Impact of 3-D Virtual Reality Visualization on Patient Education, Engagement, and Satisfaction in Pre-surgical Consultation
Article Information
Matthew Z Sun MD1, Sophie M Peeters MD1, Anthony C Wang MD1
Department of Neurosurgery, University of California Los Angeles, Los Angeles, CA, USA
*Corresponding author: Anthony C. Wang M.D., UCLA Department of Neurosurgery, 300 Stein Plaza, Suite 520
Los Angeles, CA 90095, USA
Received: 03 August 2021; Accepted: 10 August 2021; Published: 01 December 2021
Supplementary File
Citation:
Matthew Z Sun MD, Sophie M Peeters MD, Anthony C Wang MD. Impact of 3-D Virtual Reality Visualization on Patient Education, Engagement, and Satisfaction in Pre-surgical Consultation. Journal of Surgery and Research 4 (2021): 711-722.
View / Download Pdf Share at FacebookAbstract
Background
Effective physician-patient communication is a key component of the therapeutic relationship. Recently, virtual reality has emerged as a novel communications tool in healthcare.
Objective
To evaluate the impact of the Surgical Theater 360-degree virtual reality (360°VR) visualization platform on patient education, engagement, and satisfaction in pre-surgical consultations.
Methods
Forty-seven consecutive patients were prospectively surveyed for their pre-surgical consultation experience that incorporated 360°VR renderings created from patient-specific cross-sectional imaging. Patients anonymously completed an online questionnaire that used a 5-point Likert scale or a 10-point value scale (1 = “no value” to 10 = “highly valuable”) regarding their 360°VR and prior consultations. Wilcoxon Signed Rank Test was used to compare responses for prior versus 360°VR consultations.
Results
More than 90% of the patients gave the highest possible rating regarding physician communication and overall satisfaction during the 360°VR consultation. Patients’ responses regarding how well the neurosurgeon explained their medical condition to them, as well as how satisfied they were with their consultation, were significantly more positive for the 360°VR consultation than for previous consultations (p < 0.001). More than 90% of the patients agreed that 360°VR helped improve their understanding of their condition, their ability to weigh the different management options, their comfort level with the proposed management option, and 96% agreed that they selected a management option together with their neurosurgeon during the 360°VR consultation.
Virtual reality, Communication, Satisfaction, Education, Surgical consultationKeywords
Virtual reality articles; Communication articles; Satisfaction articles; Education articles; Surgical consultation articles
Virtual reality articles Virtual reality Research articles Virtual reality review articles Virtual reality PubMed articles Virtual reality PubMed Central articles Virtual reality 2023 articles Virtual reality 2024 articles Virtual reality Scopus articles Virtual reality impact factor journals Virtual reality Scopus journals Virtual reality PubMed journals Virtual reality medical journals Virtual reality free journals Virtual reality best journals Virtual reality top journals Virtual reality free medical journals Virtual reality famous journals Virtual reality Google Scholar indexed journals Communication articles Communication Research articles Communication review articles Communication PubMed articles Communication PubMed Central articles Communication 2023 articles Communication 2024 articles Communication Scopus articles Communication impact factor journals Communication Scopus journals Communication PubMed journals Communication medical journals Communication free journals Communication best journals Communication top journals Communication free medical journals Communication famous journals Communication Google Scholar indexed journals Satisfaction articles Satisfaction Research articles Satisfaction review articles Satisfaction PubMed articles Satisfaction PubMed Central articles Satisfaction 2023 articles Satisfaction 2024 articles Satisfaction Scopus articles Satisfaction impact factor journals Satisfaction Scopus journals Satisfaction PubMed journals Satisfaction medical journals Satisfaction free journals Satisfaction best journals Satisfaction top journals Satisfaction free medical journals Satisfaction famous journals Satisfaction Google Scholar indexed journals Education articles Education Research articles Education review articles Education PubMed articles Education PubMed Central articles Education 2023 articles Education 2024 articles Education Scopus articles Education impact factor journals Education Scopus journals Education PubMed journals Education medical journals Education free journals Education best journals Education top journals Education free medical journals Education famous journals Education Google Scholar indexed journals Surgical consultation articles Surgical consultation Research articles Surgical consultation review articles Surgical consultation PubMed articles Surgical consultation PubMed Central articles Surgical consultation 2023 articles Surgical consultation 2024 articles Surgical consultation Scopus articles Surgical consultation impact factor journals Surgical consultation Scopus journals Surgical consultation PubMed journals Surgical consultation medical journals Surgical consultation free journals Surgical consultation best journals Surgical consultation top journals Surgical consultation free medical journals Surgical consultation famous journals Surgical consultation Google Scholar indexed journals patient communication gap articles patient communication gap Research articles patient communication gap review articles patient communication gap PubMed articles patient communication gap PubMed Central articles patient communication gap 2023 articles patient communication gap 2024 articles patient communication gap Scopus articles patient communication gap impact factor journals patient communication gap Scopus journals patient communication gap PubMed journals patient communication gap medical journals patient communication gap free journals patient communication gap best journals patient communication gap top journals patient communication gap free medical journals patient communication gap famous journals patient communication gap Google Scholar indexed journals medical therapy and rehabilitation articles medical therapy and rehabilitation Research articles medical therapy and rehabilitation review articles medical therapy and rehabilitation PubMed articles medical therapy and rehabilitation PubMed Central articles medical therapy and rehabilitation 2023 articles medical therapy and rehabilitation 2024 articles medical therapy and rehabilitation Scopus articles medical therapy and rehabilitation impact factor journals medical therapy and rehabilitation Scopus journals medical therapy and rehabilitation PubMed journals medical therapy and rehabilitation medical journals medical therapy and rehabilitation free journals medical therapy and rehabilitation best journals medical therapy and rehabilitation top journals medical therapy and rehabilitation free medical journals medical therapy and rehabilitation famous journals medical therapy and rehabilitation Google Scholar indexed journals medical education articles medical education Research articles medical education review articles medical education PubMed articles medical education PubMed Central articles medical education 2023 articles medical education 2024 articles medical education Scopus articles medical education impact factor journals medical education Scopus journals medical education PubMed journals medical education medical journals medical education free journals medical education best journals medical education top journals medical education free medical journals medical education famous journals medical education Google Scholar indexed journals immersive VR simulation articles immersive VR simulation Research articles immersive VR simulation review articles immersive VR simulation PubMed articles immersive VR simulation PubMed Central articles immersive VR simulation 2023 articles immersive VR simulation 2024 articles immersive VR simulation Scopus articles immersive VR simulation impact factor journals immersive VR simulation Scopus journals immersive VR simulation PubMed journals immersive VR simulation medical journals immersive VR simulation free journals immersive VR simulation best journals immersive VR simulation top journals immersive VR simulation free medical journals immersive VR simulation famous journals immersive VR simulation Google Scholar indexed journals pre-operative planning articles pre-operative planning Research articles pre-operative planning review articles pre-operative planning PubMed articles pre-operative planning PubMed Central articles pre-operative planning 2023 articles pre-operative planning 2024 articles pre-operative planning Scopus articles pre-operative planning impact factor journals pre-operative planning Scopus journals pre-operative planning PubMed journals pre-operative planning medical journals pre-operative planning free journals pre-operative planning best journals pre-operative planning top journals pre-operative planning free medical journals pre-operative planning famous journals pre-operative planning Google Scholar indexed journals
Article Details
1. Introduction
Effective physician-patient communication is at the heart of medicine because it is essential for building the crucial therapeutic relationship between the physician and the patient. Shared medical decision making depends on effective physician-patient communication. Nowhere is this truer than in neurosurgery, where patients by necessity have to develop their trust in their neurosurgeons to treat potentially life-threatening conditions. Lack of sufficient understanding of neurosurgical condition can not only lead to increased apprehension and overall dissatisfaction [1], but also decreased ability to make a truly informed decision weighing the risks and benefits of the proposed treatment plan. Thus, the need to bridge the physician-patient communication gap is critical [2,3].
Proper patient education regarding complex neurosurgical conditions can be particularly challenging. While various methods have been proposed and trialed in the past, advancement in display technology has allowed the possibility of supplementing verbal information with visual information to improve understanding and retention of medical information by patients [4,5]. In recent years, virtual reality (VR) has emerged as a promising tool in science and medicine [6]. The technological advancements of VR have made it increasingly affordable and accessible, and its applicability as a medical tool is gaining wide acceptance in the medical community. VR is being developed for a wide range of applications in healthcare including preventive medicine and patient education [7], medical therapy and rehabilitation [8,9], medical education and training [10-14], and surgery [6,15-17].
The Surgical Theater Precision VRTM visualization platform is one such technology capable of creating personalized, custom 360-degree VR (360°VR) models from high-resolution cross-sectional imaging within a few minutes. These 360°VR models can be manipulated and viewed at any angle at high resolution, and by using VR headsets, the 360°VR models can be viewed in an immersive VR simulation.
For neurosurgery, 360°VR technology enables interactive planning and simulation of neurosurgical procedures that can be utilized in educational and clinical applications [12,14-17]. Pre-operative rehearsal with 360°VR has been shown to increase safety and efficiency of aneurysm clipping [17]. Use of VR for pre-operative planning and intra-operative guidance have also been proposed.
Here, we aim to assess the potential impact of 360°VR visualization on patient communication, patient education, engagement, and satisfaction. To our knowledge, this is the first report of enhanced patient education, engagement, and satisfaction as a result of immersive VR technology incorporated into neurosurgical consultation.
2. Methods
Institutional Review Board approval was obtained (UCLA IRB#17-000402) to conduct a prospective anonymous patient survey study. All new-patient evaluations for operative cerebrovascular conditions in one neurosurgeon’s outpatient clinic over a 6-month period were screened for inclusion in this study. Prior to consultation, 360°VR renderings of magnetic resonance imaging (MRI) and/or computed tomography (CT) images were generated using proprietary software included with the Surgical Theater Precision VRTM visualization platform. MR angiography and/or CT angiography studies were used (Figure 1). Patients with adequate high-resolution cross-sectional imaging underwent neurosurgical consultation with the use of 360°VR, and at its conclusion, patients were recruited for participation in this study. Patients were asked to complete an anonymous survey (Supplemental Figure 1) after the neurosurgeon had exited the room by a study coordinator, and the neurosurgeon was blinded to patient participation and responses. Patients were told that neither the participation in the survey nor the individual responses would have any impact on the care of patient. Verbal consent was obtained prior to administering the survey. A legal guardian or next-of-kin was asked to complete the survey if patients were mentally unable to participate in the study, or under the age of 16. No patient had previously attended a VR-facilitated consultation.
A 5-point Likert scale (1 = “strongly disagree” to 5 = “strongly agree”) was used for all questions, except for one question in which patients were asked to rate the value of the 360°VR experience on a 10-point scale. For the 10-point scale question, the mean rating ±1 standard deviation was calculated.
Using RStudio (Version 1.1.442, RStudio, Inc. Boston, MA), the Wilcoxon Signed Rank Test was performed to compare patient-matched pre and post 360°VR consultation scores (Table 2). The V-statistic and the p-values are reported for each comparison. Kendall’s tau coefficient was calculated to assess the correlation between the change in patients’ scoring of how well their physician communicated with them before and after their 360°VR consultation and each of the following: patient’ age, gender, ethnicity, level of education, and type of insurance. Kendall’s tau coefficient was also calculated between the change in patients’ scoring of their overall satisfaction with the consultation before and after their 360°VR consultation and each of the following: patient’ age, gender, ethnicity, level of education, and type of insurance.
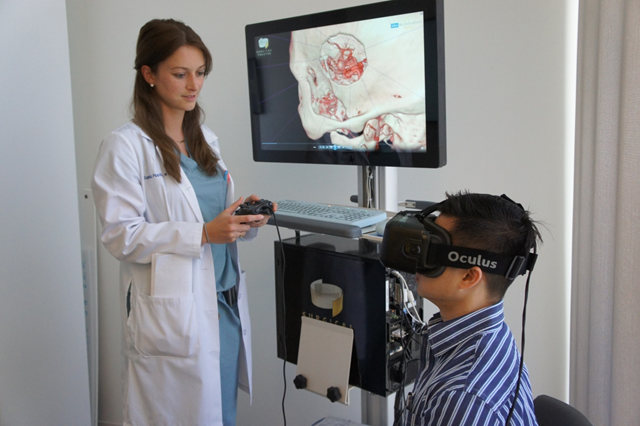
Figure 1: The 360°VR Platform.
A: An example of a high resolution cross-sectional study that was used to construct a 360°VR model.
B: The resultant 360°VR model of the CT angiography can be viewed from any angle.
C: The 360°VR model can be manipulated to reveal certain cross sections
D: The 360°VR model can be used to show only the vascular anatomy.
E: In clinic, a patient can wear the VR headset (left) and be guided by the neurosurgeon during the consultation to view his own neurosurgical anatomy (right).
3. Results
3.1 Physician-Patient communication and patient satisfaction
All patients who presented as new consultations utilizing the 360°VR technology (Figure 1) were screened for inclusion in this study, and of those who were screened, all 47 patients (100% of those who were eligible) consented to participate in this study (Supplemental Figure 1). None of these patients experienced the 360°VR technology in a clinical setting before. Table 1 summarizes the demographic information of the 47 respondents.
Patients were asked about how well their physicians communicated with them with the following 2 questions: 1) “Prior to this visit, my physician(s) explained my medical condition well,” and 2) “My neurosurgeon explained my medical condition well today.” For the 360°VR consultations, 91% patients strongly agreed that their medical condition was explained to them in a way that they could understand, whereas only 64% strongly agreed for the prior consultations. Overall, patient responses regarding how well the neurosurgeon explained their medical condition to them were more positive for the 360°VR consultation than for previous consultations (mean score of 4.91 versus 4.34). Wilcoxon signed rank test showed a statistically significant difference between patient ranks for the 360°VR consultation and prior consultations (V = 5.5, p = 0.00057) (Figure 2). A total of 47 patients participated in the study. Their gender, age, race/ethnicity, education level, insurance type, medical condition for the neurosurgical consultation, and the number of prior neurosurgical consultations in the year before were surveyed.
|
Patient Characteristic |
Number of Patients (n = 47) (%) |
|
Gender |
|
|
Male |
12 (26%) |
|
Female |
35 (74%) |
|
Age Group |
|
|
0-20 |
3 (6%) |
|
21-40 |
13 (28%) |
|
41-60 |
16 (34%) |
|
61+ |
15 (32%) |
|
Race/Ethnicity |
|
|
White/Caucasian |
23 (49%) |
|
Hispanic/Latino |
11 (23%) |
|
Asian/Pacific Islander |
10 (21%) |
|
Black/African American |
3 (6%) |
|
Education Level |
|
|
Earlier than high school |
2 (4%) |
|
High school graduate |
14 (30%) |
|
College degree or more |
31 (66%) |
|
Insurance Type |
|
|
Medicaid/ MediCal |
1 (2%) |
|
Medicare |
6 (13%) |
|
Self Pay |
2 (4%) |
|
PPO/ HMO |
32 (68%) |
|
PPO/ HMO & Medicare |
5 (11%) |
|
Did not answer |
1 (2%) |
|
Medical Condition |
|
|
Aneurysm/AVM/ Cavernous malformation/ Moyamoya/ Other vascular pathology |
42 (89%) |
|
Tumor/Other mass |
4 (9%) |
|
Did not answer |
1 (2%) |
|
No. of Prior Neurosurgical Consultations in 2016-2017 |
|
|
1-2 |
38 (81%) |
|
3-5 |
6 (13%) |
|
6+ |
3 (6%) |
Table 1: Patient Demographics Information
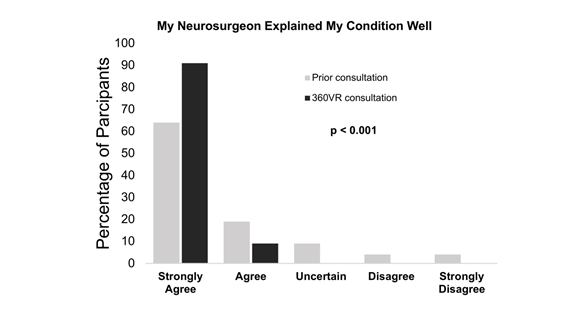
Figure 2: Comparison of Neurosurgeon’s Communication in Prior versus 360°VR Consultation
Patients were also asked how satisfied they were with their consultations. Among respondents, 94% of patients strongly agreed that they were satisfied with the 360°VR consultation, whereas only 64% were strongly satisfied with their prior consultations. Mean patient satisfaction was higher for the 360°VR consultation (4.94 versus 4.26), and a Wilcoxon signed rank test indicated that patient satisfaction from the 360°VR consultation was significantly higher compared to prior consultations (V = 3, p = 0.00069) (Figure 3). The summary of the responses is presented in Table 2. To assess whether there are confounding factors influencing how patients may perceive a difference in their physician’s communication before and after the 360°VR consultation, Kendall’s tau coefficients were calculated for how well patients’ ratings changed before and after 360°VR regarding their physicians’ communication correlated with various potential confounding factors, including patients’ age, gender, ethnicity, level of education, and type of insurance. Additionally, Kendall’s tau coefficients were calculated for how well patients’ ratings changed before and after 360°VR regarding their overall satisfaction correlated with the same set of potential confounding factors. We found that there were no statistically significant correlations between the change in responses to patient communication and satisfaction with their consultations and patients’ age, gender, ethnicity, level of education, or type of insurance (all p-values > 0.05). Percentages of patients who rated how well their neurosurgeon communicated and their level of satisfaction in prior versus 360°VR consultation (n = 47). Wilcoxon signed rank test showed statistically significant differences between patient ranks for the 360°VR consultation and prior consultations for both communication and satisfaction (p < 0.001).
|
My neurosurgeon explained my medical condition well (%) |
Strongly Agree |
Agree |
Uncertain |
Disagree |
Strongly Disagree |
|
5 |
4 |
3 |
2 |
1 |
|
|
Prior consultation |
64 |
19 |
9 |
4 |
4 |
|
360°VR consultation |
91 |
9 |
0 |
0 |
0 |
|
Satisfaction with my consultation (%) |
Strongly Agree |
Agree |
Uncertain |
Disagree |
Strongly Disagree |
|
5 |
4 |
3 |
2 |
1 |
|
|
Prior consultation |
64 |
13 |
13 |
6 |
4 |
|
360°VR consultation |
94 |
6 |
0 |
0 |
0 |
Table 2: Comparison of Patient Communication and Satisfaction in Prior versus 360°VR Consultation.
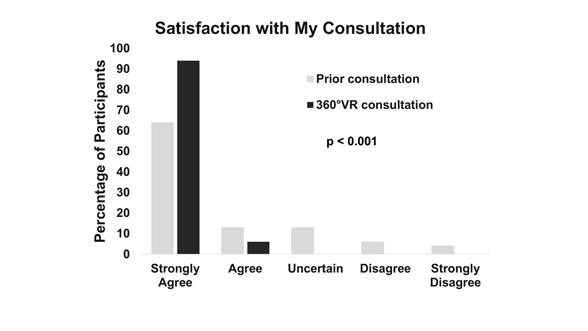
Figure 3: Comparison of Patient Satisfaction in Prior versus 360°VR Consultation
3.2 360°VR consultation experience
Patients were also surveyed more specifically on their 360°VR experience with the following three questions: 1) “Experiencing 360°VR images helped improve my understanding of my medical condition,” 2) “Experiencing 360°VR images helped improve my comfort level with my proposed management option,” and 3) “How would you rate the value of seeing your images using 360°VR?” All patients either strongly agreed (94%) or agreed (6%) that 360°VR helped improve understanding of their medical condition (Table 3). Similarly, 91% strongly agreed, and 9% agreed, that the 360°VR experience helped improve their comfort level with the proposed management options. Importantly, patients rated the value of experiencing 360°VR highly with a mean score of 9.79 ± 0.51 (1 standard deviation) on a scale of 1 to 10, with 1 being “no value” and 10 as “highly valuable” (Table 4).
|
360VR Experience (n = 47) |
Strongly Agree |
Agree |
Uncertain |
Disagree |
Strongly Disagree |
|
5 |
4 |
3 |
2 |
1 |
|
|
Experiencing 360VR images helped improve my understanding of my medical condition. |
94% (44) |
6% (3) |
0% (0) |
0% (0) |
0% (0) |
|
Experiencing 360VR images helped improve my comfort level with my proposed management option. |
91% (43) |
9% (4) |
0% (0) |
0% (0) |
0% (0) |
Table 3: Impact of 360°VR on patient understanding and comfort with management options.
|
Highly Valuable |
||||||||||
|
10 |
9 |
8 |
7 |
6 |
5 |
4 |
3 |
2 |
1 |
|
|
Value of 360VR experience (n = 47) |
83% (39) |
13% (6) |
4% (2) |
0% (0) |
0% (0) |
0% (0) |
0% (0) |
0% (0) |
0% (0) |
0% (0) |
Table 4: Patient Perceived Value of 360°VR in Consultation
3.3 Shared decision making
To assess shared decision making from the patient’s point of view, patients were asked whether or not they agreed with the following statements: 1) “My surgeon and I thoroughly weighed the different management options today,” and 2) “My surgeon and I selected a management option together.” For the former statement, 85% strongly agreed, and 15% agreed (Table 5). For the latter statement, 81% strongly agreed, 15% agreed, and 4% were uncertain.
|
Shared Decision Making (n = 47) |
Strongly agree |
Agree |
Uncertain |
Disagree |
Strongly disagree |
|
5 |
4 |
3 |
2 |
1 |
|
|
My surgeon and I thoroughly weighed the different management options today. |
85% (40) |
15% (7) |
0% (0) |
0% (0) |
0% (0) |
|
My surgeon and I selected a management option together. |
81% (38) |
15% (7) |
4% (2) |
0% (0) |
0% (0) |
Table 5: Perception of shared decision making
5. Discussion
Patient-centered care has become a principle focus of healthcare as growing evidence shows that orienting care around patients’ needs and preferences has the potential to not only improve patient satisfaction but also has a positive effect on clinical outcomes [18-21]. In 2001, the Institute of Medicine named patient-centered care as one of the six fundamental aims of the United States of America (U.S.) healthcare system [22]. Moreover, the economic value of patient-centered care is increasingly being recognized as the healthcare landscape in the U.S. is transitioning to a value-based payment system, in which reimbursement is tied to patient experience and satisfaction [23]. Specifically, the Centers for Medicare and Medicaid Services (CMS) Value-Based Purchasing Program places emphasis on Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey, which scores hospitals solely based on patient experience. In the present study, a patient-centered care approach is taken to educate and engage patients using a 3D virtual reality visualization platform (360°VR) during neurosurgical consultations for complex cerebrovascular and brain tumor pathologies. As a result, patients reported that compared to prior consultations, the neurosurgeon using the 360°VR technology explained their medical condition better, and reported higher level of satisfaction with their overall neurosurgical consultation. Patients also found that the 360°VR experience improved their understanding of their medical condition, as well as their comfort level with the proposed treatment options. These reported outcomes suggest that the 360°VR consultation may help patients be better informed about their medical condition and experience less anxiety and apprehension about the proposed treatment option. Patients also expressed that they felt more involved in a shared decision-making process during their 360°VR consultation, with 85% strongly agreeing that they thoroughly weighed the different treatment options with the neurosurgeon. Consequently, 96% of patients agreed that they selected a treatment option together with the neurosurgeon. More involvement in a shared decision-making process may reflect more comprehensive understanding of the proposed treatment plan and has been associated with overall satisfaction with provided care24-26. Furthermore, shared decision making has been shown to enhance patient-centered care along with patient safety and is considered a part of value-based care in the U.S. [27]. There are several limitations to this study that should be addressed. First, the exciting nature of VR and a new technology in this space may have influenced the positive feedback from patients. Second, satisfaction and physician communication ranks for the 360°VR consultation were compared to the ranks for previous consultations. The number of prior consultations ranged from one to six or more, and thus, a variety of different neurosurgeons were involved. However, their differences were not accounted for in this study. Recall bias, at least, could not be controlled in this study. Our study is the first to address the question of whether allowing a neurosurgical patient to see in 3D not only the complex anatomy of their own neurosurgical disease but also the specific surgical approach, would facilitate patient education, increase the perception of shared-decision making with their surgeon, and increase overall satisfaction with their pre-operative satisfaction. It adds to the existing literature that the VR platform when used in the neurosurgical setting may increase patient satisfaction experience in general, even when it doesn’t involve surgical planning and explanation of anatomy. For instance, The Thomas Jefferson University Hospital performed a randomized controlled trial in which patients watched a VR video describing the pre-operative and the postoperative experience on the day of the surgery using actors, real physicians and nurses [30]. The authors found that patients who were exposed to preoperative VR reported increased satisfaction and less anxiety. In addition to improving patient experience which can translate to mproving patient-centered care outcome measures such as the HCAHPS scores used by the CMS, the VR platform also has the potential to improve rates of surgical conversion and patient retention28. The VR platform can also play an important role in increasing patient retention rate, which is the percent of patients who were recommended surgery in clinic that eventually underwent surgery with the same surgeon. For example, two recent studies have demonstrated a high patient retention rate using 360°VR consultations: 91% (29 out of 32) and 96% (81 out of 84) of patients who received 360°VR consultations enrolled in surgery at Mount Sinai Hospital and Hoag Memorial Hospital Presbyterian, respectively [28,29]. In the latter study, the authors found that prior to 360°VR consultations, the retention rate was only 64%, which increased to 96% after patient-specific 360°VR platform was utilized in clinic. As more evidence accumulates, the role of VR in improving patient retention rate may become more prominent. Future studies on the role of VR in surgical patient care will likely become both more comprehensive and granular in approach. For example, randomized controlled studies can be performed within the same institution and by the same group of surgeons to assess the level of patient comprehension of their surgical disease, the disease anatomy, their perception of level of their own contribution to shared-decision making, their pre-operative anxiety, and post-operative satisfaction of the overall experience of patient care. This can be done by exposure to the VR platform in multiple settings in multiple sessions with both physicians and nurses, in the form of VR display of patient’s surgical disease anatomy, using VR to explain the surgical approach, playing a VR video of what to expect on the day of the surgery that use real hospital locations, and finally what to expect postoperative during the recovery period. As the VR platform gradually becomes more integrated into existing patient care experiences, surgical departments and hospitals may begin to incorporate it into their standard practices as they see its value in potentially improving the overall patient experience in a cost-effective manner.
5. Conclusion
Patient consultation with 360°VR appears to augment the patient-centered care approach, by helping to bridge the communication gap between neurosurgeons and patients. Results from this study indicate that 360°VR consultation may help patients better visualize, and thus conceptualize, their pathology and proposed surgical procedure, thereby enhancing patient understanding, engagement, and overall satisfaction.
References
- Kliot T, Zygourakis CC, Imershein S, Lau C, Kliot M. The impact of a patient education bundle on neurosurgery patient satisfaction. Surg Neurol Int. 6 (2015): 567-572.
- Ha JF, Longnecker N. Doctor-patient communication: a review. Ochsner J 10 (2010): 38-43.
- Travaline JM, Ruchinskas R, D'Alonzo GE Jr. Patient-physician communication: why and how. J Am Osteopath Assoc 105 (2005): 13-18.
- Kessels RP. Patients' memory for medical information. J R Soc Med 96 (2003): 219-222.
- Thomson AM, Cunningham SJ, Hunt NP. A comparison of information retention at an initial orthodontic consultation. Eur J Orthod 23 (2001): 169-178.
- Khor WEB, Amin K, Patel K, e al. Augmented and virtual reality in surgery- the digital surgical environment: applications, limitations and legal pitfalls. Annals of Translational Medicine 4 (2016): 454-464.
- Kamel Boulos MN, Toth-Cohen S. The University of Plymouth Sexual Health SIM experience in Second Life: evaluation and reflections after 1 year. Health Info Libr J 26 (2009): 279-288.
- Garcia-Palacios A, Hoffman HG, See SK, et al. Redefining therapeutic success with virtual reality exposure therapy. Cyberpsychol Behav 4 (2001): 341-348.
- Dascal JR, Ishak WW, Spiegel B, et al. Virtual reality and medical inpatients: a systematic review of randomized, controlled trials. Innovations in Clinical Neuroscience 14 (2017): 14-21.
- Merril JR, Notaroberto NF, Laby DM, et al. The Ophthalmic Retrobulbar Injection Simulator (ORIS): an application of virtual reality to medical education. Proc Annu Symp Comput Appl Med Care 11 (1992): 702-706.
- Aggarwal R, Ward J, Balasundaram I, et al. Proving the effectiveness of virtual reality simulation for training in laparoscopic surgery. Ann Surg 246 (2007): 771-779.
- Alaraj A, Lemole MG, Finkle JH, et al. Virtul reality training in neurosurgery: Review of current status and future applications. Surg Neurol Int 2 (2011): 52.
- Konakondla S, Fong R, Schirmer CM. Simulation training in neurosurgery: advances in education and practice. Adv Med Educ Pract 8 (2017): 465-473.
- Alaraj A, Charbel FT, Birk D, et al. Role of cranial and spinal virtual and augmented reality simulation using immersive touch modules in neurosurgical training. Neurosurgery 1 (2013): 115-123.
- Kin T, Nakatomi H, Shono N, et al. Neurosurgical virtual reality simulation for brain tumor using high-definition computer graphics: a review of the literature. Neurol Med Chir 57 (2017): 513-520.
- Kockro RA, Killeen T, Ayyad A, et al. Aneurysm surgery with preoperative three-dimensional planning in a virtual reality environment: Technique and outcome analysis. World Neurosurg 96 (2016): 489-499.
- Chugh AJ, Pace JR, Singer J, et al. Use of a surgical rehearsal platform and improvement in aneurysm clipping measures: results of a prospective, randomized trial. J Neurosurg 126 (2017): 838-844.
- Stewart M, Brown JB, Donner A, et al. The impact of patient-centered care on outcomes. J Fam Pract 49 (2000): 796-804.
- Little P, Everitt H, Williamson I, et al. Observational study of effect of patient centredness and positive approach on outcomes of general practice consultations. BMJ 323 (2001): 908-911.
- Berry LL, Seiders K, Wilder SS. Innovations in access to care: a patient-centered approach. Ann Intern Med 139 (2003): 568-574.
- Arora NK, Weaver KE, Clayman ML, et al. Physicians' decision-making style and psychosocial outcomes among cancer survivors. Patient Educ Couns 77 (2009): 404-412.
- In: Crossing the Quality Chasm: A New Health System for the 21st Washington DC (2001).
- Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood) 27 (2008): 759-769.
- Altin SV, Stock S. The impact of health literacy, patient-centered communication and shared decision-making on patients' satisfaction with care received in German primary care practices. BMC Health Serv Res 16 (2016): 450.
- Sepucha K, Atlas SJ, Chang Y, et al. Patient Decision aids improve decision quality and patient experience and reduce surgical rates in routine orthopaedic care: A prospective cohort study. J Bone Joint Surg Am 99 (2017): 1253-1260.
- Flynn D, Knoedler MA, Hess EP, et al. Engaging patients in health care decisions in the emergency department through shared decision-making: a systematic review. Acad Emerg Med 19 (2012): 959-967.
- Spatz ES, Elwyn G, Moulton BW, et al. Shared decision making as part of value based care: New U.S. policies challenge our readiness. Z Evid Fortbild Qual Gesundhwes 123 (2017): 104-108.
- Louis RG, Anderson P. Using virtual reality technology across the surgical treatment continuum results in enhanced patient engagement and satisfaction. Paper presented at: Healthcare Information and Management Systems Society (HIMSS) Annual Conference & Exhibition, Las Vegas, NV, USA (2018).
- Schlachter LC, Costa AB, Bederson JB. Simulation-based consultations and preoperative planning in patients with skull base and cerebrovascular pathology. Paper presented at: 16th European Congress of Neurosurgery Athens, Greece; September 4-8, (2016).
- Bekelis K, Calnan D, Simmons N, MacKenzie TA, Kakoulides G. Effect of an Immersive Preoperative Virtual Reality Experience on Patient Reported Outcomes: A Randomized Controlled Trial. Ann Surg 265 (2017): 1068-1073.

 No Value
No Value