Hiatal Hernia Presenting with Dyspnea
Article Information
Suat Konuk MD*, Tuncer Tug MD, Manolya Ballar MD, Ceyda Kayabasi MD
Faculty of Medicine Pulmonology Department, Abant Izzet Baysal University, Bolu, Turkey
*Corresponding Author: Dr. Suat Konuk, Faculty of Medicine Pulmonology Department, Abant Izzet Baysal University, Bolu, Turkey
Received: 19 June 2019; Accepted: 08 July 2019; Published: 16 September 2019
Citation: Suat Konuk MD, Tuncer Tuğ MD, Manolya Ballar MD, Ceyda Kayabaşi MD. Hiatal Hernia Presenting with Dyspnea. Archives of Clinical and Medical Case Reports 3 (2019): 274-277.
View / Download Pdf Share at FacebookAbstract
Hiatal hernia is defined as the escape of abdominal organs to the thorax due to the anatomical weakness of the esophageal crus of the diaphragm. Hiatal hernia is often asymptomatic and causes gastroesophageal reflux when it is symptomatic. Patients with large hiatal hernias may have significant dyspnea and exercise disorder. The cause of dyspnea can be attributed mainly to large hernias in the thoracic cavity that cause left atrial compression, increase pulmonary venous pressure, produce interstitial edema and reduce pulmonary compliance. Here we present a 79-year-old female patient with hiatal hernia whose primary symptom is dyspnea. In the differential diagnosis of persistent dyspnea without a known cause, large hiatal hernias should be considered as a rare intraabdominal reason.
Keywords
Hernia; Dyspnea; Esophageal; Thoracic
Hernia articles Hernia Research articles Hernia review articles Hernia PubMed articles Hernia PubMed Central articles Hernia 2023 articles Hernia 2024 articles Hernia Scopus articles Hernia impact factor journals Hernia Scopus journals Hernia PubMed journals Hernia medical journals Hernia free journals Hernia best journals Hernia top journals Hernia free medical journals Hernia famous journals Hernia Google Scholar indexed journals Dyspnea articles Dyspnea Research articles Dyspnea review articles Dyspnea PubMed articles Dyspnea PubMed Central articles Dyspnea 2023 articles Dyspnea 2024 articles Dyspnea Scopus articles Dyspnea impact factor journals Dyspnea Scopus journals Dyspnea PubMed journals Dyspnea medical journals Dyspnea free journals Dyspnea best journals Dyspnea top journals Dyspnea free medical journals Dyspnea famous journals Dyspnea Google Scholar indexed journals Esophageal articles Esophageal Research articles Esophageal review articles Esophageal PubMed articles Esophageal PubMed Central articles Esophageal 2023 articles Esophageal 2024 articles Esophageal Scopus articles Esophageal impact factor journals Esophageal Scopus journals Esophageal PubMed journals Esophageal medical journals Esophageal free journals Esophageal best journals Esophageal top journals Esophageal free medical journals Esophageal famous journals Esophageal Google Scholar indexed journals health articles health Research articles health review articles health PubMed articles health PubMed Central articles health 2023 articles health 2024 articles health Scopus articles health impact factor journals health Scopus journals health PubMed journals health medical journals health free journals health best journals health top journals health free medical journals health famous journals health Google Scholar indexed journals Thoracic articles Thoracic Research articles Thoracic review articles Thoracic PubMed articles Thoracic PubMed Central articles Thoracic 2023 articles Thoracic 2024 articles Thoracic Scopus articles Thoracic impact factor journals Thoracic Scopus journals Thoracic PubMed journals Thoracic medical journals Thoracic free journals Thoracic best journals Thoracic top journals Thoracic free medical journals Thoracic famous journals Thoracic Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals psychiatric disorders articles psychiatric disorders Research articles psychiatric disorders review articles psychiatric disorders PubMed articles psychiatric disorders PubMed Central articles psychiatric disorders 2023 articles psychiatric disorders 2024 articles psychiatric disorders Scopus articles psychiatric disorders impact factor journals psychiatric disorders Scopus journals psychiatric disorders PubMed journals psychiatric disorders medical journals psychiatric disorders free journals psychiatric disorders best journals psychiatric disorders top journals psychiatric disorders free medical journals psychiatric disorders famous journals psychiatric disorders Google Scholar indexed journals patient articles patient Research articles patient review articles patient PubMed articles patient PubMed Central articles patient 2023 articles patient 2024 articles patient Scopus articles patient impact factor journals patient Scopus journals patient PubMed journals patient medical journals patient free journals patient best journals patient top journals patient free medical journals patient famous journals patient Google Scholar indexed journals surgical articles surgical Research articles surgical review articles surgical PubMed articles surgical PubMed Central articles surgical 2023 articles surgical 2024 articles surgical Scopus articles surgical impact factor journals surgical Scopus journals surgical PubMed journals surgical medical journals surgical free journals surgical best journals surgical top journals surgical free medical journals surgical famous journals surgical Google Scholar indexed journals Spinal adjustment articles Spinal adjustment Research articles Spinal adjustment review articles Spinal adjustment PubMed articles Spinal adjustment PubMed Central articles Spinal adjustment 2023 articles Spinal adjustment 2024 articles Spinal adjustment Scopus articles Spinal adjustment impact factor journals Spinal adjustment Scopus journals Spinal adjustment PubMed journals Spinal adjustment medical journals Spinal adjustment free journals Spinal adjustment best journals Spinal adjustment top journals Spinal adjustment free medical journals Spinal adjustment famous journals Spinal adjustment Google Scholar indexed journals
Article Details
1. Introduction
Dyspnea can be a life-threatening symptom with many causes. Cardiac and pulmonary causes are the most common causes. Less common causes include anxiety, hyperventilation syndrome, metabolic conditions (such as acidosis and anemia) and psychiatric disorders such as neuromuscular disorder. Hiatal hernia is an unusual cause of dyspnea. Here we tried to describe a case of hiatal hernia presenting with dyspnea.
2. Case Report
A 79-year-old female patient with known HT, COPD and hypothyroidism was admitted to the outpatient clinic of chest diseases due to dyspnea. The patient complained of dyspnea persisting during rest for 3-4 years and reported that she could not do her daily work. The patient has been receiving oxygen therapy for an average of 15 hours per day for 5 years. The patient recently has been suffering from increased drowsiness. The patient was hospitalized in January 2019 due to the high risk of pulmonary embolism in ventilation perfusion scintigraphy performed to investigate the etiology of pulmonary hypertension 2 months before routine admission to the outpatient clinic. Close vital monitoring and anticoagulant treatment was started. BP: 110/60, P: 62, F: 36.2, SPO2: 93(3 lt/mn O2) was observed. Respiratory sounds were reduced. Pretibial edema was + / +. Laboratory tests revealed tsh: 0.56 t3: <1, t4: 0.68, and that the patient did not use her drug correctly. The dose of euthyrox was increased and the patient started taking it alone in the morning. Wbc: 5180, neu: 62% hb: 10.2, plt: 157 ast: 214 sub: 359 total bilirubin: 1.98 urea: 259 cre: 2.82 na: 145 k: 5.1 nr: 1.31. When the arterial blood gas was seen as ph: 7.30 pco2: 83 hco3: 33 so2: 61 be: 14.4, the patient underwent bpap 12/6. After bpap the results changed to ph: 7.35 pco2: 72.3 hco3: 35.4 and 13.8 so2: 96.8. Abdominal usg: dilatation of hepatic veins (secondary to heart failure?). Lasix 3*1 was started due to acute renal failure, after urine output lasix was reduced to 1*1 and renal function tests stabilized. Hiatal hernia was suspected at the thorax x-ray and thorax CT was requested. Thorax CT: Pulmonary truncus was measured as 32 mm, right main pulmonary artery as 30 mm, left main pulmonary artery as 26 mm and was larger than normal. Other mediastinal main vascular structures were of normal caliber.
Secondary to the compression of the hiatal hernia, atelectatic parenchyma with air bronchograms were observed in the parenchyma adjacent to the hernia in the the superior segment of the lower lobe of the right lung. In the evaluated abdominal sections, the whole stomach, transverse colon, splenic flexura, pancreatic trunk distal - tail section and abdominal fat planes were herniated into the thoracic cavity and organoaxial volvulus was observed in the stomach. No other pathological findings were detected in this upper abdominal section. The patient was consulted to general surgery, outpatient control and operation was planned. The patient was referred to general surgery with a bpap report.

Figure 1: Thorax x-ray.
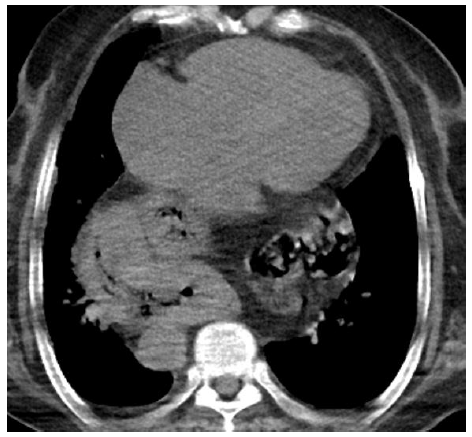
Figure 2: Thorax computerized tomography.
3. Discussion
Hiatal hernia is defined as the escape of abdominal organs to the thorax due to the anatomical weakness of the esophageal crus of the diaphragm. There are 4 types: Type I (sliding hernia; gastroesophageal junction and proximal cardia are intrathoracically in the posterior mediastinum), Type 2 (gastroesophageal compound and cardia retaining their normal position under the diaphragm, while gastric fundus and/or a portion of the large curvature proceeds through the hiatus towards the pleural cavity forming a hernia sac) Type 3 (Type 1 and 2 at the same time; although the gastroesophageal compound and the cardia are intrathoracic, the fundus and large curvature remain superior to the cardia), Type 4 (other abdominal abdominal organs other than the stomach and esophagus in the hernia sac). They are more common in women than in men. Hiatal hernia is often asymptomatic. It often causes gastroesophageal reflux when it is symptomatic. Sliding hernias are seen more frequently [1]. Although the cause of the development of hiatal hernia is not known, its incidence increases with age [2]. It is accepted that relaxation of the diaphragmatic crus caused by the aging process is the reason hiatal hernia is more common and more in the elderly population [3].
Dyspnea is often not the primary symptom of a hiatal hernia [4]. Patients with large hiatal hernias may have significant dyspnea and exercise disorder. The cause of dyspnea can be attributed mainly to large hernias in the thoracic cavity that cause left atrial compression, increase pulmonary venous pressure, produce interstitial edema and reduce pulmonary compliance [5, 6]. In our case, dyspnea was attributed to pulmonary embolism, chronic obstructive pulmonary disease and giant hiatal hernia.
Type 1 hiatal hernia does not require treatment unless symptoms are present. However, if gastroesophageal reflux is present, drug treatment is applied. If medication fails, surgical intervention is required. Type 2,3,4 hiatal hernias are indicative of surgery when detected, even if they are asymptomatic, because complications can be fatal and the disease progresses without surgical treatment.
In conclusion, large hiatal hernias should be considered as a rare intraabdominal cause of dyspnea in differential diagnosis.
References
- Maziak DE, Todd TRJ, Pearson FG et al. Massive hiatus hernia: evaluation and surgical management,” Journal of Thoracic and Cardiovascular Surgery 115 (1998): 53-62.
- Yoshimura M, Nagahara A, Ohtaka K et al. Presence of vertebral fractures is highly associated with hiatal hernia and reflux esophagitis in Japanese elderly people. Internal Medicine 47 (2008): 1451-1455.
- Cole TJ, Turner MA. Manifestations of gastrointestinal disease on chest radiographs. Radiographics 13 (1993): 1013-1034.
- Marwick TH. When the stomach rules the heart: dyspnea as aneglected complication of a large hiatal hernia. J Am CollCardiol 58 (2011): 1635e6.
- Naoum C, Falk GL, Ng AC, et al. Left atrial compression and the mechanism of exercise impairment in patients with a large hiatal hernia. J Am Coll Cardiol 58 (2011): 1624e34.
- Van der Leest K, Bogaard J, Rudolphus A, et al. Paraesophageal hiatal hernia-inducedd yspnea. Respiration 78 (2009): 105.
