Hydrocele of Canal of Nuck - Role of Radiological Imaging
Article Information
Devi Shanker Malik1*, Mahipal Singh2, Nisha Aurora3, B S Dhakad4
1Director, General and Laparoscopic Surgery, Eternal Hospital, Jaipur, India
2Director and HOD, Radiology, Eternal Hospital Jaipur, India
3Sr. Consultant, Radiology, Eternal Hospital, Jaipur, India
4SMO, General and Laparoscopic Surgery, Eternal Hospital Jaipur, India
*Corresponding Author: Devi Shanker Malik, Director, General and Laparoscopic Surgery, Eternal Hospital, Jaipur, India
Received: 01 October 2022; Accepted: 17 October 2022; Published: 04 November 2022
Citation:
Malik DS, Singh M, Aurora N, Dhakad BS. Hydrocele of Canal of Nuck - Role of Radiological Imaging. Journal of Radiology and Clinical Imaging 5 (2022): 43-46.
View / Download Pdf Share at FacebookAbstract
Hydrocele of canal of Nuck in adult females is very rare to be seen. The canal of Nuck is the portion of processus vaginalis in the inguinal canal in women. This is homologous to the processus vaginalis of male anatomy. Although canal of Nuck normally disappears without a trace in the first year of life but if it remains patent, then it can lead to development of indirect inguinal hernia or hydrocele of canal of Nuck. Radiological imaging has a great role in diagnosis. Ultrasonography is the preferred investigation. Magnetic Resonance Imaging (MRI) done to confirm the diagnosis preoperatively. The treatment remains the excision of hydrocele of canal of nuck. We are presenting two cases of hydrocele of canal of Nuck in adult female, one Bilateral and another unilateral which were treated by laparoscopic excision of hydrocele with mesh repair.
Keywords
Hydrocele of canal of nuck; Patent processus vaginalis; Canal of nuck; Female hydrocele
Hydrocele of canal of nuck articles; Patent processus vaginalis articles; Canal of nuck articles; Female hydrocele articles
Hydrocele of canal of nuck articles Hydrocele of canal of nuck Research articles Hydrocele of canal of nuck review articles Hydrocele of canal of nuck PubMed articles Hydrocele of canal of nuck PubMed Central articles Hydrocele of canal of nuck 2023 articles Hydrocele of canal of nuck 2024 articles Hydrocele of canal of nuck Scopus articles Hydrocele of canal of nuck impact factor journals Hydrocele of canal of nuck Scopus journals Hydrocele of canal of nuck PubMed journals Hydrocele of canal of nuck medical journals Hydrocele of canal of nuck free journals Hydrocele of canal of nuck best journals Hydrocele of canal of nuck top journals Hydrocele of canal of nuck free medical journals Hydrocele of canal of nuck famous journals Hydrocele of canal of nuck Google Scholar indexed journals Patent processus vaginalis articles Patent processus vaginalis Research articles Patent processus vaginalis review articles Patent processus vaginalis PubMed articles Patent processus vaginalis PubMed Central articles Patent processus vaginalis 2023 articles Patent processus vaginalis 2024 articles Patent processus vaginalis Scopus articles Patent processus vaginalis impact factor journals Patent processus vaginalis Scopus journals Patent processus vaginalis PubMed journals Patent processus vaginalis medical journals Patent processus vaginalis free journals Patent processus vaginalis best journals Patent processus vaginalis top journals Patent processus vaginalis free medical journals Patent processus vaginalis famous journals Patent processus vaginalis Google Scholar indexed journals Canal of nuck articles Canal of nuck Research articles Canal of nuck review articles Canal of nuck PubMed articles Canal of nuck PubMed Central articles Canal of nuck 2023 articles Canal of nuck 2024 articles Canal of nuck Scopus articles Canal of nuck impact factor journals Canal of nuck Scopus journals Canal of nuck PubMed journals Canal of nuck medical journals Canal of nuck free journals Canal of nuck best journals Canal of nuck top journals Canal of nuck free medical journals Canal of nuck famous journals Canal of nuck Google Scholar indexed journals Female hydrocele articles Female hydrocele Research articles Female hydrocele review articles Female hydrocele PubMed articles Female hydrocele PubMed Central articles Female hydrocele 2023 articles Female hydrocele 2024 articles Female hydrocele Scopus articles Female hydrocele impact factor journals Female hydrocele Scopus journals Female hydrocele PubMed journals Female hydrocele medical journals Female hydrocele free journals Female hydrocele best journals Female hydrocele top journals Female hydrocele free medical journals Female hydrocele famous journals Female hydrocele Google Scholar indexed journals Ultrasonography articles Ultrasonography Research articles Ultrasonography review articles Ultrasonography PubMed articles Ultrasonography PubMed Central articles Ultrasonography 2023 articles Ultrasonography 2024 articles Ultrasonography Scopus articles Ultrasonography impact factor journals Ultrasonography Scopus journals Ultrasonography PubMed journals Ultrasonography medical journals Ultrasonography free journals Ultrasonography best journals Ultrasonography top journals Ultrasonography free medical journals Ultrasonography famous journals Ultrasonography Google Scholar indexed journals Magnetic Resonance Imaging articles Magnetic Resonance Imaging Research articles Magnetic Resonance Imaging review articles Magnetic Resonance Imaging PubMed articles Magnetic Resonance Imaging PubMed Central articles Magnetic Resonance Imaging 2023 articles Magnetic Resonance Imaging 2024 articles Magnetic Resonance Imaging Scopus articles Magnetic Resonance Imaging impact factor journals Magnetic Resonance Imaging Scopus journals Magnetic Resonance Imaging PubMed journals Magnetic Resonance Imaging medical journals Magnetic Resonance Imaging free journals Magnetic Resonance Imaging best journals Magnetic Resonance Imaging top journals Magnetic Resonance Imaging free medical journals Magnetic Resonance Imaging famous journals Magnetic Resonance Imaging Google Scholar indexed journals Radiological imaging articles Radiological imaging Research articles Radiological imaging review articles Radiological imaging PubMed articles Radiological imaging PubMed Central articles Radiological imaging 2023 articles Radiological imaging 2024 articles Radiological imaging Scopus articles Radiological imaging impact factor journals Radiological imaging Scopus journals Radiological imaging PubMed journals Radiological imaging medical journals Radiological imaging free journals Radiological imaging best journals Radiological imaging top journals Radiological imaging free medical journals Radiological imaging famous journals Radiological imaging Google Scholar indexed journals Canal of The Nuck articles Canal of The Nuck Research articles Canal of The Nuck review articles Canal of The Nuck PubMed articles Canal of The Nuck PubMed Central articles Canal of The Nuck 2023 articles Canal of The Nuck 2024 articles Canal of The Nuck Scopus articles Canal of The Nuck impact factor journals Canal of The Nuck Scopus journals Canal of The Nuck PubMed journals Canal of The Nuck medical journals Canal of The Nuck free journals Canal of The Nuck best journals Canal of The Nuck top journals Canal of The Nuck free medical journals Canal of The Nuck famous journals Canal of The Nuck Google Scholar indexed journals hematoma articles hematoma Research articles hematoma review articles hematoma PubMed articles hematoma PubMed Central articles hematoma 2023 articles hematoma 2024 articles hematoma Scopus articles hematoma impact factor journals hematoma Scopus journals hematoma PubMed journals hematoma medical journals hematoma free journals hematoma best journals hematoma top journals hematoma free medical journals hematoma famous journals hematoma Google Scholar indexed journals neurofibroma sarcoma articles neurofibroma sarcoma Research articles neurofibroma sarcoma review articles neurofibroma sarcoma PubMed articles neurofibroma sarcoma PubMed Central articles neurofibroma sarcoma 2023 articles neurofibroma sarcoma 2024 articles neurofibroma sarcoma Scopus articles neurofibroma sarcoma impact factor journals neurofibroma sarcoma Scopus journals neurofibroma sarcoma PubMed journals neurofibroma sarcoma medical journals neurofibroma sarcoma free journals neurofibroma sarcoma best journals neurofibroma sarcoma top journals neurofibroma sarcoma free medical journals neurofibroma sarcoma famous journals neurofibroma sarcoma Google Scholar indexed journals
Article Details
1. Introduction
The canal of Nuck was first described by the Dutch anatomist Anton Nuck in 1691. The hydrocele of canal of Nuck, also called as female hydrocele or the cyst of canal of Nuck is a very rare condition. Canal of nuck in females is homologous to a patent processus vaginalis in males which also predispose to indirect inguinal hernia and hydrocele of spermatic cord. Thus hydrocele of canal of nuck in females is equivalent to encysted hydrocele of cord in males [1]. The canal of Nuck is normally obliterated in the first year of life but failure to achieve complete obliteration results in an indirect inguinal hernia or hydrocele of canal of nuck. The fluid in the hydrocele of canal of nuck is likely due to imbalance of the secretion and absorption of the secretary membrane lining the processus vaginalis. Usually, it is idiopathic but sometimes trauma or infection may cause disruption of lymphatic drainage which may lead to imbalance.
2. Clinical presentation
Hydrocele of the canal of nuck typically presents as a painless swelling in the inguinolabial region. If the bulge is apparent in standing position and disappears while supine, a hernia is more plausible [2]. Hydroceles can be painful and cause a red swelling extending to the labia major in case of infection.
3. Pathophysiology
During foetal development in females there is evagination of the parietal peritoneum along the round ligament, through the inguinal ring, and into the inguinal canal just like processus vaginalis in males. This portion of processus vaginalis within the inguinal canal in women is called the ‘Canal of Nuck’. If the processus vaginalis does not close, it is referred to as a patent processus vaginalis. If the patent processus vaginalis is small and only allows fluid to pass, the condition will lead to peritoneal fluid accumulation or a (communicating) hydrocele. If the patent processus vaginalis is larger and allows abdominal organs to protrude, the condition is referred to as hernia [3,4].
The fluid in the hydrocele of canal of nuck is likely due to imbalance of the secretion and absorption of the secretary membrane lining the processus vaginalis. Usually, it is idiopathic but sometimes trauma or infection may cause disruption of lymphatic drainage which may lead to imbalance.
4. Classification of Hydrocele of the Canal of The Nuck
Classification of hydrocele of the canal of Nuck has been described as follows [3]:
4.1 Type 1:
An encysted hydrocele is a kind of cyst that develops as a consequence of partial obliteration of just the proximal portion of the canal of nuck. Typical clinical presentation is a nonreducible, painless mass whose volume remains unchanged when the Valsalva maneuver is performed [4]. When there is an imbalance between fluid secretion and absorption, which can occur as a result of trauma, inflammation, or lymphatic drainage impairment, the cyst can abruptly grow in size [5]. Within a closed cyst, an infection might develop following a slight trauma or intracystic hemorrhage. The patient may complain of a painful mass that is mistaken for an incarcerated hernia [6].
4.2 Type 2:
A communicating hydrocele. This pathology occurs from the patency of the canal of nuck. It appears as a non-tender reducible mass that may only arise after performing the Valsalva maneuver or standing.
4.3 Type 3:
A combined type. The lesion has an encysted inferior section in the inguinal canal and labia majora, as well as an upper intraabdominal portion. The hydrocele is compressed by the deep inguinal ring, creating an hourglass appearance.
5. Radiographic Features
Various radiographic modalities, including MRI, CT, and US can be used individually or in combination to diagnose canal of nuck hydrocele. Sonography proves to be a very powerful tool in elucidating the features of the hydrocele, especially in comparison to hernias. Ultrasonography can be initial imaging because of its low cost and wide availability, MRI could be used for complex cases and further investigations [7], because MRI can give more precise images including septations and a communication between cystic lesion and the peritoneal cavity and information on the anatomical relations with adjacent structures.
5.1 Ultrasound
Typically presents as a cystic mass lying superficially and medially to the pubic bone at the level of the superficial inguinal ring [8]. There should be no change with the Valsalva maneuver. Ultrasound is particularly useful because of its “real-time” nature and ability to precisely depict superficial structures. Ultrasound is an excellent technique to help exclude the presence of bowel in the swelling as seen in an inguinal hernia.
5.2 Computed Tomography Scan
Literature on CT findings for this condition is scarce. The usual CT findings of hydrocele are as follows:
- Homogeneous fluid-filled unilocular cyst, extending to the labia
- The inguinal canal communication may not be identified on CT
5.3 Magnetic Resonance Imaging
MR showed a thin-walled tense cystic mass in the inguinal area.
In most, cases hydroceles are described to have a thin wall but sometimes the hydrocele may be thick-walled cystic appearance due to infection; the proximal part of the lesion is extending into the peritoneal cavity along the route of the round ligament; the distal part is blunt and extending towards the labium majus. The wall of the hydrocele may show mild contrast enhancement, especially when infected.
6. Treatment
Surgery (Open/Laparoscopic) is the treatment of choice for Hydrocele of canal of Nuck. To give advantages of minimal invasive surgery, laparoscopic excision of hydrocele of canal of Nuck on both sides with transabdominal preperitoneal repair was done in our cases.
7. Differential Diagnosis
Swelling of the inguinal region in a female may also result from a number of other conditions such as Inguinal hernia (usually hernial sac with bowel content instead of fluid), Tumor (lipoma, leiomyoma, sarcoma), Round ligament varicosities, Cyst, Abscess, Lymphadenopathy.
8. Case Presentation
8.1 Case 1:
A 45-years-old lady presented in OPD with swelling in bilateral inguino-labial region for last three months. There was no history of Diabetes, hypertension, any cardiac ailment, urinary tract infection, trauma or any infection in this region. On examination: The swellings were globular, cystic in consistency, not tender, about 4 cm × 2 cm on left side and 3 cm × 2 cm on right side. Her USG showed lobulated, thick-walled cystic lesions, few of which showing internal echos, seen in bilarteral inguinal regions measuring approximately 20 mm × 28 mm on left side and 18 mm × 34 mm on right side? Lymphangioma/Round ligament Cyst. MRI showed lobulated tubular fluid signal intensity lesions in left pelvic inguinolabial and right inguinolabial regions extending along the round ligaments suggestive of hydrocele of canal of nuck/Mesothelial cysts of the round ligament. Laparoscopic excision of hydrocele of canal of nuck on both sides with transabdominal preperitoneal repair was done. Her histo-pathological report revealed loose connective tissue with mesothelial lining with mild chronic inflammatory infiltrate, congestion of blood vessels and fibrosis suggestive of bilateral hydrocele of canal of nuck (Figure 1).
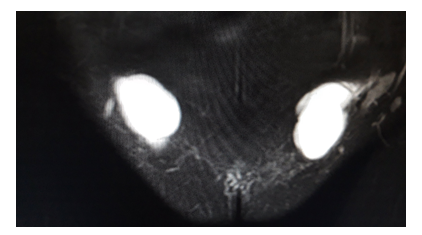
Figure 1: MRI of Case 1 showing bilateral hydrocele of canal of nuck.
8.2 Case 2:
A 35-years-old lady presented in OPD with swelling left Inguino-labial region for last 4-5 months. Earlier 2 ml fluid was aspirated from it for FNAC. There is no history of DM, HT or any cardiac ailment. She is a known case of Hyperthyroidism. On examination it was a diffuse (not very prominent because size has reduced after aspiration) cystic swelling in left inguino-labial region. USG showed left sided inguinal cystic mass of 1.6 cm × 0.8 cm size with clear fluid inside and no communication with the peritoneum. There was no change with the Valselva maneuver. Most likely Hydrocele of canal of nuck. FNAC shows average cellular smear predominantly acellular necrotic material along with cyst macrophages and inflammatory cells-suggestive of cystic nature of swelling MRI Pelvis showed fluid in the inguinal canal from deep to superficial inguinal ring-possibility of Hydrocele of canal of Nuck. Laparoscopic exicision of Hydrocele of canal of nuck along with mesh repair was done. Histopathology showed loose connective tissue with congested blood vessels and denuded ill-defined mesothelial lining. Focal mild chronic infiltrate, fibrosis and edema suggestive of hydrocele of canal of nuck.
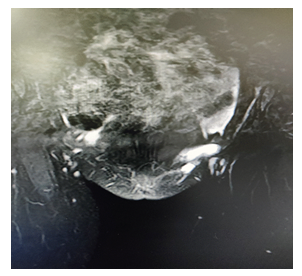
Figure 2: MRI of case 2 showing left hydrocele of canal of nuck.
9. Discussion
The canal of nuck was first described by a Dutch Anatomist Anton Nuck in 1691. The processus vaginalis in females is known as canal of nuck. The homologous structure in men is called the processus vaginalis [9]. Hydrocele of canal of Nuck should always be considered in differential diagnosis of inguinal swelling in females along with hernia, lymphadenopathy, abscess, cyst, tumors like Lipoma, Liposarcoma, neurofibroma sarcoma, hematoma [10,11]. Hydrocele of canal of nuck is usually painless but sometimes symptoms can be acute or chronic and infections of the hydrocele are also possible. Ultrasonography can be initial imaging because of its low cost and wide availability, MRI could be used for complex cases and further investigations [7] because MRI can give 123 more precise images including septations and a communication between cystic lesion and the peritoneal cavity and information on the anatomical relations with adjacent structures [12-17]. The hydrocelectomy with mesh repair is the treatment of choice.
10. Conclusion
Hydrocele of canal of nuck, although very rare, should always be considered in differential diagnosis of inguinal swelling in females along with hernia, lymphadenopathy, abscess, cyst, tumors like Lipoma, Liposarcoma, neurofibroma sarcoma, hematoma.
References
- Anderson CC, Broadie TA, Mackey JE, et al. Hydrocele of the canal of nuck: Ultrasound appearance. The American Surgeon 61 (1995): 959-961.
- De meulder F, Wojciechowski M, Hubens G, et-al. Female hydrocele of the canal of Nuck: a case report. Eur J Pediatr 165 (2006): 193-194.
- Counseller VS, Black BM. Hydrocele of the canal of nuck: Report of seventeen cases. Ann Surg 113 (1941): 625-630.
- Brainwood M, Beirne G, Fenech M. Persistence of the processus vaginalis and its related disorders. Australas J Ultrasound Me 23 (2020): 22-29.
- Stickel WH, Manner M. Female hydrocele (cyst of the canal of Nuck): sonographic appearance of a rare and little-known disorder. J Ultrasound Med 23 (2004): 429-432.
- Mandhan P, Raouf Z, Bhatti K. Infected hydrocele of the canal of Nuck. Case Rep Urol 2013 (2013): 275257.
- Thomas AK, Thomas RL, Thomas B. Canal of nuck abnormalities. Journal of Ultrasound in Medicine 39 (2020): 385-3955.
- Shadbolt CL, Heinze SB, Dietrich RB. Imaging of groin masses: inguinal anatomy and pathologic conditions revisited. Radiographics 21 (2001): S261-S71.
- Rees MA, Squires JE, Tadros S, et al. Canal of nuck hernia: A multimodality imaging review. Pediatric Radiology 47 (2017): 893-898.
- Fikatas P, Megas IF, Mantouvalou K, et al. Hydroceles of the canal of nuck in adults-diagnostic, treatment and results of a rare condition in females. Journal of Clinical Medicine 9 (2020): 4026.
- Sarkar S, Panja S, Kumar S. Hydrocele of the canal of nuck (Female hydrocele): A rare differential for Inguino-Labial Swelling. Journal of Clinical and Diagnostic Research 10 (2016): PD21-PD22.
- Park SJ, Lee HK, Hong HS, et al. Hydrocele of the canal of Nuck in a girl: ultrasound and MR appearance. Br J Radiol 77 (2004): 243-244.
- Tubbs RS, Loukas M, Shoja MM, et al. Indirect inguinal hernia of the urinary bladder through a persistent canal of Nuck: case report. Hernia 11 (2007): 287-288.
- Hydrocele and Hernia in Children by Joseph Ortenberg from emedicine.com. Hydrocele and Hernia in Children.
- De meulder F, Wojciechowski M, Hubens G, et al. Female hydrocele of the canal of nuck: a case report. Eur J Pediatr 165 (2006): 193-194.
- Shadbolt CL, Heinze SB, Dietrich RB. Imaging of groin masses: inguinal anatomy and pathologic conditions revisited. Radiographics 21 (2001): S261-S271.
- Ryu KH, Yoon JH. Ultrasonographic diagnosis of round ligament varicosities mimicking inguinal hernia: report of two cases with literature review. Ultrasonography (Seoul, Korea) 33 (2014): 216-221.
