Innovative Treatment in Grade 3 B Open Comminuted Tibial Fractures Using Hybrid Fixation (Khemka Technique)
Article Information
Sunil Khemka, Subeer Mukherjee, Ambrish Verma, Pritam Agrawal, Ram Khemka, Pradeep Patel*
Department of Orthopaedics, Shree Narayana Hospital Raipur, Chhatisgarh, India
*Corresponding Author: Pradeep Patel, Department of Orthopaedics, Shree Narayana Hospital Raipur, Chhatisgarh, India.
Received: 19 May 2025; Accepted: 26 May 2025; Published: 13 June 2025
Citation: Sunil Khemka, Subeer Mukherjee, Ambrish Verma, Pritam Agrawal, Ram Khemka, Pradeep Patel. Innovative treatment in Grade 3 B open Comminuted Tibial Fractures using Hybrid Fixation (Khemka Technique). Journal of Orthopedics and Sports Medicine. 7 (2025): 262-268.
View / Download Pdf Share at FacebookAbstract
Background: The incidence of open comminuted tibia fractures is on an increasing trend proportionate to an increase in high velocity motor vehicle accidents. These fractures are challenging to treat and usually give unfavorable results. Treatment protocols with regard to such fractures are still evolving and there is no widely acceptable consensus.
Aims and objectives: We share a series of Gustilo Anderson III B comminuted tibial fractures in which we used Ender’s Nail and LRS as a hybrid definitive fixation solution for skeletal stabilization.
Materials and methods: A prospective study was carried out from Jan, 2014 to Dec, 2023 with 90 patients in our series. The clinical and radiological evaluation was done at the end of the treatment with ASAMI Bony and Functional scoring system.
Results: Among 90 cases, we achieved excellent and good bony results in 93.3% cases as per ASAMI score. Similarly, functional results were excellent and good in 95.6% cases. Bone grafting was required in 20 patients, musculocutaneous flap in 24 and SSG in 26 cases. In 4 cases of infected non-union, implant removal, intramedullary bone grafting and antibiotic beads with revision fixation was done.
Conclusion: Advantage of this system is a very stable construct which is less cumbersome and less technically demanding procedure unlike Ilizarov fixation while avoiding the disadvantages usually associated with unilateral AO type fixators. Our technique is based on four cardinal principles of achieving a very stable construct, early mobilization, aggressive infection management with early and repeated aggressive wound debridement and soft tissue coverage as soon as possible.
Keywords
Compound Tibia fracture; Gustilo Anderson III B; LRS; Enders nail
Article Details
1. Introduction
The incidence of open comminuted tibia fracture is increasing steadily, which is commonly attributed to the increase in road traffic accidents [1] (>80% cases). Although many aspects of open long bone fracture management are widely accepted, there remains a lack of consensus regarding factors predictive of fracture complications such as infection, non-union or delayed soft tissue healing [2]. Urgent surgical debridement within 6 hours has been considered essential for preventing deep infection and ensuing non-union in open long bone fractures, but more recent studies have questioned this association [3,4]. Non-union and subsequent reoperations have considerable implications for patients’ functional capacity and quality of life, as well as health care resource demands [5].
These patients usually undergo multiple operations to achieve infection control, soft tissue coverage and bony union like serial debridement, skin grafting, flaps and bone grafting. Sometimes, getting end results like chronic osteomyelitis, Sagittal plane deformities, shortening, loss of joint ROM, sarcopenia and osteopenia due to disuse are not uncommon. Patient satisfaction and compliance also falls with the prolonged duration of treatment and multiple procedures [6,7]. Therefore, these situations require a high degree of skill and a fair amount of experience to manage effectively.
Traditional method of management of comminuted open fracture is by External fixation until soft tissue healing and subsequent definitive fixation by nailing / plating once infection subsides and soft tissue coverage is achieved [8]. Our method of using Enders nail with LRS can be considered as definitive method of management for open comminuted tibia fracture. The advantage of this combination is that the intramedullary Enders nails produce good axial alignment and rotational stability by virtue of their three-point fixation and the LRS provides additional rotational stability as well as angular stability [9] (Table 1).
The aim of this study is to assess the efficacy, bony union, joint ROM and other complications encountered in the management of Grade III B open tibial fractures with the use of Enders nail along with LRS.
2. Materials and Methods
The study was conducted in 90 patients having modified Gustilo Anderson type 3B open fracture who fulfilled the inclusion criteria. These cases were treated using Enders nail and LRS over a period of 9 years. Soft tissue involvement was classified as per AO Soft tissue classification for open skin lesions (Table 2) and bony involvement according to AO classification (Table 3). The study was conducted at a Tertiary level Trauma Centre from 1st January 2014 to 31st December 2023. The study protocol was approved by Ethical committee of the Institute.
2.1 Inclusion Criteria
- All patients with open comminuted fracture of tibia with Gustilo Anderson type 3B.
2.2 Exclusion Criteria
- Patients with closed fracture
- Open grade 1, 2, 3A & 3C fracture
- Patients with associated significant head, abdomen or chest injury which would delay treatment and/or post op mobilization
The clinical and radiological evaluation was done at the time of presentation and at specific intervals (1st month then 3 monthly for 1 year followed by 6 monthly review). At each follow up, the patients were evaluated clinically and radiologically for signs of bony union, deformity, limb length discrepancy, adjoining joint ROM and signs of pin tract infection. Bony union and functional scoring were evaluated using ASAMI scoring system at the end of follow up. Mean follow up period of the study was 15.46 months (Range: 10.1-18.2 months).
After initial management in the emergency department and assessment of associated and other life-threatening injuries, the limb was splinted and then initial radiographs were taken to assess the bony injury. Patients were taken for the procedure with minimum delay, preferably within 24 hrs.
2.3 Operative procedure
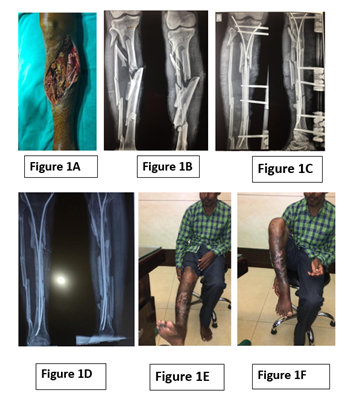
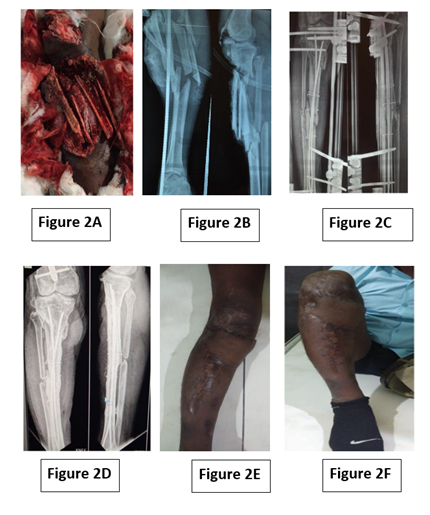
In the operating room, under appropriate anaesthesia and a tourniquet was used wherever feasible. Thorough irrigation and debridement of the wound was done bony fragments were retained in situ unless visibly and grossly contaminated which could not be cleaned adequately (Figure 1). Then, either 2 or 4 (depending upon canal diameter) appropriately sized stainless steel Enders nails were inserted from medial and lateral tibia plateau after reduction of the fracture usually under direct vision and major fragments were aligned (Figure 1C and 2C). If required, due to minimal proximal bone stock, Ender’s nails were inserted in retrograde fashion. Enders nail provides the axial alignment and length thereby helping in reduction of the comminuted fracture fragments. After that, antero-medial / Lateral LRS is applied in standard fashion depending on location of wound and need of subsequent soft tissue coverage procedure. Wound was primarily closed whenever feasible with preference given to covering the bones with minimal tension. Postoperatively Dressing of Open wounds was done using Eusol solution and also at appropriate intervals of 12-24 hours thereafter according to need. Further depending upon wound condition musculocutaneous flap/SSG was performed. bone grafting was done at later stage.
3. Results
We performed this procedure in 90 patients of comminuted open grade 3b fracture tibia (Figure 1A, 1B, Figure 2A, 2B). 38 patients had ipsilateral fractures of lower limb. This included fracture shaft of femur (16 cases), fracture Intercondylar femur (2 case), fracture Tibial plateau (6 cases), fracture Patella (4 cases) and crush injury foot (10 cases). The age distribution of patients was between 18-60 years with a mean age of 34.2 years. 80 patients were male and 10 patients were female. The most common mode of trauma was road traffic accidents (Table 1). Soft tissue involvement and bony fracture pattern data has been depicted (Table 2 and 3).
|
Variables |
Description |
|
|
1 |
Mean age |
34.2 yrs (18-64yrs) |
|
2 |
Sex |
M/F = 80/10 |
|
3 |
Associated fractures |
1) Fracture shaft femur-16 |
|
2) Intercondylar femur fracture-2 |
||
|
3) Fracture patella-4 |
||
|
4) Fracture tibial plateau-6 |
||
|
5) Crush injury foot-10 |
||
|
4 |
No of surgeries |
3.6 times (range: 2-4) |
|
5 |
Mean follow up |
15.46 months (range: 10.1-18.2 months) |
|
6 |
Level of fracture |
Proximal Third - 48, Mid Third-34, Lower Third-8 |
|
7 |
Secondary procedures |
1) Bone grafting-20 |
|
2) Flap-24 |
||
|
3) STSG-26 |
||
|
4) Supplementary LRS -2 |
Table 1: Demographic profile.
We could close the wound and achieve bony coverage in 40 of our patients. 24 cases required primary flap coverage and 26 cases were managed with skin grafting. We have used supplemantory LRS for augmentation in 2 of our cases, which had severe communition and splintering. Bone grafting was done in 20 of our cases. This was done within 6weeks- 3months period when radiological union was determined to be not progressing. We achieved union in 86 (95.5%) of our patients. Rest of the four patients with non-union were managed with revision fixation which also united subsequently. During the follow up duration, 10 patients (11.1%) developed infection. Out of these, in 6 patients, since bony union was achieved, they were managed with implant removal, debridement of sinus and placement of stimulant antibiotics beads (Biocomposites) as per culture and sensitivity report. In the other 4 patients, revision fixation with intramedullary bone grafting and stimulant antibiotic beads (Biocomposites) application was done. No patients developed pin loosening.
|
Category |
Description |
No of patients |
|
1I0 1 |
Skin breakage from inside out |
0 |
|
1I0 2 |
Skin breakage from outside in < 5 cm, contused edges. |
0 |
|
1I0 3 |
Skin breakage from outside in >5 cm, increased contusion, devitalized edges. |
28 |
|
1I0 4 |
Considerable, full thickness contusion, abrasion, extensive open degloving, skin loss. |
52 |
|
1I0 5 |
Extensive degloving. |
10 |
Table 2: Classification of soft tissue injury (AO classification).
|
Classification |
No. of patients |
|
41A3 |
42 |
|
42B3 |
22 |
|
42C3 |
12 |
|
43A3 |
8 |
|
41C2 |
6 |
Table 3: AO Classification for bony injury
Knee range of motion (active/assisted/CPM) and weight bearing (full/partial) were started within first week depending upon patient comfort. Patients with ipsilateral limb injury had delayed weight bearing and mobilization. All patients achieved good knee range of movement (120º-155º) by the end of the study period. Similarly, ankle range of motion was also attained in the satisfactory range (20º dorsiflexion and 40º plantarflexion). These were results on final follow up examination (Figure 1 E, F, 2 E, F).
Limb length discrepancy was encountered in 6 patients with shortening of 2.5 cm and all were satisfied with shoe raise and declined limb lengthening procedure. Deformity in sagittal and coronal plane was measured. Majority (77.5%) of the patients had neutral alignment. Malalignment was encountered in 22.5% of patients (varus/valgus) which was in the acceptable range (<5º). None of the patients had refractures. There was slight limp in 10 (11%) of our patients.
Among 90 cases, bony results as per ASAMI score were excellent in 88.9% (n=80) good in 4.4% (n=4) fair in 2.2% (n=2) and poor in 4.4% (n=4) of patients. Functional results were excellent in 88.9% (n=80) good in 6.7% (n=6) and poor in 4.4%(n=4) of patients (Table 4).
|
Bony Results |
No of Patients |
|
|
Excellent |
Union, no infection, deformity<70, limb length discrepancy <2.5 cms |
80 |
|
Good |
Union + any two of the following: No infection, deformity<70, limb length discrepancy <2.5 cms |
4 |
|
Fair |
Union + any one of the following: No infection, deformity<70, limb length discrepancy <2.5 cms |
2 |
|
Poor |
Nonunion/refracture/union+infection+deformity>70 + limb length discrepancy > 2.5 cm |
4 |
|
Functional Results |
||
|
Excellent |
Active, no limp, minimum stiffness (loss of <15 knee extension/< 15 dorsiflexion of the ankle), no reflex sympathetic dystrophy, insignificant pain |
80 |
|
Good |
Active with one or two of the following: Limp, stiffness, RSD, significant pain |
6 |
|
Fair |
Active with three or all of the following: Limp, stiffness, RSD, Significant pain |
0 |
|
Poor |
Inactive (unemployment or inability to return to daily activities because of injury) |
4 |
|
Failure |
Amputation |
0 |
Table 4: ASAMI Scoring.
Union was complete on an average by 10.5 months (Range: 9-12 months) in cases which united. Enders nail and LRS external fixator was kept for a period of 12-14 months (in cases which united) depending on the rate of union, after which the LRS fixator was removed (Figure 1D and 2D). Enders nails were removed after approximately 2 years on average.
In cases with LRS and Enders nail, Patient satisfaction was assessed by ASAMI Functional score where majority of patients were highly satisfied with the ease of early mobilization due to the very stable construct. The average hospital stay was 17 days and patients were able to resume their preinjury work in an average of 60 days (45-70 days)
4. Discussion
Open comminuted tibial fractures with massive soft tissue injury have become a complex problem for all trauma surgeons [10]. The goal of the trauma surgeon must be saving the life, saving the limb, prevent infection & restore function of limb [11]. Although various treatment approaches are available for the treatment of such type of fractures still this fracture remains one of the unsolved dilemmas in orthopaedic trauma.
The conventional modalities of treatment for these fractures like external fixators have a high rate of complications including shortening, soft tissue healing problem, multiple surgery, longer hospitalization and high rates of gap nonunion and malunion [9,10,12,13]. Although many studies are available on the use of LRS or Enders nail alone, literature on use of combined enders nail and LRS for management of open comminuted tibia fractures is still sparse to the best of our knowledge.
Treatment of Grade 3B open fractures with delayed primary intramedullary nailing or secondary nailing has a significant high infection rate [14-16]. According to Yokoyama et al, treatment of 3B and 3C fracture with nailing is risky due to high infection and nonunion in 20.3% [17]. Nambi et al. [18] in their study to evaluate single stage definitive management of Open grade 3 A/B fractures of Tibia with IM Nailing and fasciocutaneous flap reported the incidence of deep infection requiring major secondary intervention in 9% and the rate of major and minor soft tissue complications in 9% and 14% cases respectively. These two complications were encountered in our study with significantly less frequency. The dual modality of fixation proposed in our study provided a mechanically stable construct. This allowed for a proper soft tissue healing with decreased rate of infection. Also, for interlocking nailing in comminuted fractures, adequate length of proximal and distal fragment for fixations may not be available. Nork et al stressed upon difficulty associated with intramedullary nailing of proximal tibial fractures because of mismatch between voluminous proximal tibia and medullary implant. This often leads to coronal and sagittal malalignment [19-21]. On the contrary, Ender’s nail is ideally suited for intramedullary fixation when minimal proximal or distal bone stock is present which can be further augmented with LRS to enhance stability.
External fixators are preferred initial modality for 3A/3B fractures because of low infection rate and allow soft tissue procedure but require prolonged period of rest and need for multiple staged surgery for final fixation. Staged treatment of grade 3A/3B open tibial fractures (comprising External fixators in stage one and definitive fixation with Nailing/Plating in second stage) has its disadvantages as stated in various studies [22]. It prolongs hospital stay and external fixators as such lead to delayed union, mal union and gap non-union. Fractures in which early soft tissue coverage is not performed are prone to additional soft tissue damage and hospital acquired infection. Adequate and early soft tissue coverage is one of the primary prerequisites for proper fracture healing.
Wani et al. [23] evaluated the result of early fixation of open tibial fractures with Illizarov ring fixator [23]. Patients were managed by emergency debridement followed by Illizarov ring fixator application after 3-5 days. They reported good rate of union in all of the fractures. This modality was associated with several complications which although were mild. Pin tract infection was observed in 32 patients (77 pin sites). Others included decreased knee flexion, extensor lag, pain at fracture site and restricted ankle range of motion. This study did not encounter restricted ROM at knee and ankle and extensor lag at initial stages since we were able to attain good ROM at knee and ankle from early post operative period. This was possible since our construct was uniplanar (allowing range of motion at knee>90°) with additional intramedullary fixation.
Ilizarov fixator is a good choice for this type of fractures but it does not allow flap rotation surgeries or skin grafting without removal of frame and are cumbersome both for the patients as well as the surgeon and are technically very demanding procedures [24-30]. Lakhani et al. [29] compared the result of Mono Rail fixator system with Illizarov in management of bone loss following open fractures. They also concluded that Illizarov application is associated with more discomfort due to heavy apparatus, joint stiffness and persistent pain as compared to LRS frame.
Kim et al. [31] in their study on 34 patients with open proximal tibial fracture treated by MIPO reported satisfactory fracture and soft tissue healing along with good functional scores. But they encountered deep infection in 16.7% of their cases along with 46.2% infection in Grade 3 fractures. Also, this modality may not be feasible in fractures of middle or lower third tibia with gross comminution.
Rajasekaran et al. [32] in their study on early versus delayed closure of wound in open fractures recommended early closure of wound if it fulfilled their defined conditions. In our study, we followed the same guideline and achieved primary closure in 44.4% (40) of our cases. Rest of the cases required either skin grafting or flap coverage.
Tekin et al. [33] in their study on management of open grade 3 tibial fractures with Limb reconstruction system (LRS) in single sitting reported union in 96% of cases at mean interval of 20.4 ± 4 weeks (range: 16-24). They did not report shortening or deformity in any of their cases. There was no loss of Ankle and knee range of motion at final follow up after fixator removal. As compared, in our study, union was achieved in 95.5% of cases (86) at an average of 10.5 months (range 9-12 months). Range of movement at knee and ankle was achieved in the functional range in all the patients at final follow up. Erturk et al. [34] conducted a prospective comparative study in open tibial fractures in which they divided their patients into those with only external fixation and those with external fixation and IM fixation with elastic nails. They concluded that patients with additional intramedullary fixation showed decreased duration of external fixation, decreased time to union, better bony and functional results and decreased pin tract infection. These results corroborated with the findings of our study also.
Pandey et al. [35] in their study of 30 patients on management of open tibia fracture with elastic nailing and external fixator in single stage reported union in all patients but delayed union was observed in 5/30 patients. The average union time is 23.83+_4.47 weeks (range, 18–32 weeks). The main complication mentioned in this study was pin track infection, which occupied 6/30 cases. They concluded outcome of elastic nailing along with external fixator, as a definitive intra- and extramedullary fixation technique, which was effective in treatment of open tibial fractures.
Roy et al. [36] in their study on treatment of compound tibia fractures treated with external fixator combined with tens nail found union rate of 65% and non-union in 15% of their patients.65% patients could achieve good limb alignment whereas moderate in 30%, and poor in 5%. pin tract infections reported in 1 case. Weight bearing was achieved in on average of 4.83 months.
The complications associated with primary nailing or simple external fixators like shortening, soft tissue problem, multiple surgeries, prolonged hospital stay can be avoided with the use of Enders and LRS. Also, staged procedures for definitive fixation are avoided. Hence, the beauty of this combination of Enders nail with LRS is that it provides definitive fixation with immediate full weight bearing postoperatively and almost anatomical reduction which is not possible by other modes of fixation with unhindered access to the limb for soft tissue procedures. Patients are quite satisfied in terms of limb length, alignment and mobility of adjacent joints with this modality. We have named this technique as “Khemka Technique” of fixation of compound tibial fracture by hybrid fixation (ENDERS and LRS).
5. Conclusion
Enders nail with LRS can be considered as a definitive method of fixation. This method allows full weight bearing immediate postoperatively like intramedullary nailing with added advantage of less infection risk. With Enders and LRS, intramedullary fixation is possible even with minimal proximal/distal bone stock and can be used retrograde as well. The length and alignment of tibia is well maintained and addition of LRS supplements the stability of the fixation. As it's a unilateral frame, it allows flap rotation/ skin grafting. The stable construct, in turn, facilitates proper soft tissue healing and decreases chances of deep infection. The author advocates stable fixation of Open grade 3B fractures by Enders nail with LRS.
Our study had certain limitations. Firstly, since our study did not have a control group, we could not compare our results with other modalities of treatment. Secondly, the technique described in our study required meticulous debridement and soft tissue reconstruction which was performed by the senior author. The results may not be reproducible by orthopaedic residents and Fellowship surgeons. Further, multicentric studies are warranted which include various modalities of management of this cohort of fractures and their results be compared.
Our study has two main strengths. First, it was a prospective study in which the inclusion and exclusion criteria of the patients were predetermined prior to study and a uniform treatment modality was followed in the study. Second, it is a large consecutive series of patients treated at a single centre by an experienced Orthopaedic team.
References
- Patil MY, Gupta SM, Kurapati SKC, et al. Definitive Management of Open Tibia Fractures Using Limb Reconstruction System. Journal of Clinical and Diagnostic Research; 10 (2016): RC01-RC04.
- Struijs PA, Poolman RW, Bhandari M. Infected nonunion of the long bones. Journal of Orthopaedic Trauma 21 (2007): 507-511.
- Maurer RC, Dillin L. Multistaged surgical management of posttraumatic segmental tibial bone loss. Clinical Orthopaedics and Related Research 216 (1987):162 70.
- Keating JF, Simpson AH, Robinson CM. The management of fractures with bone loss. J Bone Joint Surgery Br 87 (2005): 142-50.
- Westgeest J. Weber D, Dulai SK, et al. Factors associated with development of nonunion or delayed healing after an open long bone fracture: a prospective cohort study of 736 subjects. Journal of Orthopaedic Trauma 30 (2016): 149-55.
- Dendrinos GK, Konto S, Lyritsis E. Use of Ilizarov technique for treatment of nonunion of tibia associated with infection. Journal of Bone Joint Surgery Br 77 (1995): 835-46.
- Motsitsi NS. Management of infected nonunion of long bone: The last decade (1996-2006). Injury 39 (2008): 155-60.
- Blachut PA, Meek RN, O’Brien PJ. External fixation and delayed intramedullary nailing of open fractures of the tibial shaft. A sequential protocol. J Bone Joint Surg Am 72 (1990): 729-35.
- Watson JT, Anders M, Moed BR. Management strategies for bone loss in tibial shaft fractures.ClincalOrthopaedics Related Research 315 (1995): 138-52.
- Maurer RC, DillinL. Multistaged surgical management of posttraumatic segmental tibial bone loss.ClincalOrthopaedics Related Research 216 (1987): 162-70.
- Azar FM, Canale ST, Beaty JH. Fractures and dislocations in adults. In: Campbell’s Operative Orthopaedics. Volume 3. 11th Philadelhia: Mosby.
- Keating JF, Simpson AH, Robinson CM. The management of fractures with bone loss. J Bone Joint Surg Br 87 (2005): 142-50.
- Cole JD, Ansel LJ. Schwartzberg R. A sequential protocol for managementof severe open tibial fractures. ClinOrthopRelatRes 315 (1995): 84-103.
- Blachut PA, Meek RN, O’Brien PJ. External fixation and delayed intramedullary nailing of open fractures of the tibial shaft. A sequential protocol. J Bone Joint Surg Am 72 (1990): 729-35.
- Reuss BL, Cole JD. Effect of delayed treatment on open tibial shaft fractures. Am J Orthop (Belle Mead NJ) 36 (2007): 215-20.
- Maurer DJ, Merkow RL, Gustilo RB. Infection after intramedullary nailing of severe open tibial fractures initially treated with external fixation. J Bone Joint Surg Am 71 (1989): 835-8.
- Yokoyama K, Itoman M, Uchino M, et al. Immediate versus delayed intramedullary nailing for open fractures of the tibial shaft: a multivariate analysis of factors affecting deep infection and fracture healing. Indian J Orthop 42 (2008): 410-19.
- Nambi GI, Salunke AA, Thirumalaisamy SG, et al. Single stage management of Gustilo type III A/B tibia fractures: Fixed with nail & covered with fasciocutaneous flap. Chinese Journal of Traumatology 20 (2017): 99-102
- Nork SE, Barei DP, Schildhauer TA, et al. Intramedullary nailing of proximal quarter tibial fractures. J Orthop Trauma 20 (2006): 523-8.
- Lindvall E, Sanders R, Dipasquale T. et al. Intramedullary nailing versus percutaneous locked plating of extra-articular proximal tibial fractures: comparison of 56 cases. J Orthop Trauma 23 (2009): 485-92.
- Ricci WM, O’Boyle M, Borrelli J, et al. Fractures of the proximal third of the tibial shaft treated with intramedullary nails and blocking screws. J Orthop Trauma 15 (2001): 264-70.
- Tielinen L, Lindahl J E, Tukiainen EJ. Acute unreamed intramedullary nailing and soft tissue reconstruction with muscle flaps for the treatment of severe open tibial shaft fractures. Injury, Int J Care Injured 38 (2007): 906-912
- Wani N, Baba A, Kangoo K, et al. Role of early Ilizarov ring fixator in the definitive management of type II, IIIA and IIIB open tibial shaft fractures. International Orthopaedics (SICOT) 35 (2011): 915-923.
- Krappinger D, Irenberger A, Zegg M, et al. Treatment of large posttraumatic tibial bone defects using the Ilizarov method: A subjective outcome assessment. Arch Orthop Trauma Surg 133 (2013): 789-95.
- Pavolini B, Maritato M, Turelli L, et al. The Ilizarov fixator in trauma: A 10- year experience. J OrthopSci 5 (2000): 108-13.
- García-Cimbrelo E, Olsen B, Ruiz- Yagüe M, et al. Ilizarov technique. Results and difficulties. Clin Orthop Relat Res 283 (1992): 116-23.
- Agarwal S, Agarwal R, Jain UK, et al. Management of soft tissue problems in leg trauma in conjunction with application of the Ilizarov fixator assembly. PlastReconstrSurg 107 (2001): 1732-8.
- Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res 250 (1990): 81-104.
- Lakhani A, Singh D, Singh R. Outcome of rail fixator system in reconstructing bone gap. Indian Journal of Orthopaedics 48 (2014): 612-16
- Sanders DW, Galpin RD, Hosseini M, et al. Morbidity resulting from the treatment of tibialnonunion with the Ilizarov frame. Can J Surg 45 (2002): 196-200.
- Kim JW. Oh CW, Jung WJ, et al. Minimally Invasive Plate Osteosynthesis for Open Fractures of the Proximal Tibia. Clinics in Orthopedic Surgery 4 (2012): 313-20.
- Rajasekaran S. Early versus delayed closure of open fractures. Injury. International Journal of Care of Injured 38 (2007): 890-895.
- Tekin AC, Saygili MS, Adas M, et al. Outcome of Type 3 Open TibialDiaphyseal Fractures Managed with a Limb Reconstruction System: Analysis of a 49-Patient Cohort. Medical principles and Practice 25 (2016): 270-275.
- Erturk C, Altay MA, Binge A, et al. Do additional intramedullary elastic nails improve the results of definitive treatment with external fixation of open tibia fractures? A prospective comparative study. Orthopaedics & Traumatology: Surgery & Research 99 (2013): 208-215.
- Pandey KK, Naik S, Vidyarthi A. To evaluate the outcome of elastic nailing along with external fixator in open tibia fractures. Int J of Adv Res 10 (2022): 1018-1024.
- Roy S, Salunkhe PM, Patidar B, et al. Treatment of compound diaphyseal tibia fractures treated with external fixator combined with intramedullary tens nail for limited internal fixation as definitive procedure. J Popl Ther Clin Pharmacol 30 (2023): 914-20.