Impact of Admission SOFA Score and 48-Hour Delta SOFA on Clinical Outcomes of Critically Ill Patients
Article Information
Cristiana SQ Vasconcelos, Manuel D de La Cruz, Gabriel HLB Nascimento, José RA Azevedo*
Intensive Care Unit, Hospital Sao Domingos, Av. Jeronimo de Albuquerque, 540 - Bequimao, Sao Luís, Maranhao, 65060-645, Brazil
*Corresponding Author: José RA Azevedo, Intensive Care Unit, Hospital Sao Domingos, Av. Jeronimo de Albuquerque, 540 - Bequimao, Sao Luís, Maranhao, 65060-645, Brazil
Received: 30 July 2022; Accepted: 09 August 2022; Published: 25 August 2022
Citation: Cristiana SQ Vasconcelos, Manuel D de La Cruz, Gabriel HLB Nascimento, José RA Azevedo. Impact of Admission SOFA Score and 48- Hour Delta SOFA on Clinical outcomes of Critically Ill Patients. Anesthesia and Critical care 4 (2022): 143-148.
View / Download Pdf Share at FacebookAbstract
Background
Assessment of SOFA score, determined upon ICU admission, can identify patients at risk of unfavorable outcomes and trigger assessment and application of interventions, of which effectiveness can be evaluated by determining the SOFA score trend after 48 hours. Herein, we evaluated the impact of an admission SOFA score ≥ 2 and the 48-hour delta SOFA on critically ill patient outcomes.
Methods
This retrospective, observational cohort study included 1101 patients admitted to three ICUs of a tertiary hospital from January 01 to December 31, 2020. SOFA scores- determined upon ICU admission and 48 hours thereafter -denoted three patient groups: those with admission SOFA scores below 2 (n = 348), those with admission SOFA scores ≥ 2 whose 48-hour delta SOFA reflected improvement (SOFA after 48 hours < admission SOFA) (n = 415), and those with admission SOFA scores ≥ 2 that had increased or remained unchanged after 48 hours (SOFA after 48 hours ≥ admission SOFA) (n = 338).
Results
Group 1 patients were significantly younger and less severely ill and both ICU (3.4%) and hospital (8.6%) mortality were significantly lower than those of Group 2 and 3 patients. Among these, patients in Group 3 were older and had significantly higher mortality, both in the ICU (27.3% versus 10.1%, p < 0.001) and hospital (53.8% versus 14.9%, p < 0.001), compared to Group 2 patients.
Conclusion
We demonstrated that the admission SOFA score and 48-hour delta SOFA are predictors of prognosis in a nonselective cohort of critically ill patients.
Keywords
Critically ill, Mortality, Organ failures, Outcomes, SOFA score.
Critically ill articles; Mortality articles; Organ failures articles; Outcomes, SOFA score articles.
Critically ill articles Critically ill Research articles Critically ill review articles Critically ill PubMed articles Critically ill PubMed Central articles Critically ill 2023 articles Critically ill 2024 articles Critically ill Scopus articles Critically ill impact factor journals Critically ill Scopus journals Critically ill PubMed journals Critically ill medical journals Critically ill free journals Critically ill best journals Critically ill top journals Critically ill free medical journals Critically ill famous journals Critically ill Google Scholar indexed journals Mortality articles Mortality Research articles Mortality review articles Mortality PubMed articles Mortality PubMed Central articles Mortality 2023 articles Mortality 2024 articles Mortality Scopus articles Mortality impact factor journals Mortality Scopus journals Mortality PubMed journals Mortality medical journals Mortality free journals Mortality best journals Mortality top journals Mortality free medical journals Mortality famous journals Mortality Google Scholar indexed journals Organ failures articles Organ failures Research articles Organ failures review articles Organ failures PubMed articles Organ failures PubMed Central articles Organ failures 2023 articles Organ failures 2024 articles Organ failures Scopus articles Organ failures impact factor journals Organ failures Scopus journals Organ failures PubMed journals Organ failures medical journals Organ failures free journals Organ failures best journals Organ failures top journals Organ failures free medical journals Organ failures famous journals Organ failures Google Scholar indexed journals Outcomes articles Outcomes Research articles Outcomes review articles Outcomes PubMed articles Outcomes PubMed Central articles Outcomes 2023 articles Outcomes 2024 articles Outcomes Scopus articles Outcomes impact factor journals Outcomes Scopus journals Outcomes PubMed journals Outcomes medical journals Outcomes free journals Outcomes best journals Outcomes top journals Outcomes free medical journals Outcomes famous journals Outcomes Google Scholar indexed journals SOFA score articles SOFA score Research articles SOFA score review articles SOFA score PubMed articles SOFA score PubMed Central articles SOFA score 2023 articles SOFA score 2024 articles SOFA score Scopus articles SOFA score impact factor journals SOFA score Scopus journals SOFA score PubMed journals SOFA score medical journals SOFA score free journals SOFA score best journals SOFA score top journals SOFA score free medical journals SOFA score famous journals SOFA score Google Scholar indexed journals ICU articles ICU Research articles ICU review articles ICU PubMed articles ICU PubMed Central articles ICU 2023 articles ICU 2024 articles ICU Scopus articles ICU impact factor journals ICU Scopus journals ICU PubMed journals ICU medical journals ICU free journals ICU best journals ICU top journals ICU free medical journals ICU famous journals ICU Google Scholar indexed journals Multiple organ dysfunction syndrome articles Multiple organ dysfunction syndrome Research articles Multiple organ dysfunction syndrome review articles Multiple organ dysfunction syndrome PubMed articles Multiple organ dysfunction syndrome PubMed Central articles Multiple organ dysfunction syndrome 2023 articles Multiple organ dysfunction syndrome 2024 articles Multiple organ dysfunction syndrome Scopus articles Multiple organ dysfunction syndrome impact factor journals Multiple organ dysfunction syndrome Scopus journals Multiple organ dysfunction syndrome PubMed journals Multiple organ dysfunction syndrome medical journals Multiple organ dysfunction syndrome free journals Multiple organ dysfunction syndrome best journals Multiple organ dysfunction syndrome top journals Multiple organ dysfunction syndrome free medical journals Multiple organ dysfunction syndrome famous journals Multiple organ dysfunction syndrome Google Scholar indexed journals Length of stay articles Length of stay Research articles Length of stay review articles Length of stay PubMed articles Length of stay PubMed Central articles Length of stay 2023 articles Length of stay 2024 articles Length of stay Scopus articles Length of stay impact factor journals Length of stay Scopus journals Length of stay PubMed journals Length of stay medical journals Length of stay free journals Length of stay best journals Length of stay top journals Length of stay free medical journals Length of stay famous journals Length of stay Google Scholar indexed journals Area under the ROC curve articles Area under the ROC curve Research articles Area under the ROC curve review articles Area under the ROC curve PubMed articles Area under the ROC curve PubMed Central articles Area under the ROC curve 2023 articles Area under the ROC curve 2024 articles Area under the ROC curve Scopus articles Area under the ROC curve impact factor journals Area under the ROC curve Scopus journals Area under the ROC curve PubMed journals Area under the ROC curve medical journals Area under the ROC curve free journals Area under the ROC curve best journals Area under the ROC curve top journals Area under the ROC curve free medical journals Area under the ROC curve famous journals Area under the ROC curve Google Scholar indexed journals
Article Details
Introduction
Multiple organ dysfunction syndrome (MODS) is an important cause of morbidity and mortality in the intensive care unit (ICU). The Sequential Organ Failure Assessment (SOFA) score developed by Vincent et al. [1] sequentially assesses the presence and severity of dysfunction in six organ systems: respiratory, cardiovascular, hematological, hepatic, neurological, and renal. Although the score was developed to quantify organ dysfunction, the obvious relationship between organ dysfunction and mortality has been widely documented. Moreno et al. [2] demonstrated that SOFA score measurements correlated with patient outcomes. Jones et al. [3], analyzing 248 patients with severe sepsis and septic shock, demonstrated that the delta SOFA (SOFA score at 72 hours after ICU admission minus initial SOFA score) was strongly correlated with mortality. Anami et al. [4], analyzing 1164 patients admitted to an adult ICU, observed that mortality was significantly higher in patients whose score increased during hospitalization. Moreover, a prospective observational study showed that the initial SOFA score and 48-hour delta SOFA were important predictors of mortality [5]. Soo et al. [6] analyzed data from 20000 critically ill patients and identified a significant correlation between the admission SOFA score and the temporal rate of change in SOFA scores and mortality. Recently, a meta-regression analysis of 87 randomized controlled studies involving septic patients identified delta SOFA as a suitable measure for replacing mortality as an endpoint in clinical trials [7]. Determining the SOFA score upon ICU admission can identify patients at risk of unfavorable outcomes and trigger specific assessments and treatment approaches, the effectiveness of which can be assessed by determining the SOFA score trend after 48 hours. The primary objective of this study was to assess the impact of a SOFA score equal to or greater than two at ICU admission and the 48-hour delta SOFA score on hospital mortality. Second, it evaluated the correlation between mortality and the length of ICU stay, as well as the duration of mechanical ventilation and vasopressor drug administration.
Methods
This retrospective, observational cohort study was conducted in a tertiary hospital with 370 beds. The trial included nonpregnant patients aged above 18 years who were admitted to the medical ICU (29 beds), surgical ICU (13 beds), and trauma and high complexity surgical ICU (12 beds) for longer than two days from January 01 to December 31, 2020. Only a patient’s first admission to the ICU during the study period was considered. The study was approved by the Research Ethics Committee of Hospital São Domingos (approval number: 4.026.766, May 13, 2020), and the study protocol was registered at ClinicalTrials.gov (NCT04980274, July 27, 2021). Due to the study’s observational and retrospective nature, the requirement of obtaining informed consent was waived. Data from patients who met the inclusion criteria were obtained from the hospital’s electronic medical records and included age, sex, the Simplified Acute Physiology Score III (SAPS 3), and primary admission diagnosis, along with the SOFA score at admission and after 48 hours. Whenever the SOFA score was ≥ 2, the result was presented to the attending physician. After 48 hours, a new SOFA score was determined, while the prospective clinical surveillance team simultaneously identified interventions in the treatment plan to identify and treat the organ dysfunction that caused the trigger. This result was presented to the attending physician in the form of delta SOFA, that is, the difference between the SOFA scores at 48 hours postadmission and upon admission. Three groups of patients were identified based on their SOFA scores at admission and the 48-hour delta SOFA values: those with an admission SOFA score < 2 (Group 1, n = 348), those with an admission SOFA score ≥ 2 whose delta SOFA reflected improvement at the end of 48 hours after admission (SOFA after 48 hours < SOFA on admission) (Group 2, n = 415), and finally, those with an admission SOFA score ≥ 2 whose SOFA score increased or remained unchanged at the end of 48 hours postadmission (SOFA after 48 hours ≥ admission SOFA) (Group 3, n = 338).
Statistical Analysis
No sample size calculation was performed; the sample size was equal to the number of patients treated during the study period. Statistical analysis was performed using SPSS version 22.0 software (IBM Corp., Armonk, NY, USA). To assess the correlation between other variables (demographics, clinical, and outcomes) and the factors that determined patient grouping, we initially tested normality using the Shapiro-Wilk test. Variables with normality were further evaluated using analysis of variance (ANOVA) and Tukey's post hoc test, whereas ordinal and numerical variables without normality were evaluated using the nonparametric Kruskal-Wallis and Dunn's post hoc tests. Nominal variables, such as the diagnostic category and outcome in the ICU and hospital, were assessed using the chi-square test of independence. In comparing Groups 2 and 3, the Mann-Whitney U test was used to evaluate age, SAPS 3, SOFA at admission, duration of mechanical ventilation, length of ICU stay, and duration of vasopressor administration. For the variables mortality in the ICU and hospital, Pearson's chi-square test was applied. Receiver operating characteristic (ROC) curve analysis was conducted using the binary dependent variable, hospital mortality, and selecting the best cutoff of the clinically relevant independent variables to conduct univariate and multivariate logistic regression analysis. First, univariate analysis was conducted, after which the variables with a p-value below 0.20 were included in multivariate analysis. The survival curve was evaluated using the Kaplan-Meier test, considering the dependent variable, the outcome (discharge/death), and the temporal measures, length of ICU and hospital stay, with group (1 to 3) as the independent variable. All statistical tests were two-tailed, and p-values < 0.05 were considered significant.
Results
From January 01 to December 31, 2020, 1949 patients were admitted to any of the respective ICUs included in the study, of which 1101 were included in our analyses.
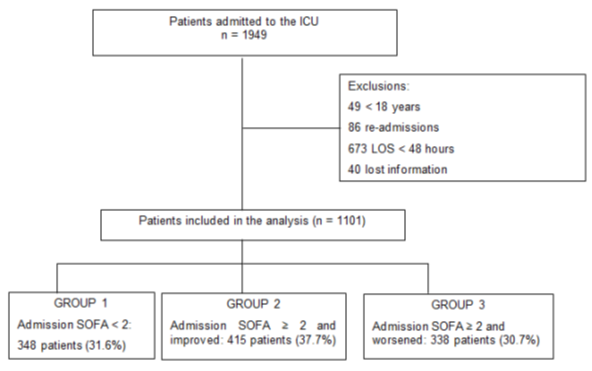
Figure 1: Flow chart of patients grouping
Table 1 shows the patients’ demographics, clinical characteristics, and outcomes among the three groups. Patients in group 1 were significantly younger and less severely ill- based on their SAPS 3 and admission SOFA scores- than those in groups 2 and 3. Their length of ICU stay was also comparatively shorter and mortality, both in the ICU (3.4%) and hospital (8.6%), was significantly lower than that of patients in groups 2 and 3.
|
Variable |
Group 1 (n = 348) |
Group 2 (n = 415) |
Group 3 (n = 338) |
p-value |
|
Age, median (IQR) |
63.5 ? (47-75) |
67.0b (55-78) |
72.0ª (62-81) |
<0.001 |
|
Female, n (%) |
170 (48.9) |
175 (42.2) |
150 (44.4) |
0.175 |
|
SAPS 3, median (IQR) |
38.0b (31-47) |
54.0ª (43-63) |
54.5ª (47-66) |
<0.001 |
|
Admission SOFA score, |
||||
|
Median (IQR) |
0.0b (0-1) |
4.0ª (3-7) |
4.0ª (3-6) |
<0.001 |
|
48 hours SOFA score, |
||||
|
median (IQR) |
3 (1-4) |
5 (3-8) |
<0.001 |
|
|
Diagnostic category |
||||
|
Respiratory, n (%) |
27 (7.8) |
31 (7.5) |
10 (3.0) |
|
|
Cardiovascular, n (%) |
58 (16.7) |
55 (13.3) |
56 (16.6) |
|
|
Neurological, n (%) |
35 (10.1) |
37 (8.9) |
30 (8.9) |
|
|
Gastrointestinal, n (%) |
50 (14.4) |
54 (13.0) |
26 (7.7) |
0.006 |
|
Renal, n (%) |
10 (2.9) |
15 (3.6) |
14 (4.1) |
|
|
Trauma, n (%) |
23 (6.6) |
18 (4.3) |
14 (4.1) |
|
|
Sepsis, n (%) |
125 (35.9) |
185 (44.6) |
172 (50.9) |
|
|
Others, n (%) |
20 (5.7) |
20 (4.8) |
16 (4.7) |
|
|
Length of stay |
||||
|
ICU, median (IQR) |
4 (3-6) |
7 (4-13) |
7 (4-15) |
<0.001 |
|
Mortality |
||||
|
ICU, n (%) |
12 (3.4) |
42 (10.1) |
93 (27.5) |
<0.001 |
|
Hospital, n (%) |
30 (8.6) |
62 (14.9) |
182 (53.8) |
<0.001 |
abc- Lowercase alphabet letters denote p < 0.05, determined using the Dunn test.
SAPS 3: Simplified Acute Physiology Score III; SOFA: Sequential Organ Failure Assessment; IQR: interquartile range
Table 1: Demographic data, clinical characteristics and outcomes
In table 2, we compare data from groups 2 and 3. Neither the SAPS 3 score, nor the SOFA score on admission, indicated any significant difference in severity between the two groups. There were also no differences between the groups in terms of length of ICU stay and duration of mechanical ventilation. Patients in group 3 were older and presented with significantly higher mortality, both in the ICU (27.5 versus 10.1%, p < 0.001) and the hospital (53.8% versus 14.9%, p < 0.001), compared to group 2 patients.
|
Variable |
Group 2 (n = 415) |
Group 3 (n = 338) |
p-value |
|
Age, y median (IQR) |
67 (55-78) |
72 (62-81) |
<0.001 |
|
SAPS 3, median (IQR) |
54 (43-63) |
54.5 (47-66) |
0.013 |
|
SOFA D1, median (IQR) |
4 (3-7) |
4 (3-6) |
0.11 |
|
Duration of MV, d |
|||
|
median (IQR) |
10 (5-22) |
12 (5-24) |
0.021 |
|
Duration of ICU stay, d |
|||
|
median (IQR) |
7 (4-13) |
7 (4-15) |
0.623 |
|
Duration of VAD, d |
|||
|
median (IQR) |
3 (1-5) |
3 (2-8) |
0.051 |
|
Mortality |
|||
|
ICU, n (%) |
42 (10.1) |
93 (27.5) |
<0.001 |
|
Hospital, n (%) |
62 (14.9) |
182 (53.8) |
<0.001 |
SAPS 3: Simplified Acute Physiology Score III; SOFA: Sequential Organ Failure Assessment; MV: mechanical ventilation; VAD: vasoactive drugs; IQR: interquartile range
Table 2: Demographic and outcomes data between groups 2 and 3
Multivariate logistic regression analysis of hospital mortality, after adjusting for independent covariates, showed statistical significance of the Charlson Comorbidity Index (p < 0.001), vasopressor use for more than 2.5 days (p < 0.001), and the use of invasive ventilatory support (p < 0.001). Figures 2 and 3 present Kaplan–Meier survival curves of patients in the three groups, indicating that ICU and hospital survival was expressively lower in group 3 than in groups 1 and 2.
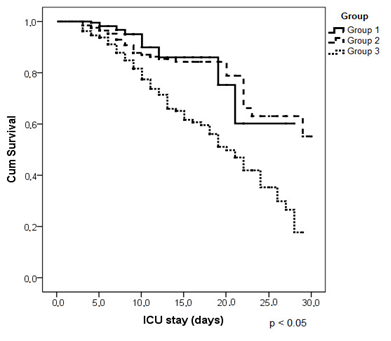
Figure 2: ICU survival curve
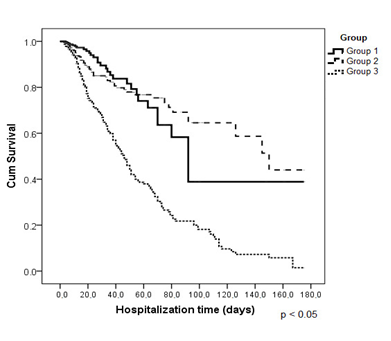
Figure 3: Hospital survival curves
Discussion
In this retrospective, observational cohort study, we found that the admission SOFA score and 48-hour delta SOFA score were predictors of prognosis in a heterogeneous population of critically ill patients. Multivariate analysis showed an independent association between age ≥ 66 years, the Charlson Comorbidity Index, prolonged vasopressor use, and hospital mortality. The Kaplan-Meier survival curves showed that ICU and hospital survival were expressively lower in patients whose SOFA scores remained unchanged or worsened after 48 hours, compared to those whose scores improved. A high admission SOFA score can be used in decision-making related to identifying sources of severity and suitable interventions. SOFA score reassessment as early as 48 hours after admission allows for evaluation of the effectiveness of interventions- with a score reduction reflecting an effective therapeutic approach- and outcome prediction. As recommended by Moreno et al. [2], the SOFA score should be evaluated, not only with regard to ICU outcomes but also pertaining to longer-term outcomes. Moreover, Jones et al. [3] showed that an increase in the SOFA score within the first 72 hours after admission was associated with 35% mortality, whereas any SOFA score decrease during the same time frame correlated with 10% mortality. Ferreira et al. [8] studied 352 patients hospitalized in a medical ICU and demonstrated that the mean SOFA score and delta SOFA were strongly associated with patient outcomes. They showed that a decreasing SOFA score in the first 48 hours after admission was associated with 6% mortality, while in patients whose SOFA scores remained unchanged or showed an increase, mortality exceeded 50%. These authors suggested that delta SOFA can translate patients’ responses to therapeutic strategies, allowing the clinician to assess response to treatment. In a cohort of patients with severe sepsis and septic shock, SOFA scores determined on day 3 after admission displayed an area under the ROC curve (AUROC) = 0.68 (95% CI 0.56–0.79), whereas a 50% SOFA decrease was associated with 61.3% sensitivity and 85.9% negative predictive value concerning ICU mortality [5]. The results of a study by Anami et al. [4] and a cohort study of critically ill patients in Canada [6] revealed mortality rates similar to those identified in our study. However, it should be emphasized that the mortality results in our study were influenced by interventions conducted subsequent to the attending physician being made aware that a SOFA score ≥ 2 had been measured. A meta-analysis of 87 randomized controlled trials, using different derivatives of the SOFA score, showed that only delta SOFA significantly correlated with mortality and was therefore best suited for use by researchers as a trial endpoint, in preference to fixed-day SOFA [7]. Some studies comparing subgroups of patients also showed the significant impact of worsening evolution of the SOFA score on mortality. Fuchs et al. [9] compared surgical and nonsurgical patients and showed that significantly higher baseline SOFA scores in nonsurgical patients translated into higher mortality. Furthermore, Huang et al. [10] identified the SOFA score as an independent predictor of long-term mortality in patients with acute myocardial infarction. There is growing interest in using the SOFA score, rather than the mortality rate, as an endpoint in clinical trials. The SOFA score would allow for analysis of an outcome within a shorter time frame, in addition to eliminating determinants that cannot be resolved by the therapeutic intervention. Furthermore, the European Medicines Agency determined that, in sepsis-related clinical trials, changes in organ dysfunction scores are valid outcomes [11]. Thus, changes in the SOFA score have been increasingly adopted as the primary endpoint in interventional trials. In a study evaluating the effect of levosimendan compared to a placebo, in patients with septic shock, the primary endpoint was to detect an absolute difference in the mean SOFA score of at least 0.5 between the two groups [12]. Another study comparing use of meropenem alone or in combination with moxifloxacin in patients with severe sepsis aimed to demonstrate a minimum1-point difference in mean SOFA scores between the two groups [13]. Concerning the strengths of this study, we analyzed a significant heterogeneous population of critically ill patients. Although analyzed retrospectively, the data used in the analyses were collected prospectively within the respective clinical surveillance protocols. Therefore, all data required for the analyses were systematically collected during the patients’ stay in the ICU. Whenever the SOFA score was ≥ 2, the result was presented to the attending physician, while the protocol team simultaneously identified interventions in the treatment plan to identify and treat the organ dysfunction that initially caused the trigger. However, our study also has certain limitations. First, this is a single-center trial conducted in only three ICUs. Second, the therapeutic interventions aimed at identifying and treating the relevant organ dysfunction, were not systematized and were performed at the discretion of the attending physician. Finally, the hospital where the study was conducted only serves patients with health insurance, potentially limiting the generalizability of the results beyond the socioeconomic reality of the studied population.
Conclusion
In this retrospective observational cohort study, we demonstrated that the admission SOFA score and 48-hour delta SOFA are predictors of prognosis in a nonselective cohort of critically ill patients.
Abbreviations
MODS: Multiple organ dysfunction syndrome
ICU: Intensive care unit
SOFA: Sequential Organ Failure Assessment
SAPS 3: Simplified Acute Physiology Score III
ROC: Receiver operating characteristic
LOS: Length of stay
AUROC: Area under the ROC curve
Declarations
Ethics approval and consent to participate
This study was approved by the Research Ethics Committee of Hospital Sao Domingos, approval number: 4.026.766 (May 13, 2020). Due to the study’s observational and retrospective nature, the requirement of obtaining informed consent was waived.
Consent for publication
Not applicable
Availability of data and materials
The dataset used and/or analyzed during the current study is available from the corresponding author on reasonable request.
Competing interests
The authors declare that they have no competing interests.
Funding
None declared
Authors' contributions
Conceptualization (CSQV, MDC, GHLBN, JRAA); Methodology (CSQV, MDC, JRAA); Data collection and analysis (GHLBN, MDC, CSQV); Original draft preparation (DDC, CSQV, GHLBN); Supervision (JRAA). All authors have read and approved the manuscript.
Acknowledgements
Not applicable
Highlights
Determining the SOFA score upon ICU admission can identify patients at risk of unfavorable outcomes and trigger specific assessments and treatment approaches Critically ill patients with ICU admission SOFA ≥ 2 that improved SOFA score after 48 hours had expressively higher ICU and hospital survival rate compared to those with 48-hour SOFA ≥ admission SOFA.
References
- Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the European Society of Intensive Care Medicine. Intensive Care Med 22 (1996): 707-710.
- Moreno R, Vincent JL, Matos R, et al. The uses of maximum SOFA score to quantify organ dysfunction/failure in intensive care: results of a prospective multicenter study. Intensive Care Med 25 (1999): 686-696.
- Jones AE, Trzeciak S, Kline JA. The sequential organ failure assessment score for predicting outcome in patients with severe sepsis and evidence of hypoperfusion at the time of emergency department presentation. Crit Care Med 37 (2009): 1649-1654.
- Anami EHT, Grion CMC, Cardoso LTQ, et al. Serial evaluation of SOFA score in a Brazilian teaching hospital. Intensive Crit Care Nurs 26 (2010): 75-82.
- De Azevedo JR, Torres OJ, Beraldi RA, et al. Prognostic evaluation of severe sepsis and septic shock: Procalcitonin clearance vs ? Sequential Organ Failure Assessment. J Crit Care 30 (2015): 219-221.
- Soo A, Zuege DJ, Fick GH, et al. Describing organ dysfunction in the intensive care unit: a cohort study of 20,000 patients. Crit Care 23 (2019): 186.
- De Grooth HJ, Geenen IL, Girbes AR, et al. SOFA and mortality endpoints in randomized controlled trials: a systematic review and meta-regression analysis. Crit Care 21 (2017): 38.
- Ferreira FL, Bota DP, Bross A, et al. Serial Evaluation of the SOFA Score to Predict Outcome in Critically Ill Patients. JAMA 286 (2001): 1754- 1758.
- Fuchs PA, Czech IJ, Krzych LJ. Mortality Prediction Using SOFA Score in Critically Ill Surgical and Non-Surgical Patients: Which Parameter Is the Most Valuable? Medicina 56 (2020): 273
- Huang SS, Chen YH, Lu TM, et al. Application of the Sequential Organ Failure Assessment score for predicting mortality in patients with acute myocardial infarction. Resuscitation 85 (2012): 591-595.
- Guidelines for the clinical investigation of medicinal products for treatment of sepsis. European Medicines Agency- Evaluation of Medicines for Human Use; CHMP/EWP/4713/03 (2006).
- Gordon AC, Perkins GD, Singer M, et al. Levosimendan for the prevention of acute organ dysfunction in sepsis. N Engl J Med 375 (2016): 1638-1648.
- Brunkhorst FM, Oppert M, Marx G, et al. Effect of empirical treatment with moxifloxacin and meropenem vs meropenem on sepsis-related organ dysfunction in patients with severe sepsis: a randomized trial. JAMA 307 (2012): 2390-2399.
