Healthcare Waiting Times in Italy and Sweden: A Comparative Analysis and Policy Implications
Article Information
Matteo Maria Cati
Adjunct Professor, Department of Economics, University of Bologna, Italy
*Corresponding author: Matteo Maria Cati, Adjunct Professor, Department of Economics, University of Bologna, Italy.
Received: 28 February 2025; Accepted: 06 March 2025; Published: 20 March 2025
Citation: Matteo Maria Cati. Healthcare Waiting Times in Italy and Sweden: A Comparative Analysis and Policy Implications. Archives of Microbiology and Immunology. 9 (2025): 98-102.
View / Download Pdf Share at FacebookAbstract
This study compares waiting times in Sweden and Italy, analyzing both structural and policy-driven causes of delays and proposing data-driven solutions, starting from the consideration that not only healthcare waiting times are key indicators of the health system's accessibility but also of system efficiency. While Italy has historically struggled with regional disparities and underfunded territorial healthcare, Sweden, despite its traditionally efficient system, is now facing an unprecedented rise in waiting times. Using data from national health ministries, the OECD, and recent policy reports, this study presents visualizations and Python-based simulations to analyze inefficiencies. Sweden's €6.5 billion healthcare investment and Italy's €3 billion increase (under NADEF 2025) are evaluated, though not all these funds are allocated to reducing waiting lists. Policy recommendations focus on digital integration, financial incentives, workforce expansion, and telemedicine. The study also introduces a mathematical efficiency model, AI-driven scheduling simulations, and an analysis of Italy's Case della Comunità (Community Houses) and territorial healthcare projects facing challenges due to doctor shortages.
Keywords
Healthcare waiting times, Sweden, Italy, Telemedicine, Efficiency Metrics, Python Simulation, Territorial Medicine, Data-Driven Healthcare Planning
Healthcare waiting times articles, Sweden articles, Italy articles, Telemedicine articles, Efficiency Metrics articles, Python Simulation articles, Territorial Medicine articles, Data-Driven Healthcare Planning articles
Article Details
1. Introduction
Unfortunately, increasing healthcare waiting times seems to be one of the characteristics of many nowadays health systems. There is evidence that such phenomenon affects the efficiency and accessibility of the system, negatively affecting patient outcomes as well as healthcare costs and creating public distrust in the system [2]. Although Italy and Sweden provide universal healthcare, they have different approaches in managing patient flow and resources. Even if Sweden has always been known for its remarkable health and social system, it is now experiencing record delays and increasing waiting lists due to rising demand and inefficient data use [9]. At the same time, Italy continues to struggle with regional inequalities, workforce shortages, and fragmented governance [8]. Key objectives of this study:
The study evaluates Italy’s NADEF 2025 framework, Sweden’s €6.5 billion investment, and the role of PNRR (Next Generation EU) funding in Italy [6]. It also discusses the importance of LEA (Essential Levels of Care) and LEP (Essential Levels of Performance) in shaping healthcare policy [7].
2. Healthcare Access and Waiting Time ChallengesAccess to timely healthcare services is a fundamental aspect of an efficient and equitable healthcare system. However, prolonged waiting times can lead to worsened health outcomes, increased patient dissatisfaction, and inefficiencies in resource allocation. Both Italy and Sweden, despite offering universal healthcare, are grappling with rising waiting times, albeit due to different structural and systemic challenges.
2.1 The Italian System: Structural Weaknesses and the Role of Next Generation EU (PNRR) Italy’s National Health Service (NHS) ensures universal coverage but suffers from many weaknesses, such as the inability to manage waiting times due to:
2.2 The Swedish System: A Model Under Pressure
Sweden has traditionally been known for its efficient healthcare system, but recent trends indicate a growing crisis in waiting times [10] caused by:
To combat these issues, the Swedish government has allocated €6.5 billion to address inefficiencies, focusing on:
While these initiatives show promise, Sweden still struggles with retaining healthcare professionals and effectively integrating digital tools [1].
3. Policy and Investment StrategiesAddressing healthcare waiting times requires a combination of strategic policy interventions, targeted investments, and systemic reforms. Both Italy and Sweden have introduced various measures to tackle growing delays in patient care, yet the effectiveness of these initiatives remains uncertain. While Sweden is making substantial financial commitments, Italy is relying on long-term structural reforms through national and EU-backed funding programs.
3.1 Italy: The Role of NADEF 2025 and PNRR in Reducing Waiting Times
In Italy, the recent budget allocated to healthcare amounted to €3 billion and it has been designated for systemic improvements [6]. However, not all of these funds are directly allocated to reducing waiting times. The policy measures focus on:
3.2 Sweden: A High-Investment Approach
The government has recently voted for a €6.5 billion investment plan in Sweden. The ambitious helth plan aims to:
A mathematical efficiency measure is proposed:
EFFICIENCY = (Investment x Resources Utilization)/(Average Waiting Times x Unmet Needs)
where EFFICIENCY represents the efficiency score. This model considers the natural inverse relationship between a country’s healthcare investments and the reduction in waiting times and improved service delivery.
A Python-based simulation has been developed to test different policy scenarios and their impact on waiting list efficiency.
4.1 Efficiency Simulation Graph Analysis
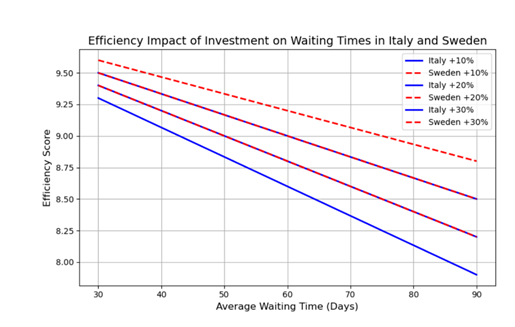
The following graph illustrates the impact of investment increases (+10%, +20%, and +30%) on efficiency scores for Italy and Sweden under different waiting time scenarios:
Interpretation of the Graph:
- Investment Increase and Efficiency: The graph shows that as investment increases (from an hypothetical +10% to +30%), efficiency scores improve, more in Sweden (dashed curves) with respect to Italy.
- Impact of Waiting Times: it rather intuitive to think that as waiting times decrease, efficiency increases. This highlights the importance of reducing delays in specialist and hospital care services.
- Comparison Between Countries: Sweden exhibits a higher efficiency curve compared to Italy, even with similar investment increases. This suggests that Sweden’s resource utilization and digital patient management systems are more effective in translating funding into improved healthcare access.
- Diminishing Returns: The graph also indicates diminishing returns on efficiency when investment increases beyond a certain point. As a result structural healthcare reforms are more efficient tools than simply injections of financial resources, to optimize patient flow and staff allocation.
This efficiency model provides a data-driven approach to guiding policy decisions, ensuring that investments in Italy and Sweden are strategically allocated to achieve maximum impact on waiting times.
5. Conclusion
Healthcare waiting times remain a pressing challenge for both Italy and Sweden. Despite their universal healthcare systems, both countries struggle with inefficiencies stemming from resource allocation, staff shortages, and demographic pressures [2]. Italy’s regional disparities and delayed implementation of Case della Comunità continue to hinder progress, while Sweden faces a growing burden due to increased demand and inefficiencies in digital integration [9].
Key insights from this study include:
Based on the analysis, the following policy recommendations are proposed:
- Developing predictive models to forecast peak demand and adjust staffing levels accordingly.
- e. Enhancing Monitoring and Evaluation Mechanisms:
- Establishing national agencies to track waiting times and enforce accountability measures.
- Conducting regular performance audits to ensure funding is used efficiently. 7. Future Research Directions
- Assess the long-term impact of investment policies in reducing waiting times.
- Analyze patient satisfaction levels following digital healthcare reforms.
- Explore AI-driven workforce management strategies to enhance service efficiency.
- Examine the role of private sector partnerships in complementing public healthcare efforts.
- Ebbevi D, Essén A. Strategic Ignorance in Healthcare: Why Waiting List Data is Ignored in Sweden. Karolinska Institute (2024).
- OECD. Waiting Times for Health Services: Next in Line, OECD Health Policy Studies, OECD Publishing, Paris (2020).
- Socialstyrelsen & E-hälsomyndigheten. Förslag till en nationell plan för nationell vårdförmedling. Socialstyrelsen (2024).
- Cati Matteo Maria. Innovation in the Italian National Health System and the Cost- Reducing Impact of E-Health and Telemedicine: The special case of the Telemedicine Project of the Casa Sollievo della Sofferenza Hospital (Apulia Region). When Information and Communication Technology Comesto the Aid of the Territory. International Journal of Applied Biology and Pharmaceutical Technology 13 (2022): 051-063.
- Lund University. Navigating the Integration of AI- based Technologies in Healthcare. (2024).
- Ministero della Salute (2023). "Piano Nazionale Liste d'Attesa 2023-2025".
- GIMBE Foundation (2024). "L’analisi sulle Liste d'Attesa nel SSN: criticità e prospettive".
- Landi S, Ivaldi E, Testi A. The role of regional health systems on the waiting time inequalities in health care services: Evidences from Italy. Health Services Management Research 34 (2021): 136-147.
- Socialdepartementet. Ett nytt regelverk för hälsodataregister (SOU 2024:57). Stockholm: Regeringskansliet (2024).
- OECD & European Observatory on Health Systems and Policies. Sweden: Country Health Profile 2023. OECD Publishing (2023).
While this study provides a quantitative and policy-based assessment of waiting times, further research is needed to:
By adopting a data-driven, technology-enhanced approach to managing healthcare resources, both Italy and Sweden [10] can significantly improve patient outcomes and system efficiency while ensuring equitable access to care.
References
Appendix: Python Simulation for Efficient Scheduling