Hemodynamic Retinal Artery Occlusion with Ipsilateral Carotid Artery Occlusion
Article Information
Jiunn-Feng Hwang1*, Yu Chen1, San-Ni Chen1,2
1Department of Ophthalmology, Changhua Christian Hospital, Changhua, Taiwan
2School of Medicine, China Medical University, Taichung, Taiwan
*Corresponding Author: Department of Ophthalmology, Chang-Hua Christian Hospital, 135 Nan-Siao St. Chang-Hua, 500, Taiwan, R.O.C.
Received: 02 September 2022; Accepted: 21 September 2022; Published: 14 October 2022
Citation: Jiunn-Feng Hwang, Yu Chen, San-Ni Chen. Hemodynamic Retinal Artery Occlusion with Ipsilateral Carotid Artery Occlusion. Archives of Clinical and Medical Case Reports 6 (2022): 686-688.
View / Download Pdf Share at FacebookAbstract
Retinal artery occlusion (RAO) with hemodynamic changes including ipsilateral carotid stenosis/occlusion, reduced blood flow, and responsive compensatory flow, is considered as hemodynamic RAO. Multiple emboli are highly associated with hemodynamic RAO that embolism may raise from turbulence of stenotic carotid artery or accompany with compensatory flow via the collaterals. With compensatory flow, most hemodynamic RAO are transient and may have fair visual outcome. In this hemodynamic RAO, severe ischemic macular edema and devastating visual outcome is a result of multiple mechanisms. Ipsilateral ICA occlusion with decreased blood flow, inadequate primary compensatory flow to the eye, elongated duration of an alternative compensatory flow to re-establish ophthalmic circulations, and terminal infarctions of multiple emboli may all contribute the irreversible retinal damage and poor vision.
Keywords
Carotid Occlusion; Cherry Red Spot; Hemodynamic; Retinal Artery Occlusion
Carotid Occlusion articles; Cherry Red Spot articles; Hemodynamic articles; Retinal Artery Occlusion articles
Carotid Occlusion articles Carotid Occlusion Research articles Carotid Occlusion review articles Carotid Occlusion PubMed articles Carotid Occlusion PubMed Central articles Carotid Occlusion 2023 articles Carotid Occlusion 2024 articles Carotid Occlusion Scopus articles Carotid Occlusion impact factor journals Carotid Occlusion Scopus journals Carotid Occlusion PubMed journals Carotid Occlusion medical journals Carotid Occlusion free journals Carotid Occlusion best journals Carotid Occlusion top journals Carotid Occlusion free medical journals Carotid Occlusion famous journals Carotid Occlusion Google Scholar indexed journals COVID-19 articles COVID-19 Research articles COVID-19 review articles COVID-19 PubMed articles COVID-19 PubMed Central articles COVID-19 2023 articles COVID-19 2024 articles COVID-19 Scopus articles COVID-19 impact factor journals COVID-19 Scopus journals COVID-19 PubMed journals COVID-19 medical journals COVID-19 free journals COVID-19 best journals COVID-19 top journals COVID-19 free medical journals COVID-19 famous journals COVID-19 Google Scholar indexed journals Cherry Red Spot articles Cherry Red Spot Research articles Cherry Red Spot review articles Cherry Red Spot PubMed articles Cherry Red Spot PubMed Central articles Cherry Red Spot 2023 articles Cherry Red Spot 2024 articles Cherry Red Spot Scopus articles Cherry Red Spot impact factor journals Cherry Red Spot Scopus journals Cherry Red Spot PubMed journals Cherry Red Spot medical journals Cherry Red Spot free journals Cherry Red Spot best journals Cherry Red Spot top journals Cherry Red Spot free medical journals Cherry Red Spot famous journals Cherry Red Spot Google Scholar indexed journals Ultrasound articles Ultrasound Research articles Ultrasound review articles Ultrasound PubMed articles Ultrasound PubMed Central articles Ultrasound 2023 articles Ultrasound 2024 articles Ultrasound Scopus articles Ultrasound impact factor journals Ultrasound Scopus journals Ultrasound PubMed journals Ultrasound medical journals Ultrasound free journals Ultrasound best journals Ultrasound top journals Ultrasound free medical journals Ultrasound famous journals Ultrasound Google Scholar indexed journals Hemodynamic articles Hemodynamic Research articles Hemodynamic review articles Hemodynamic PubMed articles Hemodynamic PubMed Central articles Hemodynamic 2023 articles Hemodynamic 2024 articles Hemodynamic Scopus articles Hemodynamic impact factor journals Hemodynamic Scopus journals Hemodynamic PubMed journals Hemodynamic medical journals Hemodynamic free journals Hemodynamic best journals Hemodynamic top journals Hemodynamic free medical journals Hemodynamic famous journals Hemodynamic Google Scholar indexed journals Radiotherapy articles Radiotherapy Research articles Radiotherapy review articles Radiotherapy PubMed articles Radiotherapy PubMed Central articles Radiotherapy 2023 articles Radiotherapy 2024 articles Radiotherapy Scopus articles Radiotherapy impact factor journals Radiotherapy Scopus journals Radiotherapy PubMed journals Radiotherapy medical journals Radiotherapy free journals Radiotherapy best journals Radiotherapy top journals Radiotherapy free medical journals Radiotherapy famous journals Radiotherapy Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals Prognosis articles Prognosis Research articles Prognosis review articles Prognosis PubMed articles Prognosis PubMed Central articles Prognosis 2023 articles Prognosis 2024 articles Prognosis Scopus articles Prognosis impact factor journals Prognosis Scopus journals Prognosis PubMed journals Prognosis medical journals Prognosis free journals Prognosis best journals Prognosis top journals Prognosis free medical journals Prognosis famous journals Prognosis Google Scholar indexed journals Thrombolysis articles Thrombolysis Research articles Thrombolysis review articles Thrombolysis PubMed articles Thrombolysis PubMed Central articles Thrombolysis 2023 articles Thrombolysis 2024 articles Thrombolysis Scopus articles Thrombolysis impact factor journals Thrombolysis Scopus journals Thrombolysis PubMed journals Thrombolysis medical journals Thrombolysis free journals Thrombolysis best journals Thrombolysis top journals Thrombolysis free medical journals Thrombolysis famous journals Thrombolysis Google Scholar indexed journals Retinal Artery Occlusion articles Retinal Artery Occlusion Research articles Retinal Artery Occlusion review articles Retinal Artery Occlusion PubMed articles Retinal Artery Occlusion PubMed Central articles Retinal Artery Occlusion 2023 articles Retinal Artery Occlusion 2024 articles Retinal Artery Occlusion Scopus articles Retinal Artery Occlusion impact factor journals Retinal Artery Occlusion Scopus journals Retinal Artery Occlusion PubMed journals Retinal Artery Occlusion medical journals Retinal Artery Occlusion free journals Retinal Artery Occlusion best journals Retinal Artery Occlusion top journals Retinal Artery Occlusion free medical journals Retinal Artery Occlusion famous journals Retinal Artery Occlusion Google Scholar indexed journals
Article Details
1. Introduction
Retinal artery occlusion (RAO) with hemodynamic changes including ipsilateral carotid stenosis or occlusion, reduced blood flow, and responsive compensatory flow, is considered as hemodynamic RAO. With compensatory flow, most hemodynamic RAO are transient and may have fair visual outcome. Herein, we performed multimodal imaging to investigate the reason why a case of hemodynamic RAO had severe macular edema and devastating visual outcome.
2. Case Presentation
A 64-year-old male present with acute vision loss in his right eyes. He was a smoker with history of systemic hypertension. On general physical examination, no focal neurologic deficits were noted. On ophthalmic examination, his best corrected visual acuity was light perception in the right eye and 10/10 in the left eye. Fundus examination revealed dense retinal whitening and a small cherry-red spot. Multiple emboli were found on the disc, at the bifurcations, and terminals of retinal arteries (Figure 1). Fluorescein angiography (FA) showed delayed slow retinal arterial filling present after 30 seconds. Arterial flow is not obstructed by emboli on the disc, but is infarcted at peripheral terminals. Central macula remained dark with enlarged foveal avascular zone. Immediate spectral-domain optical coherence tomography (OCT) revealed marked macula swelling and high reflectivity of the inner retina with fluid accumulation. Foveal thickness exceeded 600 um. OCT at one week follow up showed ischemic macular edema with ILM detachment. There were migration of emboli at the posterior pole by infrared photograph. Carotid color Doppler images (CDI) showed atherosclerosis with severe stenosis to nearly total occlusion of right internal carotid artery (ICA). Arterial flow decreased to 76.5 (cc/min) at proximal ICA and were vanished at the occlusion site. There were relatively increased flows of left proximal ICA (301.3 cc/min) and left vertebral artery (221.3 cc/min) as responsive compensatory flow to maintain the intracranial circulation. Orbital CDI revealed reversed right ophthalmic flow. This patient was referred to neurology department for further evaluation and treatment. Vascular surgery such as carotid stenting was suggested but refused by patient after explanation due to stable condition and no neurologic deficit developed during follow up. His visual acuity maintained light perception in the right eye. At five week follow up, OCT demonstrated subsided macular edema. More emboli can be identified at central macula. At three year follow up, OCT demonstrated macula thinning with flat fovea. No rubeosis iridis was found.
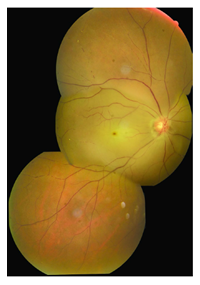
Figure 1: Montage fundus photograph of right RAO with dense retinal whitening and a small cherry red spot. There are emboli on the disc, at the bifurcations and terminals; with presence of boxcarring of blood column in the retinal vessels.
3. Discussion and Conclusions
Embolism originated from carotid or cardiac lesion is the most common cause of retinal artery occlusion (RAO) while ipsilateral carotid occlusion with hemodynamic changes, including reduced ocular/cerebral blood flow and responsive compensatory flow, may also result in retinal ischemia [1,2]. RAOs with multiple emboli are highly associated with severe carotid occlusion with hemodynamic flow changes [2]. Embolism may raise accompany with compensatory flow via the collaterals [2]. Herein, we performed comprehensive evaluations including FA, OCT, and CDI to investigate the reason why a hemodynamic RAO had severe macular edema. At first glance, we can find dense macular opacity with a small cherry-red spot by ophthalmoscopy (Figure 1), and pompous edematous retina demonstrated by OCT. It is well known that ganglion cells are absent within the fovea but clustered at the foveal margin, and are highly sensitive to ischemia. During RAO, these neuronal cells become edematous and the intracellular swelling accounts for the retinal opacity. It could lead to sequential displacement of ischemic swollen neuronal cells toward the fovea and thus derange foveal contour [3]. More ischemic the retina is, more edematous neuronal cells are displaced toward central fovea, which in turn might obscure the border of fovea to form a cherry-red spot in smaller size [3]. In response to ipsilateral ICA occlusion, compensatory flow from contralateral ICA may be adequate to maintain the intracranial circulations that there happened no neurologic deficit in this case. But primary compensatory flow may be inadequate to the eye that FA showed delayed slow retinal arterial filling and orbital CDI revealed reversed ophthalmic flow indicating an alternative compensatory flow arise from external carotid/ophthalmic collaterals for substitute. It went a longer way to reach the eye. The retina can tolerate transient ischemia but suffers irreversible damage after prolonged occlusion [4]. A schematic diagram illustrates the compensatory flow and collateral pathways to demonstrate above hemodynamic changes (Figure 2). During hemodynamic changes, reopen the external carotid/ophthalmic collaterals and flow direction changes may raise dust or facilitate debris scaling off the vessel wall and become micro emboli in the fundus [2]. Accompany with the compensatory flow, most micro emboli will migrate and disappear in distal arteries and are believed to cause no harm at all. Clinically, this is true for the brain but not always right for the eye once there is an accumulation to infarct the retinal terminals. These emboli may accumulate on the disc, the bifurcations, and disperse to peripheral retinal territories to cause terminal infarctions (Figure 1). Infrared photograph of OCT is helpful to identify emboli and to demonstrate the migration, appearance and disappearance of emboli. Restored retinal flow with absence of macular filling on FA is a very specific sign of transient RAO [5]. It is considered that the retinal capillaries in central macula do not refill because of compression by the surrounding swollen retinal tissue5. In this case, we can find the same pictures, RAO with dense retinal whitening; restored retinal flow and enlarged foveal avascular zone by FA; and high elevated macular thickness by OCT to support this mechanism. However, as ischemic retinal whitening subsided at follow up, more retinal emboli can be identified at the posterior pole under infrared photographs of OCT. It is possible that micro emboli may embed into the capillary network to cause terminal infarctions to aggravate the retinal damage and to contribute formation of enlarged foveal avascular zone on FA as well. In this case of hemodynamic RAO, severe ischemic macular edema and devastating visual outcome is a result of multiple mechanisms. Ipsilateral ICA occlusion with decreased blood flow, inadequate primary compensatory flow to the eye, elongated duration of an alternative compensatory flow to re-establish ophthalmic circulations, and terminal infarctions of multiple emboli may all contribute the irreversible retinal damage and poor vision. It is our suggestion that RAO patient should have thorough ocular and carotid evaluations, including orbital CDI.
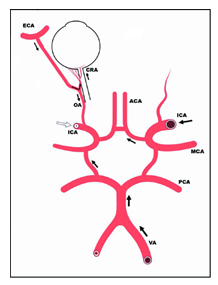
Figure 2: Schematic diagram illustrates the collateral pathways in the status of right ICA occlusion. There are compensatory flows from the left ICA and vertebral arteries for the brain but may not be sufficient to the eye. The source of ocular blood supply is then from the branch of ECA that the ophthalmic flow become retrograde in the orbit. (Abbreviations: ICA- Internal Carotid Artery; ECA- External Carotid Artery; ACA- Anterior Cerebral Artery; MCA- Middle Cerebral Artery; VA- Vertebral Artery; OA- Ophthalmic Artery.)
References
- Hayreh SS, Podhajsky PA, Zimmerman MB. Retinal artery occlusion: associated systemic and ophthalmic abnormalities. Ophthalmology. 116 (2009): 1928-1936.
- Chen SN, Hwang JF, Huang J, et al. Retinal arterial occlusion with multiple retinal emboli and carotid artery occlusion disease. Haemodynamic changes and pathways of embolism. BMJ Open Ophth 5 (2020): e000467.
- Chen SN, Hwang JF, Chen YT. Macular thickness measurements in central retinal artery occlusion by optical coherence tomography. Retina 31 (2011): 730-737.
- Hayreh SS, Zimmerman MB, Kimura A, et al. Central retinal artery occlusion. Retinal survival time. Exp Eye Res 78 (2004): 723-736.
- Hayreh SS, Zimmerman MB. Central retinal artery occlusion: visual outcome. Am J Ophthalmol 140 (2005): 376-391.
