Health, Environmental and Social Conditions for the Urban Poor in the Largest Cities of Pakistan –Policy and Planning Implications for Urban Poor Health Strategy
Article Information
Khawaja Aftab Ahmed1*, John Grundy2, Ms. Lubna Hashmat3, Imran Ahmed4, Saadia Farrukh5, Dexter Bersonda6, Muhammad Akram Shah7, Soofia Yunus7, Hari Krishna Banskota8
1Health Specialist – HSS, UNICEF Pakistan | St. 5., Diplomatic Enclave, Islamabad, Pakistan
2College of Public Health, Medicine, and Veterinary Sciences, James Cook University, Australia
3Chief Executive Officer, Civil Society Human and Institutional Development Programme – CHIP, CHIP House # 1, Street # 9, G.8/2, Islamabad, Pakistan
4Civil Society Human and Institutional Development Programme – CHIP, CHIP House # 1, Street # 9, G.8/2, Islamabad, Pakistan
5Health manager, Programme Section, Sana'a, UNICEF CO Yemen
6UNICEF Consultant, The Philippines
7EPI Program,National Institute of Health (NIH), Prime Minister’s Health Complex, Park Road, Chakshahzad, Islamabad, Pakistan
8Chief of Health Section, UNICEF, Pakistan, UNICEF Pakistan | St. 5., Diplomatic Enclave, Islamabad, Pakistan
*Corresponding Author: Dr. Khawaja Aftab Ahmed, Health Specialist – HSS, UNICEF Pakistan | St. 5., Diplomatic Enclave, Islamabad, Pakistan
Received: 22 April 2022; Accepted: 26 April 2022; Published: 08 June 2022
Citation: Khawaja Aftab Ahmed , John Grundy, Lubna Hashmat, Imran Ahmed, Saadia Farrukh, Dexter Bersonda, Muhammad Akram Shah, Soofia Yunus, Hari Krishna Banskota. Health, Environmental and Social Conditions for the Urban Poor in the Largest Cities of Pakistan –Policy and Planning Implications for Urban Poor Health Strategy. Journal of Environmental Science and Public Health 6 (2022): 217-235.
View / Download Pdf Share at FacebookAbstract
Uncertainty regarding numbers and locations of slums resulted in the conducting of urban slum profiles in the ten most populated cities of Pakistan between 2017 and 2019. The aim of this paper is to provide a national overview of health and social conditions in these urban areas and consider the policy and planning implications for improvements in health and social services. The Urban Slum Profiles included physical verification of slums, and assessments of health and social services and an immunisation coverage survey. The profiles found that 48% of the total urban population of the ten cities is living in slums or areas classified as being underserved by essential health services. Lower health service coverage is associated with poor housing and environmental conditions, under-employment, low-income status, inadequate availability of health services, and low health literacy coupled with profound gender and education disparities. Of the 14,531 children surveyed, 53% are fully immunised (n=5774), with rates of zero dose vaccination greater than 15% (n=1985) in six of the ten cities. Facility surveys (n=422 facilities) demonstrate insufficient availability of vaccination, social welfare, and nutrition services. Just 66% (n=9659) of mothers stated that vaccination protects from disease. Low participation in health by community-based organisations reinforces social marginalisation and lack of access to information on health care. Policy and planning implications from these findings rationalise the need for pro equity health services planning in urban poor areas, integration of services, and development of governance and social accountability mechanisms for health and immunization services management and delivery. The development of an integrated urban health strategy with a costed action plan will not only benefit the health of the urban poor, but will also serve to accelerate the overall economic, health and social development of Pakistan.
Keywords
Pakistan; Immunisation; Health Equity; Urban Health; PHC; Social Determinants
Pakistan articles; Immunisation articles; Health Equity articles; Urban Health articles; PHC articles; Social Determinants articles
Immunisation articles Immunisation Research articles Immunisation review articles Immunisation PubMed articles Immunisation PubMed Central articles Immunisation 2023 articles Immunisation 2024 articles Immunisation Scopus articles Immunisation impact factor journals Immunisation Scopus journals Immunisation PubMed journals Immunisation medical journals Immunisation free journals Immunisation best journals Immunisation top journals Immunisation free medical journals Immunisation famous journals Immunisation Google Scholar indexed journals Health Equity articles Health Equity Research articles Health Equity review articles Health Equity PubMed articles Health Equity PubMed Central articles Health Equity 2023 articles Health Equity 2024 articles Health Equity Scopus articles Health Equity impact factor journals Health Equity Scopus journals Health Equity PubMed journals Health Equity medical journals Health Equity free journals Health Equity best journals Health Equity top journals Health Equity free medical journals Health Equity famous journals Health Equity Google Scholar indexed journals Urban Health articles Urban Health Research articles Urban Health review articles Urban Health PubMed articles Urban Health PubMed Central articles Urban Health 2023 articles Urban Health 2024 articles Urban Health Scopus articles Urban Health impact factor journals Urban Health Scopus journals Urban Health PubMed journals Urban Health medical journals Urban Health free journals Urban Health best journals Urban Health top journals Urban Health free medical journals Urban Health famous journals Urban Health Google Scholar indexed journals PHC articles PHC Research articles PHC review articles PHC PubMed articles PHC PubMed Central articles PHC 2023 articles PHC 2024 articles PHC Scopus articles PHC impact factor journals PHC Scopus journals PHC PubMed journals PHC medical journals PHC free journals PHC best journals PHC top journals PHC free medical journals PHC famous journals PHC Google Scholar indexed journals Social Determinants articles Social Determinants Research articles Social Determinants review articles Social Determinants PubMed articles Social Determinants PubMed Central articles Social Determinants 2023 articles Social Determinants 2024 articles Social Determinants Scopus articles Social Determinants impact factor journals Social Determinants Scopus journals Social Determinants PubMed journals Social Determinants medical journals Social Determinants free journals Social Determinants best journals Social Determinants top journals Social Determinants free medical journals Social Determinants famous journals Social Determinants Google Scholar indexed journals health articles health Research articles health review articles health PubMed articles health PubMed Central articles health 2023 articles health 2024 articles health Scopus articles health impact factor journals health Scopus journals health PubMed journals health medical journals health free journals health best journals health top journals health free medical journals health famous journals health Google Scholar indexed journals immunization articles immunization Research articles immunization review articles immunization PubMed articles immunization PubMed Central articles immunization 2023 articles immunization 2024 articles immunization Scopus articles immunization impact factor journals immunization Scopus journals immunization PubMed journals immunization medical journals immunization free journals immunization best journals immunization top journals immunization free medical journals immunization famous journals immunization Google Scholar indexed journals ecosystems articles ecosystems Research articles ecosystems review articles ecosystems PubMed articles ecosystems PubMed Central articles ecosystems 2023 articles ecosystems 2024 articles ecosystems Scopus articles ecosystems impact factor journals ecosystems Scopus journals ecosystems PubMed journals ecosystems medical journals ecosystems free journals ecosystems best journals ecosystems top journals ecosystems free medical journals ecosystems famous journals ecosystems Google Scholar indexed journals EPI articles EPI Research articles EPI review articles EPI PubMed articles EPI PubMed Central articles EPI 2023 articles EPI 2024 articles EPI Scopus articles EPI impact factor journals EPI Scopus journals EPI PubMed journals EPI medical journals EPI free journals EPI best journals EPI top journals EPI free medical journals EPI famous journals EPI Google Scholar indexed journals
Article Details
1. Background
Almost one billion people are estimated to live in urban slums globally [1]. In South Asia, slums make up a significant proportion of a country’s urban population, as illustrated by the cases of Bangladesh (55%), Nepal (54%), and India (24%). [2] As is the case in these neighbouring Asian countries, slum growth in Pakistan is being driven by accelerating rates of urbanisation. According to one estimate in 2014, 46% of the urban population in Pakistan resided in slum areas (referred to as “Katchi abadis”), which is equivalent to over 32 million people [3]. These “Katchi abadis” were initially developed as unauthorized settlements, and are constructed in less attractive city or peri urban locations such as along natural water ways or drains, or near places of employment in low income neighbourhoods [4].
A range of studies conducted in Pakistan have confirmed high prevalence of environmentally related communicable diseases and low immunisation coverage in slum like settlements [5, 6], with these outcomes being associated in other studies with low numbers of Lady Health Workers (LHWs) in slums [7], and lack of accessibility to services due to high transport costs [8]. In the slums, ethnicities and level of education have been associated with lower coverage [9], with higher coverage being associated with positive awareness of vaccines and proximity to health services [10]. Humanitarian emergencies and conflict are also drivers of internal migration in Pakistan and are contributing to clustering of urban poor populations residing in unplanned illegal settlements. In conjunction with the rapid transition to urban living, the context of decentralisation in Pakistan is contributing to the policy and planning challenge of governance and financing of public health services in these urban settings.
Given the scope of the problem of public health in the urban slums of Pakistan, government, international organisations, and civil society partnered to undertake a series of health studies between 2017 and 2019 in urban poor areas in the ten most highly populated cities of Pakistan [1], with an estimated total population of 41.04 million. The aim of this paper is to summarise the main findings of these health and social studies into a single national overview of health and social conditions and discuss the policy and planning implications of these findings for improvement of the health and immunization situation of the urban poor in Pakistan.
2. Methods
For the purpose of identifying the slum and underserved areas in these cities, the international definition of slums was applied with a slum household being defined as a group of individuals who live under the same roof that lacks one or more of the following conditions: Limited access to improved water & sanitation, weak housing structures, insufficient living area, and lack of certainty about legal ownership of the residential area [11]. For identification of “underserved” areas, the Department of Health at the Provincial level classified these according to characteristics such as poor housing, low immunisation coverage, high numbers of vaccination refusals or numbers of migrants. There were overall two main assessments, which included the urban health slum profiles and immunisation coverage surveys.
2.1 Urban slum profiles
Profiling was conducted in all 10 cities in two phases, in Karachi and Hyderabad in phase 1 in 2017 and the remaining eight cities in phase 2 in 2018 and 2019. There were four main types of assessment for the urban slum profiles. These assessments included (1) physical verification of slums and underserved areas,
- assessment of vaccination facilities and services (hereafter referred to as Expanded Program of Immunisation or “EPI” Facility Assessment Surveys),
- mapping of health resources in the union councils (UCs) [2] and finally (4) assessment of health resources in the UCs having slums or underserved areas within their urban territory. For sampling procedure, once a consolidated list of slums and underserved areas was prepared, each UC was individually visited by the survey team to identify the slum areas and to gather a group of 3-5 residents and undertake an interactive group discussion. Further details on sampling, inclusion, and exclusion criteria for selection for group discussion, variables for profiles and EPI facility assessments, methods of analysis, the study monitoring system and team structure, are all elaborated in the national profile report [12], with a summary of sampling and methods provided in Table
|
Study Types |
Sample Sizes |
# Cities |
Data and Information Collected |
|
Urban Slum Profile - Physical verification |
868 Union Councils |
10 |
The slums & underserved areas were physically verified, and social profile collected through group discussions. A provincial, District and Union Council wide list of slums was developed and used. |
|
Urban Slum Profile - EPI Facility Surveys |
422 Facilities |
8 |
EPI facilities surveyed in or near slums & underserved areas were physically assessed for availability, numbers and types of services, human resources, availability of vaccines & supplies, cold chain, waste management, water and sanitation at facility. All EPI facilities were assessed without sampling. EPI facility surveys were not conducted in two of the cities (Karachi & Hyderabad) |
|
Urban Slum Profile - Resource Mapping |
868 Union Councils |
10 |
UC maps were prepared with locations of slums, underserved areas. Health facilities were recorded through real time Geographic Information System (GIS) coordinates. The maps enable evidence-based plans for covering uncovered population. |
|
Urban Slum Profile Health Resource Assessment |
868 Union Councils 4441 Slums & Underserved Areas |
10 |
Data of health resources available at UC level in relation to facilities, human resources, availability of EPI services |
|
Immunisation Coverage Surveys |
14,531 Children 14,491 Mothers 14,467 Households |
10 |
The vaccination coverage survey was conducted for children aged 12-23 months. The survey applied the WHO cluster survey methodology) included background information on households and mothers of children |
Table 1: Summary of study types, sample sizes, and data and information collected.
2.2 Coverage surveys
After profiling of the slums as described above, it became clear there were significant gaps in both supply and demand for immunisation services. Health professionals and planners realized that information was required to assess the extent of zero dose [3], defaulter and under vaccinated children in the slums and underserved areas. A childhood vaccination coverage survey for children aged 12-23 months was conducted for children living in slums and underserved areas in the 10 mega cities according to the latest sampling methodology by World Health Organization (WHO) [13]. Survey questionnaires included physical features of the houses, economic situation of the households, profile of mothers, and the status of vaccination. The effective sampling size was determined through expected coverage and desired precision level was set at 95% Confidence
Interval (CI) as per Table B - 1, Page 118, World Health Organization (WHO) reference manual. For analysis of survey data, survey datasets for each city were merged using Microsoft Access to create a national dataset. The combined dataset was then exported to SPSS to conduct goodness-of-fit test and binary logistic regression analysis. Further details of the coverage survey methodology are elaborated in the National Coverage Survey report [14].
Ethical clearance for the studies was not sought, given that they were initiated for the purpose of internal program evaluation of the immunisation program, and for setting a baseline for program improvement for immunisation and urban primary health care. Survey teams were however provided with an orientation on the objectives of this exercise, basic concepts on healthcare and immunization services and field ethics. Information from these five survey and assessment sources were then integrated into city and province wide urban slum profiles, and thereafter into a national urban slum profile and a national coverage survey report. A key principle informing the development of these urban slum profiles is that of triangulation of data from multiple sources to provide a broader perspective of the social determinants of inequities in immunisation and health coverage. The variables and subject headings in the profiles reflect this broader perspective and are illustrated in figure 1 below.
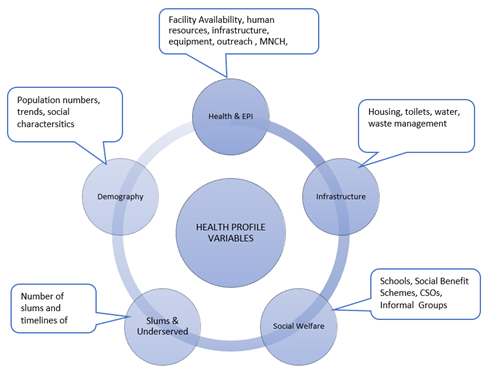
Figure 1: Summary Pakistan urban slum profile categories of analysis.
Presentation of the main findings will be presented according to the main categories outlined in figure 1.
2.3 Study limitations
A main limitation of the health profiles was that relevant local authorities did not always have an updated list of slums, which meant it was challenging to find all slums located in each UC. To manage this limitation, multiple sources such as relevant departments, key informants and CSOs were approached for the compilation of slum lists. Information on the state of various public health infrastructure in the slums such as water, sanitation and housing provide information about the frequencies of availability of supply but does not study the impact that poor quality infrastructure has on the health and well-being of slum populations. In summary, although slum listing and boundaries and survey responses are inexact, we consider that the range of survey methods, and the ability to triangulate findings from each survey method, has provided sufficient evidence on which to base conclusions regarding improved health planning and service delivery for urban slums and underserved areas.
3. Findings
3.1 Populations and types of residents
The 10 cities included in this study are the most highly populated in Pakistan. These include the two main cities of Sindh Province (Karachi and Hyderabad), the five main cities of Punjab Province (Faisalabad, Gujranwala, Lahore, Multan and Rawalpindi), Quetta in Balochistan Province, Peshawar in Khyber Pakhtunkhwa (KPT) Province, and finally the Islamabad Capital Territory.
|
TOTAL |
|
|
Total Population of 10 Cities (Census Data) |
41,049,208 |
|
Total Population of Slums in 10 Cities |
13,325,853 |
|
Total Population of Underserved Areas in 10 Cities |
6,294,743 |
|
Total Population of Slums and Underserved Areas in 10 Cities |
19,620,596 |
|
Women of Childbearing Age in Slums & Underserved Areas |
4,316,532 |
|
Under 5 Children in slums & Underserved Areas |
3,332,830 |
Table 2: Population data from urban poor areas in the 10 largest cities of Pakistan.
As illustrated by Table 2, nearly half of the urban populations are living in slums and underserved areas in the 10 cities. The size of the population residing in slums alone ranges from 6.9 million in Karachi to 273,840 in Islamabad City. Populations of slums and underserved areas are highly diverse in terms of population status (temporary or permanent), language and culture. 86% of residents of slums and underserved areas at the time of survey had been living in these locations for more than two years and are therefore referred to as permanent settlers. The highest proportion of permanent settlers is found in the slums and underserved areas of Gujranwala (92%) and Islamabad (90%). The lowest proportion of permanent settlers is found in Peshawar (75%), and the remaining population are either temporarily displaced or are of other nationalities. A major planning challenge of this city is rapid population growth, driven in part by a large influx of migrants affected by natural disasters and conflict. There are also high rates of temporary displaced in Peshawar, which are attributed to refugees who have low financial resources and who tend to settle in and around the city in squatter settlements.
The floods of 2005 also made an estimated 3.5 million homeless [15]. These migrations also contribute to high levels of ethnic and linguistic diversity as illustrated by the case of Quetta City, where the slums and underserved areas accommodates multiple ethnic and linguistic groups including Pashtuns, Baloch, Brahvi, Hazara and Punjabi.
As would be expected, households surveyed demonstrated high levels of socio-economic disadvantage. 54% (n=7873) of all households surveyed in the 10 cities rely on daily wage labour to sustain the households, and a further 56% of households (n=8075) stated that they were always or occasionally in daily income deficit. Of the 14,491 mothers surveyed, 96% (n=13,658) had no employment outside the home, and 56% (n=8075) had zero years of schooling.
As will be seen in subsequent presentation and discussion of results, this background of economic, gender and social disadvantage has important implications for the design of pro equity urban health strategy.
3.2 Slums and underserved areas-Time of establishment and legal status
The Urban Slum Profiles undertook data collection with local authorities in UCs about how long the slums had been established and their current legal or registration status.
Timelines: Slums have been growing at a comparable rate. In the five cities of Punjab Province, the growth rate of slums in four out of the five cities was above 60% between 1950 and 1990, with only Gujranwala (59%) and Peshawar (48%) having a growth rate below 60% in this period. The rapid growth rate of slum areas in Punjab Province between 1950 and 1990 demonstrates that some of the families are multigenerational slum dwellers, and the urban slum growth is also being driven by an influx of new temporary residents [4]. The recent slower growth in the number of slum areas does not equate with a decline in the absolute number of slum residents, with overall city population numbers demonstrating steady rates of population growth [16]. The projected average annual rate of change for urban population in the ten cities ranges from 2.2% in Rawalpindi to 3% in Lahore per annum between 2018 and 2030 [17].
Registration: Not being recognised or “regularised” by local authorities means these communities are less open to the benefits of State sponsored development planning for essential public health infrastructure and services such as health, education, water, and sanitation.
In five of the ten cities, more than 50% of the total number of slums have not been registered or “regularised” with local authorities. In the largest population city of Karachi, of the 986 slums in that city, just 7% (n=64) have been regularised. As an indication of the degree to which lack of registration can contribute to administrative and legal marginalisation, the urban slum health profile from Quetta City in Balochistan reports that it is not clear whether the slum populations were included in the recent 2017 census [18].
Infrastructure in slums and underserved areas Levels of socioeconomic and administrative marginalisation are reinforced by findings in surveys of the state of housing and public health infrastructure in the slums. The urban slum profiles found that highest percentage of “Kacha structures” (nonconcrete mud houses or tents) is found in the slums of Quetta (66%), while the lowest proportion of these structures being observed in Multan (9%) and Faisalabad (9%). In addition to substandard housing, the community is also exposed to risks of lack of access to safe water and sanitation. Of the 14,467 households surveyed in the coverage survey, 44% (n=6328) have access to government water supply and 59% of households (n=8598) are connected to street drains, with average number of people using one toilet being seven across the 10 cities. Overcrowding is a common feature of slum communities, and applies across the 10 cities where the average family size of households was 9, ranging from households sizes of 11 in Quetta and 10 in Peshawar, to six in three cities of Punjab Province (Multan, Lahore, Gujranwala). In Quetta City, Balochistan Province, the situation is more acute, where the survey of 1782 households found that 54% of the houses surveyed in slums areas are mud made “Kacha”(nonconcrete mud houses or tents). Assessment of the water and sanitation conditions reveal that the government water supply exists in only 27% of households (n=486) in this city. Given the exposure to these environmental risks of temporary housing, undersupply of safe water and sanitation, and household overcrowding, the survey demonstrates high rates of exposure by slum populations to communicable disease risk.
3.4 Social services and social welfare in slums and underserved areas
The urban slum profiles in ten cities collected information from local authorities and from community members on the availability of social services and networks in the slums and underserved areas. This information is essential to consider to what extent social support and networking can compensate for the forces of marginalisation described earlier in relation to the population, environmental and infrastructure characteristics of slums. The profiles found that across the ten cities, there are 1188 slums and underserved areas without schools (public or private), which represents 27% of all slums and underserved areas in the 10 cities (n=4441). This aligns with findings from the coverage survey, which found of the 14,491 mothers interviewed on the question of schooling, 56% (n=8115) had zero years of schooling, with Quetta and Peshawar having zero schooling rates of 83% and 74% respectively.
Lack of access to schooling implies lack of access to information unless communities compensate through building of strong local area communication and support networks. One way to build such communication and support networks is through the work of Civil Society Organisations. In the eight cities urban slum profiles that collected data on civil society organisations and social welfare, just 3% (n=79) of the 3124 slums and underserved areas in the eight cities had a CSO or NGO operating within them (from any sector). Seven of the eight cities have less than 5% of slums with a functioning CSO within them. Lack of CSO participation can be compensated for by formation of informal groups including health, school and Masjid committees, Jirga, Zakat, and unregistered community-based organisations. Overall, 35% (n= 1082) of the total number of slums and underserved areas (n=3114) in the eight cities report having informal groups.
Communication and social support can be also provided through public welfare such as loan and stipend schemes, social benefit cards and vocational skills schemes. Overall, just half of the slums and underserved areas in the eight cities (n=1512)) have any one of these schemes in operation. Only 2% of slums and underserved areas in the five cities of Punjab Province have welfare schemes provided by the Government in the form of loan schemes or vocational skill building schemes, and only 3% of the slums and underserved areas have welfare schemes provided by the government and private sector. In Quetta, 12% of slums have some form of public welfare scheme. These findings on social services and public welfare confirm a picture of disadvantaged communities being disconnected and isolated from the mainstream government service sector as well as from social organisation and support through a scarcity of local area formal and informal social networks.
3.5 Health and immunisation services in slums and underserved areas
Immunisation coverage in slums and underserved areas: Nationally in the sample of children (n=14531) aged 12- 23 months in slums and underserved areas, 53% (n=7754) of eligible children eligible were fully immunised (verified by record and recall). Of the remaining children, 33% (n=4792) were partially immunised and 14% (n= 1985) received zero doses of vaccines. There was a significant drop out of 27 percent from the first vaccination (BCG) of 85% coverage (n=12366) to the coverage with the fifth contact with health services for measles 1 vaccination of 58% (n=8435).
As can be observed in figure 2, even cities with comparatively higher coverage of fully immunised child such as Gujranwala (65%) and Rawalpindi (69%) had high rates of zero dose immunisation at 24% and 18% respectively, confirming that accessibility, availability or acceptance of vaccination services may be a significant problem in these areas. In Quetta City (n=1792), there are as many children fully immunised as there are who had zero dose.
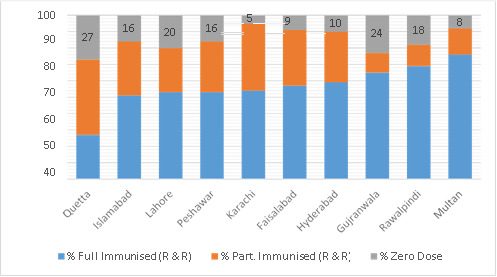
Figure 2: Immunisation coverage - fully immunised child, partially immunised child, zero dose (record/ recall).
The survey also found that 14% (n=1985) of the national sample (n=14531) had zero doses of vaccines. Table 3 compares household characteristics of zero dose and fully immunised child households.
|
Kacha Houses |
844 |
43% |
576.323 |
0.000 |
1136 |
15% |
532.721 |
0.000 |
|
Daily Wage Labour |
1256 |
63% |
106.767 |
0.000 |
3842 |
50% |
144.409 |
0.000 |
|
Daily Income Deficit |
1235 |
62% |
46.780 |
0.000 |
4062 |
53% |
69.365 |
0.000 |
|
Zero Education Level of Mothers |
1505 |
76% |
376.611 |
0.000 |
3598 |
47% |
614.171 |
0.000 |
Table 3: Comparison of household characteristics of zero dose and fully immunised child households.
The survey data indicates that the children of households who live in Kacha houses are likely to have zero doses (43%, p<0.001) and very unlikely to be fully immunised (15%, p<0.001) compared to those living in Kacha houses. Children in households with daily wage labour as the main income source has a higher chance of having zero doses (63%, p<0.001) than those in households with better sources of income. Similarly, children in households with income deficits are more likely to have zero doses as well (62%, p<0.001) compared to children in households who has enough income. Children born to mothers with zero education have a much higher likelihood of having zero doses (76%, p<0.001) and lower likelihood of being fully immunized (47%,
p<0.001) than those born to mothers who had at least 1 year of education.
Findings on the influence of education are also reflected in the data from the coverage surveys. In the national sample of 14491 mothers, a total of 67% (n=9659) stated that vaccination protects from disease, while 20% (n=2836) stated they did not know the purpose, and the final 14% (n=1996) indicated that vaccination is given for purposes other than protecting from disease. In the mothers of children of zero dose children (n=1978), 23% (n=472) stated that vaccination causes more diseases. Autonomy of decision making is also identified as an issue by 33% (n=352) mothers of zero dose children with “no family permission” as the most stated reason for the zero-dose status of their children. The response for “no family permission” as a reason for zero dose is highest in the slums and underserved areas of Peshawar (54%), Karachi (48%) and Quetta (43%).
|
S.E. |
P |
OR |
Lower 95% CI |
Upper 95% CI |
Reference Category |
|
|
Kacha Houses |
.024 |
.000 |
1.408 |
1.342 |
1.476 |
Kacha Houses (= 0) is the reference category. |
|
Daily Wage Labour |
.036 |
.001 |
1.125 |
1.048 |
1.207 |
Non-daily wage labor (= 0) is the reference category. |
|
Daily Income Deficit |
.035 |
.000 |
1.170 |
1.093 |
1.253 |
No deficit (= 0) is the reference category. |
|
Zero Education Level of Mothers |
.037 |
.000 |
1.873 |
1.741 |
2.015 |
Mother had education (= 0) is the reference category. |
Table 4: Summary of logistic regression analysis for variables predicting children not being fully immunized.
A logistic regression was performed to determine the effects of several socioeconomic factors on the immunization status of a child. The logistic regression model explained 61% of the cases. The logistic regression model was statistically significant (Chi- square 19.397, p=.013) and the indicators added significantly to the model. These factors associated with incomplete immunization status of the child were: kacha houses (OR:1.408; 95% CI:1.342-1.476), daily wage labour as household source of income (OR:1.125 95% CI:1.048-1.207), daily income deficit for the household (OR:1.170; 95% CI:1.093-1.253), and zero education for mothers (OR 1.873; CI:1.741- 2.015). The gender of the child was less significant (p=0.378) and didn’t influence the outcome of the model (OR 1.031; CI:0.964-1.103).
|
S.E. |
P |
OR |
Lower 95% CI |
Upper 95% CI |
Reference Category |
|
|
Kacha Houses |
.034 |
.000 |
1.658 |
1.550 |
1.772 |
Pakka Houses (= 0) is the reference category. |
|
Daily Wage Labour |
.053 |
.004 |
1.167 |
1.051 |
1.296 |
Non-daily wage labor (= 0) is the reference category. |
|
Daily Income Deficit |
.051 |
.001 |
1.181 |
1.068 |
1.306 |
No deficit (= 0) is the reference category. |
|
Zero Education Level of Mothers |
.060 |
.000 |
2.036 |
1.811 |
2.289 |
Mother had education (= 0) is the reference category. |
Table 5: Summary of logistic regression analysis for variables predicting children having zero-doses.
The logistic regression model for zero dose children was also significant (Chi-square 44.042, p=<.001) and explained 86% of the cases. Living in Kacha houses (OR:1.658; 95% CI:1.550-1.772), daily wage labour as household source of income (OR:1.167 95% CI:1.051-1.296), daily income deficit for the household (OR:1.181; 95% CI:1.068-1.306), and zero education for mothers (OR 2.036; CI:1.811-2.289) were all significant predictors of having zero doses.
These findings confirm that demand side factors related to the gender and social determinants of health are having an impact on the capabilities and willingness of mothers to seek out health care for their children (both boys and girls). The findings underscore the deep-rooted gender related barriers that become more profound in a high population density and low resource settings. The findings also illustrate that households of fully immunised children in slums and underserved areas are exposed to less social disadvantage, illustrating that the social gradient must be considered when planning for more equitable public services, even in slums and underserved areas.
3.6 Service availability and accessibility in slums and underserved areas
The fact that in the sample of 14531 children aged 12-23 months in the 10 cities, 85% (n=12366) had received a BCG vaccine indicates a high proportion of the eligible population are accessing immunisation services, but are not utilising the services for subsequent doses, thereby contributing to high numbers of partially immunised children. The large vaccination dropout rate raises questions about the availability and accessibility of services in these locations. Table 5 summarises findings from the EPI Facility Survey and the health resource mapping and other health profile data on health services at UC Level.
|
EPI Facility Surveys (n=422 EPI Facilities) |
|
|
EPI Facilities with Functional Refrigeration |
97% (n=409) |
|
EPI Facilities with Drinking Water |
65% (n=288) |
|
EPI Facilities with Toilets |
74% (n=306) |
|
EPI Facilities - Availability of Vaccinators |
99% (n=419) |
|
EPI Facilities with Vaccine Shortage |
12% (n=54) |
|
EPI Facilities Availability Vaccine Carriers |
98% (n=415) |
|
EPI Facilities Availability of Safety Boxes |
97% (n=418) |
|
Health Profiles (n=4441 Slums and Underserved Areas) |
|
|
Public Health Facility in Slums & Underserved Areas |
6% (n=246) |
|
EPI Facility Slums & Underserved Areas |
7% (n=342) |
|
Lady Health Worker Coverage in Slums & Underserved Areas |
35% (n=1558) |
|
Outreach in Slums & Underserved Areas |
64% (n=2862) |
Table 6 : Summary of main findings on service availability urban slum profiles Pakistan.
The data confirms that the EPI facilities in the slums and underserved areas, though short of some essential infrastructure such as water and sanitation in some locations, are reasonably equipped with vaccines and cold chain systems and supplies, and all have vaccinators. However, as outlined in Table 5, the Urban Slum Profiles found that a significant proportion of slums and underserved areas are without public health facilities (94%) and EPI facilities (93%) and are not sufficiently covered by Lady Health Workers. The problem of inadequate availability of health facilities is compounded by limited health outreach services, with outreach services operational in just 64% of the slums and underserved areas.
Gaps in availability of services are also compounded by gaps accessibility to services based on geographic distance. In the eight cities where data was collected on distance to facilities, it was found that only 7% (n=204) of 3114 slum areas had an EPI facility within 2kms. Accessibility to services is also constrained by the limited reach of Lady Health Workers (LHWs). Findings from the coverage survey found that in the sample of 14491 mothers, only 44% (n=6329) know about the work of LHWs, and only 1% of mothers (n=105) stated that the LHW provided information about vaccination. In the logistic regression model, the mother’s knowledge about the work of LHWs has a significant influence on whether the child will be fully immunized (OR:1.467; 95% CI:1.369-1.571).
The GIS mapping complements the above assessments and illustrates the undersupply of health facilities and workers in the slums and underserved areas. In one mapping example from Union Council 110 of Lahore City, 12 slum areas were identified, with just one fixed EPI facility with two vaccinators and seven LHWs for an overall UC population of 85,607. The GIS and health resource mapping confirmed that, even though EPI facilities are reasonably well equipped, there are insufficient facilities, outreach services and health workers to ensure that services are available to the population. These shortages of service availability, coupled with limited social support, networking and information dissemination described in earlier sections, illustrates the size of the challenge in expanding health coverage in the slums and underserved areas of Pakistan.
4. Discussion
4.1 Summary of main findings
The Urban Health Slum Profiles was conducted and completed in Pakistan between 2017 and 2019 in 10 cities have confirmed that poverty and poor health is an outcome of low investment in both public health infrastructure as well as in essential health and educational services. The social marginalisation associated with low levels of development financing is being compounded by lack of social connections and community support in local areas, major gaps in education and health services, as well as by lack of legal recognition of slums at higher levels of government. The health disadvantage of the urban poor communities is being reinforced by via pathways of low incomes, poor environmental conditions, educational and gender disparities, and health service availability inequities, all of which inhibit the capacity of families to protect themselves from preventable disease, and to know about, access and use public health services. This is locking families and communities into multi-generational cycles of socio-economic, health and educational disadvantage. The trap of multi-generational slum dwelling is reinforced by evidence of the historical timeline of slum development, most of which were established between 1950 and 1990, and which have been sustained to the current day. The rapid growth of the cities of Pakistan driven by migration, conflict, and natural disasters, coupled with the ongoing threats posed by polio outbreaks [19] and emergence of COVID 19 pandemic disease [20], confirms that the health of the urban poor in Pakistan is an urgent national and international priority.
4.2 Social sector and health policy and planning implications
The social determinants of health: The Pakistan National Demographic and Health Survey (PDHS-2018) found that 71% of urban children received all basic vaccines [21]. This compares with just 53% of the urban poor children that were fully immunised (record and recall) in 10 cities surveyed in this study. The urban health slum profiles therefore raise major questions as to how policy makers and planners at all levels of the decentralised administrative system in Pakistan respond to the overwhelming evidence of the impact of social and economic disadvantage on the health and social well- being of the urban Studies published in Pakistan identify that proximity to facilities, positive awareness of vaccines, other Primary Health Care (PHC) services [10] and availability of LHWs [7] are essential requirements for higher coverage and are in all probability a necessary condition for achieving polio eradication. In addition to these health service determinants, evidence from these Urban Slum profiles demonstrates that addressing the root causes of health and social inequities requires more attention on the political and social structures that sustain such inequities over generations [22].
As illustrated in the conceptual framework in figure 1, and further demonstrated by the evidence of the urban slum health profiles, health inequities are being influenced by forces of migration, socio economic status, availability of public health infrastructure, educational access and attainment, gender perspectives and finally legal recognition of slums by authorities, all of which become amplified in population dense urban poor settings. Given the significant gaps in socially determined access to health care and education services, “legal recognition” and rights to security of tenure could be extended to recognition of rights to health and education for slum dwellers and underserved populations [23]. The National Health Vision recognises the potential of rapid urbanisation to aggravate the current health situation, and that lower income groups are more likely to have lower coverage of health services, and recommends “ acting upon the social determinants within the health and social sectors, if a wider impact is to be achieved [24]”.
The Urban Slum Profiles recommend health sector agencies address the wider social determinants of health through initiatives such as advocating for improvements to female literacy and partnering with environmental agencies to consider joint actions on the environmental determinants of health. Given the persistence of social and environmental conditions in the slums, which will require long term strategic planning, short to medium term actions will also be required to relieve health and social conditions in the slums, such as improved operational planning and community engagement. Evidence of lack of social connections and capital in the slum communities also provides a case for strengthening partnerships with civil and community organisations to improve dissemination of health knowledge to families and community leaders. Building community partnerships and engagement mechanisms can reinforce the “neighbourhood effects” of slum dwelling, where densely populated communities who share a common set of environmental, health and social risks, also have the potential to rapidly share the effects of beneficial interventions [25]. Developing community engagement strategy will also assist responding to the challenge of zero-dose children and other aspects of low health care facility utilisation, and assist polio eradication efforts by addressing ethnic disparities in health care [9], as well as through expanding the role of LHWs to build a bridge between communities and the PHC system [26].
Urban health services planning: Despite low coverage and associated disease outbreak challenges, the Urban Health Slum Profiles provides a window of opportunity to improve the health and social conditions of the urban poor. The coverage data, resource and GIS mapping of UCs, combined with updated detailed listing of slums and underserved areas in urban areas across Pakistan, provides a baseline to develop evidence-based health coverage and costed operational micro-plans. The identification of gaps in the provision of wider PHC services, points to a policy and planning imperative to expand the range of services of the population beyond vaccination to also cover needs in the areas of reproductive health and nutrition.
This of course has major implications for public health infrastructure and human resource investment, the two issues of which cannot be resolved exclusively through operational micro-planning as it requires solid evidence base and political advocacy to prioritize government resources for addressing socio economic inequities. Resolution of the issue of health inequities in slums is not simply a technical question but requires high level advocacy and strategic planning to mobilise the political will and resources to address health inequities. The question remains as to how such political and social organisation and commitment will be mobilised to translate research findings into policy and practice.
Governance and accountability for urban health: These questions of governance and accountability for urban health aligns with the findings of a review of 30 successful urban development programs across Asia. This review found that the critical ingredients for implementation success were national policy triggers, and sub national state and local government leadership in innovation [27]. A recent implementation of a demand generation strategy for Improving equity and coverage in the slums of Lahore resulted in a reduction in zero-dose immunisation in children from 19% to 5%. These results were attributed to successful partnerships between health workers, Provincial and District Authorities, and community elders and organisations in supporting social mobilisation, planning and monitoring, which illustrates the value in building social networks and partnerships locally to improve utilisation of services [28].
The recommendations in the health profiles to promote actions on registration and development of health coverage plans, as well as developing partnerships and engagement mechanisms in
communities, may be important initial steps in better engaging political and community actors in leadership for both health and social change. This conclusion reinforces the observation that governance and accountability are not only functions of ‘government’, but are also functions of civil and private agencies, religious leaders and communities and families through ‘social accountability’ community engagement strategies. Development of governance and accountability mechanisms, along with functional community health networks could be enabled through research and development of a coverage plan for health in the slums, reinforced by such an accountability framework, that clearly sets out the roles of different stakeholders in financing, advocacy, implementation and evaluation [27]. This research should also provide the evidence base for development of an urban health strategy, resourced through an urban health coordination mechanism to oversee development and implementation of strategic and operational plans for improved health of the urban poor.
5. Conclusions
The urban slum health profiles and coverage surveys demonstrate that the health and social conditions of the urban poor in the 10 most populated cities in Pakistan are exposing communities to multiple deprivations and high levels of public health risk. The limited access to public services is expressed clearly in the shortage of schools and health facilities in the slums, poor standards of public health infrastructure, high prevalence of zero-dose children for immunisation, and inadequate human resources to support provision of a minimum essential level of public health services. Action on the social determinants of health, health services planning, and development of governmental and social accountability frameworks for public service provision provide a window of opportunity for alleviating the health and social conditions of the urban poor. The development of a health services coverage plan, urban health strategy and related PHC integrated micro-plans are recommended to be the next steps in translating these research findings into policy and practice, and to take further steps towards attaining a continuum of care to support a universal health coverage vision. Given that nearly half of the population in these 10 cities reside in slums and underserved areas, the development and implementation of a coordinated and integrated urban health strategy will not only benefit the health of the urban poor, but will also serve to accelerate the overall economic, health and social development of Pakistan.
Ethics Approval and Consent to Participate Approval was not sought from an institutional ethics committee, as the studies were part of formal program evaluation.
Consent for Publication
Not Applicable.
Availability of Data and Materials
Refer to references [12] and [14].
Competing Interests
The authors have no competing interests.
Funding
This program of research was co funded through National Immunization Support Project (NISP)/Multi donor trust funds (MDTF), Gavi, the Vaccine Alliance and the EPI Program Pakistan.
Authors' Contributions
KA was the technical lead for the urban slums profiling and study and provided overall coordination, concept development, capacity building, training and monitoring of the third party involved in implementation. JG supported analysis of findings and drafted the original paper. LH undertook data Collection/ implementation of the study. IA supported data collection and monitoring in the field. SF supported review of the paper and DB undertook data analysis. AS, SY, YC and HB supported oversight and coordination with provincial and districts counterparts Supported funding arrangement.
Acknowledgements
We hereby acknowledge the substantial efforts undertaken by the following Organisations in facilitating implementation of the urban health studies. These include the management and staff of the Federal and Provincial EPI Programs as well as the District Health Offices in the ten mega cities and for the technical advice provided by the staff of the World Health Organization and Civil Society for Human and Institutional Development Program (CHIP). We would also extend our acknowledgements to UNICEF country office (Immunization team) and sub offices for their technical support, coordination and monitoring during implementation of this research, as well as to Regional and Headquarter technical staff especially
Alyssa Sharkey, for their supervision and review of this paper. We also extend our thanks to Gavi- the vaccine Alliance for the commitments to improvements in vaccination services in Pakistan. Most of all, we would like to extend our appreciation to the many field researchers, health workers, managers and community members who participated in our field research.
References
- Sustainable Urban Development (2020).
- UN HABITAT. United Nations System Data Catalogue UN-HABITAT: Proportion of urban population living in slum (1990-2014).
- UNHABITAT United Nations System Data Catalogue UN-HABITAT: Proportion of urban population living in slum (1990-2014).
- UNICEF Profiling of Urban/Peri-Urban Slums of Karachi & Hyderabad, Pakistan UNICEF Country Office Pakistan (2019).
- Noor S, Fatima M, Sehrish S. Unsustainable environment and prevalence of diseases in slums: A case of Bahawalpur, Pakistan. International Research Journal of Environment Sciences 3 (2014): 74-82.
- Adil M, Zubair M, Alam A, et al. Knowledge of mothers about children’s immunization status in the urban areas of Islamabad. Rawal Medical Journal 34 (2009): 33-35.
- Government of Pakistan Comprehensive Multi Year Plan for Immunisation (2014- 2018).
- Majrooh M, Hasnain S, Akram J, et al. Accessibility of antenatal services at primary healthcare facilities in Punjab, JPMA. The Journal of the Pakistan Medical Association 63 (2013): S60-S66.
- Siddiqui N, Owais A, Agha A, et al. Ethnic disparities in routine immunization coverage: A reason for persistent poliovirus circulation in Karachi, Pakistan? Asia Pac J Public Health 26 (2014): 67-76.
- Cockcroft A, Andersson N, Omer K, et One size does not fit all: Local determinants of measles vaccination in four districts of Pakistan. BMC International Health and Human Rights (2009): S4.
- UN Habitat. The Challenge of Slums: Global Report on Human Settlements (2010):
- Profiles of Slums/Underserved Areas of 8 Largest Cities of Pakistan (2020).
- World Health Organisation Immunisation Cluster Survey Guidelines WHO GVA (2018).
- Coverage Survey in Slums/Underserved Areas of 10 Largest Cities of Pakistan (2020).
- Government of Pakistan Ministry of Climate Change, Islamabad, Pakistan National Report of Pakistan for HABITAT III (2015).
- Government of Pakistan. Pakistan Population Bureau of Statistics Population Size and Growth of Major Cities (2020).
- United Nations. The Worlds Cities in Data Booklet (2018).
- CHIP Quetta City Balochistan Urban Slum Profile 2019, UNICEF Country Office Islamabad
- Pakistan Polio Eradication Programme Polio Cases in Provinces (2020).
- Pakistan Ministry of National Health Services, Regulation and Coordination Govt. Pakistan National Action Plan for Preparedness and Response to Corona Virus Disease (Covid-19) Pakistan (2020).
- National Institute of Population Studies Islamabad, Pakistan. The DHS Program ICF Rockville, Maryland, USA Demographic and Health Survey, Pakistan (2018).
- Plamondon et al. Connecting knowledge with action for health equity: a critical interpretive synthesis of promising practices International Journal for Equity in Health 18 (2019):
- Forman L. What do human rights bring to discussions of power and politics in health policy and systems?, Global Public Health 14 (2019): 489-502.
- Government of Pakistan National Health Vision (2016-2025).
- Lilford R, Oyinlola Oyebode, David Satterthwaite, et al. Improving the health and welfare of people who live in slums Lancet 389 (2017).
- Jalal S. The lady health worker program in Pakistan—a commentaryEuropean Journal of Public Health 21 (2011): 143-144.
- Xuemei Bai, Brian Roberts, Jing Chen. Urban Sustainability Innovation in Asia: patterns and pathways. Environmental Science and Policy 13 (2010): 312-325.
- Prototype on Demand Generation for Improving Equity & Coverage in Slums of Lahore. UNICEF Country Office Pakistan (2019).
