Gross Trunnion Failure in Total Hip Arthroplasty: A Case Study and Review Article
Article Information
Johannes M van der Merwe1*, Jefferson Scott2
1Adult Reconstruction, Orthopaedic Surgery, University of Saskatchewan, Saskatoon, Saskatchewan, Canada
2Department of Orthopaedic Surgery, University of Saskatchewan, Saskatoon, Saskatchewan, Canada
*Corresponding Author: Johannes M van der Merwe, Adult Reconstruction, Orthopaedic Surgery, University of Saskatchewan, Saskatoon, Saskatchewan, Canada.
Received: 28 March 2022; Accepted: 13 April 2022; Published: 22 April 2022
Citation: Johannes M van der Merwe, Jefferson Scott. Gross Trunnion failure in Total hip arthroplasty: A Case study and review article. Archives of Clinical and Medical Case Reports 6 (2022): 286-297.
View / Download Pdf Share at FacebookKeywords
Total Hip Arthroplasty; Trunnionosis; Junctional interface; T-cells
Total Hip Arthroplasty articles; Trunnionosis articles; Junctional interface articles; T-cells articles
Total Hip Arthroplasty articles Total Hip Arthroplasty Research articles Total Hip Arthroplasty review articles Total Hip Arthroplasty PubMed articles Total Hip Arthroplasty PubMed Central articles Total Hip Arthroplasty 2023 articles Total Hip Arthroplasty 2024 articles Total Hip Arthroplasty Scopus articles Total Hip Arthroplasty impact factor journals Total Hip Arthroplasty Scopus journals Total Hip Arthroplasty PubMed journals Total Hip Arthroplasty medical journals Total Hip Arthroplasty free journals Total Hip Arthroplasty best journals Total Hip Arthroplasty top journals Total Hip Arthroplasty free medical journals Total Hip Arthroplasty famous journals Total Hip Arthroplasty Google Scholar indexed journals COVID-19 articles COVID-19 Research articles COVID-19 review articles COVID-19 PubMed articles COVID-19 PubMed Central articles COVID-19 2023 articles COVID-19 2024 articles COVID-19 Scopus articles COVID-19 impact factor journals COVID-19 Scopus journals COVID-19 PubMed journals COVID-19 medical journals COVID-19 free journals COVID-19 best journals COVID-19 top journals COVID-19 free medical journals COVID-19 famous journals COVID-19 Google Scholar indexed journals Arthroplasty articles Arthroplasty Research articles Arthroplasty review articles Arthroplasty PubMed articles Arthroplasty PubMed Central articles Arthroplasty 2023 articles Arthroplasty 2024 articles Arthroplasty Scopus articles Arthroplasty impact factor journals Arthroplasty Scopus journals Arthroplasty PubMed journals Arthroplasty medical journals Arthroplasty free journals Arthroplasty best journals Arthroplasty top journals Arthroplasty free medical journals Arthroplasty famous journals Arthroplasty Google Scholar indexed journals Trunnionosis articles Trunnionosis Research articles Trunnionosis review articles Trunnionosis PubMed articles Trunnionosis PubMed Central articles Trunnionosis 2023 articles Trunnionosis 2024 articles Trunnionosis Scopus articles Trunnionosis impact factor journals Trunnionosis Scopus journals Trunnionosis PubMed journals Trunnionosis medical journals Trunnionosis free journals Trunnionosis best journals Trunnionosis top journals Trunnionosis free medical journals Trunnionosis famous journals Trunnionosis Google Scholar indexed journals Ultra Sound articles Ultra Sound Research articles Ultra Sound review articles Ultra Sound PubMed articles Ultra Sound PubMed Central articles Ultra Sound 2023 articles Ultra Sound 2024 articles Ultra Sound Scopus articles Ultra Sound impact factor journals Ultra Sound Scopus journals Ultra Sound PubMed journals Ultra Sound medical journals Ultra Sound free journals Ultra Sound best journals Ultra Sound top journals Ultra Sound free medical journals Ultra Sound famous journals Ultra Sound Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals Radiology articles Radiology Research articles Radiology review articles Radiology PubMed articles Radiology PubMed Central articles Radiology 2023 articles Radiology 2024 articles Radiology Scopus articles Radiology impact factor journals Radiology Scopus journals Radiology PubMed journals Radiology medical journals Radiology free journals Radiology best journals Radiology top journals Radiology free medical journals Radiology famous journals Radiology Google Scholar indexed journals Syndrome articles Syndrome Research articles Syndrome review articles Syndrome PubMed articles Syndrome PubMed Central articles Syndrome 2023 articles Syndrome 2024 articles Syndrome Scopus articles Syndrome impact factor journals Syndrome Scopus journals Syndrome PubMed journals Syndrome medical journals Syndrome free journals Syndrome best journals Syndrome top journals Syndrome free medical journals Syndrome famous journals Syndrome Google Scholar indexed journals T-cells articles T-cells Research articles T-cells review articles T-cells PubMed articles T-cells PubMed Central articles T-cells 2023 articles T-cells 2024 articles T-cells Scopus articles T-cells impact factor journals T-cells Scopus journals T-cells PubMed journals T-cells medical journals T-cells free journals T-cells best journals T-cells top journals T-cells free medical journals T-cells famous journals T-cells Google Scholar indexed journals
Article Details
1. Introduction
Total Hip Arthroplasty (THA) has been a foundational tenant in orthopedic reconstructive surgery for decades. Design improvements have contributed to improved outcomes, allowing for reproducibility and longevity with 10 year follow up of survivorship between 92% - 100% [1]. Modularity is a primary example of such a design improvement. Currently most primary THA systems manufacture and package femoral heads and stems separately, to be later assembled intraoperatively. This allows for flexibility in adjustments performed by the surgeon both pre-operatively (via templating) and/or intraoperatively. In light of this, modularity has contributed to benefits by decreasing inventory, reducing revision times, and creating more natural hip biomechanics through ease of adjustments in off-sets, limb-length discrepancies, and soft tissue tensioning [2]. The Morse taper design is a successful and widely used system for achieving modularity between the femoral head and the neck [3]. From an engineering standpoint, the design is simple but remarkably effective, using the principle of a cone fitting within a cone, thus allowing stable fixation through circumferential compression of the slightly smaller walls of the bore (female taper of the femoral head) and the trunnion (male taper on the femoral stem) when driven into the femoral head during impaction [3]. Modularity, in its application to THA, is not without complications. The circumferential fit within the Morse taper can potentially have small microscopic gaps between the trunnion and bore, subjecting the interface to a phenomenon known as Mechanically Assisted Crevice Corrosion (MACC) [4, 5]. Corrosive damage at the modular interface, although not completely understood, is likely multifactorial. Firstly, there is micromotion with cyclic loading, a mechanical corrosion known as fretting. Additionally, a physiochemical alteration of the metal surface, such as break down of the protective oxide layers, is a localized occurrence of damage known as crevice corrosion. And finally, there is electrochemical dissolution from the reaction between dissimilar metals (cobalt chromium alloy [CoCr] for the femoral head, and titanium alloy [Ti-6Al-4V] for the femoral stem) is known as galvanic corrosion [4-8]. This occurrence of wear and corrosion at the modular interface is, by definition, trunnionosis [9]. Trunnionosis and wear debris in the setting of Metal On Metal (MoM) articulations has been well documented in the literature. The Incidence of Metal-on-Polyethylene is estimated to be 0.032% to 2% of patients with a total hip replacement [9, 12-15]. As our level of knowledge around it grows, so does the incidence of cases, suggesting there has historically been a potential under diagnosis/reporting of this phenomenon in MoP articulations [9].
Continued wear and corrosion at the modular interface can perpetuate leading to destruction of soft tissues surrounding a total joint arthroplasty. Over time the corrosive process can break down the metal alloys within the femoral head and neck modular interface causing visible, and profound deformity at the junctional interface, eventually resulting in complete dissociation otherwise known as Gross Trunnion Failure (GTF) [2, 16, 17]. GTF is considerably rare, the incidence of this is currently unknown due to the sparsity of literature around this phenomenon. A recent systematic review reported only 46 cases documented in the literature (published in case series or case reports) to date [5]. Up until recently GTF was unheard of outside the context of traumatic events such as direct trauma to the hip, or multiple dislocations/reductions leading to direct femoral head distraction at the edge of the acetabular cup upon reduction. The mechanisms leading to non-traumatic GTF are most certainly multifactorial. However, factors associated with a higher risk can be broken into three broad categories: component related, surgical/surgeon related and patient related [6, 9, 18]. Patient-related factors include male gender and high Body Mass Index (BMI). Component-related factors include stem design, high-offset implants, head-neck angle, femoral head diameter, and metal alloys. Surgical-related factors include damage to the head-neck surfaces and inappropriate surgical technique [9, 18].
2. Case Study
Mrs. FT is a 76 year old female who underwent staged bilateral total hip arthroplasties for osteoarthritis. Written and verbal consent was obtained from Mrs FT. This study has been reported in line with the SCARE criteria [38]. The left THA was placed in September 2009, and the right was performed in March 2010. She had an uncomplicated course following the hip arthroplasties and both healed well without any signs of infection or complications. Five months prior to GTF of the right hip she developed a “clicking” and “grinding” sensation in the affected hip. This was initially evident when she ascended or descended stairs but became more frequent over the subsequent months, with symptoms brought on by walking or simple twisting motions. Pain and difficulty ambulating followed with increasing severity. Initially the pain was bearable and controlled with intermittent Tylenol use, however it rapidly increased to the point that she was unable to perform activities of daily living. She denied constitutional symptoms and didn’t have any infections leading up to GTF. FT had a known diagnosis of Type 2 Diabetes Mellitis, which was diagnosed in 2018. Her HBA1C was elevated at 8.5. Additionally, she was also being treated for atrial fibrillation, hypothyroidism, and hypertension. Previous surgical interventions consisted of; hysterectomy, cholecystectomy, tubal ligation and dilatation and curettage. She had no allergies and denied a smoking or alcohol history on physical examination she, had a negative Trendelenburg sign, but ambulated with an antalgic gait favouring the right hip. Furthermore, there was a new leg length discrepancy, with the right shorter than the left, along with significant limitations in her right hip’s range of motion secondary to pain. Both lower extremities were neurovascularly intact. Radiographs demonstrated an oblique angle between the femoral head and the trunnion as well as faint radiodensities in the capsule surrounding the total hip arthroplasty (see figure 1). 4 weeks later, CT-scan and x-rays clearly demonstrated the femoral head disengaged from the trunnion and eroding at the superior acetabular rim (see figure 2 and 3). Serological markers for infection were negative (CRP < 10 and ESR < 30). Fibrinogen levels were 3.63 g/l. Cobalt levels were 6.5 PPB and Chromium levels were 4.1 PPB.

Figure 1: Right total hip arthroplasty with impending GTF demonstrating an oblique angle between the femoral head and the trunnion (narrow arrow); Faint radiodensities can be seen around the hip (three larger arrows).
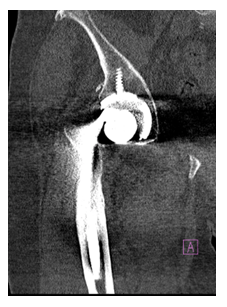
Figure 2: The femoral stem is seen disengaged from the trunnion and is seen between the femoral head and the acetabular rim.
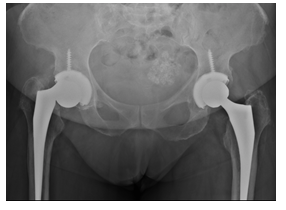
Figure 3: Radiographs demonstrating disengagement of the femoral head from the trunnion.
A revision of the hip was planned in an urgent manner. A posterolateral approach was used. Dark coloured fluid was present once we incised the hip capsule. The synovium was black stained (figure 4). Five intraoperative samples were obtained revealing a negative gram stain. Closed spaced cultures did not grow any anaerobic or aerobic organisms after 5 days. Furthermore, there was no fungal growth after 30 days, direct fluorescent stain was negative for acid fast bacilli, and mycobacterium cultures also showed no proliferation. Pathology from the synovial tissue demonstrated chronic inflammatory infiltrate with no evidence of aberrant lymphoid population. The lymphoid population consisted of follicular hyperplasia with primary and incipient lymphoid follicles. T-cells were unremarkable and plasma cells were scant and polytypic. Intraoperatively, the femoral head was found to be disengaged from the stem (figure 4), along with gross damage to the femoral trunnion (figure 6). The trunnion also damaged the superolateral aspect of the acetabular component and the locking mechanism (figure 5), allowing an effortless extraction of the liner. Due to the trunnion damage the femoral stem was successfully removed through an endofemoral approach. The acetabulum was deemed to be ingrown in a satisfactory position. Considering the locking mechanism was disrupted the decision was made to cement a liner in place, taking care to restore the offset and the appropriate anteversion. A femoral stem was cemented in 15 degrees of anteversion. A 36mm diameter ceramic femoral head was carefully impacted.

Figure 4: Black discoloration due to metal debris. Arrow demonstrates the worn polyethylene liner and acetabular rim
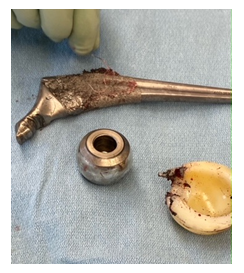
Figure 5: All the components are extracted and demonstrates the “bird beak” appearance of the trunnion as well as the worn polyethylene liner and black discoloration of the femoral head.

Figure 6: A close view of the “bird beak” appearance of the femoral trunnion.
3. Discussion
Gross Trunnion Failure (GTF) is defined as considerable corrosion at the head neck junction of a total hip arthroplasty that can be visually seen and can lead to dissociation or fracture between the head and neck interface [2,5]. This is a devastating complication because it is always associated with significant morbidity and revision surgery. Although the exact etiology of GTF is still unknown, two theories have been proposed. The first includes abrasive wear from a loose trunnion taper inside the female taper of the femoral head. The second includes, the end stage of Mechanically Assisted Crevice Corrosion (MACC) of an initially well-fixed modular junction [19]. Gradual loss of material due to MACC could lead to loosening of the modular junction with subsequent abrasive wear and potentially GTF. Modularity in total hip arthroplasty allows the surgeon to modify intraoperatively the femoral head size, offset and material composition, to increase stability and adjust length. The femoral head-trunnion connection relies on a cold-weld between the two components which prevents micromotion during movement of the hip. Theoretically, multiple factors can negatively influence the friction fit: the impaction force, larger head size and/or trunnion debris (fat, blood).
3.1. Impaction force
Danoff et al. and Pennock et al [20, 21] both concluded that the single most important factor that determines pull off force of the femoral head is the impaction force. One study proposed that the impaction strength needed to obtain the best pull off force is equivalent to the force required to broach the canal [20]. Rehmer et al. [22] quantifies the impaction force of 4 kN needed to obtain sufficient taper fixation in all bearing conditions. The surgeon should use a metal hammer on a metal impactor with a firm plastic tip keeping in mind it is important that the axis of impaction is in line with the axis of the taper. Off axis blows impede the force needed to seat the femoral head on the trunnion [21].
3.2. Multiple strikes at impaction
With regard to this controversial topic, Danoff et al [20] concluded that multiple strikes do not increase pull off strength, while Pennock et al [21] demonstrated an increase in pull off strength with multiple strikes. Rehmer et al. [22] concluded that a single blow is sufficient, however, if multiple impactions were administered, it should be done consecutively and with increasing force. In light of this, they both agreed that the first strike contributed to 90% of the pull off force. Certain prostheses did not see an additive effect after 2 consecutive hits. Both studies concluded that multiple blows of varying force do not increase pull off strength, and that the strongest impaction force contributes to the most pull off strength.
3.3. Taper conditions
Dry versus wet conditions (serum/water) influence taper strength. One study [21] showed that wet conditions (water/serum) changed mechanical strength of the taper by 50%. Taper design influenced if the strength was increased or decreased. Some tapers demonstrated a significant increase in pull off force with wet conditions while other demonstrated the opposite. Importantly, dry conditions when impacting the femoral head on the trunnion, delivers consistent taper strength with all the tested prosthesis [21].
3.4. Femoral offset
Danoff et al. found that increased femoral offset did not influence pull-off force [20]. Whilst pull off force might not be influenced; the larger offset can theoretically increase torsional forces on the head neck junction which can lead to accelerated fretting corrosion. Additionally, there is an association between GTF and femoral stems with a high offset femoral neck angle (127-degree stems) and larger femoral neck offsets [19]. Similarly, we found this is also demonstrated when we only include case studies looking at the Accolade stem. Eighty six percent of the 45 cases included had an offset equal or larger than 4 mm (see table 1), while twenty percent of the 45 cases had an offset equal or larger than 8mm.
3.5. Femoral head size
Larger femoral heads were introduced to decrease dislocation rates by allowing wider impingement-free range of motion. Del Baso et al. [23] however, demonstrated in their retrieval analysis study that larger femoral heads (>=32) and longer necks (>5mm) lead to increased fretting at the head neck junction. This was echoed by Bansal et al. [5] who demonstrated that 90% of their cases with GTF had a head size of >=36 and 79.5% had a neck length of >=5mm. Larger femoral heads lead to larger torsional forces. Similarly, longer femoral heads lead to an increase in the distance between the femoral head engagement area and the center of the femoral head. This can lead to an increased head-neck moment arm which can lead to increased fretting. The combination of increased neck length and larger heads can lead to increased fretting [23]. Other studies also demonstrated increased fretting and corrosion associated with larger femoral heads [24,25,26,27]. We also demonstrated an association of larger femoral heads and GTF looking only at the Accolade stems (see table 1). 93% percent of GTF was seen with a head size equal or larger than 36mm. Only 13% of those cases had a head size similar or larger than 40mm. Conversely, other studies demonstrated no association between larger femoral heads and fretting or corrosion [28,29]. Therefore, more studies are needed to investigate if larger femoral heads do increase the risk for GTF.
3.6. Taper design
Trunnions have become shorter and thinner, to increase impingement-free range of motion. The short trunnion causes the base to sit inside the female taper. The base has been shown to have significantly greater corrosion scores, mechanical loading and torque [24], It is controversial if the shorter thinner trunnions leads to the aforementioned complications with multiple studies demonstrating conflicting results confirming and refuting it [30, 31, 32]. Therefore, there are inconclusive evidence regarding trunnion design and increased fretting.
3.7. Increased implantation time
Most of the case series demonstrated that the stems have been implanted for at least 7-9 years before failure occurred [5, 19, 33]. This was a similar finding looking only at GTF associated with the Accolade stem. We found the mean time to revision to be 7.3 years (range: 4 years 7 months to 12 years) (see table 1). The median age at time of revision was 68.7 years (range 49 – 88) (see table 1). A recent meta-analysis concluded that the mean age at the time of the index procedure was slightly lower at 61.89 years (41-80), and agreed that the mean time for revision surgery to occur after the index procedure was 8.24 years (4.7-14 years) [5].
3.8. Male sex, BMI
Ko et al. [17] among others have commented that in their case study the combination of increased height, BMI, higher activity levels and male sex did increase the risk for gross trunnion failure [5,17]. In our review of GTF associated with the Accolade stem we concluded that 88.9% of cases were male. Bansal et al. [5] found that 91.3% were male in a meta-analysis looking at 13 studies with a combined total of 46 patients. Interestingly we found that 14.6% of cases had a BMI between 18.5-25. 41.1% of cases were overweight with a BMI between 25.1 -29.9. Thirty two percent of cases had a BMI between 30-39.9 and only 9.8% of cases had a BMI larger than 40. We found that 85.4% of cases with GTF had an increased BMI (>24.9) (see table 1). This was similar in a study by Urish et al. [19] who did see a statistical difference in mean BMI between patients undergoing revisions for GTF (Mean BMI -31.8 +-8 kg/M2) and taper corrosion alone (Mean BMI 26.2 +-4.2 Kg/M2).
3.9. Alloys
The Accolade 1 stem has a great overall survivorship with only 3.64% of stems revised since its introduction in 2003 [33]. This stem has demonstrated some failures in the past several years when used in conjunction with the LFIT V40 or MITCH CoCr heads [33]. Stryker and the Therapeutic Goods Administration recalled The MITCH heads in 2012 and the LFIT heads in 2016 due to higher-than-expected rates of revision. The Young’s Modulus (measure of stiffness of a solid material) of the Accolade 1 stem was 70 GPa (compared to conventional titanium alloys with a modulus of 110 GPa) while the modulus was rated as 210 GPa for the LFIT and Mitch CoCr heads. This mismatch between the stiffness and alloy composition can lead to accelerated galvanic and fretting corrosion [33]. In 2011 the Accolade 1 stem (Ti-12Mo-6Zr-2Fe) has been revised to a stronger titanium alloy (Ti-6Al-4V). GTF is not only associated with the Accolade 1 stem but cases were also reported with the Accolade TMZF, Accolade TMZF Plus, Biomet TaperLoc, DePuy Ultima, Harris Hip stem, Zimmer ML Taper and Zimmer Porous Coated Titanium stem [5].
On the other hand, increasing stiffness should be done cautiously seeing that by increasing stiffness of the femoral component by using CoCr neck tapers do bring about their own concerns. There is lower fixation capacity with CoCr – CoCr tapers compared to CoCr -Ti tapers or Ti -ceramic couplings [22]. Urish et al [19] found elevated serum Cobalt and Chromium levels in 80% of their 25 patients with GTF. The mean Cobalt levels were 8.9+-8.2 ug/L compared to Chromium levels of 4.4+-3.3ug/L. They concluded that the ratio of Cobalt compared to Chromium is 2.5 in GTF, compared to the ratio of 4.9 in patients with head neck corrosion alone. This was similar in the study by Bansal et al. 5 who found mean serum Cobalt levels of 9.36ug/L (0.5 – 33.6) and mean serum Chromium levels of 4ug/L. Intraoperative findings: Bansal et al. [5] found metallosis in 93.3% of cases, 47.7% had black/brown synovial fluid and 40.9% had synovial hypertrophy. They also noted that pseudotumor formation and abductor muscle involvewas seen in a lot of cases. This certainly complicates revision surgery with higher morbidity
3.10. Proposed evaluation
Early detection may be difficult because patients may not present with symptoms for a long duration before catastrophic failure occurs. Therefore, surgeons should be vigilant in monitoring patients at risk. Patients with the Accolade 1 stem fitted with a LFIT and MITCH CoCr head should be carefully monitored. This is particularly important in young males, increased BMI, higher offset stems, longer femoral neck or implantation for at least 7-9 years. This can be achieved clinically and radiographically. Clinically, patients with new onset pain or difficulty in walking should be assessed urgently [5]. Also, symptoms of clicking, clunking or popping are commonly noted in GTF. Serum markers (CRP and ESR) should be obtained routinely to rule out periprosthetic joint infection. Radiographs should be obtained annually and scrutinized for findings of GTF. Large radiolucent fluid collections can be seen on radiographs. Faint radiodensities can be seen around the hip capsule as well as metal debris. Impending GTF is difficult to diagnose on radiographs. Radiographs should be analysed and slight oblique angle between the femoral head and the trunnion should raise suspicion of impending failure. MARS MRI should only be obtained as an adjunct if not clear on physical examination and radiographic assessment. Findings on MRI will be similar than findings of ALTR. This includes cystic lesions and fluid collections. Metal ions should only be used as an adjunct, or in research settings, and not solely in decision making regarding trunnionosis. If they are performed the trend of metal ions might be more useful for interpretation than the individual values at one point in time. Also, the usual reference numbers used (7PPB) in MoM articulations is not applicable to MoP articulations. The ratio of CoCr should be considered as well when obtaining these investigations. Hip aspirates can be obtained to rule out infection preoperatively. If the aspirate is black then it can be an indication of GTF or impending failure. In these cases, the surgeon should plan to revise the femoral stem as well. Once gross trunnion failure is diagnosed the hip should be revised. This should be performed at a tertiary center. The trunnion should be inspected and if it is intact without significant wear, the stem can be left alone if solidly fixed. Any corrosion should be cleaned off. A different alloy femoral head should be used (ceramic femoral head with a titanium sleeve). If the trunnion is severely damaged then the stem should be revised.
4. Conclusion
Gross trunnion failure is a rare but serious complication. It is important to identify patients at risk so that they can be monitored closely. This can lead to earlier intervention which could decrease the morbidity associated with larger revisions.
5. Highlights
- Gross trunnion failure is a rare but serious complication.
- Gross Trunnion Failure (GTF) is defined as considerable corrosion at the head neck junction of a total hip arthroplasty that can lead to fracture or dissociation between the head and neck interface.
- Multiple factors (Impaction force, multiple strikes at impaction, taper conditions, femoral offset and head size, taper design, sex, BMI and alloys) can influence friction fit of the femoral head on the trunnion.
- Patients at risk should be closely monitored.
- Early intervention can decrease morbidity associated with major reconstructions.
References
- Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. The Lancet 370 (2007): 1508-1519.
- Banerjee S, Cherian JJ, Bono JV, et al. Gross trunnion failure after primary total hip arthroplasty. The Journal of arthroplasty 30 (2015): 641-648.
- Hernigou P, Queinnec S, Flouzat Lachaniette CH. One hundred and fifty years of history of the Morse taper: from Stephen A. Morse in 1864 to complications related to modularity in hip arthroplasty. Int Orthop 37 (2013): 2081.
- Gilbert JL, Buckley CA, Jacobs JJ. In vivo corrosion of modular hip prosthesis components in mixed and similar metal combinations. The effect of crevice, stress, motion, and alloy coupling. J Biomed Mater Res 27 (1993): 1533-1544.
- Bansal T, Aggarwal S, Dhillon MS, et al. Gross trunnion failure in metal on polyethylene total hip arthroplasty-a systematic review of literature. International Orthopaedics 4 (2020): 1-3.
- Jacobs JJ, Gilbert JL, Urban RM. Corrosion of metal orthopaedic implants. J Bone Joint Surg Am 80 (1998): 268-282.
- Panagiotidou A, Meswania J, Osman K, et al. The effect of frictional torque and bending moment on corrosion at the taper interface: an in vitro study. Bone Joint J 97 (2015): 463-472.
- Raju S, Chinnakkannu K, Puttaswamy MK, et al. Trunnion corrosion in metal-on-polyethylene total hip arthroplasty: a case series. JAAOS-Journal of the American Academy of Orthopaedic Surgeons 25 (2017): 133-139.
- Weiser MC, Lavernia CJ. Trunnionosis in total hip arthroplasty. JBJS 99 (2017): 1489-1501.
- Langton DJ, Sidaginamale R, Lord JK, et al. Taper junction failure in large-diameter metal-on-metal bearings. Bone Joint Res 1 (2012): 56-63.
- Lanting BA, Teeter MG, Howard JL, et al. Metal-on-metal compared with metal-on-polyethylene: the effect on trunnion corrosion in total hip arthroplasty. J Arthroplast 32 (2017): 2574-2579.
- Whitehouse MR, Endo M, Zachara S, et al. Adverse local tissue reactions in metal-on-polyethylene total hip arthroplasty due to trunnion corrosion: the risk of misdiagnosis. The bone & joint journal 97 (2015):1024-1030.
- McGrory BJ, MacKenzie J, Babikian G. A high prevalence of corrosion at the head–neck taper with contemporary Zimmer non-cemented femoral hip components. The Journal of arthroplasty 30 (2015): 1265-1268.
- Green M, Wishart N, Beaumont R. National Joint Registry for England, Wales, Northern Ireland and the Isle of Man: 12th Annual Report (2017).
- Matharu GS, Pandit HG, Murray DW, et al. Adverse reactions to metal debris occur with all types of hip replacement not just metal-on-metal hips: a retrospective observational study of 3340 revisions for adverse reactions to metal debris from the National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. BMC musculoskeletal disorders 17 (2016):1-2.
- Talmo CT, Sharp KG, Malinowska M, et al. Spontaneous modular femoral head dissociation complicating total hip arthroplasty. Orthopedics 37 (2014): 592-595.
- Ko LM, Chen AF, Deirmengian GK, et al. Catastrophic femoral head-stem trunnion dissociation secondary to corrosion. JBJS 98 (2016): 1400-1404.
- Hemmilä M, Karvonen M, Keemu H, et al. Accolade TMZF trunnion corrosion and mechanical failure 9 yr after primary surgery: A case report and treatment options. Current Orthopaedic Practice 31(2020): 318-321.
- Urish KL, Hamlin BR, Plakseychuk AY, et al. Trunnion failure of the recalled low friction ion treatment cobalt chromium alloy femoral head. The Journal of arthroplasty 32 (2017): 2857-2863.
- Danoff JR, Longaray J, Rajaravivarma R, et al. Impaction force influences taper-trunnion stability in total hip arthroplasty. The Journal of arthroplasty 33 (2018): 270-274.
- Pennock AT, Schmidt AH, Bourgeault CA. Morse-type tapers: factors that may influence taper strength during total hip arthroplasty. The Journal of arthroplasty 17 (2002): 773-778.
- Rehmer A, Bishop NE, Morlock MM. Influence of assembly procedure and material combination on the strength of the taper connection at the head–neck junction of modular hip endoprostheses. Clinical Biomechanics 27 (2012): 77-83.
- Del Balso C, Teeter MG, Tan SC, et al. Trunnionosis: does head size affect fretting and corrosion in total hip arthroplasty?. The Journal of arthroplasty 31 (2016): 2332-2326.
- Mistry JB, Chughtai M, Elmallah RK, et al. Trunnionosis in total hip arthroplasty: a review. Journal of Orthopaedics and Traumatology 17 (2016): 1-6.
- Bolland BJ, Culliford DJ, Langton DJ, et al. High failure rates with a large-diameter hybrid metal-on-metal total hip replacement: clinical, radiological and retrieval analysis. The Journal of bone and joint surgery. British volume 93 (2011): 608-615.
- Dyrkacz RM, Brandt JM, Ojo OA, et al. The influence of head size on corrosion and fretting behaviour at the head-neck interface of artificial hip joints. The Journal of arthroplasty 28 (2013): 1036-1040.
- Lavernia CJ, Iacobelli DA, Villa JM, et al. Trunnion–head stresses in tha: are big heads trouble?. The Journal of arthroplasty 30 (2015): 1085-1088.
- Matthies AK, Racasan R, Bills P, et al. Material loss at the taper junction of retrieved large head metal-on-metal total hip replacements. Journal of Orthopaedic Research 31 (2013): 1677-1685.
- Triantafyllopoulos GK, Elpers ME, Burket JC, et al. Otto Aufranc Award: large heads do not increase damage at the head-neck taper of metal-on-polyethylene total hip arthroplasties. Clinical Orthopaedics and Related Research®. 474 (2016): 330-338.
- Brock TM, Sidaginamale R, Rushton S, et al. Shorter, rough trunnion surfaces are associated with higher taper wear rates than longer, smooth trunnion surfaces in a contemporary large head metal-on-metal total hip arthroplasty system. Journal of Orthopaedic Research 33 (2015): 1868-1874.
- Hussenbocus S, Kosuge D, Solomon LB, et al. Head-neck taper corrosion in hip arthroplasty. BioMed research international 14 (2015).
- Nassif NA, Nawabi DH, Stoner K, et al. Taper design affects failure of large-head metal-on-metal total hip replacements. Clinical Orthopaedics and Related Research® 472 (2014): 564-571.
- Wylde CW, Jenkins E, Pabbruwe M, Bucher T. Catastrophic failure of the Accolade I hip arthroplasty stem: a retrieval analysis study. HIP International 30 (2020): 481-487.
- Runner RP, Bellamy JL, Roberson JR. Gross trunnion failure of a cobalt-chromium femoral head on a titanium stem at midterm follow-up: a report of 3 cases. JBJS Case Connector 6 (2016): 96.
- Swann RP, Webb JE, Cass JR, et al. Catastrophic head-neck dissociation of a modular cementless femoral component. JBJS case connector 5 (2015): 71.
- Spanyer J, Hines J, Beaumont CM, et al. Catastrophic femoral neck failure after THA with the Accolade® I stem in three patients. Clinical Orthopaedics and Related Research® 474 (2016): 1333-1338.
- Wood TJ, Alzahrani M, Langohr D, et al. Catastrophic femoral head trunnion dissociation: A case series with surface wear analysis. HIP International 29 (2019): 1-5.
- Agha RA, Fowler AJ, Saetta A, et al. The SCARE Statement: Consensus-based surgical case report guidelines. International Journal of Surgery (2016).
