Hybrid Ilizarov’s Method and Fibular Strut for Humeral Diaphyseal Nonunion: A Case Report after Multiple Failed Plating
Article Information
Sujan Shakya1*, Roshan Lal Shrestha2, Shikshya Prakash Shrestha2, Niraj Shrestha2, Umesh Bahadur Bogatee2, Anil Shakya2
1Department of Orthopedics, West China Hospital, Sichuan University, Chengdu, Sichuan, China
2Department of Orthopedics, Kathmandu Model Hospital, Exhibition Road, Kathmandu, Nepal
*Sujan Shakya, Department of Orthopedics, West China Hospital, Sichuan University, Chengdu, Sichuan, China.
Received: 10 July 2022; Accepted: 25 July 2022; Published: 29 July 2022
Citation: Sujan Shakya, Roshan Lal Shrestha, Shikshya Prakash Shrestha, Niraj Shrestha, Umesh Bahadur Bogatee, Anil Shakya. Hybrid Ilizarov’s Method and Fibular Strut for Humeral Diaphyseal Nonunion: A Case Report after Multiple Failed Plating. Journal of Orthopedics and Sports Medicine 4 (2022): 211-216.
View / Download Pdf Share at FacebookAbstract
Humeral diaphyseal fracture with non-union and failed implant in situ is a complex case. It is more challenging when the case is accompanied by infection, multiple ORIF, and osteopenic bone. Smoking and alcohol consumption synergically enhances delay in fracture healing and nonunion. The various surgical procedures are prevalent and conducted by orthopedic surgeons for its management. We hereby present a complex case of non-union humeral shaft fracture with an implant in situ by the use of autologous fibula strut as a biological nail to fit the non-union gap stabilized by K-wire and hybrid Ilizarov’s external fixator for mechanical support in a single setting. During this process, radical bone debridement was done. At 9 months of follow-up, bone union was achieved and the implants were removed. The final functional outcome was graded as good according to QuickDASH shoulder score with improved shoulder and absence of pain at the non-union site.
Keywords
Humeral shaft; Non-union; Ilizarov fixation; Bone defect; Fibula bone graft
Article Details
1. Introduction
Humeral shaft fractures constitute about 3% - 8% of all the fractures [1,2]. The incidence of humeral shaft fracture that undergoes non-union after Open Reduction and Internal Fixation (ORIF) accounts for 15% - 30% [2,3]. The most common classification of non-union has been proposed by Weber and Cech as hypertrophic and atrophic non-union .The most common treatment option for long bone non-union are intramedullary nailing, dynamic or locking compression plate with bone grafting, Ilizarov fixation followed by bone grafting with vivid clinical results.
Smoking, alcohols, diabetes mellitus, age, unstable primary osteosynthesis, open fractures, vessel injuries, and infections are the common risk factors for developing a non-union [4]. Osteopenia, osteoporosis, and soft tissue damage with extensive skin scar increases the likelihood of repeated fracture of metallic implantations in long bone such as femur, tibia, and humerus [5]. In infected non-union, the concept of management are implant removal, debridement, external fixation, subside infection, grafting, and / or internal fixation which is a challenging job for the orthopedic surgeons.
The purpose of this case report was to illustrate the outcome of free fibular strut grafting and application of the hybrid Ilizarov’s method in the treatment of atrophic non-union of humerus shaft fracture that has failed ORIF multiple attempts. This case report shall add evidence based operative procedure to the growing literature.
2.Case Report
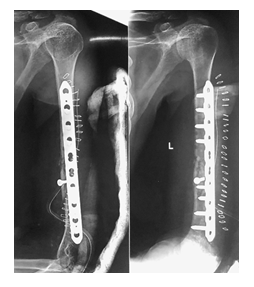
A 40-year old man suffered an isolated closed left humeral shaft fracture with intact Distal Neurovascular System (DNVS) after a motorbike fall, 4 years ago (2017) (Figure 1). His denying history of hypertension, diabetes, and other chronic medical comorbidities. He had the habit of drinking and smoking a pack of cigarettes for 20 years. At a local institute, he was treated conservatively with long hanging cast. In 3 months, fracture healed with hypertropic non-union accompanied with limited range of activity and pain in the arm (Figure 2). He was surgically treated by Open Reduction and Internal Fixation (ORIF) with Dynamic Compression Plate (DCP) without postoperative complications (Figure 3).
Within 3 months, he again complained with pain on the arm and restricted movement of the shoulder. Upon X-ray examination, he sustained the screws backout and implant loosening (Figure 4). Thereafter, he was surgically managed at the same institute with Limited Contact Dynamic Compression Plate (LCDCP) with Iliac bone autografting (Figure 5). After 28 months (2019) from initial injury time, the patient presented in our department with pain in the arm, swollen, restricted Range of Motion (ROM) of shoulder and elbow and intact DNVS. There was no sinus discharge, or keloid scar.
On examination, his left biceps, triceps, and forearm muscles had atrophied. His left arm was shortened approximately 3 cm compared with the contralateral arm. The blood parameters evaluation showed increase in Erythrocyte Sedimentation Rate (ESR), C-reactive protein (CRP) and White Blood Cells (WBC) counts. The radiograph showed atrophic non-union of humerus diaphysis, loosening and lysis at the screw and plate surface (Figure 6).
We decided to manage this complex, infected and atrophic, non-union of left humeral shaft fracture by radical debridement, fibular strut grafting and Ilizarov fixation in a single sitting.
3. Surgical Procedure
At first, the required autologous fibular strut was harvested (a length of 5-6 cm) with the distal fibula being left in place for ankle stability (Figure 7). This fibular strut, or “biological nail,” was fashioned to fit the host humerus medullary canal as the biological strut should be inserted into the host bone as early as possible to maximize its viability.
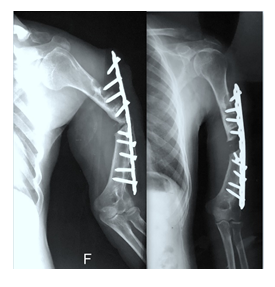
The 4-5 cm anterior deltopectoral approach incision was adopted to expose the humeral shaft. The radial nerve was isolated between brachioradialis and brachialis. The broken plate was removed entirely. The radial nerve was seen hypertrophied with the fibrotic bands. Deep tissue was obtained for culture. The radical debridement around the bone was carried with excision of fibrous tissue and callus. The medullary canal was minimally shaved and reamed. The full-length fibular graft was inserted into the medullary cavity of the humerus proximally and distally. At the time of the procedure, a Kirschner wire was inserted through the proximal humerus passing through the fibular graft distally. These helped to intact the strut and increased the strength and minimize the displacement (Figure 8).
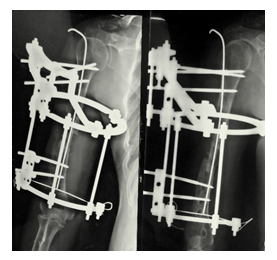
3.1 Ilizarov fixation
The hybrid Ilizarov ring external fixator configuration was preconstructed before surgery by measuring the length and height of the X-rays films and the affected arm. After the placement of the fibular graft, the immediate Ilizarov ring was installed. The proximal ring was fixed with the three Schanz screws over the proximal humerus, mid-ring was fixed to the mid-shaft humeral diaphysis, and the distal ring was fixed using 2 Schanz screws and one 1.8 mm k wire drilled over the distal humerus. The ring was position just anteriorly to the elbow to facilitate the elbow range of motion. Special care was taken to avoid nerve injuries while drilling the Ilizarov trans-osseous implant. The installation was verified with the C-arm image intensifier. The wound closure was carried out and pin sites were cleaned and dressed in a sterile manner.
3.2 Post-operative care
At each clinical visit, the patient was informed and given instructions about the pin site care and sterile dressing with 0.5% chlorhexidine solution and mupirocin ointment. The pin site was inspected at each visit for swelling, erythema, purulent drainage, or pain. The result of deep tissue culture was negative. However, intravenous third generation prophylactic antibiotics was used for 5 days. Active and passive joint mobilization of elbow, hand, wrist as tolerated was instructed. Ultrasonic wave therapy was also done to increase the osteogenic activity. X-rays (AP, Lateral, Oblique views) were taken to observe the bone compression, callus formation.
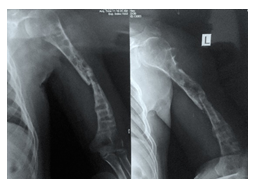
The results of the treatment were assessed on the basis of clinical and radiographic evidence of union, time to union, and the function of the extremity. The complete bone union took place after 9 months. The Ilizarov fixator was removed as a daycare elective operative procedure and the patient was discharged on the same day with pain management medications, oral antibiotics, and long arm slab (Figure 9). A postoperative sling was used to protect the arm for a week .Then Sarmeinto bracing was applied in the affected arm. Pin site dressing was done every alternative day. The QuickDASH score after one month was found to be 25 which were clinically satisfying with no disability. This score was designed be useful in patients with any musculoskeletal disorder of the upper limb. The scores range from 0 (no disability) to 100 (most severe disability) [6]. The patient had improved shoulder abduction, improved movement in elbow flexion and extension, shoulder joint strength, and absence of pain at the non-union site (Figure 10).
4.Discussion
Humerus fracture is one of the long bone fractures and is still managed conservatively with good functional outcome. Due to the fact that, shortening up to 3 cm, rotation of less than 30 degree and angulation up to 20 degree are acceptable for non-operative management with functional bracing [7]. However, non-union occurs up to 10 % in such fractures after conservative treatment and further treatment of such condition can be burdensome with complications [8]. After repeated implant failures, non-union is often resistant to treatment. Moreover, infected humeral non-union is more challenging relative to uninfected cases [9]. In such case, bone is often osteoporotic and osteopenic and fixation is difficult to achieve due to implant loosening and inhibition of osteogenesis [5]. The development of this non-union also synergized by smoking and alcohol abuse, poor patient compliance and irregular follow-ups. The smoking and alcohol consumption negatively affects in the bone fracture healing [10]. Smoking has a negative impact on Bone Mineral Density (BMD), reducing calcium absorption and lowering levels of vitamin D, changes hormone levels, and reduces body mass [11]. The increase of non-union and rate after plating in proximal humerus fractures with smoking was found in a clinical study [12]. The risk for development of non-union after ORIF was 3.9-fold higher in heavy smokers (>20cigarettes per day) [13].
We utilized fibular strut with Ilizarov fixation for successful bone union to achieve clinical outcomes. We believe that fibula graft worked as a biological nail that engaged with the host bone firmly. The additional ring fixator helped as mechanical protection to minimize the displacement and infection. Fibula graft is a fresh cancellous autograft with the properties of osteoconduction, osteogenic, and osteoinduction. The property of autogenic cancellous bone can function as a good structure, which might facilitate mesenchymal stem cells associated with bone regeneration, adding the osteogenic activity to the necrosis area and benefiting the repair of the defects [14]. We must be conscious that non-vascularized fibula graft has the risk of absorption, necrosis, and takes time to incorporate. Thus, well debridement and immediate insertion of graft are essential to retain the available bone properties. The non-vascularized grafts are inferior about integration, resistance to bacterial infection, and hypertrophy compared to vascularized grafts [15]. However, there is evidence in the literature that even non-vascularized bone grafts are also capable of remodeling and integrating into the host bone [16,17]. Likewise, the integration of avascular grafts could be attributed to periosteal hypertrophy leading to new bone formation around the graft and eventual bony integration of the graft in some cases [18].
Patients with non-union with multiple implant failures previously treated with ORIF by plating exhibits metal reaction leading to metallosis with implant breakage, metal debris, bony erosion with extensive bone loss, scalloping around screws, and osteopenia [2]. Such cases differ from routine procedures as it is difficult to manage to predict the favorable outcome. In a case like ours, complications such as multiple implant failure, poor bone quality, infections and non-union exist. Therefore, the surgical correction with DCP or LCP or double plating may not provide a reliable outcome. Instead, it could cause extensive soft tissue stripping leading to vessel and nerve damage. Therefore, we intended to use Ilizarov technique as it has been successfully established as a gold standard for treating all types of non-unions, defects and bone infection [19]. The application of ring fixator enables the conversion of incumbent deformity either intraoperatively or gradually postoperatively [20]. Even though, it has disadvantages of bulky apparatus on the arm, impingement of the apparatus skin, pin tract infection, associated vessel and nerve damage while K-wire insertion, time-consuming, and social hesitation.
In summary, the treatment goal of non-union, infected diaphyseal fracture of the humerus can be achieved with biological stimulation using fibula strut, mechanical stabilization using Ilizarov ring fixator in the arm, and early mobilization for better clinical outcome.
Funding
There was no external source of funding for this study.
References
- Updegrove GF, Mourad W, Abboud JA. Humeral shaft fractures. Journal of shoulder and elbow surgery 27 (2018): e87-e97.
- Kashayi-Chowdojirao S, Vallurupalli A, Chilakamarri VK, et al. Role of autologous non-vascularised intramedullary fibular strut graft in humeral shaft nonunions following failed plating. J Clin Orthop Trauma 8 (2017): S21-S30.
- Padhye KP, Kulkarni VS, Kulkarni GS, et al. Plating, nailing, external fixation, and fibular strut grafting for non-union of humeral shaft fractures. Journal of orthopaedic surgery (Hong Kong) 21 (2013): 327-331.
- Leiblein M, Verboket R, Marzi I, et al. Nonunions of the humerus – Treatment concepts and results of the last five years. Chinese Journal of Traumatology 22 (2019): 187-195.
- Yadav SS. The Use of a Free Fibular Strut as a "Biological Intramedullary Nail" for the Treatment of Complex Nonunion of Long Bones. JB and JS open access 3 (2018): e0050.
- Beaton DE, Wright JG, Katz JN. Development of the QuickDASH: comparison of three item-reduction approaches. The Journal of bone and joint surgery American volume 87 (2005): 1038-1046.
- Papasoulis E, Drosos GI, Ververidis AN, et al. Functional bracing of humeral shaft fractures. A review of clinical studies. Injury 41 (2010): e21-e27.
- Wali MGR, Baba AN, Latoo IA, et al. Internal fixation of shaft humerus fractures by dynamic compression plate or interlocking intramedullary nail: a prospective, randomised study. Strategies Trauma Limb Reconstr 9 (2014): 133-140.
- Li XK, Wang HQ, Wei YY, et al. Treatment of nonunions of humeral fractures with interlocking intramedullary nailing. Chinese journal of traumatology=Zhonghua chuang shang za zhi 11 (2008): 335-340.
- Xu B, Chen L, Lee JH. Smoking and alcohol drinking and risk of non-union or delayed union after fractures: A protocol for systematic review and dose–response meta-analysis. Medicine 99 (2020): e18744.
- Hernigou J, Schuind F. Tobacco and bone fractures: A review of the facts and issues that every orthopaedic surgeon should know. Bone Joint Res 8 (2019): 255-265.
- Boesmueller S, Wech M, Gregori M, et al. Risk factors for humeral head necrosis and non-union after plating in proximal humeral fractures. Injury 47 (2016): 350-355.
- Boesmueller S, Wech M, Gregori M, et al. Risk Factors for Humeral Head Necrosis and Non-Union After Plating in Proximal Humeral Fractures. Injury 47 (2015).
- Changjun C, Donghai L, Xin Z, et al. Mid- to long-term results of modified non-vascularized allogeneic fibula grafting combined with core decompression and bone grafting for early femoral head necrosis. Journal of Orthopaedic Surgery and Research 15 (2020): 116.
- Soucacos PN, Korompilias AV, Vekris MD, et al. The free vascularized fibular graft for bridging large skeletal defects of the upper extremity. Microsurgery 31 (2011): 190-197.
- Schuh R, Panotopoulos J, Puchner SE, et al. Vascularised or non-vascularised autologous fibular grafting for the reconstruction of a diaphyseal bone defect after resection of a musculoskeletal tumour. The bone and joint journal 96 (2014): 1258-1263.
- Krieg AH, Lenze U, Gaston MS, et al. The outcome of pelvic reconstruction with non-vascularised fibular grafts after resection of bone tumours. The Journal of bone and joint surgery British volume 92 (2010): 1568-1573.
- de Boer HH, Wood MB. Bone changes in the vascularised fibular graft. The Journal of bone and joint surgery British volume 71 (1989): 374-378.
- Gubin A, Borzunov D, Marchenkova L, et al. Contribution of G.A. Ilizarov to bone reconstruction: historical achievements and state of the art. Strategies Trauma Limb Reconstr 11 (2016).
- Kiran M, Jee R. Ilizarov's method for treatment of nonunion of diaphyseal fractures of the humerus. Indian journal of orthopaedics 44 (2010): 444-447.