Immunosuppressed Children and Young People, Psychosocial Wellbeing, and the COVID-19 Pandemic: a Prospective Cohort Study
Article Information
Corine Driessens*, 1, Lynne Mills2, Ravin Patel3, David Culliford1, Diane Gbesemete2,3, Emma Lee2, Meera Shaunak2, Harry Chappell2, Saul N. Faust#, 2, 3, Hans de Graaf#, 2, 3, On behalf of the ImmunoCOVID19 study group (Appendix A)
1NIHR Applied Research Collaboration Wessex, University of Southampton, 2 Venture Rd, Chilworth, Southampton, SO16 7NP, UK
2NIHR Southampton Clinical Research Facility and Biomedical Research Centre, University Hospital Southampton, NHS Foundation Trust, Southampton SO16 6YD, UK
3Faculty of Medicine and Institute for Life Sciences, University of Southampton, Southampton SO16 6YD, UK.
#shared last author
*Corresponding author: Corine Driessens, NIHR Applied Research Collaboration Wessex, University of Southampton, 2 Venture Rd, Chilworth, Southampton, SO16 7NP, UK.
Received: 08 November 2023 Accepted: 16 November 2023 Published: 04 December 2023
Citation: Corine Driessens, Lynne Mills, Ravin Patel, David Culliford, Diane Gbesemete, Emma Lee, Meera Shaunak, Harry Chappell, Saul N. Faust, Hans de Graaf, On behalf of the Immuno COVID19 study group (Appendix A). Immunosuppressed Children and Young People, Psychosocial Wellbeing, and the COVID-19 Pandemic: a Prospective Cohort Study. Archives of Microbiology and Immunology. 7 (2023): 350-361.
View / Download Pdf Share at FacebookAbstract
Aim: This study aims to describe the psychosocial experiences of immunosuppressed CYP while Britain moved from the COVID-19 pandemic to epidemic.
Methods: We invited 1021 CYP participating in the ImmunoCOVID-19 study to complete a mental wellbeing survey in November/December 2021, January/February 2022, and March/April 2022, 467 accepted the invitation. At these 3 timepoints we assessed health-related-quality-of-life (HRQOL) and mood using the positive and negative affect scale. A linear mixed model repeated measure approach was used to analyse this prospective cohort data.
Results: In November/December 2021 and January/February 2022 the CYP reported HRQOL levels were noticeably lower compared to pre-COVID-19 norm levels. However, as the immunosuppressed CYP moved towards the COVID-19 epidemic (March/April 2022), HRQOL levels increased and negative mood decreased. Our findings confirmed early pandemic findings indicating that younger children’s positive mood and school functioning were less affected by the COVID-19 pandemic and that CYP’s mood, physical and school functioning and social support were more affected by the pandemic if they lived in low-income households. Moreover, parental anxiety and/or depression decreased CYP’s HRQOL and mood, except for psychological functioning and autonomy.
Conclusion: As Britain moved into the COVID-19 epidemic immunosuppressed CYP were slowly recovering from the psychosocial impact of the pandemic. More importantly, CYP’s psychosocial wellbeing was impacted by parental mental health, household income, and age regardless of the COVID-19 circumstances. Health and social care provided to immunosuppressed CYP should therefore include family guidance and interventions to support not only the psychosocial wellbeing of the paediatric patients but also parents.
Keywords
child & adolescent, COVID-19, immunosuppression, emotional mental health, prospective cohort study
Article Details
1. Introduction
In March 2020 children and young people (CYP) living with an immunosuppressive disorder in the UK were informed that they were clinically extremely vulnerable (CEV) to the SARS-CoV-2 virus. The UK government advised families with CEV children to shield. A few months into the pandemic scientific findings indicated that children in general were less affected by SARS-CoV-2 [1]. At this time, the government reversed their shielding guidance for CEV CYP (August 2020). Most immunosuppressed CYP were removed from the CEV list and informed that they were not more likely than their healthy peers to experience severe adverse effects from a SARS-Cov-2 infection, despite their generally higher risk for other bacterial and/or viral infections [2].
The SARS-CoV-2 preventative measures taken early in the COVID-19 pandemic had a profound psychological impact on the British CEV community [3, 4]. British data collected in the early stages of the pandemic showed that children with health conditions had higher levels of emotional mental health problems during the first few months of the pandemic compared to children without chronic health conditions [5, 6]. These findings were corroborated by international studies [7], which revealed negative mental health outcomes for CYP living with inflammatory bowel syndrome, chronic respiratory conditions, and neuromuscular disorders. The studies reporting on the psychosocial impact of the COVID-19 pandemic on children with health conditions are either cross-sectional studies conducted in the first few months of the pandemic or longitudinal studies examining the effects of the first year of the COVID-19 pandemic.
In order to provide effective paediatric health and social long-term condition care in the COVID epidemic it is important to understand the prolonged effects of the pandemic on CYP living with chronic health conditions. The ImmunoCOVID-19 study, a prospective longitudinal study exploring the daily clinical and life experiences of immunosuppressed paediatric patients and their carers between March 2020 and April 2022, provides a unique opportunity to gain further insight into the long-term psychosocial effects of the COVID-19 pandemic on CYP living with a chronic health condition. As described by Shaunak et al. [8], 1631 immunosuppressed CYP were recruited into this study between March and July 2020. Based on the serology testing it was estimated that about 10% of the vulnerable CYP in this study had experienced a SARS-Cov-2 infection by March 2021 [9]. By April 2022, it was estimated, based on self-report data, while also taking into account participant attrition, that about half of the vulnerable CYP had experienced a SARS-CoV-2 infection, some experiencing repeated infections. Parental concern for their immunosuppressed child was high at the beginning of the COVID-19 pandemic. Most parents gradually adapted to the ever-changing realities, yet around 10% of the parents experienced continuous high concern levels throughout the pandemic [10]. Those parents experiencing continuous high levels of concern were more likely to experience emotional mental health problems than the parents who gradually adapted to the COVID-19 pandemic adversities [11].
Parental emotional mental wellbeing has been shown to be a strong predictive factor for CYP mental wellbeing [12, 13]. In this current study we will therefore not only explore the psychosocial wellbeing of vulnerable CYP while Britain moved from COVID-19 pandemic to COVID-19 epidemic, but also examine the impact of parental mental wellbeing on this change.
2. Methods
2.1 Participants
Paediatric clinical teams from 46 UK hospitals referred 2856 CYP receiving care for an immunosuppressive condition, defined as having a medical indication for an annual influenza vaccine, to the ImmunoCOVID-19 team. 1631 (57.1%) of these CYP and their carers consented to participation and were sent weekly online questionnaires between March 2020 and April 2022 assessing weekly COVID symptom presentation, COVID testing and results, COVID vaccinations, NHS attendance, hospital admissions, missing out on school, sport/leisure activities and parental concern. In July 2021, the 1021 CYP and their carers who regularly completed the weekly survey, were invited to participate in a mental wellbeing extension study, 467 consented (45.7%) and were sent online mental wellbeing surveys to complete in November/December 2021, January/February 2022, and March/April 2022. The CYP and their carers completed informed consent/assent for both the weekly ImmunoCOVID-19 survey and the mental wellbeing survey. Ethical approval for both components of the ImmunoCOVID-19 study was provided by the Leeds NHS Research Ethics Committee (IRAS 281544). The ImmunoCOVID-19 study complied to the latest version of the Helsinki Declaration.
2.2 Measures
CYP’s emotional wellbeing was assessed using the self-report child version of the positive and negative affect schedule (PANAS-C) [14]. The PANAS-C contains two 10-item subscales designed to measure positive (i.e., active, alert, attentive, determined, enthusiastic, excited, inspired, interested, proud, and strong) and negative affect (i.e., afraid, ashamed, distressed, guilty, hostile, irritated, jittery, nervous, scared, and upset). Answer categories on the PANAS-C range from 1, ‘very slightly’/‘not at all’, to 5, ‘extremely’/‘very much’, leading to a minimum combined score of 10 and a maximum combined score of 50. CYP’s health related quality of life (HRQOL) was measured using the self-report child and adolescent version of the KIDSCREEN-27 [15]. The 27-items scale measures CYP HRQOL in relation to physical wellbeing, psychological wellbeing, parent relations and autonomy, social support and peers, and school/education.
A 5-point Likert-scale is used for the answer categories. For each of the 5 subscales, a scoring algorithm is employed to calculate T-scaled scores with a mean of 50 and a standard deviation of 10, higher scores indicating a better quality of life. Parental mental wellbeing was assessed with the 21-item self-report Depression and Anxiety Stress Scales (DASS—21) [16]. Answer categories range from 0, ‘did not apply to me at all’, to 3, ‘applied to me very much’/‘most of the time’, leading to a minimum subscale score of 0 and a maximum subscale score of 21 for each of the 7-item domain scores. The domain scores for depression and anxiety were taken into account when determining the parent’s mental health status in the currently described project. The recommended cut-off scores of 10 or higher on the depression domain and 8 or higher on the anxiety domain were used to indicate if a parent experienced depressive and/or anxiety symptoms (PMH).
The four previously discovered parental concern patterns (resilient, recovering medium concern, recovering high concern, continuous high concern) [11] were considered potential fixed effects influencing CYP emotional wellbeing and HRQOL. Further factors considered to impact CYP psychosocial wellbeing were CYP’s clinical (diagnosis) and demographic (age, gender) characteristics, which were assessed at baseline (March-July 2020). Parental demographic and household information (gender, age, geographical location, rural/urban, green space, household income, household composition, number of siblings, and employment), collected in September 2021, were also taken into account.
2.3 Quantitative analysis
The data has been cleaned, processed, and analysed in SAS9.4 [17]. First the descriptive characteristics of the sample were determined. Then we used repeated-measure analysis of variance to assess unadjusted differences in emotional wellbeing and HRQOL measured in November/December 2021, January/February 2022, and March/April 2022. Next, we visualized unadjusted differences in emotional wellbeing and HRQOL over time for those CYP with and without parents experiencing PMH. Finally, a linear mixed model repeated measure (MMRM) approach was used to explore the predictors of the CYPs HRQOL and emotional wellbeing [18]. Different models were calculated for the separate subscales (positive mood, negative mood, physical wellbeing, psychological wellbeing, parent relations and autonomy, social support and peers, and school functioning). PMH was entered as fixed effect, this independent variable changed over time, as parental mental wellbeing was measured at the same intervals as CYP’s emotional wellbeing and HRQOL.
Time, CYP’s age (0-10 vs 11-18), CYPs gender (male/female), CYPs diagnosis (rheumatological diagnosis vs other), receipt of COVID vaccine by September 2021 (yes/no), report of SARS-CoV-2 infection by September 2021 (none vs 1 or more infections), parental gender (male/female), parental age (27 – 40, 41 – 50, 51 – 62), geographical location (South -, Middle -, North of England, Wales/Scotland/Ireland), urbanization (rural, semi-rural, urban), access to green space (difficult, easy), household income (<£29500, ~ £29500, > £29500), household composition (single parent vs 2 parents), number of siblings (0, 1, 2+) parental employment (full/parttime vs non-working/disabled/retired), and parental concern level were entered into the model as fixed effects. The significance of these independent variables was first tested in univariable models. Only significant variables were entered into multivariable models, with the aim of building similar multivariable models for each of the outcomes. Parental concern, CYP’s diagnosis, report of SARS-CoV-2 infection by September 2021, geographical location, urbanization, and household composition were not significant in predicting CYP’s emotional wellbeing or HRQOL in the univariable models and thus these fixed effects were not entered in the multivariable models.
Multiple measurements taken on the same CYP are correlated with each other. Depending how far apart the measurements are taken this correlation often differs. To acknowledge this dependence between repeated measures, the MMRM model offers different covariance matrix structures to model different dependence structures. A heterogeneous Toeplitz covariance matrix was chosen for the MMRM models in this study as this matrix structure had the best fit (AIC=4263 and BIC=4283). This covariance structure has heterogeneous variances and heterogeneous correlations between the elements, meaning that the correlation between measurements taken in Nov/Dec 2021 with measurements in Jan/Feb 2022 differ from the correlations between measurements in Jan/Feb 2022 and Mar/Apr 2022 and again differ from the correlations between measurements in Nov/Dec 2021 and Mar/Apr 2022. The heterogeneous Toeplitz covariance matrix represented the simplest model with lowest AIC/BIC combination [18] when compared to compound symmetry (4274/4282), unstructured (4262/4287), autoregressive (4281/4289), heterogenous autoregressive (4270/4287), and Toeplitz structures (4273/4285). The Kenward-Roger correction was applied to reduce bias in estimation of standard errors and F-Statistics [18]. The results are presented as parameter estimates with standard errors and P-values.
4. Results
3.1 Participants
Of the 467 CYP who consented/assented to the mental wellbeing part of the ImmunoCOVID-19 study, most had a rheumatological diagnosis (43%) many had not been vaccinated by September 2021 (77.7%) nor experienced a SARS-CoV-2 infection (89.1%) at the start of the 2021 school year. There was an almost equal split between boys and girls as well as children aged 10 and under versus aged 11 to 18. Additional household and parental characteristics are described in Table 1.
Table 1: Descriptive statistics of the CYP sample (N=467)
|
Child characteristics |
N (%) |
|
Gender (female) |
237 (50.7%) |
|
Age |
|
|
0 - 10 |
159 (34.1%) |
|
Nov-18 |
249 (53.3%) |
|
Age unknown |
59 (12.6%) |
|
Diagnosis |
|
|
Rheumatological diagnoses |
201 (43%) |
|
Other diagnoses* |
185 (40%) |
|
Diagnoses unknown |
81 (17%) |
|
Vaccinated by 9/2021 (yes) |
104 (22.3%) |
|
Reported SARS -CoV-2 infection by 9/2021 |
51 (10.9%) |
|
Household characteristics |
N (%) |
|
Access to green space |
|
|
Easy |
420 (89.9%) |
|
Difficult |
25 (5.4%) |
|
Unknown |
22 (4.7%) |
|
Urbanization |
|
|
Rural |
56 (12%) |
|
Semi-rural |
149 (31.9%) |
|
Urban |
235 (50.3%) |
|
Unknown |
27 (5.8%) |
|
Region |
|
|
England – South |
208 (44.5%) |
|
England – Midlands |
75 (16.1%) |
|
England – North |
96 (20.6%) |
|
Ireland – Scotland – Wales |
70 (15.0%) |
|
Unknown |
18 (3.9%) |
|
Household income |
|
|
Below £29500 |
80 (17.1%) |
|
About £29500 |
74 (15.8%) |
|
Above £29500 |
274 (58.7%) |
|
Unknown |
39 (8.4%) |
|
Household composition |
|
|
Single parent |
62 (13.3%) |
|
2 parent-household |
373 (79.9%) |
|
Unknown |
32 (6.9%) |
|
Number of siblings |
|
|
0 |
90 (19.3%) |
|
1 |
187 (40%) |
|
2+ |
86 (18.4%) |
|
Unknown |
104 (22.3%) |
|
Parent Characteristics |
N (%) |
|
Parental Concern Trajectory |
|
|
Resilient |
104 (22.3%) |
|
Recovery medium concern |
174 (37.3%) |
|
Recovery high concern |
137 (29.3%) |
|
Continuous high concern |
52 (11.1%) |
|
Parents with mental health problems |
|
|
Nov/Dec 2021 |
37 (7.9%) |
|
Jan/Feb 2022 |
25 (10.1%) |
|
March/April 2022 |
23 (4.9%) |
|
Gender parent (female) |
395 (84.6%) |
|
Age |
|
|
27 – 40 yrs |
96 (20.6%) |
|
41 – 50 yrs |
204 (43.7% |
|
51 – 62 yrs |
63 (13.5%) |
|
Unknown age |
104 (22.3%) |
*other diagnosis: airway diseases, immunodeficiency disorder, diabetes, solid organ or bone marrow transplant, nephrotic syndrome, other kidney disease, inflammatory bowel disease, other gastroenterology and hypathology, oncological diagnosis, neurological diagnosis
252 (54%) of the CYP completed the mental wellbeing survey in November/December 2021, 229 (49%) CYP completed the survey in January/February 2022, and 196 (42%) CYP completed the survey in March/April 2022. Table 2 shows the average emotional wellbeing and standardized HRQOL experienced by the CYP at these three timepoints. According to the repeated-measure analysis of variance (F/P-value column table 2) CYP’s emotional wellbeing and HRQOL were quite stable over time. Psychological wellbeing was the lowest HRQOL reported, CYP experienced statistically significant lower levels of psychological wellbeing in January/February 2022.
Table 2: Change in CYP’s mental wellbeing over time
|
Mental wellbeing |
Measurement points |
Outcome repeated-measure analysis of variance |
||
|
Nov/Dec 2021 N=252 |
Jan/Feb 2022 N=229 |
March/Apr 2022 N=196 |
F (P-value) |
|
|
|
Mean (SD) |
Mean (SD) |
Mean (SD) |
|
|
Mood |
||||
|
Positive |
31.99 (8.63) |
32.38 (8.90) |
32.99 (8.91) |
0.72 (0.49) |
|
Negative |
18.7 (7.67) |
18.17 (7.12) |
17.14 (6.12) |
2.72 (0.07) |
|
HRQOL |
||||
|
Physical wellbeing |
43.50 (12.30) |
43.13 (7.93) |
45.38 (12.21) |
2.34 (0.10) |
|
Psychological wellbeing |
42.44 (5.29) |
34.87 (3.40) |
43.25 (5.25) |
206.10 (<0.001) |
|
Parent relations & autonomy |
50.39 (8.86) |
50.38 (8.69) |
51.34 (10.32) |
0.70 (0.50) |
|
Social support & peers |
43.85 (11.59) |
44.34 (11.57) |
45.16 (11.73) |
0.66 (0.52) |
|
School functioning |
48.64 (10.79) |
48.15 (10.12) |
50.09 (10.49) |
1.83 (0.16) |
SD=standard deviation
3.2 CYP’s mental wellbeing in relation to parental mental wellbeing
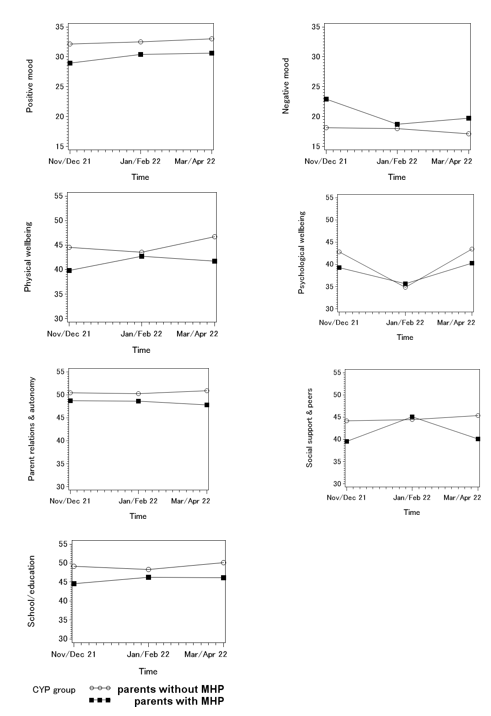
Figure 1 visualizes the association between CYP’s HRQOL as well as emotional wellbeing and parental mental wellbeing. In general, CYP whose parents experienced mental health problems reported lower HRQOL, higher negative mood, and lower positive mood. Differences were especially pronounced in November/December 2021 and March/April 2022.
Table 3 quantifies the association between child, parent, and household characteristics with changes in CYP’s emotional wellbeing and HRQOL. When all significant variables were added into the MMRM models, parental experience of anxiety and/or depressive symptoms (PMH) was associated with higher levels of negative mood, lower levels of positive mood, physical wellbeing, social support & peer interaction, and worse school functioning. Keeping in mind that the data collected in March/April 2022 was the reference category for the MMRM models, time (wave) was significantly associated with a reduction in physical and psychological wellbeing, school functioning and an increase in negative mood. Furthermore, age 10 and under and not having received the vaccination by September 2021 was significantly positively associated with positive mood, physical and psychological wellbeing. Age 10 and under was also associated with higher levels of school functioning. In contrast, lower levels of household income were associated with lower positive mood, higher negative mood, lower levels of physical wellbeing, lower levels of social support and peer interaction, and lower levels of school functioning. Parent relations and autonomy was only significantly positively related to the number of children in the household, with participants with less siblings reporting better child-parent relationships.
Table 3: Association between child, parent, and household characteristics with CYP’s emotional wellbeing and HRQOL
|
Positive Mood |
Negative Mood |
|||||
|
estimate |
S.E. |
P-value |
estimate |
S.E. |
P-value |
|
|
Wave |
||||||
|
Nov/Dec 2021 |
-0.85 |
0.59 |
0.149 |
1.32 |
0.39 |
0.001 |
|
Jan/Feb 2022 |
-0.06 |
0.54 |
0.907 |
0.81 |
0.37 |
0.03 |
|
Mar/Apr 2022 |
Reference |
reference |
||||
|
Gender CYP |
||||||
|
Female |
0.95 |
0.94 |
0.312 |
0.72 |
0.84 |
0.392 |
|
Male |
reference |
reference |
||||
|
Age Child |
||||||
|
0-9 |
5.37 |
1.14 |
<0.0001 |
0.23 |
1.02 |
0.823 |
|
10+ |
reference |
reference |
||||
|
Vaccinated by 9/2021 |
||||||
|
No |
2.61 |
1.24 |
0.037 |
-1.2 |
1.11 |
0.28 |
|
Yes |
Reference |
reference |
||||
|
Access to green space |
||||||
|
Easy |
0.29 |
2.05 |
0.888 |
-3.45 |
1.82 |
0.06 |
|
Difficult |
reference |
reference |
||||
|
Parental gender |
||||||
|
Female |
-1.45 |
2.01 |
0.473 |
0.56 |
1.82 |
0.76 |
|
Male |
reference |
reference |
||||
|
Age parent |
||||||
|
27 – 40 yrs |
0.48 |
1.72 |
0.781 |
-0.74 |
1.54 |
0.631 |
|
41 – 50 yrs |
0.62 |
1.44 |
0.669 |
-0.28 |
1.28 |
0.825 |
|
51 – 62 yrs |
reference |
reference |
||||
|
Parental Employment |
||||||
|
No work/retired/disabled |
-1.75 |
1.13 |
0.123 |
-0.48 |
1.01 |
0.635 |
|
Full/parttime employed |
reference |
reference |
||||
|
Parental mental health |
||||||
|
No problems |
2.7 |
1.04 |
0.01 |
-2.54 |
0.79 |
0.001 |
|
Mental health problems |
reference |
reference |
||||
|
Number of siblings |
||||||
|
0 |
0.19 |
1.41 |
0.893 |
0.19 |
1.26 |
0.881 |
|
1 |
1.39 |
1.18 |
0.242 |
-0.71 |
1.06 |
0.505 |
|
2+ |
reference |
reference |
||||
|
Household income |
|
|||||
|
Below £29500 |
-3.58 |
1.23 |
0.004 |
2.98 |
1.1 |
0.007 |
|
About £29500 |
-2.75 |
1.27 |
0.032 |
-0.21 |
1.13 |
0.85 |
|
Above £29500 |
reference |
reference |
||||
|
Physical Wellbeing |
Psychological wellbeing |
|||||
|
estimate |
S.E. |
P-value |
estimate |
S.E. |
P-value |
|
|
Wave |
||||||
|
Nov/Dec 2021 |
-1.83 |
0.86 |
0.035 |
-0.98 |
0.39 |
0.014 |
|
Jan/Feb 2022 |
-2.9 |
0.79 |
0.0003 |
-8.6 |
0.4 |
<0.0001 |
|
Mar/Apr 2022 |
reference |
reference |
||||
|
Gender CYP |
||||||
|
Female |
-1.19 |
1.07 |
0.27 |
-0.07 |
0.48 |
0.877 |
|
Male |
reference |
reference |
||||
|
Age Child |
||||||
|
0-9 |
4 |
1.31 |
0.003 |
1.29 |
0.59 |
0.03 |
|
10+ |
reference |
reference |
||||
|
Vaccinated by 9/2021 |
||||||
|
No |
3.28 |
1.42 |
0.022 |
1.39 |
0.63 |
0.029 |
|
Yes |
reference |
reference |
||||
|
Access to green space |
||||||
|
Easy |
3.52 |
2.5 |
0.161 |
1.8 |
1.1 |
0.102 |
|
Difficult |
reference |
reference |
||||
|
Parental gender |
||||||
|
Female |
-3.14 |
2.53 |
0.215 |
-0.25 |
1.12 |
0.824 |
|
Male |
Reference |
reference |
||||
|
Age parent |
||||||
|
27 – 40 yrs |
0.2 |
1.97 |
0.918 |
-0.69 |
0.88 |
0.431 |
|
41 – 50 yrs |
-0.99 |
1.63 |
0.547 |
-0.78 |
0.72 |
0.282 |
|
51 – 62 yrs |
reference |
reference |
||||
|
Parental Employment |
||||||
|
No work/retired/disabled |
-2.24 |
1.29 |
0.084 |
-0.11 |
0.57 |
0.842 |
|
Full/parttime employed |
reference |
reference |
||||
|
Parental mental health |
||||||
|
No problems |
2.72 |
1.36 |
0.047 |
1.04 |
0.66 |
0.117 |
|
Mental health problems |
reference |
reference |
||||
|
Number of siblings |
||||||
|
0 |
0.14 |
1.61 |
0.929 |
1.26 |
0.72 |
0.083 |
|
1 |
0.92 |
1.36 |
0.502 |
0.47 |
0.61 |
0.447 |
|
2+ |
reference |
reference |
||||
|
Household income |
||||||
|
Below £29500 |
-3.94 |
1.43 |
0.006 |
-0.96 |
0.63 |
0.131 |
|
About £29500 |
-3.14 |
1.48 |
0.035 |
-0.42 |
0.66 |
0.527 |
|
Above £29500 |
reference |
reference |
||||
|
Parent relations & autonomy |
Social support & peer interaction |
|||||
|
estimate |
S.E. |
P-value |
estimate |
S.E. |
P-value |
|
|
Wave |
||||||
|
Nov/Dec 2021 |
-0.81 |
0.65 |
0.215 |
-0.74 |
0.86 |
0.393 |
|
Jan/Feb 2022 |
-0.79 |
0.71 |
0.262 |
0.16 |
0.93 |
0.867 |
|
Mar/Apr 2022 |
reference |
reference |
||||
|
Gender CYP |
||||||
|
Female |
-0.73 |
1.12 |
0.518 |
1.78 |
1.34 |
0.186 |
|
Male |
reference |
reference |
||||
|
Age Child |
||||||
|
0-9 |
-0.13 |
1.37 |
0.925 |
1.17 |
1.65 |
0.481 |
|
10+ |
reference |
reference |
||||
|
Vaccinated by 9/2021 |
||||||
|
No |
1.44 |
1.48 |
0.331 |
1.9 |
1.76 |
0.283 |
|
Yes |
reference |
reference |
||||
|
Access to green space |
||||||
|
Easy |
2.66 |
2.46 |
0.282 |
2.13 |
2.91 |
0.466 |
|
Difficult |
reference |
reference |
||||
|
Parental gender |
||||||
|
Female |
-2.24 |
2.55 |
0.38 |
0.63 |
3.08 |
0.839 |
|
Male |
reference |
reference |
||||
|
Age parent |
||||||
|
27 – 40 yrs |
-0.74 |
2.04 |
0.717 |
-0.59 |
2.44 |
0.809 |
|
41 – 50 yrs |
-1.11 |
1.69 |
0.513 |
-2.53 |
2.01 |
0.21 |
|
51 – 62 yrs |
reference |
reference |
||||
|
Parental Employment |
||||||
|
No work/retired/disabled |
-0.28 |
1.34 |
0.836 |
-3.86 |
1.59 |
0.016 |
|
Full/parttime employed |
Reference |
reference |
||||
|
Parental mental health |
||||||
|
No problems |
2.21 |
1.27 |
0.082 |
3.76 |
1.66 |
0.024 |
|
Mental health problems |
reference |
reference |
||||
|
Number of siblings |
||||||
|
0 |
4.53 |
1.66 |
0.007 |
0.84 |
1.99 |
0.675 |
|
1 |
3.23 |
1.42 |
0.024 |
1.47 |
1.7 |
0.388 |
|
2+ |
reference |
reference |
||||
|
Household income |
||||||
|
Below £29500 |
-1.92 |
1.46 |
0.189 |
-3.74 |
1.74 |
0.033 |
|
About £29500 |
-1.85 |
1.52 |
0.226 |
-2.68 |
1.83 |
0.143 |
|
Above £29500 |
reference |
reference |
||||
|
School functioning |
||||||
|
estimate |
S.E. |
P-value |
||||
|
Wave |
||||||
|
Nov/Dec 2021 |
-1.74 |
0.76 |
0.024 |
|||
|
Jan/Feb 2022 |
-1.78 |
0.67 |
0.008 |
|||
|
Mar/Apr 2022 |
reference |
|||||
|
Gender CYP |
||||||
|
Female |
0.91 |
1.22 |
0.457 |
|||
|
Male |
reference |
|||||
|
Age Child |
||||||
|
0-9 |
4.62 |
1.5 |
0.002 |
|||
|
10+ |
reference |
|||||
|
Vaccinated by 9/2021 |
||||||
|
No |
2.37 |
1.6 |
0.14 |
|||
|
Yes |
reference |
|||||
|
Access to green space |
||||||
|
Easy |
0.25 |
2.71 |
0.925 |
|||
|
Difficult |
reference |
|||||
|
Parental gender |
||||||
|
Female |
0.9 |
2.81 |
0.749 |
|||
|
Male |
reference |
|||||
|
Age parent |
||||||
|
27 – 40 yrs |
-0.55 |
2.22 |
0.806 |
|||
|
41 – 50 yrs |
0.33 |
1.83 |
0.856 |
|||
|
51 – 62 yrs |
reference |
|||||
|
Parental Employment |
||||||
|
No work/retired/disabled |
-1.23 |
1.45 |
0.397 |
|||
|
Full/parttime employed |
reference |
|||||
|
Parental mental health |
||||||
|
No problems |
2.78 |
1.36 |
0.042 |
|||
|
Mental health problems |
reference |
|||||
|
Number of siblings |
||||||
|
0 |
-1.25 |
1.82 |
0.494 |
|||
|
1 |
-0.74 |
1.55 |
0.633 |
|||
|
2+ |
Reference |
|||||
|
Household income |
||||||
|
Below £29500 |
-4.86 |
1.59 |
0.003 |
|||
|
About £29500 |
-2.55 |
1.65 |
0.123 |
|||
|
Above £29500 |
reference |
|||||
S.E.= Standard Error; printed in bold are those findings that are statistically significant
4. Discussion
Our findings indicate that from November/December 2021 to January/February 2022 the average physical wellbeing, psychological wellbeing, and social support & peer interaction levels reported by CYP included in the ImmunoCOVID-19 study was lower than the reported European pre-COVID norm [19]. Even in comparison to pre-COVID average scores reported by adolescent renal transplant patients, the reported ImmunoCOVID-19 study scores on the KIDSCREEN subscales suggest a noticeable reduction in HRQOL [20]. This is in line with findings reported by the CLoCk study who reported that around 40% of the British adolescents included in their study felt worried, sad or unhappy in 2021 irrespective of their SARS-CoV-2 status [21]. On the positive side, our results show that as the CYP included in the ImmunoCOVID-19 study moved closer to the ‘living with COVID’ phase in UK’s COVID-19 pandemic they experienced a significantly increase in physical wellbeing, psychological wellbeing, and school functioning as well as a significant reduction in negative mood. These findings suggest that they are on their way to recovery. The psychosocial wellbeing of ImmunoCOVID-19’s younger CYP was significantly better than the psychosocial wellbeing of the older CYP. European pre-pandemic findings align with these results showing that CYPs’ HRQOL decreased with age, with older CYP self-reporting lower HRQOL than younger CYP [22]. Of concern was our finding that CYP from lower income households reported lower levels of HRQOL and positive mood and higher levels of negative mood. Throughout the COVID-19 pandemic it has been reported that lower income British households are most affected by the COVID-19 pandemic [23]. Early in the pandemic it was determined that CYP from lower income households disclosed higher levels of emotional mental health problems [24, 25]. These findings are however not new, even before the pandemic, research had indicated that lower household income was associated with low HRQOL, especially for older CYP [26]. Research conducted in the last 2 years however has indicated that these existing income inequalities have amplified [27]. Further research is needed to specify the association between low household income and CYP psychosocial wellbeing, especially since recent findings indicate that mediators such as self-efficacy, optimism and social support influence the association between socio-economic status, financial strain, and CYP mental wellbeing [28]. As previously discussed, pre-pandemic CYP mental wellbeing was shown to be significantly affected by parental mental wellbeing [12, 13]. Our findings show that these findings can be generalized to the CEV population, parental mental wellbeing did impact the change in psychosocial wellbeing of CYP living with an immunosuppressive disorder. Other COVID-19 studies confirm that the pre-pandemic association between parental mental wellbeing and their offspring’s mental health holds true during the unprecedented time of the COVID-19 pandemic [25] and is not unique to the CEV population. We can only speculate about the relationship between vaccination status and CYPs’ emotional wellbeing and HRQOL, theorizing that vaccination status might have been related to severity of long-term health condition, an aspect of CYP clinical condition the ImmunoCOVID-19 study did not explore. CYP with more severe conditions were placed on priority lists for vaccination while other children with long-term health conditions were vaccinated at the same time as their healthy-age-equivalent peers [29]. This speculation is supported by the presence of a significant medium level correlation between vaccination status and CYP age (spearman correlation = 0.50) in the ImmunoCOVID-19 data.
5. Strengths and limitations
The main strength of this study is that in contrast to most British COVID-19 cohort studies the ImmunoCOVID-19 study focused on a marginalized population, CYP living with an immunosuppressive disease. The psychosocial wellbeing of the CYP and their carers was assessed with well-validated instruments. Attrition, a methodological problem for all longitudinal studies, deteriorates the generalizability of the findings as does our sampling methods, a form of convenience sampling used by the majority of COVID-19 studies to quickly deploy data collection. A MMRM approach was chosen to analyse the data as it reduces the bias introduced by sporadic non-response. However, it also needs to be mentioned that the underlying assumption of this methodology is that missing data is missing at random [17]. It is important to note that the ImmunoCOVID-19 study did not collect pre-pandemic data, hence comparisons were made with pre-COVID norm data. Regardless of the limitations, the collection of prospective longitudinal data from a marginalized population with diverse demographic backgrounds provided a unique opportunity to examine the prolonged psychosocial impact of the pandemic on CYP living with chronic health conditions.
6. Conclusion
Our findings revealed important insights into the psychosocial changes of CYP living with an immunosuppressive disease during the transition period from COVID-19 pandemic to COVID-19 epidemic. The findings confirm that parental mental health, household income, and age impacted CYP’s psychosocial wellbeing throughout the COVID-19 pandemic. We recommend future studies to focus on enhancing our understanding of the complex relationship between household income and CYP psychosocial wellbeing. Health professionals caring for CYP living with an immunosuppressive disorder should be aware of the greater risk for decreased emotional wellbeing and HRQOL for immunosuppressed CYP. This is particularly relevant in the case of adolescents, CYP living in low-income households and/or living with parents experiencing emotional mental health problems. Health professions caring for immunosuppressed CYP should be aware of appropriate psychosocial interventions and guidance and implement when needed.
Declarations
Ethics approval
The Leeds NHS Research Ethics Committee provided ethical approval to this study (IRAS 281544). All procedures contributing to this work comply with the latest version of the Helsinki Declaration. Informed consent was obtained from all the participants and their legal guardians to participate in the study.
Consent to participate
Informed consent/assent was obtained from CYP and their carers included in the ImmunoCOVID-19 study. Informed consent was obtained from all the participants and their legal guardians to participate in the study.
Consent for publication
Not applicable.
Competing interest
The authors have no competing interests to declare that are relevant to the content of this article.
Funding
Partial financial support was received from the British Paediatric Allergy, Immunity and Infection Group and the Southampton Rheumatology Trust. Participant recruitment and database management was in part supported by SNFs NIHR Senior Investigator award. The study received no further charity, public or commercial funding support. For the purpose of open access, the author has applied a CC BY public copyright licence to any Author Accepted Manuscript version arising from this submission.
Author contribution
SNF, HdG and RP conceived and designed the original ImmunoCOVID-19 study, and secured partial funding. ImmunoCOVID study group have recruited the participants and provided clinical guidance to the original ImmunoCOVID-19 study. RP, HC, MS, DG have been responsible for the weekly data collection, project administration, and data quality checks of the original ImmunoCOVID-19 study. CD and LM conceptualized and designed the mental wellbeing extension study. EL provided clinical psychological expertise. RP has been responsible for the mental wellbeing data collection. LM has been responsible for weekly survey and mental wellbeing data management. CD and DC conceptualized methodology to be used in data analysis and CD led on data analysis. CD has had full access to all the data in this study and takes responsibility for the integrity of the data and accuracy of the analysis. CD drafted this manuscript which was reviewed and edited by all co-authors.
Acknowledgements
We would like to acknowledge all the children, young people, and parents who participated in the ImmunoCOVID-19 study. This study was badged as a UK NIHR Urgent Public Health Study and we would also like to thank the NIHR Clinical Research Network (CRN) and all associated NIHR Local CRNs and site staff who supported recruitment. The authors would like to thank Prof Ulrike Ravens-Sieberer for approving the use of the Kidsscreen-27 questionnaire for the ImmunoCOVID-19 study.
Data availability
Due to the quick deployment of the ImmunoCOVID-19 study we have not actively asked for participants’ permission to safely deposit their data for re-share and re-use, thus while quantitative analysis code can be shared (available upon request from corresponding author) the data for this project cannot be deposited.
References
- Sinaei R, Pezeshki S, Parvaresh S, Sinaei R. Why COVID-19 is less frequent and severe in children: a narrative review. World Journal of Pediatrics 17 (2021): 10-20.
- Memoli MJ, Athota R, Reed S, Czajkowski L, Bristol T, Proudfoot K, et al. The natural history of influenza infection in the severely immunocompromised vs nonimmunocompromised hosts. Clinical infectious diseases 58 (2014): 214-24.
- Lasseter G, Compston P, Robin C, Lambert H, Hickman M, Denford S, et al. Exploring the impact of shielding advice on the wellbeing of individuals identified as clinically extremely vulnerable amid the COVID-19 pandemic: a mixed-methods evaluation. BMC Public Health 22 (2022): 1-1.
- Fisher A, Roberts A, McKinlay AR, Fancourt D, Burton A. The impact of the COVID-19 pandemic on mental health and well-being of people living with a long-term physical health condition: a qualitative study. BMC Public Health 21 (2021): 1-2.
- Raw JA, Waite P, Pearcey S, Shum A, Patalay P, Creswell C. Examining changes in parent?reported child and adolescent mental health throughout the UK's first COVID?19 national lockdown. Journal of Child Psychology and Psychiatry 62 (2021): 1391-401.
- McKinlay AR, May T, Dawes J, Fancourt D, Burton A. ‘You’re just there, alone in your room with your thoughts’: a qualitative study about the psychosocial impact of the COVID-19 pandemic among young people living in the UK. BMJ open 12 (2022): e053676.
- Samji H, Wu J, Ladak A, Vossen C, Stewart E, Dove N, et al. Mental health impacts of the COVID?19 pandemic on children and youth–a systematic review. Child and adolescent mental health 27 (2022): 173-89.
- Shaunak M, Patel R, Driessens C, Mills L, Leahy A, Gbesemete D, et al. COVID-19 symptom surveillance in immunocompromised children and young people in the UK: a prospective observational cohort study. BMJ open 11 (2021): e044899.
- Chappell H, Patel R, Driessens C, Tarr AW, Irving WL, Tighe PJ, et al. Immunocompromised children and young people are at no increased risk of severe COVID-19. Journal of Infection 84 (2022): 31-9.
- Driessens C, Mills L, Culliford D, Patel R, Lee E, Gbesemete D, et al, ImmunoCOVID19 study group (Appendix A). Parental concern for clinically vulnerable child during first 18 months of the COVID pandemic. Pediatric Research 22 (2022): 1-9.
- Driessens C, Mills L, Patel R, Culliford D, Lee E, Gbesemete D, et al. Psychological distress experienced by parents caring for an immunosuppressed child during the COVID-19 pandemic. Journal of Psychiatric Research (2022).
- Lawrence PJ, Murayama K, Creswell C. Systematic review and meta-analysis: anxiety and depressive disorders in offspring of parents with anxiety disorders. Journal of the American Academy of Child & Adolescent Psychiatry 58 (2019): 46-60.
- Warner V, Mufson L, Weissman MM. Offspring at high and low risk for depression and anxiety: Mechanisms of psychiatric disorder. Journal of the American Academy of Child & Adolescent Psychiatry 34 (1995): 786-97.
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of personality and social psychology 54 (1988): 1063.
- Ravens-Sieberer U, Herdman M, Devine J, Otto C, Bullinger M, Rose M, et al. The European KIDSCREEN approach to measure quality of life and well-being in children: development, current application, and future advances. Quality of life research 23 (2014): 791-803.
- Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour research and therapy 33 (1995): 335-43.
- SAS software. Copyright © (2022). SAS Institute Inc., Cary, NC, USA
- Stroup WW, Milliken GA, Claassen EA, Wolfinger RD. SAS for mixed models: introduction and basic applications. SAS Institute 12 (2018).
- KIDSCREEN Group Europe. The KIDSCREEN Questionnaires-Quality of life questionnaires for children and adolescents. Handbook (2006).
- Dobbels F, Decorte A, Roskams A, Van Damme?Lombaerts R. Health?related quality of life, treatment adherence, symptom experience and depression in adolescent renal transplant patients. Pediatric transplantation 14 (2010): 216-23.
- Stephenson T, Pereira SM, Shafran R, De Stavola BL, Rojas N, McOwat K, et al. Physical and mental health 3 months after SARS-CoV-2 infection (long COVID) among adolescents in England (CLoCk): a national matched cohort study. The Lancet Child & Adolescent Health 6 (2022): 230-9.
- Berman AH, Liu B, Ullman S, Jadbäck I, Engström K. Children’s quality of life based on the KIDSCREEN-27: child self-report, parent ratings and child-parent agreement in a Swedish random population sample. PloS one 11 (2016): e0150545.
- Whitehead M, Taylor-Robinson D, Barr B. Poverty, health, and covid-19. bmj 12 (2021): 372.
- Waite P, Pearcey S, Shum A, Raw JA, Patalay P, Creswell C. How did the mental health symptoms of children and adolescents change over early lockdown during the COVID?19 pandemic in the UK? JCPP advances 1 (2021): e12009.
- Adegboye D, Williams F, Collishaw S, Shelton K, Langley K, Hobson C, et al. Understanding why the COVID?19 pandemic?related lockdown increases mental health difficulties in vulnerable young children. JCPP advances 1 (2021): e12005.
- Von Rueden U, Gosch A, Rajmil L, Bisegger C, Ravens-Sieberer U. Socioeconomic determinants of health related quality of life in childhood and adolescence: results from a European study. Journal of Epidemiology & Community Health 60 (2006): 130-5.
- Gagné T, Nandi A, Schoon I. Time trend analysis of social inequalities in psychological distress among young adults before and during the pandemic: evidence from the UK Household Longitudinal Study COVID-19 waves. J Epidemiol Community Health 76 (2022): 421-7.
- Schoon I, Henseke G. Social inequalities in young people's mental distress during the COVID-19 pandemic: Do psychosocial resource factors matter?. Frontiers in public health 14 (2022): 10.
- Majeed A, Pollock K, Hodes S, Papaluca M. Implementation of covid-19 vaccination in the United Kingdom. bmj 29 (2022): 378.