How Does Online Health Information Impact Senior Patients’ Perception of Control in Collaborative Decision-making Process with Physicians?
Article Information
Mehraneh Shantiaei*
*School of Information Systems and Technology, Claremont Graduate University, Claremont, CA, 91711, USA
*Corresponding Author: Mehraneh Shantiaei, PhD, School of Information Systems and Technology, Claremont Graduate University, Claremont, CA, 91711, USA
Received: 09 January 2021; Accepted: 18 January 2021; Published: 26 January 2021
Citation: Mehraneh Shantiaei. How Does Online Health Information Impact Senior Patients’ Perception of Control in Collaborative Decision-making Process with Physicians?. Fortune Journal of Health Sciences 4 (2021): 221-242.
View / Download Pdf Share at FacebookAbstract
The American population is aging. The rise of healthcare costs of the aging population in the USA is becoming a national challenge. Fortunately, patient–physician collaborative decision making (CDM) has shown to be an effective way to improve health outcomes and to lower costs. Additionally, the Internet has proven to be a rich source of health information for patients. The aim of this study was to examine senior patients’ perceptions regarding CDM and the impact of using online health information (OLHI) on their perceived control in the CDM process with physicians. The study used a mixed method approach, including quantitative and qualitative methods. Data was collected through surveys and open-ended interviews. A total of 73 senior patients and 14 physicians were surveyed. Senior patients were the main group of participants, and the physicians were recruited just to validate the collected data obtained on the patient side. Among the patients, 50 individuals were OLHI users, and 23 were not. A total of 20 patient participants volunteered to be interviewed. Interviews were face-to-face, open-ended, and semi-structured. Conducting t-tests on the quantitative data showed that the OLHI users in comparison to the non-OLHI users perceive more control in the CDM process with their physicians through higher levels of 1) patient-physician collaborative information exchange; 2) collaborative decision-making behavior of physicians; and 3) willingness to be authoritative in the clinical CDM process. Moreover, descriptive statistics as well as qualitative analysis supported the quantitative results, revealing the positive impact of using OLHI on senior patient empowerment.
Keywords
Patient-Physician Relationship; Patient-Physician Communication; Collaborative Clinical Decision-Making; Online Health Information; Information Exchange; Perceived Control; Health Outcomes, Elderly Healthcare; Ageism; Trust, Empathy, and Rapport
Patient-Physician Relationship articles; Patient-Physician Communication articles; Collaborative Clinical Decision-Making articles; Online Health Information articles; Information Exchange articles; Perceived Control articles; Health Outcomes articles, Elderly Healthcare articles; Ageism articles; Trust articles, Empathy articles, and Rapport articles, Patient-Physician Relationship articles Patient-Physician Relationship Research articles Patient-Physician Relationship review articles Patient-Physician Relationship PubMed articles Patient-Physician Relationship PubMed Central articles Patient-Physician Relationship 2023 articles Patient-Physician Relationship 2024 articles Patient-Physician Relationship Scopus articles Patient-Physician Relationship impact factor journals Patient-Physician Relationship Scopus journals Patient-Physician Relationship PubMed journals Patient-Physician Relationship medical journals Patient-Physician Relationship free journals Patient-Physician Relationship best journals Patient-Physician Relationship top journals Patient-Physician Relationship free medical journals Patient-Physician Relationship famous journals Patient-Physician Relationship Google Scholar indexed journals Patient-Physician Communication articles Patient-Physician Communication Research articles Patient-Physician Communication review articles Patient-Physician Communication PubMed articles Patient-Physician Communication PubMed Central articles Patient-Physician Communication 2023 articles Patient-Physician Communication 2024 articles Patient-Physician Communication Scopus articles Patient-Physician Communication impact factor journals Patient-Physician Communication Scopus journals Patient-Physician Communication PubMed journals Patient-Physician Communication medical journals Patient-Physician Communication free journals Patient-Physician Communication best journals Patient-Physician Communication top journals Patient-Physician Communication free medical journals Patient-Physician Communication famous journals Patient-Physician Communication Google Scholar indexed journals Collaborative Clinical Decision-Making articles Collaborative Clinical Decision-Making Research articles Collaborative Clinical Decision-Making review articles Collaborative Clinical Decision-Making PubMed articles Collaborative Clinical Decision-Making PubMed Central articles Collaborative Clinical Decision-Making 2023 articles Collaborative Clinical Decision-Making 2024 articles Collaborative Clinical Decision-Making Scopus articles Collaborative Clinical Decision-Making impact factor journals Collaborative Clinical Decision-Making Scopus journals Collaborative Clinical Decision-Making PubMed journals Collaborative Clinical Decision-Making medical journals Collaborative Clinical Decision-Making free journals Collaborative Clinical Decision-Making best journals Collaborative Clinical Decision-Making top journals Collaborative Clinical Decision-Making free medical journals Collaborative Clinical Decision-Making famous journals Collaborative Clinical Decision-Making Google Scholar indexed journals Online Health Information articles Online Health Information Research articles Online Health Information review articles Online Health Information PubMed articles Online Health Information PubMed Central articles Online Health Information 2023 articles Online Health Information 2024 articles Online Health Information Scopus articles Online Health Information impact factor journals Online Health Information Scopus journals Online Health Information PubMed journals Online Health Information medical journals Online Health Information free journals Online Health Information best journals Online Health Information top journals Online Health Information free medical journals Online Health Information famous journals Online Health Information Google Scholar indexed journals Information Exchange articles Information Exchange Research articles Information Exchange review articles Information Exchange PubMed articles Information Exchange PubMed Central articles Information Exchange 2023 articles Information Exchange 2024 articles Information Exchange Scopus articles Information Exchange impact factor journals Information Exchange Scopus journals Information Exchange PubMed journals Information Exchange medical journals Information Exchange free journals Information Exchange best journals Information Exchange top journals Information Exchange free medical journals Information Exchange famous journals Information Exchange Google Scholar indexed journals Perceived Control articles Perceived Control Research articles Perceived Control review articles Perceived Control PubMed articles Perceived Control PubMed Central articles Perceived Control 2023 articles Perceived Control 2024 articles Perceived Control Scopus articles Perceived Control impact factor journals Perceived Control Scopus journals Perceived Control PubMed journals Perceived Control medical journals Perceived Control free journals Perceived Control best journals Perceived Control top journals Perceived Control free medical journals Perceived Control famous journals Perceived Control Google Scholar indexed journals Health Outcomes, Elderly Healthcare articles Health Outcomes, Elderly Healthcare Research articles Health Outcomes, Elderly Healthcare review articles Health Outcomes, Elderly Healthcare PubMed articles Health Outcomes, Elderly Healthcare PubMed Central articles Health Outcomes, Elderly Healthcare 2023 articles Health Outcomes, Elderly Healthcare 2024 articles Health Outcomes, Elderly Healthcare Scopus articles Health Outcomes, Elderly Healthcare impact factor journals Health Outcomes, Elderly Healthcare Scopus journals Health Outcomes, Elderly Healthcare PubMed journals Health Outcomes, Elderly Healthcare medical journals Health Outcomes, Elderly Healthcare free journals Health Outcomes, Elderly Healthcare best journals Health Outcomes, Elderly Healthcare top journals Health Outcomes, Elderly Healthcare free medical journals Health Outcomes, Elderly Healthcare famous journals Health Outcomes, Elderly Healthcare Google Scholar indexed journals Ageism articles Ageism Research articles Ageism review articles Ageism PubMed articles Ageism PubMed Central articles Ageism 2023 articles Ageism 2024 articles Ageism Scopus articles Ageism impact factor journals Ageism Scopus journals Ageism PubMed journals Ageism medical journals Ageism free journals Ageism best journals Ageism top journals Ageism free medical journals Ageism famous journals Ageism Google Scholar indexed journals Trust articles Trust Research articles Trust review articles Trust PubMed articles Trust PubMed Central articles Trust 2023 articles Trust 2024 articles Trust Scopus articles Trust impact factor journals Trust Scopus journals Trust PubMed journals Trust medical journals Trust free journals Trust best journals Trust top journals Trust free medical journals Trust famous journals Trust Google Scholar indexed journals Empathy articles Empathy Research articles Empathy review articles Empathy PubMed articles Empathy PubMed Central articles Empathy 2023 articles Empathy 2024 articles Empathy Scopus articles Empathy impact factor journals Empathy Scopus journals Empathy PubMed journals Empathy medical journals Empathy free journals Empathy best journals Empathy top journals Empathy free medical journals Empathy famous journals Empathy Google Scholar indexed journals
Article Details
Abbreviations:
CDM-Collaborative Decision Making; PDM-Participatory Decision Making; SDM-Shared Decision Making; OLHI-Online Health Information
1. Introduction
1.1 Rising costs of elderly healthcare
The issue of aging population is becoming an important national challenge in the United States of America. According to the U.S. Senate Special Committee on Aging (1991), by the year 2030, about 22% of the American population will age 65 and over [1]. Because of chronic diseases and age-related issues, the elderly needs more health-related resources than others. As an example, they usually need more and longer doctor visits. A research study in 1992 showed that by the year 2040, doctor visits needed by senior adults in the U.S. will double [2]. Such an extensive rise of physician visits as well as increase in other health care resources needed by the elderly is likely to cause an extensive rise in healthcare costs in this country.
Fortunately, there are some factors that can mitigate the aforementioned problems. Among these factors is clinical collaborative decision making as an effective model of patient-physician communication and interaction.
1.2 Patient-physician communication
Communication and interactions between patients and their physicians have been at the center of attention in numerous research studies conducted in the recent years. These studies have shown that effective relationship and communication between patients and their physicians can improve health outcomes through extensive impacts on patient safety, treatment, patient satisfaction, and in many cases, lowering the number of malpractice-lawsuits (Table 1). There have been several models for patient-physician relationship and communication. One of the most important and effective ones among them is patient-physician collaborative decision making (CDM). Research studies have shown that CDM is expected to play an important role in addressing the challenge of senior adult healthcare costs.
|
Quality factors affected by patient-physician relationship and communication |
Citations |
|
Patient safety |
[3-15] |
|
Patient satisfaction |
[16-28] |
|
Treatment adherence |
[16, 18-28] |
|
The risk of malpractice lawsuits |
[28-32] |
Table 1: Articles Citing the Impacts of Patient-Physician Communication on Health Quality Factors
1.3 Collaborative decision making (CDM)
Collaborative decision making (CDM) - also known as participatory decision making (PDM), or shared decision making (SDM)[1] – is an effective model of patient-physician relationship and communication. It is a process where the patient is involved in treatment decision making by physicians. There are numerous research studies in the existing literature emphasizing the important role of CDM in healthcare improvement [33-47]. Based on these studies, CDM has played an active role in 1) securing the goals of medicine, 2) providing patient autonomy, and 3) improving health outcomes.
CDM is a process where both a patient and a physician play important roles in a collaborative decision-making process regarding the treatment of the patient. In such a process, the physician provides the patient with required and relevant health information, the patient discloses her/his own preferences, the patient and physician discuss different options, and they reach an agreement on a joint decision which is consistent with the patient’s values and preferences [33,48,49]. This completely contrasts with the traditional models of clinical decision making, where treatment decisions were made solely by physicians, without considering patients’ concerns, values, and preferences. In particular, a CDM process can be used more appropriately in situations where: 1) the clinical evidence cannot support a single action as the best one, 2) there are some kinds of harm and benefit trade-off between different treatment options, and 3) the existing options are associated with a wide range of personal values [50]. CDM has proved to be an effective factor in health outcomes, including short-term outcomes (such as patient satisfaction), intermediate outcomes (including treatment adherence), and long-term outcomes (such as resolution of symptoms and improving the quality of life) [3,51]. Furthermore, a study [46] showed important advantages of CDM as to be: making clinical decision-making more ethical, more practically functional, and patient supportive.
[1] For the purpose of this study, the CDM abbreviation has been used rather than the PDM or SDM abbreviations.
1.4 Perceived control over CDM process
Control is characterized as a certain degree of influence over others, environments, or events. Perceived control has been defined as “the belief that one can determine one’s own internal states and behavior, influence one’s environment, and/or bring about desired outcomes” [52, P.1]. In recent years, one of the areas in which this concept has been highly used is individuals’ perceptions of control over their own health and treatments. Studies have shown that the individuals’ perceptions of control over their health problems, the symptoms, and the related treatment can affect their well-being in a positive manner [53,54]. In research studies pertaining to patient empowerment and patient autonomy, the concept of perceived control is very important. It should be noted that the concepts of control and responsibility are not equivalent. As stated by a study, responsibility is about “what one should do,” while control is about “what one is able to do” [52, p.2]. Control should not be mistaken for responsibility of treatment.
1.5 Online health information (OLHI)
Retrospectively, research studies have found that Internet health information (or online health information, OLHI) is an important resource for patients to improve their knowledge about health and their well-being [ 55-57]. The Internet has shown to be the largest medical library across the world. A study demonstrated that on a typical day where 70 million Americans went online, about 7 million people searched for health-related information [56]. Through improving health-related knowledge, OLHI enables patients to enhance their communication and interactions with their physicians. Researchers state that the Internet is expected to be a critical player in healthcare-related communication in the future [58-60]. In particular, OLHI has shown to be an important factor in senior healthcare. Use of this information can help seniors to: (1) become more knowledgeable about diseases they suffer from, (2) verify their doctors’ diagnostics, (3) compare different treatment options, (4) become more knowledgeable about the medication they are using, and (5) assess their physicians’ credentials [61,62]. Obviously, such capabilities can improve seniors’ roles in communication and collaborative decision making with physicians.
There exist numerous research studies in the current literature pertaining to the various sub-areas of the present study (including senior healthcare, patient-physician communications and interactions, clinical collaborative decision making, and using OLHI by patients). However, no one has investigated the intersections of all these areas. The present study aimed to fill this gap. It investigated the impact of the use of OLHI by senior patients on their perceived control in the CDM process with physicians during their visits. This article is based on the author’s doctoral dissertation research, which was conducted at Claremont Graduate University [88].
2. Materials and Methods
2.1 Research questions and hypotheses
2.1.1 Research question1: Is access and use of online health information associated with elderly patients’ perceptions of control in the collaborative decision-making process with physicians?.
2.1.2 Research question2: Are senior patients’ perceptions validated by physicians who treat elderly patients?.
2.1.3 Hypothesis: The access and use of online health information is associated with elderly patients’ perceived control, in a way that cause them to perceive more control in the collaborative decision- making process during physician visits.
2.2 Methodology rationale
The use of multiple methods can improve the validity of a research, because it will help ensure the completeness of the findings [63]. For this purpose, the present study used a mixed-method approach, including quantitative and qualitative methods. The reasons of the combination of these two particular methods were:
- Quantitative method, which was the main approach of the study, provided a scientific approach and facilitated an effective way of gathering information and studying the phenomenon from a distance.
- Qualitative method provided a wider and deeper angle lens to look at multiple dimensions of the phenomenon in an open-ended manner. The descriptive nature of qualitative data provided a better understanding of the overall picture.
Furthermore, through using a dual-perspective approach, the study included two complementary investigations: senior patients and physicians studies. While senior patients were considered as the main group of participants, physicians were also invited in order to validate the collected data on the patient side based on their own experience of interacting with senior patients. The quantitative method included patient and physician surveys. Through these surveys, senior patients’ attitudes and preferences regarding different aspects of the study were investigated. Additionally, in order to obtain the senior patients’ viewpoints in a more explanatory manner, multiple face-to-face, semi-structured, and open-ended interviews were conducted.
2.3 Participants
The study included two groups of participants: 73 senior patients, age 65 and over, and 14 physicians. Among the senior patients, 50 individuals were online health information users (OLHI users), and 23 were not (considered as non-OLHI users). Senior patients were the main group of participants, and physicians were recruited just to validate the data collected on the patient side. The study was conducted in Los Angeles County in the Southern CA. The majority of the patient participants (64.4%) were residing in retirement/senior communities located in this area. The remainders (35.6%) were those who live in their independent residences in the area.
The study used a dual-perspective approach to examine elderly patients’ perceptions about different aspects of the study, and physicians’ viewpoints and experiences regarding patients’ perspectives, attitudes, and preferences. In the cover letter of the surveys, the respondents were asked whether they would like to attend a 30-60-minute interview or not. If they volunteered to attend, interview sessions were scheduled at their convenience. Each interview was conducted at the interviewee’s residence.
2.4 Study sampling
Participants were selected based on purposeful sampling techniques introduced by [64]. Based on a number of criteria, participants, including senior patients and physicians, were chosen to participate in the current study. These criteria are mentioned below. In addition, in conducting interviews, the study employed samples of convenience, where participants volunteered to attend the interviews. In this way, the sampling used in the current study was not a purely random sampling method. The study also used a planned sample size. In the plan of this study, the desired size on the patient side was 50 patients to participate in the study. Moreover, based on some similar research studies, the expected participation rate was considered to be 60%. However, practically, 73 patients participated in the study, where the participation rate was not very clear because the survey distribution was mostly done by the senior communities’ administration offices. On the physician side, however, the participation rate was 30%.
2.5 Recruitment criteria
The following criteria were used to recruit participants:
Patients: Being age 65 or over, having the experiences of a number of interactions during doctors’ visits in the last few years, and being able to understand and speak English.
Physicians: Having the experience of interactions with senior patients, particularly those patients who have used online health information.
2.6 Recruitment resources
2.6.1 Senior patient recruitment resources: Senior patient recruitment was done through one of the following ways:
(a) Retirement/senior communities: Through contacting and negotiating with the administration offices of five senior communities in Los Angeles County area, the survey questionnaires were distributed among the residents. The mentioned senior communities were:
- Pilgrim Place (Claremont)
- Claremont Manor (Claremont)
- Mt San Antonio Gardens (Pomona)
- Hillcrest (La Verne)
- Joslyn Center (Claremont)
(b) Direct recruitment: A limited number of participants were recruited directly. They received the surveys via email, mail, or in person.
2.6.2 Physician recruitment resources: The physician participants of the study all were practicing in Los Angeles County area. The majority of them were recruited directly, through contacting by email or phone, and inviting to participate in the study. There was just an exception case. It was in Pomona Valley Hospital, where the investigator attended a regular event (weekly educational seminar) held in the hospital and delivered a presentation about the study and the need and importance of participation of the physicians in that. It was done with support of the hospital administration.
The surveys and the consent forms were sent to the physician participants via mail or email, or delivered in person at their convenience.
2.7 Data collection
The main purpose of collecting data was 1) to understand the needs, expectations, and viewpoints of elderly patients about CDM during doctor visits and their perceptions about how using of online health information can help them in such a process; 2) to understand the specific viewpoints and experiences of physicians regarding elderly patients’ perceptions and preferences about communication, CDM, and the impact of the use of online health information on these issues. Data gathering was done through surveys and in-depth interviews. The data gathering phase lasted 11 months.
2.7.1 Constructs and instruments: Associated with different aspects of the study, 10 theoretical constructs were identified. These constructs were the basis of the design of the instruments used for data gathering for both surveys and interviews. Table 2 shows these constructs. In accordance with these constructs, in design of the patient survey, two different groups of items were identified: the common items (the questions that were expected to be answered by the both groups of patients) and the OLHI-related items (the ones that were expected to be answered by just OLHI users). The physician survey was mostly included the same questions used in the patient survey. The physicians were asked to provide their viewpoints regarding the patients’ perspectives, expectations, and preferences based on the experiences gained by them in senior-patients visits. In the first step, the participants took part in the survey. In the questionnaires, respondents had been asked whether or not they would like to be interviewed. If their answers were positive, interviews were scheduled with them (after a few days). Interviews were in-depth and semi structured and were recorded, unless the interviewee refused.
2.7.2 Quantitative data gathering – surveys: All subjects of the study participated in the survey. In line with the objective of the study and the identified research questions, the design of the surveys and their items were based on the aforementioned theoretical constructs (Table 2). Since the main objective of the study was to compare the perspectives and perceptions of the two main sub-groups of the patient participants (OLHI users and non-OLHI users), the majority of the sub-parts and items (questions) in the patient survey were chosen to be common to the both groups (supposed to be responded by all the patient participants).
However, to obtain some particular information regarding the attitudes and behaviors of the online user participants, a number of questions were also designed related to the use of online health information. Furthermore, since the physicians’ responses were expected to provide a validation of the patients’ perspectives, the format and content of the physician survey were designed to be similar to the patient survey.
The response format of the items in the surveys was a 5-point Likert-type scale, with the five options as strongly disagree (1), disagree (2), neutral (3), agree (4), strongly agree (5).
73 surveys were completed by senior participants, and 14 ones were completed by physician participants.
2.7.3 Qualitative data gathering – interviews: Qualitative data in this study was gathered through a number of semi-structured and in-depth interviews. The semi-structured form of interviewing provided a better opportunity to collect the required data in a more flexible manner. 20 senior patients were interviewed. The interview locations were chosen based on the interviewees’ preferences. Each interview lasted about 60 minutes, and was recorded. Interviews were scheduled by person, through email, or by the administrative staff of the senior communities. A reminder - through a phone call, email, or text message - was made the day before the interview.
|
(1). Patients’ and Physicians’ Characteristics (demographics/general information) (2). Senior Patients’ Needs and Expectations (3). Trust, Empathy, and Rapport (4). Age and Gender- related Aspects (5). Online Health Information (6). Access to Online Health Information (7). Use of Online Health Information (8). Patient-Physician Communication and Interactions (9). Information Exchange (10). Collaborative Decision Making & Perceived Control |
Table 2: List of the Theoretical Constructs
2.8 Measurement and variables
2.8.1 Measures: The study measured elderly patients’ perceptions, attitudes, and preferences regarding different aspects of the research. The constructs considered in this study (Table 2) were the basis of the design of the instruments used for data gathering for both surveys and interviews. For each of the constructs multiple items were developed (both in the patient survey and physician survey).
Some of the measures and items employed in the present study have been adapted from some other studies conducted in the past. Moreover, in design of the survey items, some ideas were adapted, in a very general form, from the existing literature, including [33,57,65].
2.8.2. Independent variables: This group of variables were related to the general information and socio-demographic characteristics of the participants (construct #1 in Table 2). They included age, gender, ethnicity, educational level, marital status, health insurance status, etc. (for patients); age, gender, ethnicity, etc. (for physicians); health-status related variables (for patients); professionalism variables, such as specialty and clinical practice related variables (for physicians); situational characteristic variables, including visit time, information related to using the Internet (for both patients and physicians) and more. A description of the demographic and background information of the participants is provided in Tables 3,4, 5 and 6.
2.8.3. Dependent variables: These kinds of variables pertained to the specific attitudes, perceptions, and preferences of patient participants regarding different aspects of this study (as shown by the constructs 2-10 in Table 2).
|
Demographic Characteristic |
Non-online health information users (%) (n=23) |
Online health information users (%) (n=50) |
Total (%) (n=73) |
|
Age groups 65-74 75-84 85-94 |
8.2% 19.2% 4.1% |
27.4% 23.3% 17.8% |
35.6% 42.5% 21.9% |
|
Gender Female Male |
20.8% 9.7% |
36.1% 33.3% |
56.9% 43.1% |
|
Living place Live in retirement/senior communities Living in independent house |
6.4% 15.1% |
47.9% 20.5% |
64.49% 35.6% |
|
Education High school/GED Junior/community college Undergraduate college Graduate school Post-graduate (PhD, MD, etc.) |
6.8% 6.8% 5.5% 11.0% 1.4% |
2.7% 5.5% 15.1% 32.9% 12.3% |
9.6% 12.3% 20.5% 43.8% 13.7% |
|
Annual household income Less than $20,000 $20,000-$39,999 $40,000-$59,999 $60,000-$79,999 $80,000 or more |
5.8% 10.1% 2.9% 5.8% 4.3% |
4.3% 13.0% 18.8% 10.1% 24.6% |
10.1% 23.2% 21.7% 15.9% 29.0% |
|
Having any chronic diseases/health problems No Yes |
12.9% 17.1% |
20.0% 50.0% |
32.9% 67.1% |
Table 3: Patient Demographic Characteristics
|
Physician Background Information |
Mean |
|
Number of years being practicing medicine |
25.08 |
|
Primary practice in what U.S. state? 1= CA, 2= Other states |
1.07 |
|
practice type: 1= Private practice 2= Hospital-based 3= HMO-based 4= Academic/university-based 5= Other |
1.93 |
|
The number of patients visited per day (approximately) |
19.79 |
|
The percentage of the visited patients who are seniors aged 65 and over |
49.07 |
|
Use of the Internet to update the medical knowledge 0= No, 1= Yes |
0.92 |
|
Use of the Internet to know more about the needs and expectations of patients Values: 0= No, 1= Yes |
0.42 |
|
Usual use of the Internet to connect to the patients 0= No, 1= Yes |
0.14 |
|
Usual use of electronic mail (email) to interact with the patients 0= No, 1= Yes |
0.29 |
|
The physician’s office has any specific website 0= No, 1= Yes |
0.57 |
|
Characterization of the relationship with the senior patients 1= Good, 2= Fair, 3= Bad |
1.00 |
|
Believing that physicians’ relationship and communication with senior patients will affect their quality of life 1= Strongly disagree, 2= Disagree, 3= Neutral, 4= Agree, 5= Strongly agree |
4.29 |
|
Recommendation of any website to the senior patients to obtain health/medical information 0= No, 1= Yes |
0.46 |
|
Believing that senior patients should collaborate with doctors in decision making about their treatment 0= No, 1= Yes |
1.00 |
Table 4: Physician Background Information
|
· Family Medicine · Internal Medicine · Internal Medicine–Diabetes · Endocrinology, Diabetes & Metabolism · Hospice& Palliative Medicine · Rheumatology · Gastroenterology · Critical care · Urgent Care · Emergency Medicine · Ear, Nose, and Throat (ENT) · DDS Family and Cosmetic Dentistry · Gynecology · Alternative Medicine- Chiropractic |
Table 5: Physicians’ Specialty Area of Practice
|
Characteristics |
Mean |
|
Age (years) |
55.50 |
|
Gender 1= Female, 2= Male |
1.93 |
|
Ethnicity 1= Native American 2= African American/Black 3= Caucasian /White (non-Middle Eastern) 4= Latino/Hispanic 5= Asian /Pacific Islander 6= Middle Eastern 7= Other |
4.43 |
|
Born in the U.S.? 0= No, 1= Yes |
0.38 |
Table 6: Physician Demographic Information
2.9 Data analysis
2.9.1 Quantitative data analysis: The main analytical method in this study was quantitative. The quantitative data were analyzed using IBM SPSS. A 5-point Likert-type scale was used in the surveys. The quantitative data were analyzed using both descriptive and inferential statistics. In order to obtain sample demographics, the first step of data analysis was running a number of descriptive statistics, including central tendency measurement (such as mean, mode, median) and dispersion measurement (including range and standard deviation). Inferential statistics was used to test any relationships between variables. It included the t-test, ANOVA, ANCOVA, Pearson Chi-Square, exploratory factor analysis and reliability test (Cronbach's alpha).
2.9.2 Qualitative data analysis: Once an interview was completed, the obtained data was transcribed and analyzed. The related text was examined to find any patterns or codes, and to find any relationships and themes in the text.
After conducting qualitative and quantitative analyses separately, through a comparative data analysis, the obtained results were incorporated. The outline of data analysis is shown in Figure 1.
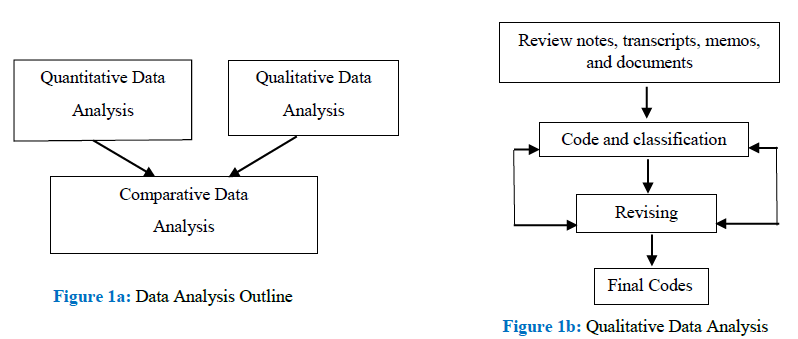
Figure 1: Data Analysis Outline
3. Results
To test the hypothesis, through the following steps, the perspectives of the two groups of patients were compared across all common items:
- Through running Chi-Square tests, the demographic characteristics of the two groups were compared, and the items that showed significant differences across the two groups were identified.
- Through conducting ANCOVA tests on all common parts of the survey, with considering the items identified in the previous step as the potential co-variates, the existence of any co-variate was investigated. The results showed that there were no co-variates.
- Then, through conducting exploratory factor analysis (EFA), reliability tests (Cronbach's alpha), and t-tests on all the common parts of the survey, the three following parts were identified to be significantly different across the two groups:
- “collaborative information exchange” (N=70, df=68, p=.033)
- “collaborative decision-making behavior by physicians” (N=69, df=67, p=.028)
- “the respondent’s belief about the desired role of a senior patient in a collaborative clinical decision-making process” [Pearson Correlation=0.356, N=65, Sig (2-tailed) = 0.004, Sig.(1-tailed) = 0.002].
These results indicated that those patient participants who use OLHI, 1) report more collaborative information exchange with their physicians; 2) find their physician’s behavior to be more collaborative; and 3) believe in a stronger authority for themselves as an active patient during visits. Due to the related findings in the existing literature, patient-physician collaborative information exchange, physicians’ collaborative behavior, and patients’ willingness toward playing an active role in the clinical CDM process are among the most important factors in a patient-physician CDM process [34,36,42,66,67]. According to these findings, the above results demonstrated that among senior patients, OLHI users perceive more control in the CDM process with physicians, in comparison to those seniors who do not use OLHI.
The aforementioned results provided a clear answer to the first research question. Pertaining to the second research question, the collected data and obtained results on the patient side were validated by the results obtained from physician survey. The physicians’ responses supported the results gained on the patient side. As mentioned earlier, the format and structure of the patient survey and physician survey were similar. This helped the investigator to find out the perspectives and experiences of physicians regarding senior patients and differences in behavior and expectations of the two groups of OLHI users and non-OLHI users.
The physician participants were specialized and practicing in 14 different medical specialties which are usually highly required by senior patients (Table 5). Moreover, as demonstrated in Table 4, about half of the number of patients visited by these physicians were seniors age 65 and over. The physicians’ perspectives suggest that when senior patients use online health information pertaining to their own health issues, they become more knowledgeable and empowered, capable of playing a more active role in clinical decision making and in the treatment process.
4. Discussion
Following, the findings of this study and their relevance with the existing body of literature will be discussed.
4.1 Senior patient-physician communication and interactions
- Seniors participating in this study stated that because of their age-related weaknesses and changes (both physical and mental), they have specific needs and expectations regarding the way their physicians interact with them. This finding is consistent with the existing literature, where several studies have highlighted these particular needs and expectations [68-74]. Furthermore, the current study demonstrated that among all, the physician rapport with patients is one of the most important needs of senior patients. Physician rapport was highly demanded by senior participants in this study, and it was even more required by those seniors who used OLHI.
- Unlike many studies indicating senior patients’ experience of ageism by physicians, the participants of this study stated that they had no experience of prejudices or ageism by their physicians. The reason for this might be related to the fact that the participants of the present study have been living in a specific area where the level of welfare and education is high, in comparison to many others in the country.
- Regarding the impact of the age of physicians on their communication and interactions with patients, the participants believed that the age of their physicians has had no impact on the way they communicate and interact with them.
- In general, all participants of this study had positive evaluation and experiences on the way their physicians interact with them, except for one thing that they were not satisfied about, enough: the amount of information their physicians provide them with regarding medications. In particular, they stated that they need more information about the potential side effects and interactions between different medications they are taking.
4.2 Senior patient-physician collaborative decision making
As stated before, patient-physician collaborative decision making (CDM) is an effective model of patient-physician relationship where the patient is involved in treatment decision making by physicians. The joint clinical decision made in a CDM process will be in line with the patient’s value and preferences [33,48,49].
The findings of the present study contradicted the findings of several studies that stated CDM is not desirable enough among senior patients [70,72,74]. In fact, none of the senior patients participating in this study (neither OLHI nor non-OLHI users) objected to the benefits or importance of clinical CDM. On the contrary, they all stated that they do want to be involved in their treatment process and in an effective patient-physician CDM process.
Another key finding of this study was related to the importance of patients’ understanding of the information provided by health care providers and its impact on the clinical CDM process. Several research studies have emphasized the important role of the patient’s understanding in a CDM process. For instance, reminding the importance of this understanding, [42] argued that there are many cases where patients leave their physicians’ offices without enough understanding of what their physicians has told them, or even with a misunderstanding about their illnesses or the treatment offered by their physicians. Furthermore, many studies have demonstrated that a high level of medical information is lost by patients after a doctor visit, ranging from 46% to 63% [75-80]. Regarding these issues, researchers argue that restating of the medical information by patients can be a very important solution to such issues. A study stated that patients who are requested to restate the important medical information before leaving the doctor’s office can retain and recall the information better than others [81]. Another study demonstrated that patients themselves would rather to restate the important medical information [42]. The results of the current study supported these findings. The participants of this study believed that because of cognitive and physical problems, senior patients are likely not to understand or misunderstand the medical information that their physicians provide them with. Because of this issue, they stated that any mechanisms that address this problem could be very helpful. They believed that one of such mechanisms would be restating the important medical information provided in a patient-physician interaction. Furthermore, some of them believed that not only doctors should ask senior patients for restating important information, but also patients should be allowed to ask their physicians to repeat some parts of the provided information that they are not sure if they have understood well. In other words, they stated that a bi-directional restatement of the important information will be needed.
4.3 Senior patients’ use of OLHI
As stated before, in recent years numerous research studies have investigated the use of online health information by patients. Many of these studies have indicated that using health information provided on the Internet can significantly improve the knowledge of information seekers, making a considerable enhancement in their well-being [55-57,82-87]. The studies demonstrate that the Internet has significantly empowered patients through providing them with health information and knowledge. Moreover, empowering patients has improved physician-patient communication [59]. In particular, the Internet has shown to be an important health-information resource for elderly adults [89].
The present study supported the aforementioned findings. It demonstrated that those senior patients who use OLHI before, after, or between visits perceive more control in the CDM process with their physicians in comparison to those who do not. In this argument, the major evidences were as follows:
- In comparison to the non-OLHI users, OLHI users perceived more powerful role and authority for themselves in a clinical CDM process;
- They reported collaborative exchange of more information with their physicians in a CDM process;
- They stated that their physician’s behaviors are more collaborative.
5. Conclusions
The rise of health care costs due to the aging of the population in the United States is becoming a national issue. Elderly patients usually need more health care resources and services than younger people. The existing literature illustrates that patient-physician collaborative decision making is an effective way to improve health outcomes. On the other hand, the Internet has proved to be a valuable source of health information, and can improve the knowledge of information seekers. Such knowledge can empower patients to interact more actively with their physicians and to participate in the decision making about their own health in a more effective way. The aim of this study was to examine senior patients’ perceptions regarding CDM and the impact of using health information obtained from the Internet on their perceived control in the CDM process with physicians. The results of the study revealed that those seniors who use OLHI before, after, or between visits perceive more control in the CDM process with physicians in comparison to the seniors who do not.
Acknowledgements
This paper is based on my doctoral dissertation research at Claremont Graduate University. I would like to thank my thesis committee members, Professors Tom Horan (Chair), Lorne Olfman, and Darleen Peterson for their valuable guidance and support.
Also, I would like to express my appreciation to several outside experts who shared with me their precious experiences, perspectives and guidelines from the standpoint of medical practice.
They are: Thomas M. Priselac, President and CEO of Cedars-Sinai Health System in Los Angeles, and a faculty member of UCLA School of Public Health; Robert E. Tranquada, M.D., an internist and an Emeritus Professor of USC; Daniel Z. Sands, MD, MPH, Co-Chairman, Co-Founder, and Past-President of Society for Participatory Medicine; Martin S. McLeod, DC, an experienced and popular doctor in Claremont and the nearby areas; and Timothy J. Dauwalder, DO, a Family Practitioner and Primary Care Physician, and Medical Director of VNA Hospice & Palliative Care of Southern California.
I should also express my deep appreciation to the management and administrative staff of the retirement and senior communities that provided me great support and facilities to access, invite, and interact with senior participants. These communities include Pilgrim Place (Claremont), Hillcrest (La Verne), Claremont Manor (Claremont), Mt San Antonio Gardens (Pomona), and Joslyn Center (Claremont).
Most importantly, I want to express my sincere appreciation to my research participants (both patients and physicians). Certainly, without them and the help they provided through sharing their valuable perspectives, experiences, and thoughts, this study would not have been completed.
Conflicts of interest:
No conflict of interest to disclose
References
- S. Senate. Special Committee on Aging. Aging America: Trends and Projections. Washington, D.C.: U.S. Government Printing Office (1991).
- Manton KG, Suzman R. Forecasting health and functioning in aging societies: Implications for health care and staffing needs, In Ory MG, Abeles RP, & Lipman PD. Aging, health and behavior. Newbury Park, CA: Sage (1992): 327-357.
- Research in ambulatory Patient Safety, 2000-2010: A 10-year review, Executive summary (2011): 8.
- Dovey SM, Meyers DS, Phillips RL, et al. A preliminary taxonomy of medical errors in family practice. BMJ Quality & Safety 11 (2002): 233-238.
- Elder NC, Meulen MV, Cassedy A. The identification of medical errors by family physicians during outpatient visits. The Annals of Family Medicine 2 (2004): 125-129.
- Fernald DH, Pace WD, Harris DM, et al. Event reporting to a primary care patient safety reporting system: a report from the ASIPS collaborative. The Annals of Family Medicine 2 (2004): 327-332.
- Kuzel AJ, Woolf SH, Gilchrist VJ, et al. Patient reports of preventable problems and harms in primary health care. The Annals of Family Medicine 2 (2004): 333-340.
- Makeham MA, County M, Kidd MR, et al. An international taxonomy for errors in general practice: a pilot study. Medical Journal of Australia 177 (2002): 68-72.
- Pace WD, Fernald DH, Harris DM, et al. Developing a taxonomy for coding ambulatory medical errors: a report from the ASIPS Collaborative. Advances in Patient Safety: from research to implementation 2 (2005): 63-73.
- Phillips RL, Dovey SM, Graham D, et al. Learning from different lenses: reports of medical errors in primary care by clinicians, staff, and patients: a project of the American Academy of Family Physicians National Research Network. Journal of Patient Safety 2 (2006): 140-146.
- Plews-Ogan ML, Nadkarni MM, Forren S, et al. Patient safety in the ambulatory setting: a clinician-based approach. Journal of General Internal Medicine 19 (2004): 719-725.
- Rubin G, George A, Chinn DJ, et al. Errors in general practice: development of an error classification and pilot study of a method for detecting errors. BMJ Quality & Safety 12 (2003): 443-447.
- West DR, Pace WD, Dickinson LM, et al. Relationship between patient harm and reported medical errors in primary care: a report from the ASIPS Collaborative. InAdvances in Patient Safety: New Directions and Alternative Approaches 1 (2008). Agency for Healthcare Research and Quality.
- Woolf SH, Kuzel AJ, Dovey SM, et al. A string of mistakes: the importance of cascade analysis in describing, counting, and preventing medical errors. The Annals of Family Medicine 2 (2004): 317-326.
- Metlay JP, Hennessy S, Localio AR, et al. Patient reported receipt of medication instructions for warfarin is associated with reduced risk of serious bleeding events. Journal of General Internal Medicine 23 (2008): 1589.
- Bertakis KD, Callahan EJ, Helms LJ, et al. Physician practice styles and patient outcomes: differences between family practice and general internal medicine. Medical Care (1998): 879-891.
- Blanck PD, Buck R, Rosenthal R. Nonverbal communication in the clinical context. University Park, PA: The Pennsylvania State University Press (1986).
- Buckman R. How to break bad news: A guide for health care professionals. Baltimore: The John Hopkins University Press (1992).
- Campbell JD, Neikirk HJ, Hosokawa MC. Development of a psychosocial concern index from videotaped interviews of nurse practitioners and family physicians. J Fam Pract 30 (1990): 321-326.
- Comstock LM, Hooper EM, Goodwin JM, et al. Physician behaviors that correlate with patient satisfaction. Academic Medicine 57 (1982): 105-112.
- Greene MG, Adelman RD. Psychosocial factors in older patients' medical encounters. Research on Aging 18 (1996): 84-102.
- Evans BJ, Kiellerup FD, Stanley RO, et al. A communication skills programme for increasing patients' satisfaction with general practice consultations. British Journal of Medical Psychology 60 (1987): 373-378.
- Hall JA, Dornan MC. Meta-analysis of satisfaction with medical care: description of research domain and analysis of overall satisfaction levels. Social Science & Medicine 27 (1988): 637-644.
- Irwin WG, McClelland R, Love AH. Communication skills training for medical students: an integrated approach. Medical Education 23 (1989): 387-394.
- Korsch BM, Gozzi EK, Francis V. Gaps in doctor-patient communication: I. Doctor-patient interaction and patient satisfaction. Pediatrics 42 (1968): 855-871.
- Korsch BM, Negrete VF. Doctor-patient communication. Scientific American 227 (1972): 66-75.
- Van Servellen GM. Communication skills for the health care professional: Concepts and techniques. Jones & Bartlett Learning (1997).
- Tasso K. Attributes of patient-physician relationships in a teaching hospital: An emergent model of interactions (Doctoral dissertation, University of Florida).
- Beckman HB, Markakis KM, Suchman AL, et al. The doctor-patient relationship and malpractice: lessons from plaintiff depositions. Archives of Internal Medicine 154 (1994): 1365-1370.
- Doyley RA. Elder Patient-Physician Communication: Satisfaction in the Medical Encounter in One Rural and One Suburban Family Practice Clinic (Doctoral dissertation, Fielding Graduate University) (2011).
- Lefevre FV, Waters TM, Budetti PP. A survey of physician training programs in risk management and communication skills for malpractice prevention. The Journal of Law, Medicine & Ethics 28 (2000): 258-266.
- Pichert JW, Hickson GB, Trotter TS. Malpractice and communication skills for difficult situations. Ambulatory Child Health 4 (1998): 213.
- Araki SS. Shared decision making in the treatment of endometriosis pain (2004).
- Braddock III CH, Edwards KA, Hasenberg NM, et al. Informed decision making in outpatient practice: time to get back to basics. JAMA 282 (1999): 2313-2320.
- Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean?(or it takes at least two to tango). Social Science & Medicine 44 (1997): 681-692.
- Elwyn G, Frosch D, Thomson R, et al. Shared decision making: a model for clinical practice. Journal of General Internal Medicine 27 (2012): 1361-1367.
- Epstein RM, Alper BS, Quill TE. Communicating evidence for participatory decision making. JAMA 291 (2004): 2359-2366.
- Gabe J, Olumide G, Bury M. ‘It takes three to tango’:: a framework for understanding patient partnership in paediatric clinics. Social Science & Medicine 59 (2004): 1071-1079.
- Elwyn G, Edwards A, Kinnersley P, et al. Shared decision-making: defining the competencies of involving patients in healthcare choices. Cardiff: Department of General Practice, University of Wales College of Medicine (1999).
- Heisler M, Bouknight RR, Hayward RA, et al. The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-Journal of General Internal Medicine 17 (2002): 243-252.
- Kelchner E. Voices not heard: A feminist look at the nature and meaning of communications between older persons and physicians. InGerontologist 42 (2002): 140-141.
- Kemp EC, Floyd MR, McCord-Duncan E, et al. Patients prefer the method of “tell back-collaborative inquiry” to assess understanding of medical information. The Journal of the American Board of Family Medicine 21 (2008): 24-30.
- Makoul G, Clayman ML. An integrative model of shared decision making in medical encounters. Patient Education and Counseling 60 (2006): 301-312.
- Murray E, Charles C, Gafni A. Shared decision-making in primary care: tailoring the Charles et al. model to fit the context of general practice. Patient Education and Counseling 62 (2006): 205-211.
- Schermer M. The different faces of autonomy: patient autonomy in ethical theory and hospital practice. Springer Science & Business Media (2002).
- Solomon RM. Cultivating shared decision making in the physician-patient relationship: Re-conceptualizing patient autonomy. (Ph.D., The University of Texas Medical Branch Graduate School of Biomedical Sciences). ProQuest Dissertations and Theses (2006).
- Stacey D, Legare F, Pouliot S, et al. Shared decision-making models to inform an interprofessional perspective on decision making: A theory analysis. Patient Education and Counseling 80 (2010): 164-172.
- Wennberg JE. On the status of the prostate disease assessment team. Health Services Research 25 (1990): 709-716.
- Wennberg JE, Mulley AG, Hanley D, et al. An assessment of prostatectomy for benign urinary-tract obstruction - geographic variations and the evaluation of medical-care outcomes. JAMA-Journal of the American Medical Association 259 (1988): 3027-3030.
- Llewellyn-Thomas HA, Holmes-Rovner M, O ’Connor AM, et al. The role of decision aids in shared decision making: mapping the future. Presented at: Quality Agenda in Health and Social Care Seminar Series, Oxford Brookes University. Oxford, UK (2000).
- Stewart M. Effective physician-patient communication and health outcomes - a review. Canadian Medical Association Journal 152 (1995): 1423-1433.
- Wallston KA, Wallston BS, Smith S, et al. Perceived control and health. Current Psychology 6 (1987): 5-25.
- Tennen H, Affleck G, Urrows S, et al. Perceiving control, construing benefits, and daily processes in rheumatoid arthritis. Canadian Journal of Behavioural Science/Revue Canadienne des Sciences du Comportement 24 (1992): 186.
- Affleck G, Tennen H, Pfeiffer C, et al. Appraisals of control and predictability in adapting to a chronic disease. Journal of Personality and Social Psychology 53 (1987): 273.
- Murray E, Lo B, Pollack L, et al. The impact of health information on the internet on health care and the physician-patient relationship: National US survey among 1.050 US physicians. Journal of Medical Internet Research 5 (2003): e17.
- Fox S. Older Americans and the Internet: Just 22% go online, but their enthusiasm for email and search may inspire their peers to take the leap. Pew Internet & American Life Project (2004).
- Kaiser Family Foundation. E-health and elderly: how seniors use the internet for health- survey (2005). Accessed from : http://kff.org/medicare/poll-finding/e-health-and-the-elderly-how-seniors/ (accessed Aug. 25, 2013).
- Akerkar SM, Bichile LS. Health information on the internet: Patient empowerment or patient deceit?. Indian Journal of Medical Sciences 58 (2004): 321-326.
- Dumitru RC, Buerkle T, Potapov S, et al. Use and perception of internet for health related purposes in Germany: Results of a national survey. International Journal of Public Health 52 (2007): 275-285.
- Hussain N, Agyeman A, Das Carlo M. Access, attitudes, and concerns of physicians and patients toward e-mail use in health-related communication. Texas Medicine 100 (2004): 50.
- Campbell R, Wabby J. The Elderly and the Internet: A Case Study. The Internet Journal of Health 3 (2003).
- Fox S, Rainie L. The online health care revolution: how the Web helps Americans take better care of themselves. Washington, D.C.: The Pew Internet & American Life Project (2000). Retrieved from: http://www.pewinternet.org/~/media//Files/Questionnaire/Old/PIP_Health_Questionnaire. pdf (2013).
- Campbell D, Fiske D. Convergent and discriminant validation by the multitrait-multimethod matrix. Psychological Bulletin 56 (1959): 81–105.
- Patton MQ. Qualitative evaluation and research methods. SAGE Publications, inc (1990).
- Biedrzycki BA. Decision making and outcomes in cancer clinical trial. (Ph.D., John Hopkins University). ProQuest Dissertations and Theses (2010).
- Hewson MG, Budev M. Cultural consults for caring trans-culturally. Medical Encounter 15 (2000): 3-5.
- Weiss B. Health literacy: a manual for clinicians. Chicago (IL): American Medical Association Foundation (2003).
- Ende J, Kazis L, Ash A, et al. Measuring patients desire for autonomy - decision-making and information-seeking preferences among medical patients. Journal of General Internal Medicine 4 (1989): 23-30.
- Kaplan SH, Gandek B, Greenfield S. Patient and visit characteristics related to physicians participatory decision-making style results from the medical outcomes study. Medical Care 33 (1995): 1176-1187.
- Kaplan SH, Greenfield S, Ware JE. Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Medical Care 27 (1989): S110-S127.
- McCormick WC, Inui TS, Roter DL. Interventions in physician elderly patient interactions. Research on Aging 18 (1996): 103-136.
- Stewart M, Meredith L, Brown JB, et al. The influence of older patient-physician communication on health and health-related outcomes. Clinics in Geriatric Medicine 16 (2000): 25-36.
- Thompson SC, Pitts JS, Schwankovsky L. Preferences for involvement in medical decision-making - situational and demographic influences. Patient Education and Counseling 22 (1993): 133-140.
- Roter DL. Patient question asking in physician-patient interaction. Health Psychology 3 (1984): 395-409.
- Anderson JL. Patients' recall of information and its relation to the nature of the consultation. Research in Psychology and Medicine 2 (1979): 238-246.
- Joyce CR, Caple G, Mason M, et al. Quantitative study of doctor-patient communication. Quarterly Journal of Medicine 38 (1969): 183-194.
- Ley P. Memory for medical information. British Journal of Social and Clinical Psychology 18 (1979): 245-255.
- Ley P. Improving clinical communication: Effects of altering doctor-patient behavior. InResearch in Psychology and Medicine. Academic Press New York (1979).
- Ley P. Patients’ understanding and recall in clinical communication failure. Doctor-patient communication. London: Academic Press, Inc (1983): 89-107.
- Rost K, Roter D. Predictors of recall of medication regimens and recommendations for life-style change in elderly patients. Gerontologist 27 (1987): 510-515.
- Bertakis KD. The communication of information from physician to patient: a method for increasing patient retention and satisfaction. The Journal of Family Practice 5 (1977): 217-222.
- Cline RJW, Haynes KM. Consumer health information seeking on the internet: The state of the art. Health Education Research 16 (2001): 671-692.
- Gerber BS, Eiser AR. The patient-physician relationship in the internet age: Future prospects and the research agenda. Journal of Medical Internet Research 3 (2001).
- Jadad AR, Sigouin C, Cocking L, et al. Internet use among physicians, nurses, and their patients. JAMA-Journal of the American Medical Association 286 (2001): 1451-1452.
- Jee YG. A Qualitative Case Study on the Usability of internet Usage for the Aged. Unpublished Master Thesis, Sookmyung Women’s University, Seoul (2003).
- Morrell RW, Mayhorn CB, Bennett J. A survey of world wide web use in middle-aged and older adults. Human Factors 42 (2000): 175-182.
- Song TM, Park EJ, Lim EJ. The survey of demand for health information on the internet. Journal of Korean Society of Medical Informatics 8 (2002): 17-24.
- Shantiaei M. The Impact of the Access and Use of Online Health Information on Senior Patients' Perceived Control in the Collaborative Decision Making Process with Physicians (Doctoral dissertation, The Claremont Graduate University) (2015).
- Chung J, Gassert CA, Kim HS. Online health information use by participants in selected senior centres in Korea: Current status of internet access and health information use by Korean older adults. International Journal of Older People Nursing 6 (2011): 261-271.
