pulpal pocket approach: Retrograde periodontitis. J Periodontol 35 (1964): 22-48.
- Mazur B, Massler M. Influence of periodontal disease on the dental pulp. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 17 (1964): 592-603.
- Simon JH, Glick DH, Frank AL. The relationship of endodontic periodontic lesions. J Periodontol 43 (1972): 202-208.
- Tsesis I, Faivishevsky V, Kfir A, et al. Outcome of surgical endodontic treatment performedby a modern technique: a meta-analysis of literature. J Endod 35 (2009): 1505-1511.
- Golla K, Epstein JB, Cabay RJ. Liver disease: current perspectives on medical and dental management. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 98 (2004): 516-521.
- Kim S, Kratchman S. Modern endodontic surgery concepts and practice: a review. J Endod 32 (2006): 601-623.
- Hattar S, Berdal A, Asselin A, et al. Behaviour of moderately differentiated osteoblast-like cells cultured in contact with bioactive glasses. Eur Cell Mater 31 (2002): 61-69.
- Bottino MC, Thomas V, Schmidt G, et al. Recent advances in the development of GTR/GBR membranes for periodontal regeneration-a materials perspective. Dent Mater 28 (2012): 703-721.
- Dohan DM, Choukroun J, Diss A, et al. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part I: technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101 (2006): 37-44.
- Panda S, Sankari M, Satpathy A, et al. Adjunctive effect of autologus platelet-rich fibrin to barrier membrane in the treatment of periodontal intrabony defects. J Craniofac 27 (2016): 691-696.
