Helical vs Conventional CT in Routine Head Imaging. A Comparison of Dose and Image Quality using VGC Analysis
Article Information
Dousi M1,2*, Fatsi A1, Sotirakou K1, Gkatzia N3, Patelarou M1, Theodosiou A1
1General Hospital “Elpis”, Athens, Greece
2University of West Attica, Athens, Greece
3General Oncology Hospital “Agioi Anargyroi”, Athens, Greece
*Corresponding Author: Maria Dousi, 59 Mylon, 10441 Athens, Greece
Received: 14 March 2021; Accepted: 23 March 2021; Published: 30 March 2021
Citation: Dousi M, Fatsi A, Sotirakou K, Gkatzia N, Patelarou M, Theodosiou A. Helical vs Conventional CT in Routine Head Imaging. A Comparison of Dose and Image Quality using VGC Analysis. Journal of Radiology and Clinical Imaging 4 (2021): 036-049.
View / Download Pdf Share at FacebookAbstract
Purpose: To compare and evaluate the sequencial and helical head CT imaging acquisition nodes in terms of patient dose and image quality.
Material and Methods: Sixty patients were studied in total for one week from July 2018 to July 2019 and all underwent two head CT exams. The first time a conventional technique was used and the other one the helical technique. Scan parameters and dose indices were recorded on a checklist at the end of each examination. The images were rated by three radiologists according to the criteria of the European Guidelines on Quality Criteria for Computed Tomography.
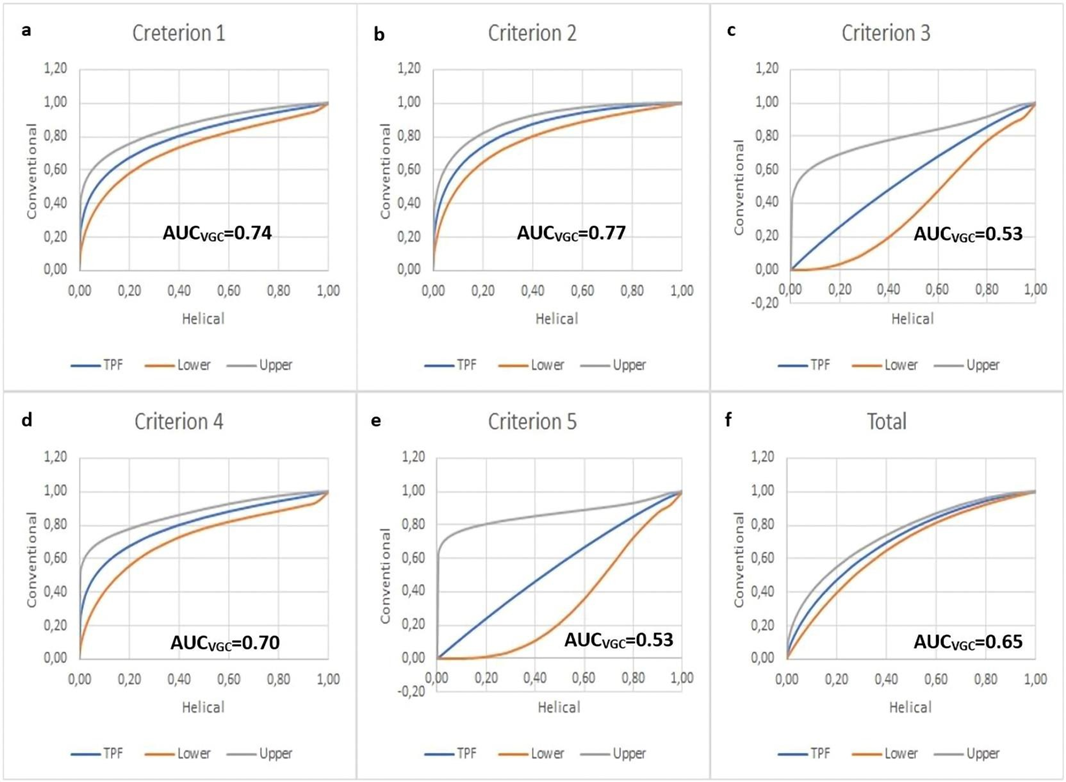
Results: Mann-Whitney U test showed that both dose indicators CTDIvol and DLP were statistically higher (p<0.05) in helical (Mean CTDIvol=34.15, Mean DLP=532.47) than in conventional scanning mode (Mean CTDIvol=31.73, Mean DLP=464.91). According to our study, the helical technique recorded a higher dose in patients compared to the conventional one. Visual Grading Characteristics analysis showed that image quality based on criteria 1, 2, 4 is statistically higher (Criterion 1 AUCVGC=0.74, Criterion 2 AUCVGC=0.77, Criterion 4 AUCVGC=0.70, p<0.05) in conventional technique and does not differ in statistics based on criteria 3, 5 (Criterion 3 AUCVGC: 0.52, Criterion 5 AUCVGC=0.52, p>0.05). According to the AUCVGC, the scores of the conventional technique images were statistically significantly higher than the helical ones (AUCVGC=0.65, p<0.05).
Conclusions: The radiation dose from sequential scanning was found to be statistically lower than in the helical scanning. According to the AUCVGC the sequential acquisition mode produces images of superior image quality than helical acquisition mode.
Keywords
Multidetector Computed Tomography; Brain; Image Quality Enhancement
Multidetector Computed Tomography articles; Brain articles; Image Quality Enhancement articles
Article Details
1. Introduction
CT brain scan was believed to be a revolutionary brain imaging method [1]. Therefore, it is a first line brain exam and the most frequently performed to identify various brain disorders [2]. Introduced in 1989, helical CT [3, 4] was proved to be a revolutionary technique as it reduced the scanning time, established the breath-hold technique and was able to reduce the motion artefacts [5]. In addition, the data acquisition in helical technique is continuous, which results in an improvement in post processing of MPR and VRT reconstructions [6]. Despite its advantages, the helical technique is not preferred for brain imaging, since head CT scan is not seriously affected from motion respiration artefacts. Furthermore, low contrast differences, such as gray and white matter, are not adequately revealed [7]. Up to now, it is not clear whether the helical CT produces such good quality images to replace those of conventional CT. For example, studies have revealed that the axial technique yields better image quality, especially in structures with low contrast differences [7, 8], yet another study has shown that the two techniques attribute similar image quality [9]. In addition, there are studies suggesting that helical technique has a lower dose [8, 10] whereas other show the exact opposite [11].
Τhe production of high quality images in CT is of great importance for the early diagnosis of pathologies [12, 13]. However, the improvement of CT image quality is accompanied by an increase in the dose [14]. Optimisation aims to reduce the dose of radiation by maintaining meanwhile a diagnostically acceptable result. More specifically, the gradual modification of exposure parameters aims to reduce exposure to radiation, but without compromising the quality of imaging [15]. There are various methods to determine the image quality, such as visual grading analysis (VGA), which is a well established method [16, 17]. VGA analysis determines image quality by evaluating the anatomical structures displayed in CT images based on a set of criteria that have to be fulfilled [18-20]. To our knowledge, on one hand no study has been conducted so far where both techniques were used to the same patients. On the other hand, our study is the first one to have used the VGC analysis. The purpose of our study was to compare and evaluate the sequential and helical acquisition mode for head CT imaging in terms of doses and image quality. Doses were compared and evaluated based on dose indexes CTDIvol and DLP. Image quality was evaluated by three radiologists. Each radiologist visually rated the anatomical structures according to the European Quality Criteria Guidelines for Computed tomography. VGA analysis was then performed based on radiologist scores.
2. Materials and Methods
Prior to conducting the study, a permission was requested and approved by the scientific council of the hospital where the data was collected.
The study lasted for a whole year and was conducted from July 2018 to July 2019. Τhe study included patients who performed routine head CT and the indications leading to an examination were intracranial hemorrhage, stroke, headache or vertigo. As the patients' clinical condition deteriorated, the clinicians requested a second computed tomography scan. Those patients who repeated the examination in less than one week were included in the study. The second exam was requested when despite the fact that the first was negative, the patient's condition deteriorated. In addition, the second exam was requested to investigate hemorrhagic conversion, in cases where ischemic stroke was found in the first exam. The first exam was performed using the conventional (i.e. sequential) acquisition mode and the second one using the helical technique.Τhe study initially included 65 patients. A total of five patients were excluded from the study, as three of them suffered extensive cerebral hemorrhage, so the image quality criteria could not be estimated. In the fourth patient, the images suffered from extensive motion artefacts. Although the fifth patient had a normal first exam, the second revealed an extensive stroke, which would lead to heterogeneity in the data, therefore the patient was excluded from the study. As a result, this study finally included 60 patients. In 48 patients, both of the exams were normal, whereas, twelve patients had a minor stroke. Those patients were not excluded from the study so as to evaluate the quality of the images of both techniques in the disclosure of pathologies. All exams were performed by the same dual slice CT (Siemens Emotion Duo).
Data was recorded on a checklist and collected prospectively. The recorded exam parameters were the following:
- Mean mAs
- kV
- Rotation Time
- Slice thickness
- Section Collimation
- Gantry tilt
- Feed
- Pitch
- Exposure Time
- Scan length
- CTDIvol
- DLP
Images were scored by three radiologists, each of whom had at least three years of experience in CT. The radiologists rated five anatomical structures according to their level of visibility on a scale of 1 to 5 (1 indicating confident that the criterion is not fulfilled and therefore the anatomical structure was not at all visible, 2 indicating somewhat confident that the criterion is not fulfilled, 3 indicating indecisive whether the criterion is fulfilled or not, 4 indicating somewhat confident that the criterion is fulfilled and 5 indicating confident that the criterion is fulfilled and therefore excellent visibility) according to the European Guidelines on Quality Criteria for CT [21] (Table
1). The examinations were anonymous and the radiologists scored them blindly at the Siemens workstation.
|
1. Visually sharp reproduction of the border between white and grey matter. |
|
2. Visually sharp reproduction of the basal ganglia |
|
3. Visually sharp reproduction of the ventricular system. |
|
4. Visually sharp reproduction of the cerebrospinal fluid space around the mesencephalon. |
|
5. Visually sharp reproduction of the cerebrospinal fluid space over the brain. |
Table 1: European Guidelines on Quality Criteria for Computed Tomography.
Statistical analysis was performed using SPSS (Version 25.0. Armonk, NY: IBM Corp). In order to assess the reliability of the observers and because the data were ordinal, we conducted a Pearson’s correlation. In order to determine the dose differences between the two techniques, we checked the distribution of the variables CTDIvol and DLP. The Kolmogorov - Smirnoff and Shapiro - Wilk tests showed that both CTDIvol and DLP variables do not follow a normal distribution for a 5% significance level. Therefore, the non-parametric control of Mann-Whitney U test was used. Paired sample t-test was used in order to determine differences in the exam parameters. In addition, dose differences were found between the two techniques using paired sample t-test. 95% confidence interval was selected for all measurements. The non-parametric statistical analysis, developed by Båth and Månsson [17] and called Visual Grading Characteristics (VGC) was used for VGA analysis. VGC analysis is a method similar to Receiver Operating Characteristics (ROC) analysis, with the difference that ROC focuses on the detection of pathology, while VGC on assessing image quality [22]. The VGC curves of the VGC analysis were created using the web- based calculator for ROC curves developed by John Eng, M.D., and Russell H. Morgan at the Department of Radiology and Radiological Science, Johns Hopkins University, Baltimore, MD, USA (available online at: http://www.rad.jhmi.edu/jeng/javarad/roc/JROCFITi.ht ml). The visual grading characteristics (VGC) data points are plotted to produce a VGC curve indicating the sensitivity or True Positive Fraction (TPF).
3. Results
3.1 Group of patients
The age of the patients ranged from 47 to 90 years with an mean of 74 years. 29 (48.3%) were men and 31 women
(51.7%).
3.2 Routine scan protocols
Both helical and conventional techniques are performed in the general hospital from which the data was collected. For each technique only one scan was conducted. The scan parameters of the 2 techniques are shown in Table 2. Paired sample t-test showed that there is a statistically significant difference in the following scan parameters, mAs (p<0.05), Scan length (p<0.05) and Exposure time (Table 3).
3.3 Observer reliability
In order to assess the reliability of the observers, we performed Pearson’ s correlation. All corelations were positive, which shows agreement on al three radiologists ratings. Additionally Pearson’ s correlation (r) for all criteria ranged between r=0.35 and 0.88 for the convertional technique. All correlations were statistically significant at 95% level (p<0.05), indicating consistency in all trhee radiologists scores proving that the reliability of the observers can not be attributed to chance. Cronbach’s alpha for each observer fell into the range of 0.66-0.94, indicating satisfactory internal consistency. Furthermonre, interobserver reliability with Pearson’s correlation (r) for helical technique ranged from r=0.39 to 0.93. All correlations were statistically significant at 95% level (p<0.05). Cronbach’s alpha ranged from 0.73 to 0.93, indicating very good internal consistency for each observer.
3.4 CTDI vol and DLP
The non-parametric test of Mann-Whitney showed that there was a statistically significant difference in the dose between the two techniques both in CTDIvol (p < 0,05) and DLP (p < 0,05) index. In addition, paired sample t-test showed that there is a statistically significant difference in both CTDIvol (p<0.05) and DLP (p<0.05) between the 2 methods (Table 3). Mean CTDIvol and Mean DLP were 34.15 and 532.47 for the helical CT and 31.73 and 464.91 for the conventional CT. The conventional method recorded the lower doses. Descriptive statistics from the two variables are shown in Table 4.
3.5 VGA analysis
The mean rating scores for all 5 image quality criteria are shown in Table 5.
VGC analysis was performed for the scores of each criterion as well as for the average of the total scores. The results of the VGC analysis are shown in Figure 1. The area under the curve (AUCVGC) is a measurement of the difference in image quality between the two techniques. A VGC curve located on or near the diagonal (AUCVGC=0.5) indicates that the two techniques produce images of the same quality. The greater the AUCVGC (>0.5) value, the better image quality produced by the technique on the vertical axis of the chart. An overall comparison of the AUCVGC values of the three observers for all criteria of the two techniques is shown in Table 6. For criterion 1, AUCVGC was 0.74 with a standard error of 0.047. For criterion 2, AUCVGC was 0.77 with a standard error of 0.049. For criterion 3, AUCVGC was 0.52 with a standard error of 0.061. For criterion 4, AUCVGC was 0.70 with a standard error of 0.046. For criterion 5, AUCVGC was 0.52 with a standard error of 0.06. Finaly, for both techniques, AUCVGC was 0.65 with a standard error of 0.06.
P value was calculated with one sample t-test. The results are shown in Table 7. Statistically significant differences (p<0.05) were recorded in the AUCVGC values from the 0.5 value for criteria 1, 2, 4, indicating that the conventional technique has statistically superior image quality than the helical one. Νο statistically significant differences (p>0.05) were recorded in the AUCVGC values from the 0.5 value for criteria 3, 5, indicating similar image quality between the two techniques. Finaly, statistically significant differences (p<0.05) were recorded in the AUCVGC values from the 0.5 value for all criteria, indicating that the conventional technique has overall statistically superior image quality than the helical one.
|
Conventional and Helical Scan Protocols |
||
|
Scan parametrs |
Conventional |
Hellical |
|
Mean mAs |
99.2 |
134.82 |
|
Kv |
130 |
130 |
|
Rotation Time |
1.5 |
1.5 |
|
Slice thickness |
2.5 mm |
3 mm |
|
Section Collimation |
2x2.5 mm |
2x2.5 mm |
|
Gantry tilt |
16-30 (Mean: 27) |
- |
|
Feed |
5 mm |
- |
|
Pitch |
- |
1 |
|
Mean Exposure Time |
40.98 |
42.49 sec |
|
Mean Scan length |
145.9 |
157.18 mm |
Table 2: Scan parameteters for the protocols of the 2 techniques.
Table 3: Results from the paired sample t-test.
|
Dose Indexes |
Technique |
n |
Mean |
Std. Deviation |
Min |
Μax |
|
CTDIvol (mGy) |
Conventional |
60 |
31.73 |
3.33 |
26.68 |
40.11 |
|
DLP (mGy cm) |
Helical |
60 |
34.15 |
4.45 |
28.73 |
48.44 |
|
Conventional |
60 |
464.91 |
75.18 |
324.22 |
683.83 |
|
|
Helical |
60 |
532.47 |
76.29 |
398.74 |
738.04 |
Table 4: Descriptive statistics from the 2 indexes. Mean, min and max values from the dose indexes CTDIvol and DLP of the helical technique are significantly higher than the values of the conventional technique.
|
Criteria |
Mean Rating Score |
|
|
Conventional |
Helical |
|
|
1 |
4.68 |
4.16 |
|
2 |
4.48 |
3.83 |
|
3 |
4.86 |
4.80 |
|
4 |
4.78 |
4.37 |
|
5 |
4.90 |
4.86 |
Table 5: Mean Rating Score in Image Quality Criteria.
Figure 1: The visual grading characteristic (VGC) curve from the data of scores. The boxes represent the operating points corresponding to the observer’s interpretation of the rating scale steps. (a) VGC for criterion 1; (b) VGC for criterion 2; (c) VGC for criterion 3; (d) VGC for criterion 4; (e) VGC for criterion 5; (f) VGC for the 2 techniques.
|
Conversional vs Helical technique |
AUCVGC |
Mean AUCVGC for 3 observers for all criteria |
|
Observer 1 |
0.66 |
Criterion 1:0.74 Criterion 2:0.77 Criterion 3:0.53 Criterion 4:0.70 Criterion 5:0.53 Total:0.65 |
|
Criterion 1 |
0.73 |
|
|
Criterion 2 |
0.83 |
|
|
Criterion 3 |
0.56 |
|
|
Criterion 4 |
0.72 |
|
|
Criterion 5 |
0.50 |
|
|
Observer 2 |
0.62 |
|
|
Criterion 1 |
0.71 |
|
|
Criterion 2 |
0.74 |
|
|
Criterion 3 |
0.50 |
|
|
Criterion 4 |
0.72 |
|
|
Criterion 5 |
0.53 |
|
|
Observer 3 |
0.66 |
|
|
Criterion 1 |
0.77 |
|
|
Criterion 2 |
0.73 |
|
|
Criterion 3 |
0.52 |
|
|
Criterion 4 |
0.72 |
|
|
Criterion 5 |
0.55 |
Table 6: Statistical comparison of AUCVGC values for each observer and each criterion for the two techniques.
|
One-Sample Test |
||||||
|
Test Value = 0.5 |
||||||
|
t |
df |
Sig. (2-tailed) |
Mean Difference |
95% Confidence Interval of the Difference |
||
|
Lower |
Upper |
|||||
|
Criterion 1 |
13.418 |
2 |
0.006 |
0.23667 |
0.1608 |
0.3126 |
|
Criterion 2 |
8.386 |
2 |
0.014 |
0.26667 |
0.1299 |
0.4035 |
|
Criterion 3 |
1.512 |
2 |
0.270 |
0.02667 |
-0.0492 |
0.1026 |
|
Criterion 4 |
9.302 |
2 |
0.011 |
0.20333 |
0.1093 |
0.2974 |
|
Criterion 5 |
1.835 |
2 |
0.208 |
0.02667 |
-0.0358 |
0.0892 |
|
Total |
11.000 |
2 |
0.008 |
0.14667 |
0.0893 |
0.2040 |
Table 7: Results from the one sample t test.
4. Discussion
The findings of this study regarding the radiation dose contradict the findings of Pace and Zarb's [8] and Abdeen et [10] studies showing that the helical technique has a lower dose than the conventional one. Certain variants in screening protocols may lead to dose differences [23]. For example, in Pace and Zarb's study, two different protocols were used in the sequential technique: one for the posterior fossa, and another for the cerebrum. On the other hand, only one protocol was used in the spiral technique. Respectively, in the Abdeen et al. study, two different protocols were used for the conventional and one for the helical technique. There were differences in mA and KV between the two protocols of the conventional technique. 120 kVp and 150 mA were used for cerebrum and 140 kVp and 170 mA for posterior fossa. Difference in the peak kilovoltage may lead to different dose results. When the tube potential increases, both outlet and the beam penetration are improved, while image contrast decreases [24]. These differences in those studies may have led to different results from ours. Another factor than can affect radiation dose is Automatic Exposure Control (AEC) systems. In fact, AEC systems (e.g., quality reference mAs for Siemens, smart mAs for GE) can significantly reduce the dose [25].
Αn essential factor that may have increase the dose in helical scanning is the number of CT slices. This hypothesis is confirmed by the Straten et al. study, in which the findings argued that the old CT scanners, like the 4 sections, yielded a higher dose in the helical technique [26]. Another factor that can affect the dose is z overscanning, which is a feature of helical technique. This feature is required because interpolation algorithms are used in helical scanning. To be more specific, interpolation algorithms use data beyond the imaging volume. As the Tzedakis et al. study showed, z overscanning can significantly increase the patient dose to all protocols [27]. Slice collimation may also affect dose thus leading our study to different results. A narrow slice collimation is necessary for a narrow slice thickness, but its impact on patient dose is restricted to aspects of overbeaming and overscanning. In practice, overbeaming is not a real problem for single- and dual-slice scanners, as the limited coverage does not allow narrow beam width with the exception of some exams with a limited scanning range. In contrast, overbeaming effects have to be taken into account in MSCT, as those systems aims to improve the resolution along the z-axis, which requires a reduction in slice collimation. Generally, beam width, larger than 10 mm has almost equally good performance, with the exception of small scan areas (e.g., pediatric patients). In such cases, a beam width of between 10 and 20 mm is more appropriate. A beam width less than 10 mm width should be avoided due to overbeaming [24].
The present study showed that the conventional technique produces higher quality images, which agrees with the findings of Abdeen et al. [8] and Pace and Zarb [10] study, but contradicts the one of Straten et al. [26]. Although the scanning protocols in the two techniques were identical, the conventional technique yields better quality images. This may be due to a number of factors, such as the increase in noise in helical images due to the interpolation algorithm. The 180o interpolation algorithm can increase the noise in images by 13% [28]. Since dose and image quality are linked [29], the exposure parameters affect both. The Straten et al. study [26] showed that radiologists prefer helical scanning both because it generates generally higher quality images and highlights low contrast differences, such as between gray and white matter [26]. Similarly, Jones et al. study showed the observer's preference for helical scan images produced by a CT of 4 sections [30] whose findings contradict our study. One reason for this is probably the different CT systems used which can lead to image differences. Comparisons in single, 4-, 16- and 64- computed tomography systems showed improved image quality and reduced posterior fossa artefacts in the head exam when a 64-slice system was used for the helical technique [31].
Another reason is probably the two different protocols used e.g., in the study of Abdeen et al., since sequential acquisitions contained more posterior fossa artefacts compared to the helical technique, in both 16- and 64-slice systems [10]. This artefacts reduction is due to a decrease in collimation and slice thickness between the two protocols. Helical scan had a smaller slice thickness. Α narrow collimation is necessary to produce thin slices. Reducing the slice thickness can lead to better detail contrast (due to the reduction of the partial volume effect), but also an increase in the noise. However, the total gain in the contrast to noise ratio (CNR) offsets the noise increase without increasing the dose [24]. Of course, different protocols should be used according to different clinical indications [32, 33]. This is because the use of the same parameters in patients with different clinical indications can lead to misdiagnosis. For example, the inconsistency of the reconstruction interval in the spiral scans can lead to neglect of pathologies e.g., metastasis, hemorrhage), especially when MPR reconstructions are not performed [32].
The Kuntz et al. study used a CT of 4 sections and found small to no differences between the gray and the white matter and the overall image quality between the two techniques [9]. This is in contrast to our own findings were the differences between white and gray matter (criterion 1) according to VGC curve were statistically significant between the two techniques. The importance of quality criteria has been highlighted in other studies, which point out that criteria 1 (Visually sharp reproduction of the border between white and grey matter) and 5 (Visually sharp reproduction of the cerebrospinal fluid space over the brain) are the most important for observers [34]. It should be noted that modern CT systems, which have modern IR algorithms could differentiate the result in image quality and dose between the two techniques. Studies have shown that the IR algorithms of four manufacturers (Siemens, GE, Phillips, Toshiba) improved the overall image quality in the head examination compared to the conventional Filtered Back Projection (FBP) reconstruction in most or all of the evaluated quality criteria. Further improvement was achieved with one of the model-based IR algorithms, especially at lower dose levels, indicating further possibility of dose reduction [35].
VGC analysis is advantageous because it can be used directly in the image quality criteria as defined by the European Commission and in the existing images, without the necessity of a gold standard during the evaluation [17, 28]. In addition, it can be used to simultaneously assess multiple factors that affect image quality [31]. This may result to an increase in the use of criteria in order to produce better quality images [17]. VGC analysis in this study showed that conventional technique prevails over helical technique in all criteria and specifically in criteria 1, 2, 4 the differences between the two methods were statistically significant. In addition, the VGC analysis suggested that the conventional method is better than the helical one and the differences of overall quality were statistically significant. This contradicts the findings of Kuntz et al. [9], which argue that in a modern scanner the quality of an adult's brain images produced by the two techniques is almost equivalent.
The differences in our study compared to others is mainly due to the different CT systems and the different protocols used. Different organizations (American College of Radiology-ACR, European Commission-EC) recommend different protocols for head examination. Even nowadays, helical CT has not completely replaced conventional technique in routine brain examinations. This may be due to practical limitations but also the fact that there are still unresolved issues regarding image quality [23]. All these findings were confirmed by our study. One of this study limitations was that data derived from a single 2 slices CT and a single public hospital where the equipment is old and does not have the modern IR algorithms. Another limitation was the use of local scanning protocols, which may have led to differences between the two techniques.
5. Conclusion
The radiation dose using the conventional technique was found to be statistically lower than the helical one when it came to CTDIvol and DLP indexes. Statistically significant differences were found in scanning parameters (mAs, Scan length, Exposure Time) between the two techniques. According to the VGC curves, the quality of images based on criteria 1, 2, 4 was found to be statistically higher in the conventional technique. On the other hand, image quality based on criteria 3, 5 does not differ statistically between the two techniques. In conclusion, the conventional method produces statistically better image quality, according to the AUCVGC.
Acknowledgments
None.
Conflicts of Interest
There are no conflicts of interest to declare.
References
- Erkonen WE, Smith WL. Radiology 101: the basics and fundamentals of imaging. Lippincott Williams & Wilkins (2009): 295-310.
- Lee B, Newberg A. Neuroimaging in traumatic brain imaging. NeuroRx 2 (2005): 372-383.
- Kalender W, Seissler W, Vock P. Single-breath-hold spiral volumetric CT by continuous patient translation and scanner rotation. InProceedings of the 75th anniversary scientific assembly and annual meeting Radiological Society of North America (Abstracts) (1989).
- Rigauts H, Marchal G, Baert AL, et al. Initial experience with volume CT scanning. J Comput Assist Tomogr 14 (1990): 675-682.
- Vock P, Soucek M, Daepp M, et al. Lung: spiral volumetric CT with single-breath-hold technique. Radiology 176 (1990): 864-867.
- Ney DR, Fishman EK, Kawashima A, et al. Comparison of helical and serial CT with regard to three-dimensional imaging of musculoskeletal Radiology 185 (199): 865-869.
- Bahner ML, Reith W, Zuna I, et al. Spiral CT vs incremental CT: is spiral CT superior in imaging of the brain? Eur Radiol 8 (1998): 416-420.
- Pace I, Zarb F. A comparison of sequential and spiral scanning techniques in brain CT. Radiol Technol 86 (2015): 373-378.
- Kuntz R, Skalej M, Stefanou A. Image quality of spiral CT versus conventional CT in routine brain imaging. Eur J Radiol 26 (1998): 235-240.
- Abdeen N, Chakraborty S, Nguyen T, et al. Comparison of image quality and lens dose in helical and sequentially acquired head CT. Clin Radiol 65 (2010): 868-873.
- Van Straten M, Venema HW, Majoie CB, et al. Image quality of multisection CT of the brain: thickly collimated sequential scanning versus thinly collimated spiral scanning with image combining. AJNR Am J Neuroradiol 28 (2007): 421-427.
- Mayo JR, Aldrich J, Muller NL. Radiation exposure at chest CT: a statement of the Fleischner Society. Radiology 228 (2003): 15-21.
- Kalra MK, Maher MM, Toth TL, et al. Strategies for CT radiation dose optimization. Radiology 230 (2004): 619-628.
- Watson SJ, Jones AL, Oatway WB, et al. Ionising radiation exposure of the UK population: 2005 review. Chilton, Oxon: Health Protection Agency (2005).
- Wallace AB, Goergen SK, Schick D, et al. Multidetector CT dose: clinical practice improvement strategies from a successful optimization program. J Am Coll Radiol 7 (2010): 614-624.
- Ludewig E, Richter A, Frame M. Diagnostic imaging– evaluating image quality using visual grading characteristic (VGC) analysis. Vet Res Commun 34 (2010): 473-479.
- Bath M, Mansson LG. Visual grading characteristics (VGC) analysis: a non-parametric rank-invariant statistical method for image quality evaluation. Br J Radiol 80 (20078): 169-176.
- Jurik AG, Jessen KA, Hansen J. Image quality and dose in computed tomography. Eur Radiol 7 (1997): 77-81.
- Crawley MT, Booth A, Wainwright A. A practical approach to the first iteration in the optimization of radiation dose and image quality in CT: estimates of the collective dose savings achieved. Br J Radiol 74 (2001): 607-614.
- Gerber TC, Kuzo RS, Morin RL. Techniques and parameters for estimating radiation exposure and dose in cardiac computed tomography. Int J Cardiovasc Imaging 21 (2005): 165-176.
- Menzel HG, Schibilla H, Teunen D. European guidelines on quality criteria for computed Luxembourg: European Commission (2000).
- Buttigieg EL, Grima KB, Cortis K, et al. An evaluation of the use of oral contrast media in abdominopelvic Eur Radiol 24 (2014): 2936-2944.
- Smith-Bindman R, Lipson J, Marcus R, et Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Archives of internal medicine 169 (2009): 2078-2086.
- Nagel HD. CT parameters that influence the radiation dose. In Radiation dose from adult and pediatric multidetector computed tomography. Springer, Berlin, Heidelberg (2007): 51-79.
- McCollough CH, Bruesewitz MR, Kofler Jr, JM. CT dose reduction and dose management tools: overview of available Radiographics 26 (2014): 503-512.
- Van Straten M, Venema HW, Majoie CB, et al. Image quality of multisection CT of the brain: thickly collimated sequential scanning versus thinly collimated spiral scanning with image combining. AJNR Am J Neuroradiol 28 (2007): 421-427.
- Tzedakis A, Damilakis J, Perisinakis K, et al. The effect of overscanning on patient effective dose from multidetector helical computed tomography examinations. Med Phys 32 (2005): 1621-1629.
- Polacin A, Kalender WA, Marchal G. Evaluation of section sensitivity profiles and image noise in spiral Radiology 185 (1992): 29-35.
- Brooks RA, Di Chiro G. Statistical limitations in x-ray reconstructive Med Phys 3 (1976): 237-240.
- Jones TR, Kaplan RT, Lane B, et al. Single–versus multi–detector row CT of the brain: quality Radiology 219 (2001): 750-755.
- Ertl-Wagner B, Eftimov L, Blume J, et al. Cranial CT with 64-, 16-, 4-and single-slice CT systems– comparison of image quality and posterior fossa artifacts in routine brain imaging with standard protocols. Eur Radiol 18 (2008): 1720-1726.
- Mahdavi M, Rahimi S, Eghlidospoor M. Evaluation of some spiral and sequential computed tomography protocols of adults used in three hospitals in Shiraz, Iran with American College of Radiology and European Commission guidelines. Pol J Radiol 83 (2018): 297.
- Brat H, Zanca F, Montandon S, et al. Local clinical diagnostic reference levels for chest and abdomen CT examinations in adults as a function of body mass index and clinical indication: a prospective multicenter study. Eur Radiol 29 (2019): 6794-6804.
- Zarb F, McEntee MF, Rainford L. Visual grading characteristics and ordinal regression analysis during optimisation of CT head examinations. Insights into imaging 6 (2015): 393-401.
- Löve A, Olsson ML, Siemund R, et al. Six iterative reconstruction algorithms in brain CT: a phantom study on image quality at different radiation dose BR J Radiol 86 (203): 20130388.