Impact of Opioids and Paracetamol after Liver Resection for Colorectal Cancer Metastasis
Article Information
Emil Östrand MD1, 2, Maja Bergfelt MD1, 2, Jenny Rystedt MD, PhD1, 2, Bodil Andersson MD, PhD1, 2, Bobby Tingstedt MD, PhD1, 2
1Department of Surgery, Skåne University Hospital, Lund, Sweden
2Department of Clinical Sciences Lund, Surgery, Lund University, Sweden
*Corresponding Author: Bobby Tingstedt, PhD, Department of Surgery, Skåne University Hospital Lund, SE-221 85 Lund, Sweden.
Received: 29 March 2023; Accepted: 16 May 2023; Published: 12 June 2023
Citation: Emil Östrand, Maja Bergfelt, Jenny Rystedt, Bodil Andersson, Bobby Tingstedt. Impact of Opioids and Paracetamol after Liver Resection for Colorectal Cancer Metastasis. Archives of Clinical and Medical Case Reports. 7 (2023): 261-268.
View / Download Pdf Share at FacebookAbstract
Background: Altered metabolism after liver surgery adds complexity to postoperative pain management. Opioids administered via intravenous Patient Controlled Analgesia (PCA) is one of the main alternatives for initial pain management. Paracetamol is considered potentially dangerous after liver surgery but used selectively. This study evaluates whether there is a difference in patient outcome after hepatic resection, based on the amounts of opioids used in the first postoperative period, and on the use of postoperative paracetamol.
Methods: 208 consecutive patients with hepatic resection for colorectal liver metastasis in Lund, Sweden, were included. Opioids consumed within the first 24 hours postoperatively were summed up. The use of paracetamol in the first four days was recorded. The effect of opioid consumption was analysed by grouping patients into those consuming higher amounts of opioids than the median (HO) and those consuming less amounts (LO). Patient outcome was evaluated by length-of-stay (LOS) and postoperative complications.
Results: The HO-group had a longer LOS than the LO-group, by a regression coefficient of 1.19, p=0.001, after adjusting for confounders. Use of paracetamol individually shortened the LOS, by 0.83, p=0.002. There was no impact of these factors on postoperative complications.
Conclusion: Larger consumption of opioids in the first postoperative day negatively impacts the LOS. Paracetamol shortens the LOS and should be considered after hepatic surgery.
Keywords
Liver resection, Outcome, opioids, Length of stay (LOS), Paracetamol
Liver resection articles, Outcome articles, opioids articles, Length of stay (LOS) articles, Paracetamol articles
COVID-19 articles COVID-19 Research articles COVID-19 review articles COVID-19 PubMed articles COVID-19 PubMed Central articles COVID-19 2023 articles COVID-19 2024 articles COVID-19 Scopus articles COVID-19 impact factor journals COVID-19 Scopus journals COVID-19 PubMed journals COVID-19 medical journals COVID-19 free journals COVID-19 best journals COVID-19 top journals COVID-19 free medical journals COVID-19 famous journals COVID-19 Google Scholar indexed journals Liver resection articles Liver resection Research articles Liver resection review articles Liver resection PubMed articles Liver resection PubMed Central articles Liver resection 2023 articles Liver resection 2024 articles Liver resection Scopus articles Liver resection impact factor journals Liver resection Scopus journals Liver resection PubMed journals Liver resection medical journals Liver resection free journals Liver resection best journals Liver resection top journals Liver resection free medical journals Liver resection famous journals Liver resection Google Scholar indexed journals Outcome articles Outcome Research articles Outcome review articles Outcome PubMed articles Outcome PubMed Central articles Outcome 2023 articles Outcome 2024 articles Outcome Scopus articles Outcome impact factor journals Outcome Scopus journals Outcome PubMed journals Outcome medical journals Outcome free journals Outcome best journals Outcome top journals Outcome free medical journals Outcome famous journals Outcome Google Scholar indexed journals opioids articles opioids Research articles opioids review articles opioids PubMed articles opioids PubMed Central articles opioids 2023 articles opioids 2024 articles opioids Scopus articles opioids impact factor journals opioids Scopus journals opioids PubMed journals opioids medical journals opioids free journals opioids best journals opioids top journals opioids free medical journals opioids famous journals opioids Google Scholar indexed journals Ultrasound articles Ultrasound Research articles Ultrasound review articles Ultrasound PubMed articles Ultrasound PubMed Central articles Ultrasound 2023 articles Ultrasound 2024 articles Ultrasound Scopus articles Ultrasound impact factor journals Ultrasound Scopus journals Ultrasound PubMed journals Ultrasound medical journals Ultrasound free journals Ultrasound best journals Ultrasound top journals Ultrasound free medical journals Ultrasound famous journals Ultrasound Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals Dermatitis Bullous Variants articles Dermatitis Bullous Variants Research articles Dermatitis Bullous Variants review articles Dermatitis Bullous Variants PubMed articles Dermatitis Bullous Variants PubMed Central articles Dermatitis Bullous Variants 2023 articles Dermatitis Bullous Variants 2024 articles Dermatitis Bullous Variants Scopus articles Dermatitis Bullous Variants impact factor journals Dermatitis Bullous Variants Scopus journals Dermatitis Bullous Variants PubMed journals Dermatitis Bullous Variants medical journals Dermatitis Bullous Variants free journals Dermatitis Bullous Variants best journals Dermatitis Bullous Variants top journals Dermatitis Bullous Variants free medical journals Dermatitis Bullous Variants famous journals Dermatitis Bullous Variants Google Scholar indexed journals Paracetamol articles Paracetamol Research articles Paracetamol review articles Paracetamol PubMed articles Paracetamol PubMed Central articles Paracetamol 2023 articles Paracetamol 2024 articles Paracetamol Scopus articles Paracetamol impact factor journals Paracetamol Scopus journals Paracetamol PubMed journals Paracetamol medical journals Paracetamol free journals Paracetamol best journals Paracetamol top journals Paracetamol free medical journals Paracetamol famous journals Paracetamol Google Scholar indexed journals Spinal Anesthesia articles Spinal Anesthesia Research articles Spinal Anesthesia review articles Spinal Anesthesia PubMed articles Spinal Anesthesia PubMed Central articles Spinal Anesthesia 2023 articles Spinal Anesthesia 2024 articles Spinal Anesthesia Scopus articles Spinal Anesthesia impact factor journals Spinal Anesthesia Scopus journals Spinal Anesthesia PubMed journals Spinal Anesthesia medical journals Spinal Anesthesia free journals Spinal Anesthesia best journals Spinal Anesthesia top journals Spinal Anesthesia free medical journals Spinal Anesthesia famous journals Spinal Anesthesia Google Scholar indexed journals
Article Details
1. Introduction
The rates of hepatic resection have increased during the last decades as the outcome has improved [1]. Colorectal cancer is the world’s third most common cancer, and approximately half of the patients present with, or develop, colorectal liver metastasis (CRLM). The main potentially curative treatment for patients with CRLM is liver resection, combined with oncological treatment with chemotherapy [2]. The 5-year overall survival after liver surgery for CRLM is about 50% [3]. The improved outcome after hepatic resection can be attributed to improvement in surgical techniques, patient selection and perioperative management [1].
Enhanced Recovery Pathways (ERPs), standardised perioperative management plans, have been developed and implemented in various surgical fields, also suggested in liver surgery [4, 5]. Postoperative pain control is of great importance for patients’ recovery, as inadequate pain control can increase the incidence of complications, prolong the length of stay (LOS) in hospital and worsen the patients’ experience of recovery [5-8]. Postoperative pain management remains a difficult issue, partly due to the postresection metabolism specific to hepatic surgery. The metabolism of opioids can be affected by large resections [9]. Opioids may cause respiratory depression, pruritus, sedation, postoperative ileus, and nausea [10-13]. They can also induce tolerance, dependence, and hyperalgesia in the postoperative patient [13]. These adverse effects may worsen outcomes after surgery. Epidural analgesia (EA) is an opioid sparing alternative in pain management. Still, it has other problems associated with it in liver surgery, such as the risk of more problematic fluid management, an increased risk of epidural hematomas due to postoperative coagulopathy associated with liver surgery, and more difficult postoperative mobilisation [8, 14, 15]. Studies comparing opioids and EA have demonstrated conflicting results [5, 10-12, 16, 17]. By ERPs, and the PROSPECT work group, it is recommended also to also analgesic supplements, such as non-steroid anti-inflammatory drugs, local anaesthetic infusion pumps, subcostal transversus abdominis plane blocks or paracetamol [5, 8, 18-21]. In other types of surgery, paracetamol is often considered a standard part of the multimodal postoperative pain management [4]. In liver surgery, though, changes in metabolism after liver resection might increase the plasma concentration of paracetamol, possibly causing toxic effects. Hence paracetamol is often avoided after major hepatectomies [20, 22].
The aim of this study was to evaluate whether there is a difference in patient outcome after hepatic resection based on both the amounts of opioids used and the use of paracetamol or not.
2. Material and Methods
2.1 Patients and perioperative management
Patient records of patients who had partial hepatectomy for CRLM at Skåne University Hospital in Lund, from 1 January 2014 to 31 December 2017 were analysed retrospectively. Patient characteristics, perioperative parameters and outcome parameters were collected from patient records and Patient Controlled Analgesia (PCA) work sheets. Patients were excluded if they had preoperative chronic opioid use, had other synchronous surgery, had an Associating Liver Partition and Portal vein Ligation for Staged hepatectomy (ALPPS), had irresectable metastasis, had laparoscopic surgery, or had missing patient records, Figure 1.
Patients were anesthetised by routine using Propofol, Fentanyl, Rocuronium and Sevoflurane or Remifentanyl. By routine patients had a postoperative intravenous PCA, with Morphine, Ketobemidone or Oxycodone, depending on the standard at the time of surgery. The initial PCA standard-setting was: continuous infusion of 0.5-1 mg per hour; Bolus dosage of 1 mg; Lock-out time 10 minutes; Upper limit of 6 bolus doses per hour. The settings could be changed at the discretion of a specialised pain-team. Patients who did not use a PCA received oral opioids combined with nurse-administered intravenous opioids, as needed. Paracetamol was given at the surgeon’s discretion.
The total amount of opioids consumed from the end of surgery and the following days was analysed. The noted total use closest to 24 hours postoperative was used to calculate the 24 hours PCA consumption. All opioids administered via the PCA, any other extra injections, and any oral opioids were included. Opioids such as oxycodone given as a postoperative bolus at the end of surgery, were also included, but perioperative Fentanyl or Remifentanil given as part of the anaesthesia was excluded due to short-acting nature of it. Opioids were converted to oral morphine equivalents (OME) [23]. and summed up. Based on the total amount of opioids consumed, patients were divided into two groups; patients who had consumed less opioids than the median “low opioids” (LO), and patients who had consumed more than median “high opioids” (HO). Paracetamol (acetaminophen) was individually dosed; the normal dose was 1000mg x4, iv or po.
2.2 Definitions
Major hepatic resection was defined as resection of three or more Couinaud segments. Complications were categorised based on the Clavien-Dindo classification [24]. Major complications were defined as Clavien-Dindo ≥3a. Nausea was defined as receiving medical treatment with Ondansetron or Metoclopramide the first four days. Paracetamol use was defined as receiving paracetamol within the first four days post-surgery. Day of bowel recovery was defined as the day of first bowel movement. American Society of Anaesthesiologists (ASA) classification was dichotomised into class <3 versus class ≥3. Length-of-stay (LOS) was defined as day of discharge to home.
2.3 Statistics
The main outcomes LOS, minor complications and major complications were analysed for relation to opioid consumption, and paracetamol consumption by using linear regression, and logistic regression, in univariable and multivariable analyses. In the multivariable analyses variables considered to be clinically relevant or had a p <0.10 in the univariable analysis were tested for independent effect on the outcome. Bowel recovery and nausea were not included in the multivariable analyses, as they were considered mediators. In an iterative process of variable selection using backward stepwise selection, covariates were removed from the model if they were non-significant. LOS was log-transformed in order to fulfill assumptions about the normality and homoscedasticity of the residuals.
Patient data and perioperative data are described in absolute numbers and percentages, distribution in median and interquartile range (IQR). The results of linear regression analysis are presented as Exp(B) for LOS, with 95% confidence interval (CI), and the logistic regression as Odds Ratio (OR) with 95% CI. Two-tailed p-values <0.05 were considered statistically significant. All statistical analyses were performed using SPSS version 25.0, 2017 (IBM, Armonk, New York, USA). Ethics were approved by the Regional Human Ethics Committee at Lund University (Dnr 2019/00762).
3. Results
In total 268 consecutive patients subject to liver resection for CRLM at Skåne University Hospital in Lund were identified. Sixty patients were excluded, Figure 1. A cohort of 208 patients was obtained.
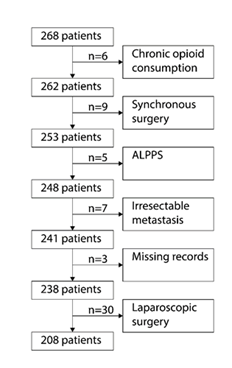
Figure 1: Flow Chart.
Flow chart for included and excluded patients. ALPPS= Associating Liver Partition and Portal vein Ligation for Staged hepatectomy.
Median consumed opioids during the first 24 hours after surgery was 116.8mg (87.6-164.5mg) in the whole cohort, and the patients were grouped as HO or LO accordingly. Patients in LO consumed 87.9mg in median in the first 24 hours, and in HO 164.1mg. Patients in HO were younger, more often male, weighed more and had higher BMI, Table 1. LOS was longer in the HO group. There was no significant difference between the groups in rates of diabetes, smoking, ASA class. The blood loss during surgery and operation time was similar. No difference in bowel recovery could be found. No difference was found regarding nausea, or complications. The use of paracetamol was the same in both groups.
|
|
|
Groups |
|
|
|
Variable |
n |
Low opioids |
High opioids |
p-value |
|
Gender, male |
208 |
59 (56.7%) |
77 (74.0%) |
0.009 |
|
Age |
208 |
71.5 (64.25 – 76) |
66 (57 – 72) |
<0.001 |
|
BMI |
208 |
24.8 (23.1 – 28.6) |
26.6 (23.9 – 28.6) |
0.047 |
|
Weight |
208 |
74.8 (65.0 – 83.3) |
81.8 (72.9 – 89.0) |
0.001 |
|
Diabetes |
208 |
13 (12.5%) |
10 (9.6%) |
0.507 |
|
Smoking |
207 |
18 (17.3%) |
13 (12.6%) |
0.345 |
|
ASA-score ≥3 |
208 |
38 (36.5%) |
43 (41.3%) |
0.477 |
|
Re-resection |
208 |
12 (11.5%) |
8 (7.7%) |
0.347 |
|
Operation time, hours |
195 |
4.0 (2.9 – 5.8) |
4.5 (3.5 – 6.1) |
0.052 |
|
Blood loss, litres |
208 |
0.4 (0.2 – 0.7) |
0.5 (0.25 – 0.8) |
0.122 |
|
Major hepatic resection |
208 |
45 (43.3%) |
39 (37.5%) |
0.397 |
|
Opioids, mg |
208 |
87.9 (71.0 – 103.0) |
164.1 (138.1 – 189.7) |
- |
|
Paracetamol postop |
208 |
62 (59.6%) |
61 (58.7%) |
0.888 |
|
Nausea |
208 |
61 (58.7%) |
53 (51.0%) |
0.265 |
|
Bowel recovery, days |
165 |
4 (3-5) |
4 (3-5) |
0.455 |
|
Complications |
208 |
51 (49.0%) |
62 (59.6%) |
0.126 |
|
12 (11.5%) |
11 (10.6%) |
0.825 |
||
|
LOS, days |
208 |
6 (5 – 7.75) |
6 (5.25 – 8.75) |
0.009 |
Table 1: Patient and treatment characteristics.
Cut-off between groups is at median consumption of opioids per the first 24 hours: 116.8mg/24h. BMI=Body mass index. ASA=American Society of Anaesthesiologists. LOS= Length of stay in hospital. Data presented in actual numbers and percent, medians and IQR, Inter Quartile Range. Statistics: Chi-Square or Mann-Whitney.
3.1 Regression models
The correlation of LOS and confounders is presented in Table 2. HO was independently associated with LOS by regression coefficient of 1.19, p=0.001. Use of paracetamol was associated with shorter LOS, regression coefficient 0.83, p=0.002. Age, operation time, and minor and major complications were covariates associated with LOS.
HO was not found to individually impact minor complications, nor was paracetamol, Table 3. Longer operation time was associated with minor complications, OR 1.21, p=0.021. Smoking decreased the risk for minor complications, OR 0.38, p=0.026.
Paracetamol use and blood loss were found to impact major complications in univariate analysis, but in multivariable analysis no individual impacts were found, table 4.
|
|
Univariable analysis |
Multivariable analysis |
||||
|
Missing data |
Exp(B) (95% CI) |
p-value |
Exp(B) (95% CI) |
p-value |
||
|
Gender, male |
1.11 (0.97 – 1.27) |
<0.001 |
||||
|
Age |
1.06 (1.00 – 1.01) |
0.403 |
1.20 (1.00 – 1.01) |
0.001 |
||
|
BMI |
1.08 (0.99 – 1.03) |
0.255 |
||||
|
Diabetes |
1.13 (0.98 – 1.47) |
0.079 |
||||
|
Smoking |
1 |
1.08 (0.99 – 1.03) |
0.433 |
|||
|
ASA ≥3 |
1.17 (1.02 – 1.33) |
0.02 |
||||
|
Re-resections |
0.89 (0.66 – 1.03) |
0.085 |
||||
|
Operation time, hours |
13 |
1.45 (1.06 – 1.13) |
<0.001 |
1.18 (1.01 – 1.07) |
0.008 |
|
|
Blood loss, litres |
1.28 (1.11 – 1.41) |
<0.001 |
||||
|
Major hepatic resection |
1.29 (1.12 – 1.45) |
<0.001 |
||||
|
Nausea |
1.21 (1.05 – 1.36) |
0.006 |
||||
|
Bowel recovery |
43 |
1.41 (1.07 – 1.17) |
<0.001 |
|||
|
Complications |
Minor |
1.19 (1.04 – 1.34) |
0.011 |
1.41 (1.25 – 1.54) |
<0.001 |
|
|
Major |
1.63 (1.74 – 2.49) |
<0.001 |
1.82 (2.11 – 2.95) |
<0.001 |
||
|
Paracetamol postop |
0.68 (0.61 – 0.77) |
<0.001 |
0.83 (0.75 – 0.94) |
0.002 |
||
|
High Opioids (HO) |
1.19 (1.04 – 1.34) |
0.012 |
1.19 (1.07 – 1.30) |
0.001 |
||
n=208. ASA=American Society of Anaesthesiologists. BMI = Body Mass Index.
Table 2: Length of stay, linear regression models.
|
|
Univariable analysis |
Multivariable analysis |
|||
|
Missing data |
OR (95% CI) |
p-value |
OR (95% CI) |
p-value |
|
|
Gender, male |
0.78 (0.44 - 1.39) |
0.399 |
0.57 (0.30 – 1.09) |
0.088 |
|
|
Age |
1.00 (0.97 – 1.02) |
0.793 |
|||
|
BMI |
1.02 (0.96 – 1.10) |
0.509 |
|||
|
Diabetes |
0.75 (0.31 – 1.78) |
0.508 |
|||
|
Smoking |
1 |
0.48 (0.22 – 1.05) |
0.066 |
0.38 (0.16 – 0.89) |
0.026 |
|
ASA ≥3 |
1.39 (0.79 – 2.44) |
0.255 |
|||
|
Re-resections |
0.66 (0.26 – 1.67) |
0.381 |
|||
|
Operation time, hours |
13 |
1.19 (1.02 – 1.38) |
0.03 |
1.21 (1.03 – 1.42) |
0.021 |
|
Blood loss, litres |
1.52 (0.87 – 2.66) |
0.144 |
|||
|
Major hepatic resection |
1.03 (0.59 – 1.80) |
0.917 |
|||
|
Nausea |
1.49 (0.86 – 2.58) |
0.157 |
|||
|
Bowel recovery |
43 |
1.03 (0.81 – 1.31) |
0.808 |
||
|
Paracetamol postop |
0.74 (0.42 – 1.28) |
0.28 |
|||
|
High Opioids (HO) |
1.53 (0.89 – 2.66) |
0.126 |
|||
n = 208. ASA=American Society of Anaesthesiologists. BMI = Body Mass Index.
Table 3: Minor Complications, logistic regression models
|
Univariable analysis |
Multivariable analysis |
||||
|
Missing data |
OR (95% CI) |
p-value |
OR (95% CI) |
p-value |
|
|
Gender, male |
1.57 (0.59 – 4.18) |
0.365 |
|||
|
Age |
0.99 (0.95 – 1.03) |
0.689 |
|||
|
BMI |
1.07 (0.97 – 1.19) |
0.195 |
|||
|
Diabetes |
1.84 (0.57 – 5.97) |
0.311 |
|||
|
Smoking |
1 |
0.84 (0.23 – 3.00) |
0.783 |
||
|
ASA ≥3 |
1.83 (0.77 – 4.38) |
0.172 |
|||
|
Re-resections |
2.22 (0.67 – 7.34) |
0.19 |
|||
|
Operation time, hours |
13 |
1.24 (0.99 – 1.55) |
0.06 |
||
|
Blood loss, litres |
2.07 (1.06 – 4.02) |
0.033 |
|||
|
Major hepatic resection |
1.71 (0.72 – 4.09) |
0.226 |
|||
|
Nausea |
2.57 (0.97 – 6.81) |
0.058 |
|||
|
Bowel recovery |
43 |
1.55 (1.11 –2.17) |
0.01 |
||
|
Paracetamol postop |
0.40 (0.17 – 0.97) |
0.043 |
0.41 (0.16 – 1.04) |
0.06 |
|
|
High Opioids (HO) |
0.91 (0.38 – 2.16) |
0.825 |
|||
n = 208. ASA=American Society of Anaesthesiologists. BMI = Body Mass Index.
Table 4: Major complications. Logistic regression models
4. Discussion
This study shows that patients consuming high amounts of opioids in the first 24 hours after liver surgery have longer LOS, and that patients having paracetamol postoperatively have shorter LOS after liver surgery for CRLM. No individual correlations between complications and opioids or paracetamol were found. To our knowledge it is the first study to demonstrate a correlation between LOS and opioid consumption in liver surgery.
The amounts of opioids consumed were found to diverge broadly, with patients in LO using almost half as much as patients in HO. Younger patients consumed more opioids than older patients, consistent with previous studies and the lower metabolism and age-related renal impairment that is expected with increasing age [25, 26]. Age also correlated individually with LOS in the present study. Worse outcomes for elderly, including longer LOS after surgery, is previously established [27]. Females were found to consume less opioids than males, possibly depending on lower average weight, and lower opioid metabolism [25]. Higher weight and BMI were found to be more common in the HO group. Gender and BMI had no individual impact on LOS or complications. Postoperative hepatic metabolism of opioids can be affected by the extent of the resection [9, 28]. No difference in frequency of major resections was found between opioid groups in the present study, and the extent of resections was not found to be individually associated to neither LOS nor complications.
This study measured the opioids consumed only early in the postoperative recovery, in the first 24 hours after surgery, and found that patients in HO had longer LOS than LO. This implies that high amounts of opioids consumed this early during recovery negatively affect the rest of the hospital stay. Early in recovery, many complications have not started to present, and hence complications are not likely to have affected the amounts of opioids consumed yet. Correlation between opioid consumption and LOS has previously been demonstrated, in orthopaedic surgery [29]. Patients in this study were naive to opioids, as patients with chronic opioid use were excluded from the cohort. Hence, any individual opioid tolerance in this cohort is native and impossible to control.
In this study the amounts of opioids used did not correlate individually to complications. Opioids can contribute to postoperative complications, however [6]. As major complications are more frequent after complex liver surgery, associations with blood loss, operation time and extent of hepatic resections would be expected, but no such association was found. Nausea, and late bowel recovery, are expected side effects of opioids [17]. Nausea treated with antiemetics is classed as a minor complication according Clavien Dindo. Late bowel recovery secondary to large amounts of opioids may lead to a longer LOS [24]. Possible correlations to complications and LOS can thus be secondary to opioid use and therefore nausea and bowel recovery could not be included in multivariate analyses.
Minor complications had, surprisingly, an individual negative correlation to smoking, opposite of what was expected. The low smoking prevalence in this study may raise questions about the accuracy of the patients’ smoking reports and difficult to interpret. Due to changes in metabolism after liver resection paracetamol is often avoided after major hepatectomies [20, 22, 30]. No correlation between paracetamol and complications could be seen, in this study. This might be due to patient selection, since paracetamol was used at the discretion of the surgeon, and it can be suspected that fragile patients and patients expected to have a limited liver function postoperatively were not administered paracetamol.
In this cohort, paracetamol was found to be an individual predictor for shorter LOS. It was given to approximately two-thirds of the patients. We had expected to find an opioid-sparing effect to paracetamol, in accordance with previous studies [8, 30], but no such effect could be seen. Previous studies have demonstrated that hepatic resections may result in altered metabolism of paracetamol, but not in toxic blood concentration or toxic effects [20, 22]. Risk factors for hepatotoxicity of paracetamol that need to be considered before using it after liver resections, are liver disease, age, malnutrition, intraoperative liver ischemia and low remnant liver volume [8]. The results of this study show that paracetamol should be used in hepatectomy patients whenever no such contraindications apply.
In this study cohort, no other postoperative analgesics were given than opioids and paracetamol. Recent literature and ERPs suggest that multimodal pain management using analgesic supplements such as non-steroid anti-inflammatory drugs, local anaesthetic infusion pumps, subcostal transversus abdominis plane blocks and paracetamol is effective in reducing opioid consumption and may improve recovery and shorten the LOS [5, 8, 18-21]. The present study shows that patients receiving analgesia with opioids alone have a longer hospital stay than patients combining opioids and paracetamol, thus confirming the need to implement multimodal pain management.
This study was performed in an actual clinical setting, with unselected patients, naive to opioids, having hepatic resections for CRLM. A strength of the study is that even though different opioids were used during the study period, all opioids were converted to OME to be able to make comparisons between patients and previous publications easy. As the present study is a retrospective cohort study there are limitations. The study relies on the data in the patient records and worksheets and the accuracy of these data. Patient records had some missing data, mainly concerning bowel recovery, and nausea was measured as receiving antiemetics postoperatively instead of actual patient ratings.
Future studies on opioid use during postoperative recovery should explore multimodal pain management, using analgesic supplements together with opioids. Studies should aim to include patients prospectively and to include pain scores and Quality-of-recovery-scores to investigate the analgetic effect and patient satisfaction in the different arms.
5. Conclusion
In conclusion, this study shows that larger consumption of opioids the first 24 hours postoperatively negatively impacts the surgical outcome, with a longer LOS. To improve the surgical outcome, multimodal pain management should be implemented to lower opioid doses, and paracetamol should be given postoperative when possible.
Acknowledgments
None
Summary Box
What is already known
- Postoperative pain management after liver surgery is complex, partly due to postoperative alterations in hepatic metabolism.
- Postoperative opioids may cause side effects with impact on patient outcome
- Multimodal pain management can lower the need for opioids postoperatively
- What the new findings are:
- High opioid use in the first 24 hours postoperative after liver surgery impacts the patient outcome negatively.
- Paracetamol shortens the LOS and should be considered after hepatic surgery.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Zhao Y, Qin H, Wu Y, et al. Enhanced recovery after surgery program reduces length of hospital stay and complications in liver resection: A PRISMA-compliant systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore) 96 (2017): e7628.
- Adam R, De Gramont A, Figueras J, et al. The oncosurgery approach to managing liver metastases from colorectal cancer: a multidisciplinary international consensus. Oncologist 17 (2012): 1225-1239.
- Isaksson B, Rizell M, Genell A, et al. Swedish national registry for liver surgery, Sweliv. Annual report 17(2019).
- Ljungqvist O, Scott M, Fearon KC. Enhanced Recovery After Surgery: A Review. JAMA Surg 152 (2017): 292-298.
- Melloul E, Hubner M, Scott M, et al. Guidelines for Perioperative Care for Liver Surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations. World J Surg 40 (2016): 2425-2440.
- Kehlet H, Holte K. Effect of postoperative analgesia on surgical outcome. Br J Anaesth 87 (2001): 62-72.
- Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet 367 (2006): 1618-1625.
- Dieu A, Huynen P, Lavand'homme P, et al. Pain management after open liver resection: Procedure-Specific Postoperative Pain Management (PROSPECT) recommendations. Reg Anesth Pain Med 46 (2021): 433-445.
- Rudin A, Lundberg JF, Hammarlund-Udenaes M et al. Morphine metabolism after major liver surgery. Anesth Analg 104 (2007): 1409-1414.
- Hausken J, Fretland AA, Edwin B, et al. Intravenous Patient-controlled Analgesia Versus Thoracic Epidural Analgesia After Open Liver Surgery: A Prospective, Randomized, Controlled, Noninferiority Trial. Ann Surg 270 (2019): 193-199.
- Li J, Pourrahmat MM, Vasilyeva E, et al. Efficacy and Safety of Patient-controlled Analgesia Compared With Epidural Analgesia After Open Hepatic Resection: A Systematic Review and Meta-analysis. Ann Surg 270 (2019): 200-208.
- Merath K, Hyer JM, Mehta R, et al. Use of perioperative epidural analgesia among Medicare patients undergoing hepatic and pancreatic surgery. HPB (Oxford) 21 (2019): 1064-1071.
- Colvin LA, Bull F, Hales TG. Perioperative opioid analgesia-when is enough too much? A review of opioid-induced tolerance and hyperalgesia. Lancet 393 (2019): 1558-1568.
- Sakowska M, Docherty E, Linscott D et al. A change in practice from epidural to intrathecal morphine analgesia for hepato-pancreato-biliary surgery. World J Surg 33 (2009): 1802-1808.
- Jacquenod P, Wallon G, Gazon M, et al. Incidence and Risk Factors of Coagulation Profile Derangement After Liver Surgery: Implications for the Use of Epidural Analgesia-A Retrospective Cohort Study. Anesth Analg 126 (2018): 1142-1147.
- Aydogan MS, Bicakcioglu M, Sayan H et al. Effects of two different techniques of postoperative analgesia management in liver transplant donors: a prospective, randomized, double-blind study. Transplant Proc 47 (2015): 1204-1206.
- Salicath JH, Yeoh EC, Bennett MH. Epidural analgesia versus patient-controlled intravenous analgesia for pain following intra-abdominal surgery in adults. Cochrane Database Syst Rev 8 (2018): CD010434.
- Qiao XF, Jia WD, Li YQ, et al. Effectiveness of Parecoxib Sodium Combined with Transversus Abdominis Plane Block for Pain Management After Hepatectomy for Hepatocellular Carcinoma: A Prospective Controlled Study. Med Sci Monit 25 (2019): 1053-1060.
- Kitlik A, Erdogan MA, Ozgul U, et al. Ultrasound-guided transversus abdominis plane block for postoperative analgesia in living liver donors: A prospective, randomized, double-blinded clinical trial. J Clin Anesth 37 (2017): 103-107.
- Hughes MJ, Harrison EM, Jin Y et al. Acetaminophen metabolism after liver resection: A prospective case-control study. Dig Liver Dis 47 (2015): 1039-1046.
- Gavriilidis P, Roberts KJ, Sutcliffe RP. Local anaesthetic infiltration via wound catheter versus epidural analgesia in open hepatectomy: a systematic review and meta-analysis of randomised controlled trials. HPB (Oxfod) 21 (2019): 945-952.
- Galinski M, Delhotal-Landes B, Lockey DJ, et al. Reduction of paracetamol metabolism after hepatic resection. Pharmacology 77 (2006): 161-165.
- Nielsen S, Degenhardt L, Hoban B et al. A synthesis of oral morphine equivalents (OME) for opioid utilisation studies. Pharmacoepidemiol Drug Saf 25 (2016): 733-737.
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240 (2004): 205-213.
- Smith HS. Opioid metabolism. Mayo Clin Proc 84 (2009): 613-624.
- Behman R, Cleary S, McHardy P, et al. Predictors of Post-operative Pain and Opioid Consumption in Patients Undergoing Liver Surgery. World J Surg 43 (2019): 2579-2586.
- Reddy SK, Barbas AS, Turley RS, et al. Major liver resection in elderly patients: a multi-institutional analysis. J Am Coll Surg 212 (2011): 787-795.
- Moss CR, Caldwell JC, Afilaka B, et al. Hepatic resection is associated with reduced postoperative opioid requirement. J Anaesthesiol Clin Pharmacol 32 (2016): 307-313.
- Cozowicz C, Olson A, Poeran J, et al. Opioid prescription levels and postoperative outcomes in orthopedic surgery. Pain 158 (2017): 2422-2430.
- Murphy V, Koea J, Srinivasa S. The efficacy and safety of acetaminophen use following liver resection: a systematic review. HPB (Oxford) 22 (2022) 1-8.
