Impact of Sleep Disruptions on the Mental Health of Atrial Fibrillation Inpatients: A Cross-Sectional Study
Article Information
Lixing Hu1, Xiaotong Ding1, Min Tang1*
1Center of Arrhythmia, Fuwai Hospital, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences, Peking Union Medical College, Beijing 100037, China
*Corresponding Author: Min Tang, Center of Arrhythmia, Fuwai Hospital, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences, Peking Union Medical College, Beijing 100037, China
Received: 28 July 2023; Accepted: 09 August 2023; Published: 30 August 2023
Citation: Lixing Hu, Xiaotong Ding, Min Tang. Impact of Sleep Disruptions on the Mental Health of Atrial Fibrillation Inpatients: A Cross-Sectional Study. Journal of Psychiatry and Psychiatric Disorders. 7 (2023): 147-155.
View / Download Pdf Share at FacebookAbstract
Objectives: To evaluate the interactions between anxiety, depression and sleep attributes in atrial fibrillation inpatients of a single tertiary center in China to improve identification of patients who require additional psychological care.
Methods: We retrospectively enrolled 332 atrial fibrillation inpatients and evaluated their psychological and sleep status with the Zung Self- Rating Anxiety Scale (SAS), Zung Self-Rating Depression Scale (SDS), and Pittsburgh Sleep Quality Index (PSQI), respectively. Potential risk factors for anxiety and depression were analyzed by multivariate logistic regression. Odds ratios (OR) for risk of poor sleep quality were adjusted by age and gender in patients with different psychological statuses (anxiety only, depression only, combined anxiety and depression).
Results: Participants with an average age of 58.6±10.5 years, and 67.8% males were involved in the study. Patients with anxiety and depression accounted for 21.1 and 34.0%, respectively. Potential risk factors for anxiety were female (P = 0.045) and poor sleep quality (P = 0.001); for depression were obesity (P = 0.033) and poor sleep quality (P<0.001). The likelihood of experiencing sleep disturbances was 3.69 times greater in patients suffering from both anxiety and depression (OR: 3.69; 95% confidence interval [CI]: 1.94–7.01; P<0.001), 2.14 times greater in depressed patients (OR: 2.14; 95% CI: 1.16–3.96; P = 0.016), and 2.06 times greater in anxious patients (OR=2.06; 95%CI: 0.72-5.94; P = 0.180).
Conclusions: Psychological disturbances are prevalent among Chinese inpatients with atrial fibrillation, especially among females and obese individuals. There is an association between anxiety and depression respectively, with sleep disorders. Persistent sleep disruption may be a significant risk factor for psychological disorders, and patients suffering from anxiety and depression have the highest risk for sleep disruption.
Keywords
Anxiety, Depression, Atrial fibrillation, Psychological disturbance, Sleep quality
Anxiety articles; Depression articles; Atrial fibrillation articles; Psychological disturbance articles; Sleep quality articles
Anxiety articles Anxiety Research articles Anxiety review articles Anxiety PubMed articles Anxiety PubMed Central articles Anxiety 2023 articles Anxiety 2024 articles Anxiety Scopus articles Anxiety impact factor journals Anxiety Scopus journals Anxiety PubMed journals Anxiety medical journals Anxiety free journals Anxiety best journals Anxiety top journals Anxiety free medical journals Anxiety famous journals Anxiety Google Scholar indexed journals Depression articles Depression Research articles Depression review articles Depression PubMed articles Depression PubMed Central articles Depression 2023 articles Depression 2024 articles Depression Scopus articles Depression impact factor journals Depression Scopus journals Depression PubMed journals Depression medical journals Depression free journals Depression best journals Depression top journals Depression free medical journals Depression famous journals Depression Google Scholar indexed journals Atrial fibrillation articles Atrial fibrillation Research articles Atrial fibrillation review articles Atrial fibrillation PubMed articles Atrial fibrillation PubMed Central articles Atrial fibrillation 2023 articles Atrial fibrillation 2024 articles Atrial fibrillation Scopus articles Atrial fibrillation impact factor journals Atrial fibrillation Scopus journals Atrial fibrillation PubMed journals Atrial fibrillation medical journals Atrial fibrillation free journals Atrial fibrillation best journals Atrial fibrillation top journals Atrial fibrillation free medical journals Atrial fibrillation famous journals Atrial fibrillation Google Scholar indexed journals Psychological disturbance articles Psychological disturbance Research articles Psychological disturbance review articles Psychological disturbance PubMed articles Psychological disturbance PubMed Central articles Psychological disturbance 2023 articles Psychological disturbance 2024 articles Psychological disturbance Scopus articles Psychological disturbance impact factor journals Psychological disturbance Scopus journals Psychological disturbance PubMed journals Psychological disturbance medical journals Psychological disturbance free journals Psychological disturbance best journals Psychological disturbance top journals Psychological disturbance free medical journals Psychological disturbance famous journals Psychological disturbance Google Scholar indexed journals Sleep quality articles Sleep quality Research articles Sleep quality review articles Sleep quality PubMed articles Sleep quality PubMed Central articles Sleep quality 2023 articles Sleep quality 2024 articles Sleep quality Scopus articles Sleep quality impact factor journals Sleep quality Scopus journals Sleep quality PubMed journals Sleep quality medical journals Sleep quality free journals Sleep quality best journals Sleep quality top journals Sleep quality free medical journals Sleep quality famous journals Sleep quality Google Scholar indexed journals depression articles depression Research articles depression review articles depression PubMed articles depression PubMed Central articles depression 2023 articles depression 2024 articles depression Scopus articles depression impact factor journals depression Scopus journals depression PubMed journals depression medical journals depression free journals depression best journals depression top journals depression free medical journals depression famous journals depression Google Scholar indexed journals Zung Self- Rating Anxiety Scale articles Zung Self- Rating Anxiety Scale Research articles Zung Self- Rating Anxiety Scale review articles Zung Self- Rating Anxiety Scale PubMed articles Zung Self- Rating Anxiety Scale PubMed Central articles Zung Self- Rating Anxiety Scale 2023 articles Zung Self- Rating Anxiety Scale 2024 articles Zung Self- Rating Anxiety Scale Scopus articles Zung Self- Rating Anxiety Scale impact factor journals Zung Self- Rating Anxiety Scale Scopus journals Zung Self- Rating Anxiety Scale PubMed journals Zung Self- Rating Anxiety Scale medical journals Zung Self- Rating Anxiety Scale free journals Zung Self- Rating Anxiety Scale best journals Zung Self- Rating Anxiety Scale top journals Zung Self- Rating Anxiety Scale free medical journals Zung Self- Rating Anxiety Scale famous journals Zung Self- Rating Anxiety Scale Google Scholar indexed journals Zung Self-Rating Depression Scale articles Zung Self-Rating Depression Scale Research articles Zung Self-Rating Depression Scale review articles Zung Self-Rating Depression Scale PubMed articles Zung Self-Rating Depression Scale PubMed Central articles Zung Self-Rating Depression Scale 2023 articles Zung Self-Rating Depression Scale 2024 articles Zung Self-Rating Depression Scale Scopus articles Zung Self-Rating Depression Scale impact factor journals Zung Self-Rating Depression Scale Scopus journals Zung Self-Rating Depression Scale PubMed journals Zung Self-Rating Depression Scale medical journals Zung Self-Rating Depression Scale free journals Zung Self-Rating Depression Scale best journals Zung Self-Rating Depression Scale top journals Zung Self-Rating Depression Scale free medical journals Zung Self-Rating Depression Scale famous journals Zung Self-Rating Depression Scale Google Scholar indexed journals Pittsburgh Sleep Quality Index articles Pittsburgh Sleep Quality Index Research articles Pittsburgh Sleep Quality Index review articles Pittsburgh Sleep Quality Index PubMed articles Pittsburgh Sleep Quality Index PubMed Central articles Pittsburgh Sleep Quality Index 2023 articles Pittsburgh Sleep Quality Index 2024 articles Pittsburgh Sleep Quality Index Scopus articles Pittsburgh Sleep Quality Index impact factor journals Pittsburgh Sleep Quality Index Scopus journals Pittsburgh Sleep Quality Index PubMed journals Pittsburgh Sleep Quality Index medical journals Pittsburgh Sleep Quality Index free journals Pittsburgh Sleep Quality Index best journals Pittsburgh Sleep Quality Index top journals Pittsburgh Sleep Quality Index free medical journals Pittsburgh Sleep Quality Index famous journals Pittsburgh Sleep Quality Index Google Scholar indexed journals Odds ratios articles Odds ratios Research articles Odds ratios review articles Odds ratios PubMed articles Odds ratios PubMed Central articles Odds ratios 2023 articles Odds ratios 2024 articles Odds ratios Scopus articles Odds ratios impact factor journals Odds ratios Scopus journals Odds ratios PubMed journals Odds ratios medical journals Odds ratios free journals Odds ratios best journals Odds ratios top journals Odds ratios free medical journals Odds ratios famous journals Odds ratios Google Scholar indexed journalsArticle Details
1. Introduction
Atrial fibrillation (AF) has been suggested to be the new cardiovascular epidemic of the 21st century. Among Chinese adults, the standardized prevalence of AF is approximately 1.6% [1]. Atrial fibrillation can significantly increase the risk of heart failure, stroke, and dementia; not only compromising patients’ quality of life, but also increasing risk of early death [2]. Thus, AF is now a major cardiovascular disease that seriously threatens human health. With emergence of increasing medical evidence and the development of new technologies, knowledge of AF and its clinical management are constantly being updated. However, prevention of disease relapse and improvement of prognosis remain challenging for clinical research.
Depression and anxiety are common psychological disturbances that contribute to the rising incidences of morbidity and mortality, reducing quality of life, and increasing economic burden [3, 4]. The impact of psychological health on cardiovascular diseases is increasingly being recognized and coexistence of anxiety and depression has been associated with increased therapeutic resistance [5, 6]. Indeed, current international guidelines recommend assessing co-occurring anxiety and depression as risk factors for AF [7]. Thus, psycho-cardiology is an emerging discipline that is opening up new directions for investigation and intervention. Besides, accumulating evidences based on community studies have emphasized the significance of healthy sleep patterns in psychological health [8-12]. Our previous study in arrhythmia patients showed that psychological disruptions are associated with poor sleep quality [13]. Atrial fibrillation has also been associated with sleep quality, with healthy sleep habits associated with reduced risk of AF [14], and persistent sleep interruption predictive of AF in several different populations, both before and after correction for potential confounders such as obstructive sleep apnea [15]. However, psychological disturbances and the contribution of sleep quality to mental health in AF patients are less well understood. Thus, we seek to evaluate the psychological status of hospitalized patients with AF and the relationship with poor sleep quality. Understanding these complex relationships will lead to novel strategies to improve patient management and enhance quality of life for AF patients.
2. Materials and Methods
2.1 Patient Profile
Patients hospitalized at the Arrhythmia Center (Fuwai Hospital, China) between October and December 2019 were recruited for this cross-sectional study with the following inclusion criteria: (a) primary diagnosis of AF with clinically stable symptoms; (b) age ≥ 18 years; (c) fluency in reading and writing Chinese. The exclusion criteria were: (a) impairments in consciousness, cognition, language, vision, hearing or comprehension; (b) history of drug abuse or physical trauma; (c) inability to complete the evaluation scales due to severe symptoms; (d) refusal to participate. This study conforms with the World Medical Association's Declaration of Helsinki (1989) and was approved by the ethics committee of Fuwai Hospital (approval number 2016-780). Informed consent was provided by all participants.
2.2 Data Collection
Baseline characteristics (age; gender; height; weight; marital status) and clinical characteristics (comorbidities; duration of disease; type of AF) of participants were independently recorded and reviewed by two cardiologists. Any disagreements between them were resolved by re-evaluation of the hospital charts.
The psychological status of participants were assessed by two questionnaires, the Zung Self-Rating Anxiety Scale (SAS) and the Zung Self-Rating Depression Scale (SDS) with 20 questions each. For both questionnaires, scores ≥ 50 indicate anxiety or depression, respectively. Anxiety and depression levels were classified as mild (50 – 59), moderate (60 – 69), and severe (> 70) [16]. The validity of the SAS and SDS have been demonstrated in patients with anxiety and depression previously [17], and the Chinese editions have been used in Chinese populations with reliable results [18, 19]. The Pittsburgh sleep quality index (PSQI) with 19 questions in seven dimensions (subjective sleep quality; sleep latency; duration; efficiency; sleep disturbances; daytime dysfunction; use of hypnotic drug) was used to gauge participants’ sleep quality in the preceding month. Summation of the scores from each section provides the total score, with lower scores indicating healthier sleep. The Chinese edition of the PSQI is validated for the Chinese population [13, 20]. Good reliability is supported by consistent high scores for the Cronbach’s α coefficient (0.84), the odd and even split half reliability test (0.87), and the test/retest at week two (0.82). In the current research, an overall PSQI score >7 indicates poor sleep quality [20]. The questionnaires were completed by all participants during their hospital stay. Results were calculated and documented by two experienced psychologists. Data collectors and supervisors were trained for one week prior to experimentation to ensure data quality.
2.3 Statistical Analysis
The statistical package, SPSS™ Statistics 26 (Chicago, USA) was used for all analyses. Parametric data with normal distribution are presented as mean ± standard deviation (x-±s), while non-parametric data are presented as median with inter-quartile range [M (IQR)]. Nominal variables are expressed as absolute and relative frequencies. The parametric and non-parametric variables were analyzed with the Student’s t-test and the Mann–Whitney U-test, respectively. Interactions between various factors the levels of anxiety and depression were analyzed by univariate analyses (χ2 test or t-test) or multivariate logistic regression. Only factors with P<0.20 or show clinical significance were selected for multivariate logistic regression to avoid missing clinically significant findings. Levels of anxiety and depression between different groups were analyzed by Fisher’s exact test, with multiple comparisons in cases of statistical differences. Statistical significance is defined as P<0.05. The adjusted odds ratios (OR) and 95% confidence intervals was calculated for the logistic regression of sleep quality in patients with different mental states (anxiety only, depression only, combined anxiety and depression). Potential correlations between anxiety and depression was examined using the Spearman’s rank correlation analysis.
3. Results
3.1 Patient Characteristics
This study enrolled 332 hospitalized AF patients with an average age of 58.6±10.5 years (Table 1). Among them, 92 (27.7%) were over 65 years, and 225 (67.8%) were male. Diseases that were recorded in this cohort include hypertension (167/332; 50.3%), hyperlipidemia (192/332; 57.8%), diabetes mellitus (66/332; 19.9%), coronary artery disease (67/332; 20.2%), bradycardia (60/332; 18.1%), and obesity (75/332; 22.6%). Majority of patients (228/332; 68.7%), had live with their condition for less than five years. Two types of atrial fibrillation were detected: paroxysmal (213/332; 64.4%) and persistent (118/332; 35.6%). The median PSQI score is 6.0 with an interquartile range of 6.0; 34.0% (113/332) of patients had poor sleep quality (PSQI>7).
Table 1: Clinical characteristics of atrial fibrillation patients
*: P<0.20; SAS (Zung Self-Rating Anxiety Scale); SDS (Zung Self-Rating Depression Scale); PSQI (Pittsburgh Sleep Quality Index); M(IQR) [median (inter-quartile range)]; AF (Atrial Fibrillation).
3.2 Overall Psychological Disturbances in Atrial Fibrillation Inpatients
Evaluation of the level of anxiety in patient with the SAS show that 21.1% (70/332) of all patients were defined as being anxious, with 15.1% (50/332) showing mild anxiety, 5.1% (17/332) showing moderate anxiety, and 0.9% (3/332) showing severe anxiety (Table 2). For the paroxysmal AF group, 14.6% (31/213) of patients were mildly anxious, 5.2% (11/213) moderately, and 0.9% (2/213) severely anxious. The persistent AF group also showed a similar trend, with 15.3% (18/118), 5.1% (6/118), and 0.8% (1/118) of patients demonstrating mild, moderate and severe anxiety, respectively. Data for the two AF groups did not differ significantly (P = 0.998). Evaluation of depression status with the SDS showed that 34.0% (113/332) of all patients were depressed, with 21.4% (71/332) demonstrating mild depression, 11.4% (38/332) demonstrating moderate depression, and 1.2% (4/332) in the severely depressed category. For the paroxysmal AF group, mild, moderate and severe depression was present in 22.5% (48/213), 11.7% (25/213), and 1.4% (3/213) of patients, respectively. Similar rates were observed in the persistent AF group, with mild depression in 18.6% (22/118) of patients, moderate depression in 11.0% (13/118), and severe depression in 0.8% (1/118) of patients. The two AF groups did not differ significantly (P = 0.804). The overall SAS and SDS scores are 41.0 (13.0) and 44.0 (17.0) [M(IQR)], respectively. Spearman’s analysis showed moderate correlation between the SAS and SDS scores (rs = 0.673, P < 0.001).
Table 2: Anxiety and depression levels in patients with persistent and paroxysmal atrial fibrillation
|
Total |
No anxiety |
Mild anxiety |
Moderate anxiety |
Severe anxiety |
Fisher’s exact test |
||
|
Statistic value |
P value |
||||||
|
PAF n (%) |
213 |
169 (79.3) |
31 (14.6) |
11 (5.2) |
2 (0.9) |
0.25 |
0.998 |
|
CAF n (%) |
118 |
93 (78.8) |
18 (15.3) |
6 (5.1) |
1 (0.8) |
||
|
Total |
No depression |
Mild depression |
Moderate depression |
Severe depression |
Fisher’s exact test |
||
|
Statistic value |
P value |
||||||
|
PAF n (%) |
213 |
137 (64.3) |
71 (21.4) |
38 (11.4) |
4 (1.2) |
1.04 |
0.804 |
|
CAF n (%) |
118 |
82 (69.5) |
48 (22.5) |
25 (11.7) |
3 (1.4) |
||
PAF (paroxysmal atrial fibrillation); CAF (persistent atrial fibrillation)
3.3 Associations of Demographic and Clinical Characteristics with Psychological Status
Independent variables that may impact anxiety or depression (P<0.20) were selected for multivariant logistic regression. Since age and gender can impact both dependent and independent variables, all selected variables were adjusted according to these two parameters. Anxiety status was significantly correlated with gender (OR 1.95, 95%CI 1.13-3.34, χ2 = 5.90, P = 0.015) and sleep quality (OR 2.74, 95%CI 1.60-4.71, χ2 = 14.0, P<0.001), with female (OR 1.784, 95%CI 1.014-3.140, P = 0.045) and poor sleep quality (OR 2.640, 95%CI 1.519-4.590, P = 0.001) posing higher risk to the development of anxiety (Table 2). Depression is also significantly associated with gender (OR 1.68, 95%CI 1.04-2.70, χ2 = 4.52, P = 0.033) and poor sleep quality (OR 2.63, 95%CI 1.64-4.24, χ2 = 16.35, P<0.001) in univariate analysis (Table 3). Logistic regression with the independent variable, obesity (OR 1.810, 95%CI 1.047-3.126, P = 0.033), showed that it is significantly associated with depression, similar to poor sleep quality (OR 2.772, 95%CI 1.710-4.493, P<0.001).
Table 3: Multiple logistics regression analysis of determinants of anxiety and depression
|
Variables |
Anxiety |
|||||
|
B |
SE |
Wald |
P value |
OR |
OR(95%CI) |
|
|
Age |
-0.368 |
0.321 |
1.315 |
0.251 |
0.692 |
0.369-1.298 |
|
Gender |
0.579 |
0.288 |
4.032 |
0.045* |
1.784 |
1.014-3.140 |
|
Poor sleep quality |
0.971 |
0.282 |
11.84 |
0.001* |
2.64 |
1.519-4.590 |
|
Variables |
Depression |
|||||
|
B |
SE |
Wald |
P value |
OR |
OR(95%CI) |
|
|
Obesity |
0.593 |
0.279 |
4.521 |
0.033* |
1.81 |
1.047-3.126 |
|
Poor sleep quality |
1.02 |
0.246 |
17.121 |
<0.001* |
2.772 |
1.710-4.493 |
3.4 Association between Psychological Disturbances and Sleep Disruptions
Sleep quality can impact the level of anxiety and depression significantly. Patients who experience frequent sleep disruptions has higher rates of anxiety, with substantial difference (P = 0.001) in the levels of anxiety between patients with and without poor sleep quality (Table 4). Patients who sleep poorly showed significantly higher rates of mild and moderate anxiety than those who can sleep well (21.1% vs 11.9%, 9.7% vs 2.7%, respectively, P<0.05). The prevalence of severe anxiety is also increased in patients with poor sleep quality, but the data is not statistically significant (1.8% vs 0.5%, P>0.05). Similarly for depression, patients who experience frequent sleep disruptions has higher rates of depression, with significant difference in the levels of depression between patients with and without poor sleep quality (P<0.001). In this case, only the rate of mild depression was significantly affected by poor sleep quality (31.9% vs 16.0%, P<0.05). The rate of moderate and severe depression showed a higher trend in patients affected by poor sleep, but this was not significance (14.2% vs 10.0%, 2.7% vs 0.5%, P>0.05).
Table 4: Effect of sleep quality on the levels of anxiety and depression
|
Total |
No anxiety |
Mild anxiety |
Moderate anxiety |
Severe anxiety |
Fisher’s exact test |
||
|
Statistic value |
P value |
||||||
|
A n (%) |
219 (67.0) |
186 (84.9) |
26 (11.9) |
6 (2.7) |
1 (0.5) |
15.38 |
0.001 |
|
B n (%) |
113 (34.0) |
76 (67.3)* |
24 (21.1)* |
11 (9.7)* |
2 (1.8) |
||
|
Total |
No depression |
Mild depression |
Moderate depression |
Severe depression |
Fisher’s exact test |
||
|
Statistic value |
P value |
||||||
|
A n (%) |
219 (67.0) |
161 (73.5) |
35 (16.0) |
22 (10.0) |
1 (0.5) |
18.04 |
<0.001 |
|
B n (%) |
113 (34.0) |
58 (51.3)* |
36 (31.9)* |
16 (14.2) |
3 (2.7) |
||
A: Normal sleep quality; B: Poor sleep quality; *: P<0.05
Grouping of patients according to anxiety and depression status showed that 203 (61.1%) patients were neither depressed nor anxious (none), 16 (4.8%) displayed anxiety only, 59 (17.8%) displayed depression only, and 54 (16.3%) suffered from both disorders (Figure 1). The percentage of patients experiencing disrupted sleep within the four groups were 25.1% (51/203), 43.8% (7/16), 42.4% (25/59) and 55.6% (30/54), respectively. Patients with both anxiety and depression symptoms are 3.69 times more likely to have poor sleep quality (OR = 3.69,95%CI 1.94-7.01,P<0.001), while for patients with depression only, the likelihood of having poor sleep was 2.14 times greater (OR = 2.14,95%CI 1.16-3.96,P = 0.016). Patients with anxiety symptoms only also showed increase likelihood of poor sleep, but this is not significant (OR = 2.06,95%CI 0.72-5.94,P = 0.180).
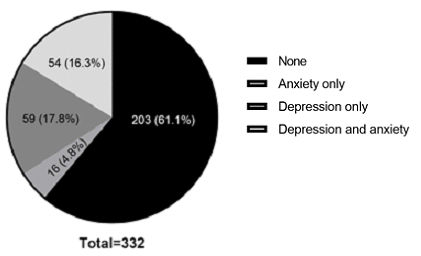
Figure 1: Pie chart showing the frequency of patients with and without anxiety, depression or both.
4. Discussion
In this descriptive and exploratory research, we found that 21.1% AF inpatients had anxiety, 34.0% had depression, and 34.0% sleep poorly. While sleep quality can impact both anxiety and depression, anxiety tends to occur more often in female patients, and obesity rate is higher in depressed patients. Anxiety and depression are moderately associated with each other but strongly associated with chronic sleep disruption, and patients with both psychological disorders showed the highest risk for poor sleep quality. Our results showed that females are at higher risk of developing anxiety but not depression. This is consistent with the work of Trovato et al., where higher mental stress was observed in females with stable AF [21], and the publication from Polikandrioti et al., in which both anxiety and depression were evaluated but only association with anxiety was detected [22]. Possible reasons for why female patients are more likely to be anxious may be due in part to well-documented gender differences for patterns of heart disease and outcomes, differences in daily life, genetics or health behaviors, delayed symptom responses, among other reasons [23]. Associations between obesity and psychological symptoms of depression in AF patients have previously been reported [24, 25]. In addition, the relationship between depression and physical inactivity was also described [26]. Interestingly, Garimella et al. found that increased depression severity, physical inactivity, and increased body mass index are all related to increased AF symptom severity [27]. They also found that the correlation between severity of AF symptom and obesity may be confounded by depression and physical fitness.
When we examined potential covariance of anxiety and depression, these symptoms did not correlate with age or type of AF, unlike previous studies [24-26]. It is likely that this cohort of Chinese AF inpatients suffer from different life stressors and have other unmeasured or unknown confounders that may mediate the development of these psychological symptoms. Anxiety and depression frequently coexistent, and moderate association between them was observed in this study. Twin and family studies suggest that comorbidity can largely be explained by shared genetic risks [28]. As for pathophysiology mechanisms, it is well established that anxiety and depressive disorders share some risk factors, such as heightened stress responsivity [29]. Comorbidity of depression and anxiety is related to increased therapeutic resistance [5, 6]. Refractory patients require a multidisciplinary team, including psychiatrists, cardiologists, and nurses, to adapt appropriate management strategies (e.g. cognitive behavioral treatment, exercise, selective serotonin reuptake inhibitors) to the patient's personal conditions [30, 31]. The ABC pathway (Anticoagulation/Avoid stroke); Better symptom management; Cardiovascular risk and comorbidity management) is a novel holistic management strategy to improve the prognosis of AF patients. Education and lifestyle changes are important aspects of this management strategy in addition to reducing risk factors for the cardiovascular system and preventing stroke [32]. Identification and management of anxiety and depression in AF patients will also improve the overall prognosis of these patients, improve their quality of life, and reduce financial impacts on the health care system [32, 33]. However, there are limited data on the usage of anti-anxiety drugs or antidepressants to control psychological symptoms in AF patients, and potential interactions between these anti-psychotics and antiarrhythmic drugs or anticoagulants for AF treatment may poses challenges. Thus, more studies are required to clarify the benefits of patient education, behavioral and/or psychological therapies in the overall management of AF [33]. Our data indicate that the incidence of mild depression is higher in patients with sleep disturbances, but the rates of moderate and severe depression are not. For anxiety, both the rates of mild and moderate anxiety are significantly higher in patients with sleep disruptions, while the rate of severe anxiety is not significantly changed. These results suggest that sleep quality may affect the development of anxiety more than depression. Indeed, Press et al. also found that depression is only correlated with sleep dissatisfaction, while anxiety is correlated with trouble falling asleep, frequent night waking, morning tiredness and daytime drowsiness [34]. The importance of sleep quality in mental health is intuitive, but is also supported by numerous studies. Persistent poor sleep quality has been shown to increase the risk for severe depression [35]. A two-way connection between depression and sleep quality has been demonstrated where depression can also lead to insomnia [36]. In fact, anxiety and depression are some of the strongest predictors for chronic insomnia [37]. Thus, sleep disruptions and mental disturbances may form a vicious cycle in which one can exacerbates the other [38]. Persistent sleep disruptions can imbalance the hypothalamic pituitary adrenal axis (HPA), and increase the levels of cortisol and inflammatory cytokines, suggesting that these pathways may be contribute partially to the bidirectional interaction between sleep and mental health [39]. Anxiety and depression may aggravate AF by causing an imbalance in the cardiac autonomic nervous system, resulting in changes to the atrial action potential and shortening of the atrial refractory period, leading to atrial ectopic agitation and triggering reentry formation [40]. Conversely, AF can induce remodeling of the autonomic nervous system, which will impact emotional states since this system is also involved in the regulation of emotion [40]. Thus, sustained poor sleep quality together with psychosocial factors, will ultimately impact the quality of life and prognosis of AF patients [41]. Sleep duration may also affect the risk of AF, but the data appeared to be mixed, with some studies indicating a higher risk for AF with long sleep duration [41, 42], while others suggest a role for short sleep duration instead [43], particularly in subgroup analyses. Thus, the effect of sleep duration may be dependent on other factors, such as the presence of other health issues and population characteristics, and more research is required to elucidate the role of sleep duration on AF development. Previous published work as well as our current study strongly indicate that AF patients with poor sleep quality are susceptible to psychological disturbances such as anxiety and depression, and thus should preferentially receive early interventions to manage these potentially debilitating conditions. However, management strategies for AF generally focus on dealing with the physical aspect of the condition, such as the use of anticoagulation and managing bleeding risk, prevention of AF onset, and surgical treatment of arrhythmia [44]. Since poor sleep quality, anxiety attack, and mood deterioration can significantly affect the physical and social function of patients with AF, failure to consider these factors may contribute to complications such as heart failure and thromboembolic stroke that will threaten patient survival. Thus, the medical team must consider psychological assessment and early intervention in AF patients with anxiety and/or depression. Currently, it is not clear whether medical interventions (e.g. cognitive therapy or pharmacotherapy) aiming to improve sleep quality can improve psychological disturbances, or whether drugs for anxiety, depression and poor sleep will aggravate patients’ arrhythmic state. Hence, further studies on the relationship between sleep quality and psychological disturbances, as well as whether strategies to improve sleep quality could improve mental health and AF prognosis are required.
Limitations
The current study has a few limitations which should be addressed in the future. First, this cross-sectional study limits any demonstration of causal relationships between sleep disruption and psychological disorders in AF patients, and unmeasured or unknown confounders are inevitable. Second, objective measurements, such as polysomnograms to evaluate sleep quality is lacking, so precise measurements of sleep quality and standard sleep stages are not available. Third, long-term effects of mental instability, poor sleep quality, and their treatment efficacies are still unknown. Thus, longitudinal studies to monitor sleep, psychological status, and lifestyle stressors will provide more insights for long term management of AF patients. Finally, as our research was performed in a single tertiary center in China, with a specific population and clinical practice, our results may not be completely generalizable to other populations and practice settings.
5. Conclusion
Our study showed that anxiety and depression are common among hospitalized Chinese AF patients. Anxiety occur more frequently in female patients and those with poor sleep quality, while depression is correlated with obesity and sleep disruption. Patients with both anxiety and depression showed the highest risk for disrupted sleep. Therefore, the identification and treatment of these patients, especially those who are female, obese or experience persistent sleep disturbances, should be prioritized. Future research focusing on assessment of mental health and sleep status, monitoring progress, and development of novel therapeutic strategies will bring significant benefits for the patient management.
Declarations
Ethics approval, guidelines and consent to participate
This study was approved by the Ethics Committee of Fuwai Hospital (2016-780) and based on the declaration of Helsinki. Informed consent was obtained from all participants.
Consent for publication
Not applicable.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available because research data is confidential, but are available from the corresponding author on reasonable request. Requests to access the datasets should be directed to doctortangmin@yeah.net.
Competing interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Authors' contributions
L-XH and MT: study conception and design. L-XH and X-TD: analysis and interpretation of data, drafting of the article, and obtaining of funding. MT: critical revision of the article for intellectual content and final approval of the article. X-TD: provision of study materials or patients. L-XH: collection of data. All authors contributed to the article and approved the submitted version.
Funding
National Natural Science Foundation of China [grant numbers 6152 7811 and U1913210]. The funding source had no role in study design; in the collection, analysis, and interpretation of data; in writing the report; and in the decision to submit the article for publication.
Acknowledgments
We thank Editideas (www.editideas.cn) for its linguistic assistance during the preparation of this manuscript.
References:
- Shi S, Tang Y, Zhao Q, et al. Prevalence and Risk of Atrial Fibrillation in China: A National Cross-Sectional Epidemiological Study. The Lancet regional health Western Pacific 23 (2022): 100439.
- Chinese Society of Pacing and Electrophysiology, Chinese Society of Arrhythmias, Atrial Fibrillation Center Union of China. Current knowledge and management of atrial fibrillation: consensus of Chinese experts 2021 Chinese Journal of Cardiac Arrhythmias 26 (2022): 15-88.
- Global, Regional, and National Incidence, Prevalence, and Years Lived with Disability for 310 Diseases and Injuries, 1990-2015: A Systematic Analysis for the Global Burden of Disease Study 2015. Lancet 388 (2016): 1545-1602.
- Kessler RC, Petukhova M, Sampson NA, et al. Twelve-Month and Lifetime Prevalence and Lifetime Morbid Risk of Anxiety and Mood Disorders in the United States. International journal of methods in psychiatric research 21 (2012): 169-184
- Fava M, Rush AJ, Alpert JE, et al. Difference in Treatment Outcome in Outpatients with Anxious Versus Nonanxious Depression: A Star*D Report. The American journal of psychiatry 165 (2008): 342-351.
- Stein DJ, Baldwin DS, Baldinetti F, et al. Efficacy of Pregabalin in Depressive Symptoms Associated with Generalized Anxiety Disorder: A Pooled Analysis of 6 Studies. European neuropsychopharmacology : the journal of the European College of Neuropsychopharmacology 18 (2008): 422-430.
- Hindricks G, Potpara T, Dagres N, et al. 2020 Esc Guidelines for the Diagnosis and Management of Atrial Fibrillation Developed in Collaboration with the European Association for Cardio-Thoracic Surgery (Eacts): The Task Force for the Diagnosis and Management of Atrial Fibrillation of the European Society of Cardiology (Esc) Developed with the Special Contribution of the European Heart Rhythm Association (Ehra) of the Esc. European heart journal 42 (2021): 373-498.
- Javaheri S, Barbe F, Campos-Rodriguez F, et al. Sleep Apnea: Types, Mechanisms, and Clinical Cardiovascular Consequences. Journal of the American College of Cardiology 69 (2017): 841-858.
- Peppard PE, Szklo-Coxe M, Hla KM, et al. Longitudinal Association of Sleep-Related Breathing Disorder and Depression. Arch Intern Med 16 (2006): 1709-1715.
- Wheaton AG, Perry GS, Chapman DP, et al. Sleep Disordered Breathing and Depression among U.S. Adults: National Health and Nutrition Examination Survey, 2005-2008. Sleep 35 (2012): 461-467.
- Alcántara C, Biggs ML, Davidson KW, et al. Sleep Disturbances and Depression in the Multi-Ethnic Study of Atherosclerosis. Sleep 39 (2016):915-925.
- Campos-Rodriguez F, Queipo-Corona C, Carmona-Bernal C, et al. Continuous Positive Airway Pressure Improves Quality of Life in Women with Obstructive Sleep Apnea. A Randomized Controlled Trial. Am J Respir Crit Care Med 194 (2016): 1286-1294.
- Hu L-x, Tang M, Hua W, et al. Psychological Disturbances and Their Association with Sleep Disturbance in Patients Admitted for Arrhythmia Diseases. Neuropsychiatric Disease and Treatment 18 (2022): 1739-1750.
- Li X, Zhou T, Ma H, et al. Healthy Sleep Patterns and Risk of Incident Arrhythmias. Journal of the American College of Cardiology 78 (2021): 1197-1207.
- Kim W, Na JO, Thomas RJ, et al. Impact of Catheter Ablation on Sleep Quality and Relationship between Sleep Stability and Recurrence of Paroxysmal Atrial Fibrillation after Successful Ablation: 24-Hour Holter-Based Cardiopulmonary Coupling Analysis. J Am Heart Assoc 9 (2020): 017016.
- Zung WW. A Rating Instrument for Anxiety Disorders. Psychosomatics 12 (1971): 371-379.
- Tian J, Li L, Tao CL, et al. A Glimpse into the Psychological Status of E.N.T Inpatients in China: A Cross-Sectional Survey of Three Hospitals in Different Regions. World J Otorhinolaryngol Head Neck Surg 5 (2019): 95-104.
- Tao M GJ. The Revised Self Rating Anxiety Scale (Sascr) the Reliability and Validity. Chinese Journal of Neuropsychiatric Diseases 10 (1994).
- Peng H, Zhang Y, Ji Y, et al. Reliability and validity analysis of Chinese version of self-rated Depression Scale for women in rural areas. Shanghai Medical and Pharmaceutical Journal 14 (2013): 20-23.
- Liu XC, Tang MQ, Hu L, et al. Reliability and validity of Pittsburgh sleep quality index [J]. Chinese Journal of Psychiatry 29 (1996): 103-107.
- Trovato GM, Pace P, Cangemi E, et al. Gender, Lifestyles, Illness Perception and Stress in Stable Atrial Fibrillation. La Clinica terapeutica 163 (2012): 281-286.
- Polikandrioti M, Koutelekos I, Vasilopoulos G, et al. Anxiety and Depression in Patients with Permanent Atrial Fibrillation: Prevalence and Associated Factors. Cardiol Res Pract 2018 (2018): 7408129.
- Ball J, Carrington MJ, Wood KA, et al. Women versus Men with Chronic Atrial Fibrillation: Insights from the Standard versus Atrial Fibrillation Specific Management Study (Safety). PLoS One 8 (2013):
- Gleason KT, Dennison Himmelfarb CR, Ford DE, et al. Association of Sex, Age and Education Level with Patient Reported Outcomes in Atrial Fibrillation. BMC Cardiovasc Disord 19 (2019): 85.
- Walters TE, Wick K, Tan G, et al. Psychological Distress and Suicidal Ideation in Patients with Atrial Fibrillation: Prevalence and Response to Management Strategy. J Am Heart Assoc 7 (2018): 005502.
- von Eisenhart Rothe A, Hutt F, Baumert J, et al. Depressed Mood Amplifies Heart-Related Symptoms in Persistent and Paroxysmal Atrial Fibrillation Patients: A Longitudinal Analysis--Data from the German Competence Network on Atrial Fibrillation. Europace 17 (2015): 1354-1362.
- Garimella RS, Sears SF, Gehi AK. Depression and Physical Inactivity as Confounding the Effect of Obesity on Atrial Fibrillation. Am J Cardiol 117 (2016): 1760-1764.
- Middeldorp CM, Cath DC, Van Dyck R, et al. The Co-Morbidity of Anxiety and Depression in the Perspective of Genetic Epidemiology. A Review of Twin and Family Studies. Psychol Med 35 (2005): 611-624.
- Janiri D, Moser DA, Doucet GE, et al. Shared Neural Phenotypes for Mood and Anxiety Disorders: A Meta-Analysis of 226 Task-Related Functional Imaging Studies. JAMA psychiatry 77 (2020): 172-179.
- MK, Qamar A, Vaduganathan M, Charney DS, et al. Screening and Management of Depression in Patients with Cardiovascular Disease: Jacc state-of-the-Art Review. Journal of the American College of Cardiology 73 (2019): 1827-1845.
- Corrigendum To: Depression and Coronary Heart Disease: 2018 Position Paper of the Esc Working Group on Coronary Pathophysiology and Microcirculation Developed under the Auspices of the Esc Committee for Practice Guidelines. European heart journal 41 (2020): 1696.
- Lip GYH. The Abc Pathway: An Integrated Approach to Improve Af Management. Nature reviews Cardiology 14 (2017): 627-628.
- Pavlicek V, Wedegärtner SM, Millenaar D, et al. Heart-Focused Anxiety, General Anxiety, Depression and Health-Related Quality of Life in Patients with Atrial Fibrillation Undergoing Pulmonary Vein Isolation. J Clin Med 11 (2022).
- Press Y, Punchik B, Freud T. The Association between Subjectively Impaired Sleep and Symptoms of Depression and Anxiety in a Frail Elderly Population. Aging clinical and experimental research 30 (2018): 755-765.
- Breslau N, Roth T, Rosenthal L, et al. Sleep Disturbance and Psychiatric Disorders: A Longitudinal Epidemiological Study of Young Adults. Biological psychiatry 39 (1996): 411-418.
- Bao YP, Han Y, Ma J, et al. Cooccurrence and Bidirectional Prediction of Sleep Disturbances and Depression in Older Adults: Meta-Analysis and Systematic Review. Neuroscience and biobehavioral reviews 75 (2017): 257-273.
- Riemann D, Spiegelhalder K, Feige B, et al. The Hyperarousal Model of Insomnia: A Review of the Concept and Its Evidence. Sleep medicine reviews 14 (2010): 19-31.
- Sivertsen B, Salo P, Mykletun A, et al. The Bidirectional Association between Depression and Insomnia: The Hunt Study. Psychosomatic medicine 74 (2012): 758-765.
- Blake MJ, Trinder JA, Allen NB. Mechanisms Underlying the Association between Insomnia, Anxiety, and Depression in Adolescence: Implications for Behavioral Sleep Interventions. Clinical psychology review 63 (2018): 25-40.
- Schnabel RB, Hasenfuß G, Buchmann S, et al. Heart and Brain Interactions: Pathophysiology and Management of Cardio-Psycho-Neurological Disorders. Herz 46 (2021): 138-149.
- Khawaja O, Sarwar A, Albert CM, et al. Sleep Duration and Risk of Atrial Fibrillation (from the Physicians' Health Study). Am J Cardiol 111 (2013): 547-551.
- Song Q, Liu X, Hu W, et al. Long Sleep Duration Is an Independent Risk Factor for Incident Atrial Fibrillation in a Chinese Population: A Prospective Cohort Study. Scientific reports 7 (2017): 3679.
- Genuardi MV, Ogilvie RP, Saand AR, et al. Association of Short Sleep Duration and Atrial Fibrillation. Chest 156 (2019): 544-552.
- Crandall MA, Bradley DJ, Packer DL, et al. Contemporary Management of Atrial Fibrillation: Update on Anticoagulation and Invasive Management Strategies. Mayo Clin Proc 84 (2009): 643-662.
