Hepatic Angiosarcoma: A Rare Cause of Acute Liver Failure Case Report and Review of the Literature
Article Information
Yasmine Laraqui Housseini*, Raissouni Khouloud, Derqaoui Sabrine, Ahmed Jahid, Zakiya Bernoussi, Kaoutar Znati
Department of Pathology, Ibn Sina University Hospital Center, Rabat, Morocco
*Corresponding Author: Yasmine Laraqui Housseini, Department of Pathology, Ibn Sina University Hospital Center, Rabat, Morocco.
Received: 22 October 2019; Accepted: 07 November 2019 Published: 15 November 2019
Citation: Yasmine Laraqui Housseini, Raissouni Khouloud, Derqaoui Sabrine, Ahmed Jahid, Zakiya Bernoussi, Kaoutar Znati. Hepatic Angiosarcoma: A Rare Cause of Acute Liver Failure Case Report and Review of the Literature. Journal of Cancer Science and Clinical Therapeutics 3 (2019): 312-317.
View / Download Pdf Share at FacebookAbstract
Hepatic Angiosarcoma is a rare, high grade, aggressive mesenchymal tumor. It is the most common malignant mesenchymal tumor of the liver, but is nonetheless rare, accounting for 2% of all primary liver malignancies, with a male predominance. Some hepatic Angiosarcoma were associated with exposure to anabolic steroids, radiation, thorium dioxide, arsenic, vinyl chloride and use of oral contraceptives, but most cases are now considered idiopathic. Given that hepatic angiosarcoma clinical, laboratory and radiologic presentation are non specific, radical resection of the tumor is being currently the best treatment option. Its diagnosis is difficult and often delayed, and requires histopathological examination. The prognosis is extremely poor with a high mortality rate and few therapeutic options. We report a case of a woman who presented with acute liver failure, which is a very unusual presentation of HAS, diagnosed with hepatic angiosarcoma through a liver biopsy. She had a rapidly worsening clinical course and died within four months of diagnosis.
Keywords
<p>Hepatic; Angiosarcoma; Liver Failure; Rare; Biopsy; Histopathological; Non Specific</p>
Hepatic Articles, Angiosarcoma Articles, Liver Failure Articles, Rare Articles, Biopsy Articles, Histopathological Articles, Non Specific Articles
Hepatic articles Hepatic Research articles Hepatic review articles Hepatic PubMed articles Hepatic PubMed Central articles Hepatic 2023 articles Hepatic 2024 articles Hepatic Scopus articles Hepatic impact factor journals Hepatic Scopus journals Hepatic PubMed journals Hepatic medical journals Hepatic free journals Hepatic best journals Hepatic top journals Hepatic free medical journals Hepatic famous journals Hepatic Google Scholar indexed journals Angiosarcoma articles Angiosarcoma Research articles Angiosarcoma review articles Angiosarcoma PubMed articles Angiosarcoma PubMed Central articles Angiosarcoma 2023 articles Angiosarcoma 2024 articles Angiosarcoma Scopus articles Angiosarcoma impact factor journals Angiosarcoma Scopus journals Angiosarcoma PubMed journals Angiosarcoma medical journals Angiosarcoma free journals Angiosarcoma best journals Angiosarcoma top journals Angiosarcoma free medical journals Angiosarcoma famous journals Angiosarcoma Google Scholar indexed journals Liver Failure articles Liver Failure Research articles Liver Failure review articles Liver Failure PubMed articles Liver Failure PubMed Central articles Liver Failure 2023 articles Liver Failure 2024 articles Liver Failure Scopus articles Liver Failure impact factor journals Liver Failure Scopus journals Liver Failure PubMed journals Liver Failure medical journals Liver Failure free journals Liver Failure best journals Liver Failure top journals Liver Failure free medical journals Liver Failure famous journals Liver Failure Google Scholar indexed journals Rare articles Rare Research articles Rare review articles Rare PubMed articles Rare PubMed Central articles Rare 2023 articles Rare 2024 articles Rare Scopus articles Rare impact factor journals Rare Scopus journals Rare PubMed journals Rare medical journals Rare free journals Rare best journals Rare top journals Rare free medical journals Rare famous journals Rare Google Scholar indexed journals Biopsy articles Biopsy Research articles Biopsy review articles Biopsy PubMed articles Biopsy PubMed Central articles Biopsy 2023 articles Biopsy 2024 articles Biopsy Scopus articles Biopsy impact factor journals Biopsy Scopus journals Biopsy PubMed journals Biopsy medical journals Biopsy free journals Biopsy best journals Biopsy top journals Biopsy free medical journals Biopsy famous journals Biopsy Google Scholar indexed journals Histopathological articles Histopathological Research articles Histopathological review articles Histopathological PubMed articles Histopathological PubMed Central articles Histopathological 2023 articles Histopathological 2024 articles Histopathological Scopus articles Histopathological impact factor journals Histopathological Scopus journals Histopathological PubMed journals Histopathological medical journals Histopathological free journals Histopathological best journals Histopathological top journals Histopathological free medical journals Histopathological famous journals Histopathological Google Scholar indexed journals Non Specific articles Non Specific Research articles Non Specific review articles Non Specific PubMed articles Non Specific PubMed Central articles Non Specific 2023 articles Non Specific 2024 articles Non Specific Scopus articles Non Specific impact factor journals Non Specific Scopus journals Non Specific PubMed journals Non Specific medical journals Non Specific free journals Non Specific best journals Non Specific top journals Non Specific free medical journals Non Specific famous journals Non Specific Google Scholar indexed journals mesenchymal tumor articles mesenchymal tumor Research articles mesenchymal tumor review articles mesenchymal tumor PubMed articles mesenchymal tumor PubMed Central articles mesenchymal tumor 2023 articles mesenchymal tumor 2024 articles mesenchymal tumor Scopus articles mesenchymal tumor impact factor journals mesenchymal tumor Scopus journals mesenchymal tumor PubMed journals mesenchymal tumor medical journals mesenchymal tumor free journals mesenchymal tumor best journals mesenchymal tumor top journals mesenchymal tumor free medical journals mesenchymal tumor famous journals mesenchymal tumor Google Scholar indexed journals etiology articles etiology Research articles etiology review articles etiology PubMed articles etiology PubMed Central articles etiology 2023 articles etiology 2024 articles etiology Scopus articles etiology impact factor journals etiology Scopus journals etiology PubMed journals etiology medical journals etiology free journals etiology best journals etiology top journals etiology free medical journals etiology famous journals etiology Google Scholar indexed journals carcinogens articles carcinogens Research articles carcinogens review articles carcinogens PubMed articles carcinogens PubMed Central articles carcinogens 2023 articles carcinogens 2024 articles carcinogens Scopus articles carcinogens impact factor journals carcinogens Scopus journals carcinogens PubMed journals carcinogens medical journals carcinogens free journals carcinogens best journals carcinogens top journals carcinogens free medical journals carcinogens famous journals carcinogens Google Scholar indexed journals
Article Details
Abbreviations:
Has-Hepatic Angiosarcoma1. Background
HAS is a rare and aggressive mesenchymal tumor associated with rapid liver failure and high mortality rate. It was associated with environmental exposure to carcinogens but etiology still unknown in the majority of the cases. Given the non specific symptoms and variable imaging findings, diagnosis is difficult and often delayed, requiring careful Histopathological examination. It carries a grim prognosis even with treatment, including surgical resection. We report a case of primary Angiosarcoma of the liver, which presented with acute liver failure, which is an uncommon presentation of a primary liver tumor. This case highlights the need to consider the diagnosis of hepatic Angiosarcoma as a differential in front of acute liver failure presentation without any clear etiology.
2. Case Report
A 58-year-old caucasian woman was presented at the hospital with asthenia, anorexia and jaundice. She didn’t report any other symptom, particularly digestive one. She had no personality, no history of alcohol intake or exposure to any carcinogen. She denied using any herbal or hepatotoxic medications ant there are no family history of liver disease. The physical examination on admission showed an ascites with jaundice without encephalopathy or focal neurological findings. Biologically, the liver function on admission revealed a hyperbilirubinemia of 280μmol/L(normal: 4–20 μmol/L), elevated alkaline phosphatase at 220 U/L(normal: 35–110U/L), gamma-glutamyltransferase of 45U/L (normal: 5–50U/L), alanine transaminase of 43U/L(normal: 5–40U/L). Her alpha fetoprotein was normal of 3 μg/L (normal: 0.5–12 μg/L), albumin rate was 29g/L(normal 34-45 g/L) and she had an international normalized ratio (INR) of 1.9. Her hepatitis, Epstein-Barr virus, cytomegalovirus, HIV, varicella zoster virus (VZV), syphilis, cryptococcal and herpes simplex serology were all negative.
An abdominal CT scan was made and demonstrated a dysmorphic liver with suspicion of cirrhosis. A gastroscopy was performed which revealed oesophageal varices, which were banded, and portal hypertensive gastropathy. The patient subsequently underwent an ultrasound-guided percutaneous core biopsy of the liver with six full length cores obtained. Microscopically, the liver core biopsies showed abnormal sinusoidal architecture proliferation of neoplastic cells around dilated sinusoids with cytological atypia, with conservation of the adjacent hepatic parenchyma. Tumor cells had atypical nuclei, elongated and hyperchromatic, with numerous mitotic figures. In the immunohistochemical study, tumor cells expressed strongly and diffusely the vascular endothelial markers (ERG, CD31) and proliferation index with Ki67 was increased (60%), and was negative for CK7 and CK20.The histopathological examination of the liver biopsy has thus confirmed the diagnosis of a hepatic Angiosarcoma with sinusoidal growth pattern. She had a rapidly worsening clinical course and died within four months of diagnosis.
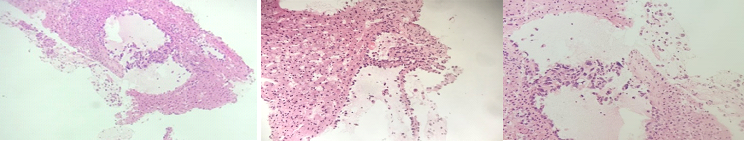
Figure 1: Liver biopsy showing tumoral proliferation around dilated sinusoids leaving normal hepatic cells.
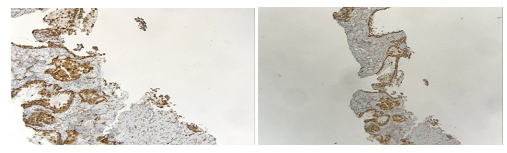
Figure 2: Tumor cells are strongly immunoreactive for the vascular endothelial marker CD34.
3. Discussion
Hepatic angiosarcoma is a rare, non cirrhotic, agressive tumour of endothelial cell origin that line the walls of blood vessels. Its accounting for 2% of primary liver malignancy and it remains the third most common primary hepatic malignant tumour and fifth most common sites for angiosarcomas [1]. It’s a late adulthood disease, which begin generally at the sixth or seventh decade of life, and with a male predominance (Sexe ratio 4:1). Although hepatic angiosarcoma was associated with the use of oral contraceptives, exposure to environmental carcinogens, including radiation, thorium dioxide, arsenic or vinyl chloride, most cases arise without any causative associated risk factors [2]. Clinically, the patient can be asymptomatic or present symptoms like diffuse abdominal pain, abdominal distension, asthenia, anorexia and weight loss that remains non specific. Physical signs may include ascites, hepatomegaly and jaundice [3]. Spontaneous hemoperitoneum, due to the rupture of blood vessels or after instrumentation happens in 17% to 27% of the cases, is highly suspicious for hepatic Angiosarcoma and its associated with a high morbidity and mortality [1]. Usually, hepatic function is maintained until late or metastatic stages of the disease. The most common finding is the increase of the alkaline phosphatase levels. The sequestration of platelets and local intravascular destruction of clotting factors both contribuate to the pathophysiologic process of disseminated intravascular coagulopathy. Some cases of microangiopathic hemolytic anemia, thrombocytemia and hyperbilirubinemia are reported. Otherwise, no tumoral markers have been associated [3, 4]. Acute liver failure is a very unusual presentation of hepatic angiosarcoma [5]. It is defined as liver disease that results in encephalopathy and coagulopathy in a patient with no prior evidence of liver disease. It is often caused by drug toxicity and hepatitis. In contrast, it develops rarely as a consequence of infiltrative metastases or primary liver tumour [6]. In HAS, the mechanism of liver failure is multifactorial. It is suggested that it be related to ischemia of the hepatic parenchyma, tumour thrombi due to portal vein occlusion and non occlusive infarction of liver due to sepsis or cardiac shock and the replacement of the hepatocytes by malignant cells that lead to secondary necrosis [7, 8]. From a radiologic point of view, currently there are no known pathognomonic features for HAS and it is difficult to distinguish HAS from other primary liver tumors due to the various morphologic appearances [3, 9]. CT and MRI both participate in the diagnosis by showing the hypervascular and heterogeneous character of HAS [10-12].
The final diagnosis is made with a histologic examination. However, the vascular nature of the tumor makes it difficult to perform the biopsy, exposing to increased risk of hemorrhage [13]. Otherwise, the risk of false- negative biopsies remain also a problem due to a high frequency of haemorragic and necrotic foci within the tumour [14]. Microscopically, it is characterized by four patterns: multiples nodules, large dominant mass, mixed pattern of dominant mass with nodules, and, rarely, a diffusely infiltrating micronodular tumor. Lesions can vary in color, from pale yellow-white to red-brown; they are general poorly limited, of spongy consistency, of herogenic aspect with alternation of haemorrhagic, necrotic foci and intraparenchymal cystic spaces filled with thrombotic contents [15]. Microscopically it is characterized by the proliferation of neoplastic cells around preformed vascular channels such as dilated sinusoids, as in our case, as well as hepatic terminal venules and portal vein branches [11]. The growth of the sinusoids is related to their dilation and atrophy of the hepatic cells. It is composed of malignant atypical epithelioid, spindle and pleomorphic cells with small vascular spaces [3]. Tumour cells contain atypical hyperchromic and elongated nuclei with frequent mitotic figures. sometimes, areas of fibrosis and haemosiderin deposits can be observed in the solid areas. Areas of hemorrhage, infarction, calcifications and necrosis can be seen as well [16]. Even if there are some sensitive immune-histological markers for the HAS diagnostic, no marker is specific. That’s why they should only be used in addition with the other investigations to assist diagnosis. Tumor cells frequently express the vascular markers like CD31, CD34, erythroblast transformation-specific-related gene (ERG), Factor VIII, and vascular endothelial growth factor receptor-3 (VEGFR-3) (1). Other immunohistochemical markers may be positive including CD10, CD117, cytokeratin, FLI-1,6 D2-40, and Ki-67 [17, 18]. Make a differential diagnosis with benign tumor is important to do. In fact, tumor cells may also form their own disorganized anastomotic vascular channels, shape solid nodules or nests, or form cavernous spaces by losing adjacent hepatocytes, which may overlap the diagnosis with cavernous haemangiomas. Adjacent hepatocytes may be atrophic or hyperplastic. Atrophic hepatocytes and sinusoidal dilation can sometimes be confused with peliosis hepatitis [15]. Due to the rarity and rapidly worsening course of the tumor, there are no formal guidelines for the treatment of hepatic Angiosarcoma [19]. Currently, surgical radical resection RO is the only curative treatment, but curative surgeries are difficult to perform. In the frequent cases of a multifocal or metastatic disease, adjuvant chemotherapy associated with surgical resection offers better chances of healing though no chemotherapy regimen has been established for its treatment. Chemotherapy can be also palliative and is indicated for patients with HAS that cannot be resected. In this case, the recommendation includes 5fluorouracil-carboplatin with doxorubicin or ifosfamide. Unfortunately, radiation therapy has had limited use, as it appears the cancer is radioresistant. Liver transplantation is an absolute contraindication for the management of HAS because of the high recurrence and low survival rates post transplant [9], with a median survival of 06 months with only 3% of patients living more than 2years, even with treatment including surgical resection [1, 15]. This poor prognosis is attributable to the rapid progression of the disease, its high recurrence rate, rapid metastatic invasion to other organs, and its resistance to radiotherapy. Metastases are common at the time of presentation, the lung (38%), spleen 18%), or bone 18%) being the most frequent secondary lesion sites. However, better prognosis is seen in patients that present with a single tumor mass, small tumor size, lack of metastases, low grade lesion, and negative surgical resection margins. Hepatic failure is the cause of death in approximately 50% of patients and haemoperitoneum in 25% of patients, followed by metastatic disease, infection and rarely, renal failure and congestive heart failure [1].
4. Conclusion
HAS is an infrequent tumor in female patients, and acute liver failure is a very rare presentation of this disease. This unusual combination of clinical characteristics was part of the case we reported. Our patient had a progressively worsening clinical course and died within four months of diagnosis. This demonstrates the rapid progression, poor prognosis, and the need to find a therapy that improves survival. In the absence of a clear etiology for acute liver failure, primary liver tumor must be considered in the differential diagnosis and a biopsy should be arranged to reach definitive diagnosis. A diagnosis made soon, will make a difference in the treatment options, outcome and prognosis of these patients.
References
- Averbukh LD, Mavilia MG, Einstein MM. Hepatic Angiosarcoma: A Challenging Diagnosis. Cureus 10 (2018): e3283
- Cioffi-Pretti JL, Kalof AN, Ebert G, et al. Hepatic angiosarcoma five years following spontaneous intraperitoneal bleed of a hepatic mass. Rare Tumors 1 (2009): e33.
- Molina E, Hernandez A. Clinical manifestations of primary hepatic angiosarcoma. Dig Dis Sci. avr 48 (2003): 677-682.
- Koyama T, Fletcher JG, Johnson CD, et al. Primary Hepatic Angiosarcoma: Findings at CT and MR Imaging. Radiology 222 (2002): 667-673.
- Lopez R, Castro-Villabón D, Álvarez J, et al. Hepatic angiosarcoma presenting as acute liver failure in young adults. Report of two cases and review of literature. Case Rep Clin Med 2 (2013): 439-444.
- Singh G, Mills C, Asadi K, et al. Hepatic angiosarcoma as a cause of acute liver failure. BMJ Case Rep (2018).
- Chandra S Bhati, Anand N Bhatt, Graham Starkey, et al. Acute liver failure due to primary angiosarcoma: A case report and review of literature. World Journal of Surgical Oncology 6 (2008).
- Gurpreet Singh, Christopher Mills, Khashayar Asadi, et al. Hepatic angiosarcoma as a cause of acute liver failure. BMJ Case Rep (2018).
- Orlando G, Adam R, Mirza D, et al. Hepatic hemangiosarcoma: an absolute contraindication to liver transplantation--the European Liver Transplant Registry experience. Transplantation 95 (2013): 872-877.
- Kim B, Byun JH, Lee JH, et al. Imaging findings of primary hepatic angiosarcoma on gadoxetate disodium-enhanced liver MRI: Comparison with hepatic haemangiomas of similar size 73 (2018): 244-253.
- Yang KF, Leow VM, Hasnan MN, et al. Primary hepatic angiosarcoma: difficulty in clinical, radiological, and pathological diagnosis. Med J Malaysia. Févr 67 (2012): 127-128.
- Cassinotto C, Rullier A, Hocquelet A, et al. Hepatic angiosarcoma: A suggestive pattern of enhancement on dynamic MR imaging 96 (2015): 293-295.
- Kang TW. Safety of Percutaneous Biopsy for Hepatic Angiosarcoma: Results of a Multicenter Korean Survey (2016).
- Ogawa M. Primary Hepatic Angiosarcoma: A Case Report with 10-Year Patient Medical Data. Case Reports in Oncology 10 (2017).
- Nelson Chen, Aidan Yu, Jihye Jung. Editor’s Pick: Primary Hepatic Angiosarcoma: A Brief Review of the Literature. European Medical Journal (2018).
- Thelin CS. Primary Hepatic Angiosarcoma: A Clinicopathologic Report of. American Journal of Gastroenterology (2016).
- Wang ZB. Transcription factor ERG is a specific and sensitive diagnostic marker for hepatic angiosarcoma (2014).
- Venkataramani V, Küffer S, Cheung KCP, et al. CD31 Expression Determines Redox Status and Chemoresistance in Human Angiosarcomas. Clin Cancer Res Off J Am Assoc Cancer Res 24 (2018): 460-473.
- Chen G. Primary hepatic angiosarcoma in a 64-year-old man: A case report (2016).
